Submitted:
25 July 2023
Posted:
26 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
- To explore the experiences of patients and health care professionals regarding the maternal health care services provided in selected hospitals.
- To describe factors affecting the provision of maternal healthcare services in selected hospitals.
- To explore views of midwives and doctors providing MHC services about existing strategies to reduce MMR and improve maternal health provision.
- To explore perceived strategies to improve maternal healthcare services and reduce MMR.
2. Materials and Methods
2.1. Study design
2.2. Setting
2.3. Data collection
2.4. Data analysis
2.5. Trustworthiness
3. Results
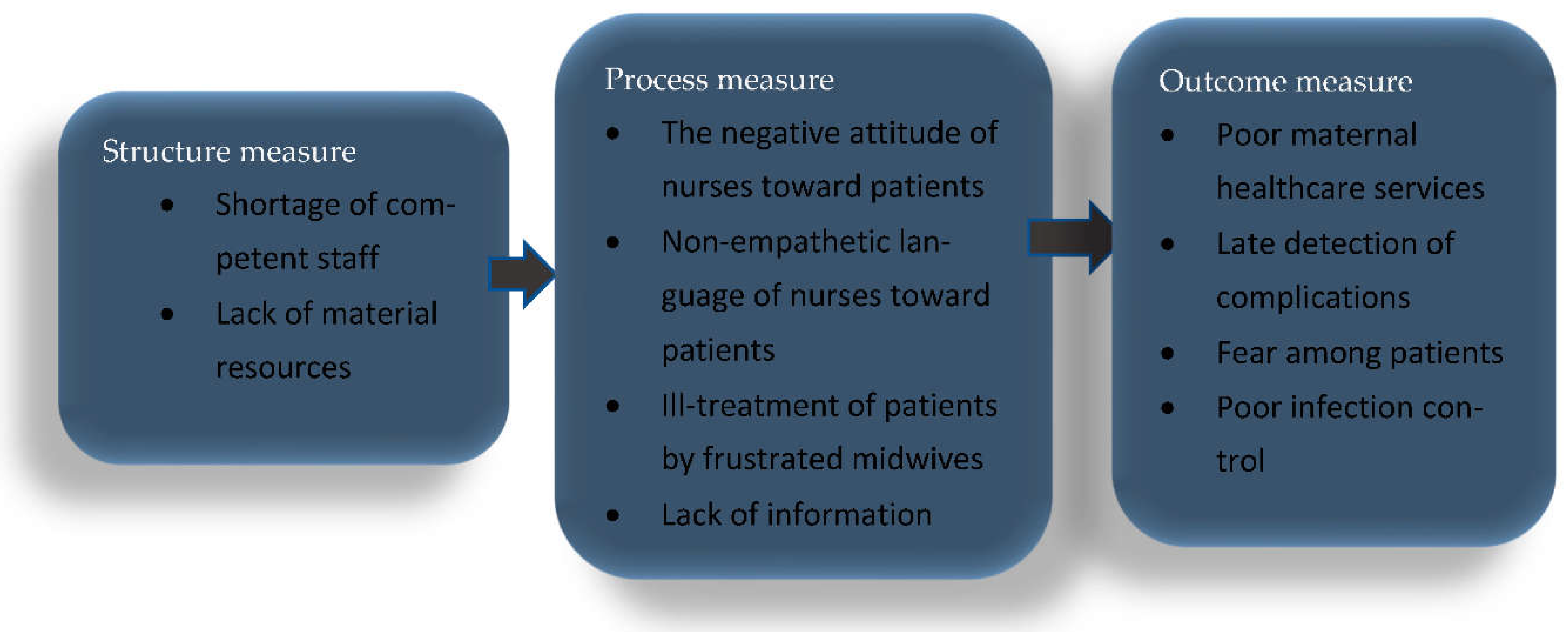
3.1. Theme 1: Patients' Experiences Regarding the maternal health care services provided in p participating hospitals
3.1.1. Negative attitude of nurses towards patients
3.1.2. Non-empathetic language of nurses towards patients
3.1.3. Frustration among Nursing and medical staff
3.1.4. Ill-treatment of Patients by Nurses
3.2. Theme 2: Factors affecting maternal care provision in participating hospitals
3.2.2. Shortage of Staff
3.2.3. Incompetent nursing staff
3.2.4. Poor infection control
3.3. Theme 3: Views of Healthcare Professionals regarding the existing Strategies to improve maternal care
3.3.1. ESMOE (Establishing Essential Steps in Managing Obstetric Emergencies) Formation
3.3.2. CARMMA (Campaign for Accelerated Reduction of Maternal Mortality in Africa) implementation
3.3.3. BANC (Basic antenatal care) establishment
3.3.4. ENAP (Every new-born action plan) Approach
3.4. Theme 4: Perceived Strategies to Improve Maternal Healthcare and Reduce MMR
3.4.1. Continuing in-service training
3.4.2. Launching maternal outreach services
3.4.3. Priority equipment provision
3.4.4. Employ more healthcare professionals
4. Discussion
Limitations of the study
- Some participants (pregnant outpatients) were reluctant to open up, fearing that whatever they said may be used against them.
- The findings of a study from medical doctors working under maternal health services cannot be generalized to a broader population because a smaller number of doctors were interviewed.
- The duration of the interviews was limited as participants needed to agree to set a proper appointment, they preferred to be interviewed the day the researcher visited the hospital, so it limited some to elaborating their responses as they were on duty.
- Female midwives were more willing to participate than males. Therefore, only female midwives were interviewed, and the researcher did not hear the males' views.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement:
Guidelines and Standards Statement:
Acknowledgments
Conflicts of Interest
References
- References must be numbered in order of appearance in the text (including citations in tables and legends) and listed United Nations Children’s Fund. (2021). Maternal mortality data.
- World Health Organisation. (2023). Maternal mortality. Pretoria, South.
- Ramavhoya, T., Maputle, M.S., & Lebese, T.R. (2022). Developing and prioritizing strategies to improve the implementation of maternal healthcare guidelines in South Africa: The nominal group technique. African Journal of primary health care & family medicine. [CrossRef]
- Maswime, S., & Chauke, L. (2022). How to prevent maternal death. University of Venda, Limpopo.
- Tomlinson, J. (2018). Obstetric GA’s. Am I doing it right? School of Clinical Medicine: Discipline of Anaesthesiology and Critical Care, University of Kwazulu-Natal.
- Karkee, R., Budhathoki, B., Maharjan, N., & Manandhar, D.S. (2022). Policies and actions to reduce maternal mortality in Nepal: perspectives of key informants. Sexual and Reproductive Health Matters: Vol 29 (2). [CrossRef]
- Magqadiyane, S. (2022). A model for improving quality of care in maternal health facilities in South Africa. Nursing Department, University of South Africa.
- Mothapo, E.K., Maputle, S.M., Shilubne, H.N., & Netshikweta, L. (2020). Challenges Midwives in Limpopo Province Encounter when Implementing Saving Mothers Recommendations. Vol 14(1): 292-299. [CrossRef]
- Massyn N., Day, C., Ndlovu, N., & Padayachee, T. (2020). District Health Barometer. Durban: Health System Trust.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007. Volume 19, Number 6: pp. 349 – 357. 19, Number 6.
- Donabedian, A (2005) Evaluating the Quality of Medical Care, The Milbank Quarterly, 83(4):691-729.
- Olayinka, O.A., Mombel, M.O., Achi, T.O., & Azibaben, I. (2012). Perceived effects of midwives’ attitude towards women in labor in Bayelsa state, Nigeria. Scholars Research Library.
- Eko, I.E., & Edet, O.B. (2022). Women’s satisfaction with maternity care and its associated factors in Ikot Omin, Nigeria. African Journal of Midwifery and Women’s Health, vol. 16, No. 1. [CrossRef]
- Uwamahoro, V., Sengoma, J.P.S., Ndagijimana, A., & Humuza, J. (2019). Perceptions and Attitude of Midwives on Respectful Maternity Care During Childbirth: A Qualitative Study in Three District Hospitals of Kigali City of Rwanda.
- Malatji, R., & Mabiba, S. (2020). Disrespect and Abuse Experienced by Women during Childbirth in Midwife-Led Obstetric Units in Tshwane District, South Africa: A Qualitative study. Department of Public Health, Sefako Makgatho Health Science University of Venda.Int J Environ Res Public Health. Vol (22), 17 (10): 3667. [CrossRef]
- Experiences and drivers of verbal abuse among women during labor and delivery in Ndola and Kitwe districts of Zambia, Cogent Medicine. [CrossRef]
- Ndikwetepo, M.N., & Strumpher, N. (2017). Midwives’ experiences of stress due to emergency childbirths in a Namibian regional hospital. African Journal of Nursing and Midwifery, Vol 19, No. 1. [CrossRef]
- Tolsma, M., Temane, A., Tagutanazvo, O.B., Lukhele, S., & Nolte, A.G. (2021). Experiences of midwives in providing care to laboring women in varied healthcare settings: A qualitative study. Health SA. [CrossRef]
- Simane-netshisaulu, K.G. (2022). Student to midwife transition: newly qualified midwives experiences in Limpopo province. Health SA. [CrossRef]
- Honikman, S., Fawcus, S., & Meintjes, I. (2015). Abuse in South African maternity settings is a disgrace: potential solutions to the problem. S Afr Med J, 105(4):284-6. [CrossRef]
- Maphumulo, S., Haskins, L., Luthuli, S., & Horwood, C. (2021). Health workers disrespectful and abusive behavior towards women during labor and delivery: a qualitative study in Durban, South Africa. Plos One. [CrossRef]
- Burrowes, S., Holcombe, S., Jara, D., Carter, D., & Smith, K. (2017). Midwives' and patients' perspectives on disrespect and abuse during labor and delivery care in Ethiopia. Pregnancy childbirth, Vol 17 (263). [CrossRef]
- Hussein, A. A., Dahlen, H.G., Ogunsiji, O., & Schied, V. (2018). Women’s experiences of childbirth in Middle Eastern countries: A narrative review. Midwifery, Vol 59. [CrossRef]
- Mayra, K., Matthews, Z., & Padmadas, S.S. (2022). Why do some healthcare providers disrespect and abuse women during childbirth in India? BMC Pregnancy Childbirth, Vol 22 (318).
- Musie, M.R, Peu, M.D., & Pema, V. (2019). Factors hindering midwives' utilization of alternative birth positions during labor in a selected public hospital. Afr J prim healthcare fam, med online, Vol 11, No 1. [CrossRef]
- Moyimane, M.D., Matlala, S.F., & Kekna, M.P. (2017). Experiences of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: a qualitative study. Pan Afr Med J. [CrossRef]
- Makhado, L.C., Mangena-Netshikweta, M.L., Mulondo, S.A., & Olaniyi, F.C. (2022). The roles of obstetric training skills and utilization of maternity unit protocols in reducing perinatal mortality in Limpopo Province, South Africa. Vol 10(4):622. [CrossRef]
- World Health Organisation. (2021). Maternal health. Pretoria, South Africa.
- Moyer, C.A., Rominski, S., Nakau, K.E., Dzomeku, M.V., Agyei-Baffour, P., & Lori, J.R. (2016). Exposure to disrespectful patient care during training: Data from midwifery students at 15 midwifery schools in Ghana. Midwifery, vol 41: 39-44. [CrossRef]
- Chirwa, M.D., Nyasulu, J., Modiba, L., & Limando, M. (2023). Challenges faced by midwives in the implementation of facility-based maternal death reviews in Malawi. BMC pregnancy and childbirth. [CrossRef]
- Netshisaulu, K.G., & Maputle, M.S. (Expected clinical competence from midwifery graduates during community services placement in Limpopo province, South Africa. Health SA. [CrossRef]
- Scar, S., Turgut, H., Toprak, S., Cirak, B., Coskun, E, Yilmaz, O., & Tekin, K. (2006). A retrospective study of central nervous system shunt infections diagnosed in a university hospital over four years. BMC Infectious Diseases. [CrossRef]
- Maphumulo, W.T, & Bhengu, B.R. (2019). Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curations. [CrossRef]
- Lowe, H., Woodd, S., Lange, I., Janjanin, S., Barnet, J., & Graham, W. (2021). A qualitative study of challenges and opportunities for infection prevention and control in hospitals in conflict-affected settings. BMC conflict and health. [CrossRef]
- Makin, J.D., Bergh, A.M., Bezuidenhout, C.M., & Pattinson, R.C. (2015). Essential steps in managing obstetrics emergencies (ESMOE): Is onsite saturation training equivalent to off-site saturation training? University of Cape Town.
- Lubbe, W. (2013). CARMMA-The campaign for accelerated reduction of maternal mortality in Africa. Journal of Neonatal Nursing, 19 (6): 301-302. [CrossRef]
- Sewnunan, A. (2021). A critical analysis of the implementation of obstetric management guidelines, on common causes of maternal deaths, as applicable to midwives. Faculty of health sciences, Durban University of Technology.
- South African National Department of Health. (2021). South African Maternal, Perinatal, and Neonatal health policy.
- Spiby, H., Stewart, J., Watts, K.., Hughes, A.J., & Slade, P. (2022). The importance of face-to-face, group antenatal education classes for first-time mothers: A qualitative study. Midwifery, Epub.
- Mirbana-Hashemi, F., Tafeyi, B., Rampisheh, Z., Tehrani-Banihashemi, A., Ramezani, M., Khalili, N, Pournik, O., Taghizadeh-Asl, R., Habibelani, A., Heidarzarzadeh, M., & Moradi-Lakeh, M. (2021) progress towards Every New-born Action Plan (ENAP) implementation in Iran: obstacles and bottlenecks. BMC pregnancy childbirth. [CrossRef]
- Bac, M., Pattinson, R.C., & Bergh, A, M. (2019). Changing maternal and perinatal health priorities in Gert Sibande District, South Africa. University of Pretoria, Vol 109, No 11.
- Lumadi, G.T., & Matlala, S.M. (2019). Perceptions of midwives on shortage and staff retention at a public hospital in Tshwane District. ResearchGate. [CrossRef]
- Welsh, J., Houkptain, H., Gross, M.M., Hanson, C., & Moller, A.B. (2022). Do in-service training materials for midwifery care providers in Sub-Saharan Africa meet international competency standards? A scooping review 2000-2020. BMC Medical Education. [CrossRef]
- Abimbola, S., Baatiema, L., & Bigdeli, M. (2019). The impacts of decentralization on health system equity, efficiency, and resilience: a realist synthesis of the evidence. Health Policy Plan. [CrossRef]
- Goyet, S., Broch-Alvarez, V., & Becker, C. (2019). Quality improvement in maternal and new-born healthcare: lessons from programs supported by the German development organization in Africa and Asia. BMJ Glob Health. [CrossRef]
- Nyanjara, s., Machuve, D., & Nykanen, P. (2022). Maternal and Child Health Care Quality Assessment: An Improved Approach Using K-means Clustering. Journal of Data Analysis and Information Processing, vol 10, NO. 3. [CrossRef]
- Matlala, M.S., & Lumadi, T.G. (2019). Perceptions of midwives on shortage and staff retention at a public hospital in Tshwane District. Science direct. [CrossRef]
- Kandjimi, E. (2021). Effects of the shortage of midwives on performance and quality of care in the maternity ward, Rundu intermediate hospital and Nyangana district hospital, Kavango East region. Master of Nursing, University of Namibia.
- Khosvari, S., Babaey, F., & Abedi, P. (2022). Strategies to improve the quality of midwifery care and developing midwife-centered care in Iran: analyzing the attitudes of midwifery experts. BMC pregnancy childbirth. [CrossRef]
| PARTICIPANTS (CODES) | GENDER | AGE | HOSPITAL | NO. OF YEARS WORKING IN A HOSPITAL |
|---|---|---|---|---|
| M 1 | Female | 52 | Hospital E | Two years |
| M 2 | Female | 29 | Hospital E | Eight years |
| M 3 | Female | 35 | Hospital E | Two years |
| M 4 | Female | 29 | Hospital A | Two years |
| M 5 | Female | 31 | Hospital A | 14 years |
| M 6 | Female | 42 | Hospital A | Four years |
| M 7 | Female | 40 | Hospital F | Four years |
| M 8 | Female | 56 | Hospital F | 16 years |
| M 9 | Female | 30 | Hospital F | Three years |
| M 10 | Female | 31 | Hospital C | Two years |
| M 11 | Female | 25 | Hospital C | Six years |
| M 12 | Female | 27 | Hospital C | 11 years |
| PARTICIPANTS (CODES) | GENDER | AGE | HOSPITAL | NO. OF YEARS WORKING IN A HOSPITAL |
|---|---|---|---|---|
| Dr 1 | Male | 34 | Hospital E | Three years |
| Dr 2 | Male | 38 | Hospital A | Three years |
| Dr 3 | Male | 40 | Hospital F | Five years |
| Dr 4 | Female | 31 | Hospital C | Two years |
| PARTICIPANTS (CODES) | GENDER | AGE | HOSPITAL |
|---|---|---|---|
| PO 1 | Female | 31 | Hospital E |
| PO 2 | Female | 33 | Hospital E |
| PO 3 | Female | 24 | Hospital E |
| PO 4 | Female | 19 | Hospital A |
| PO 5 | Female | 32 | Hospital A |
| PO 6 | Female | 23 | Hospital A |
| PO 7 | Female | 20 | Hospital F |
| PO 8 | Female | 38 | Hospital F |
| PO 9 | Female | 26 | Hospital F |
| PO 10 | Female | 29 | Hospital C |
| PO 11 | Female | 40 | Hospital C |
| PO 12 | Female | 31 | Hospital C |
| Experiences in maternal health services | Factors affecting maternal health services | Views on existing strategies/approaches | Recommended strategies to improve maternal healthcare and reduce MMR |
|---|---|---|---|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




