1. Introduction
CPMs (Congenital Pulmonary Malformations) are a wide spectrum of congenital lung benign lesions such as Pulmonary Sequestration (PS), Congenital Cystic Adenomatoid Malformation (CCAM), Congenital Lobar Emphysema, bronchial atresia, and others intermediary forms.
CCAMs are the most frequent, occurring in the 25% of all CPMs [
1] and consisting of an hamartomatous cystic replacement of normal lung parenchyma. CCAMs are gland-like cystic lesions of different sizes classified by Stocker et al. [
2] in type 1 (large cysts of 3-10 cm of diameter), type 2 (smaller cysts of <2 cm), type 3 (minute cysts of < 0.3 cm). Later, two other types were added: type 0 (solid malformation often not compatible with life) and type 4 (few peripheral cysts lined by alveolar epithelium).
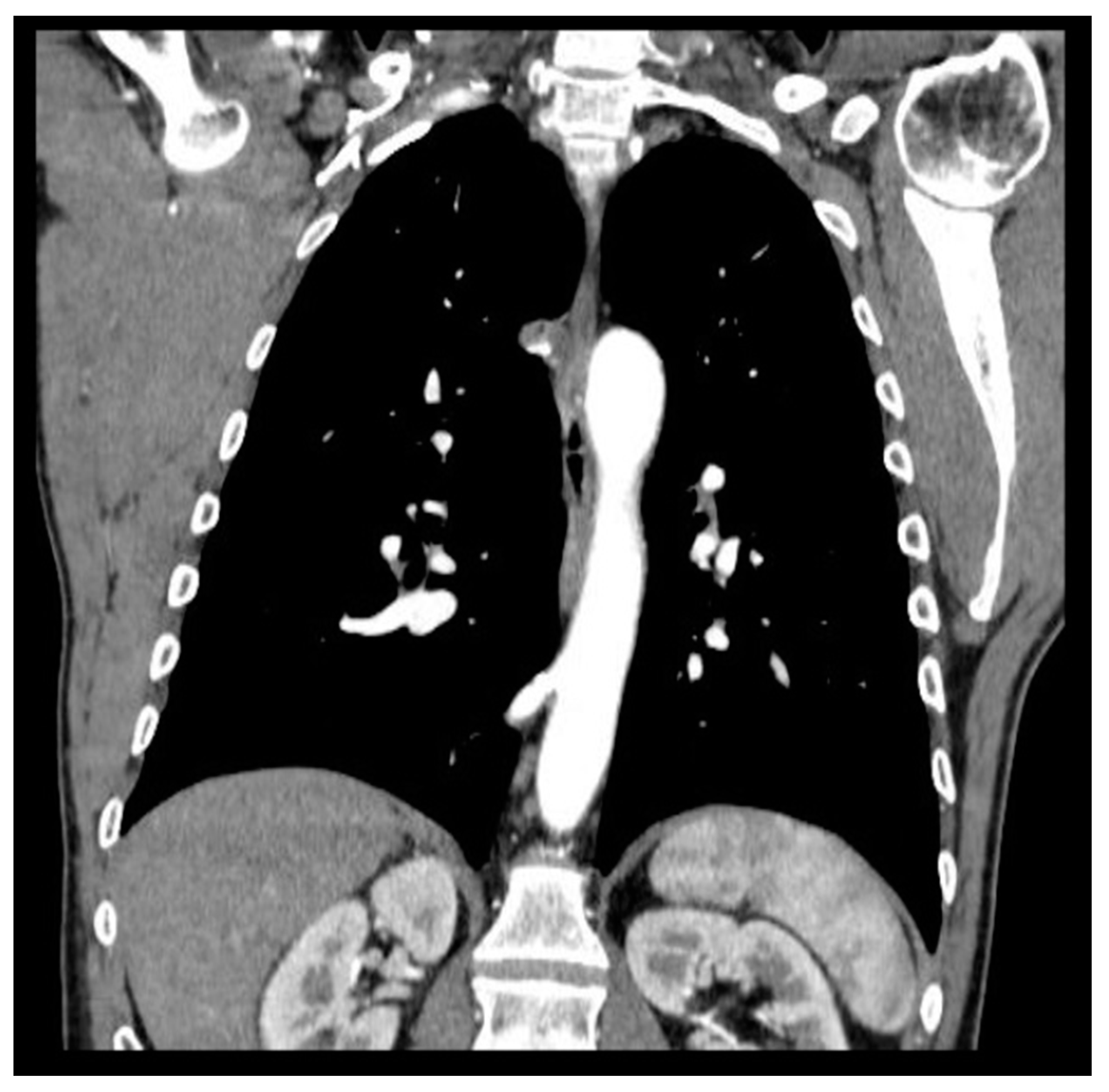
Pulmonary Sequestration (PS) represents the 0.15–6.45% of CPMs [
3]; it is characterized by a mass of non-functioning lung tissue separated from the normal tracheobronchial tree and receiving vascular supply from a systemic artery (
Figure 1). It is classified as Intra-lobar PS (IL-PS) when it is incorporated in the parenchyma of a lobe, and as Extra-lobar PS (EL-PS) when it is separated from the adjacent normal parenchyma by its own pleural envelope.
CPMs represent anomalies occurring because of abnormal embryonal developing of bronchial tree and they can often be associated with other congenital anomalies or with each other. In fact, CCAM is described in the 50% of Extra-lobar PS and in the 15% of Intra-lobar PS. [
4]
In the last decades, the spread of prenatal ultrasonography led to a progressive increase of antenatally detection of CPMs, confirmed by radiological images (Chest Rx or CT scan) early after birth.
Most neonates are asymptomatic at birth (> 75%). Clinical presentation and severity depend on the extent and on the localization of the lesions.[
5,
6] CPMs clinically present with respiratory symptoms (such pneumonia, emoptysis, productive coughing, recurrent wheeze) due to infective complications, occurring most frequently at an average age of 7 months, or later during the growth. In fact, Prenatal diagnosis is sometimes missed, and detection may occur later, either by chance or because of unexplained recurrent or persistent respiratory symptoms or signs, occurring beyond infancy, even in adolescence and/or adulthood. As reported in previous studies, the most frequent symptoms related to CPMs are pneumonia, recurrent bronchitis, bronchiolitis, severe cough, hemoptysis, dyspnea and respiratory distress. [
7,
8]
Surgical treatment is mandatory for symptomatic lesions. On the contrary, the management of asymptomatic lesions is rather controversial, while some authors sustained a conservative approach before respiratory symptoms occur. Nevertheless, there is a wide concern in literature about the indication of surgical resection even for asymptomatic lesions, to prevent recurrent respiratory symptoms, to ensure a safer surgery before inflammation complicates the lesion and finally to avoid the rare but possible malignant transformation.[
6] A preliminary study from Rotterdam evaluating pulmonary function in children undergoing pulmonary lobectomy before and after the age of 2 years showed no differences. Early resection before the development of respiratory complications such as pneumonia may also facilitate the thoracoscopic approach of surgical treatment in experienced hands.
In that order, surgery is indicated early after lesions’ detection. Moreover, considering that detection is most frequent in neonates and infants, parenchyma-sparing techniques have been proposed, depending on lesion’s size and localization. Though, potential lung growth in paediatric patients is described justifying an early lobectomy.[
7] To date, there is not a consensus indicating the correct extent of surgical resection between lobectomy and sub-lobar resection for CPMs, in both adult and paediatric patients.
This retrospective multicentric study aims to identify the appropriate surgical treatment to prevent the recurrence respiratory symptoms related to the lesions.
2. Materials and Methods
This multi-institutional retrospective observational study included 96 consecutive paediatric and adult patients surgically treated between 2010 and 2020 for CPMs in 4 centres: La Sapienza University of Rome, ASST Valtellina e Alto Lario of Sondrio, Bambino Gesu` Children’s Research Hospital of Rome and IRCCS Ca’ Granda Foundation – Policlinico of Milan.
Lesions were detected radiologically by prenatally ultrasonography of the second pregnancy trimester, then confirmed by Computed Tomography (CT) scan within the first 3 months after birth or immediately in symptomatic lesions. Lesions detected prenatally were surgically treated within the first year of age, as previously reported8. In all the other cases, lesions were detected incidentally or when symptomatic by CT scan and treated early after the diagnosis.
Preoperative assessment included respiratory functional test (spirometry and blood gas analysis) and cardiovascular test (electrocardiography and echocardiography when required). In infant before 5 years old, infant pulmonary function test was used to assess functional capacity analysis9.
To minimize selection bias a 2, 1 propensity score matching was performed based on predetermined confounders and baseline characteristics (sex and lesion side) to identify two homogenous groups of patients: finally, 75 patients with homogenous characteristics were selected and divided into group A (n=50) treated by lobectomy; group B (n=25) treated by sub-lobar resections (segmentectomies). According to the propensity score matching n= 21 patients were excluded because they did not match the variables. Videothoracoscopy was performed with a bi-portal access. Thoracotomy was performed with a muscle-sparing technique when VATS was not eligible because of lesions’ dimensions, localization, and surgical expertise to manage intra-operative complications. The choice to perform lobectomy or sub-lobar resection was made considering radiological and intra-operative characteristics of the lesion (lesions distant < 1 cm from the fissure and/or bigger than 4 cm of maximum diameter at pre-operative CT scan and/or involving two or more pulmonary segments, were considered for lobectomy).
An accurate histopathological analysis was done. Paediatric patients underwent clinical follow-up once a year up to 18 years then addressed to their general practitioner who indicates new surgical consulting in case of relapse. Adult patients were followed up for the first year, then addressed to the general practitioner as well. Demographics characteristics, diagnosis technique, histology, time of surgery, length of hospital stay, length of chest tube permanence, intra-operative and post-operative complications and symptoms recurrence were compared between the two groups.
The study was approved by the institutional review board of Sant’Andrea Hospital (PROT. N. 188 SA/2022) and informed consent was obtained before surgery.
Data were prospectively collected and stored in Excel database (Microsoft Corp, Redmond, WA). Quantitative variables were expressed as mean ± standard deviation and compared using T-test. Nominal variables were expressed binarily (presence -1 or absence – 0) and compared by Chi Square, after the Fisher’s exact test was performed. P-values less than 0.05 were considered statistically significant.
A univariate logistic regression analyses was performed to derive crude estimates of association between predictors and outcomes. After univariate analyses, variables with P-value less than 0.05 were included in a multivariate logistic regression model to identify potential independent protective or risk factors for symptoms recurrence. The adjusted odd ratios (ORs) and 95% confidence intervals (CI) were calculated to estimate and measure the association using 1000 bootstrapping samples.
Data were analyzed using statistical package SPSS, version 25.0 (SPSS Software, IBM Corp., Armonk, NY, USA).
3. Results
General characteristics of patients and postoperative results are showed in
Table 1.
In group A the average age was 12,7 years and 4,2 years in group B, with a significant statistical difference at T test analysis (p = 0,012).
Male patients were n=30 (60%) in group A and n=12 (48%) in group B.
In group A n=42 (84%) received prenatal diagnosis and n=17 (34%) were symptomatic at the diagnosis, while in group B n=18 (72%) had prenatal diagnosis and n=6 (24%) were symptomatic.
In group A the lesion was right sided in n=28 (56%) patients and in group B it was right sided in n=10 (40%) patients.
Operatory time was a mean 167 minutes in group A and 161 minutes in group B, without significative statistical significance at t test analysis.
VATS was performed in n= 31 (62%) patients in group A and in n=16 (64%) in group B, all in the last 10 years. Mini thoracotomy was performed in n=19 (38%) patients in group A and in n=9 (36%) in group B.
Histopathological analysis detected n=29 (58%) cases of combined lesions (PS and CCAM) in group A and n=8 (32%) cases in group B, with a significant statistical difference (p=0.030). Equally, CCAM alone was detected in n=19 (38%) of patients in group A and in n=2 (8%) in group B, with a significant statistical difference (p=0.005).
Intra-operative complications (pulmonary laceration, haematoma, haemorrhage) were significantly higher in sub-lobar resection group: n=6 (24%) in group B vs n=2 (4%) in group A, (p=0.014).
Post-operative complications (persistent air leak, slow re-expansion, bleeding, chest wall hematoma, prolonged liquid leaks) occurred in n=5 (10%) of patients in group A vs n=3 (12%) in group B, without a significative difference.
Hospital stay was < 7 days for n= 38 (76%) in group A and for n= 16 (64%) in group B, without a significant difference. The average of hospital stay was 8 days for group B (median of 7 days) and 8,80 days for group A (median of 5 days), without a significative difference at t test analysis.
Length of chest tube permanence was > 7 days for n=6 (12%) patients in group A and for n=9 (36%) patients in group B, with significant difference (p=0.018). An average of 3,7 days for group A (median of 3 days) and 6,6 days for group B (median of 6 days), with a significative difference at t test analysis (p= 0,005).
Finally, recurrence of respiratory symptoms related to the lesion was higher in the sub-lobar group (n=6; 24% in group B vs n=2; 4% in group A; p=0.002) as it is shown in
Table 2, that reports differences among patients who experienced symptoms’ recurrence and patients who did not.
The average follow-up period was 10,5 years.
Univariate analyses identified as risk factors for symptoms recurrence after surgical treatment: pulmonary sequestration (p=0.002), sub-lobar resection (p=0.019), intra-operative (p=0.020) and post-operative (p=0.020) complications and associated neoplasm (p=0.017). Multivariate logistic regression confirmed sub-lobar resection (p=0.040), post-operative complications (p=0.022) and associated developed neoplasm (at the edge of statistical significance) as risk factors for symptoms recurrence after surgical treatment. (
Table 3)
4. Discussion
CPMs are rare benign lesions involving 30-42 cases per 100’000 inhabitants per year [
9,
10,
11] with an increased risk for infective complications. In the last decades, the extensive use of prenatal ultrasonography has led to a progressive increase in antenatally detection of CPMs. For this reason, the highest incidence of the pathology occurs in pediatric patients, but the diagnosis may be missed until later in life, even in adulthood. Surgery is mandatory for symptomatic lesions to solve respiratory symptoms, to prevent infective complications and to avoid the rare risk of malignant transformation. Nevertheless, there is wide concern in literature about surgery indication even for asymptomatic lesions, thus, to prevent late infections and/or malignancies, to guarantee more time for alveolar compensatory growth and to reduce the risk for emergency surgery. The incidence of post- operative complications is assumed to be lower after early elective operation for CPMs than after an urgent intervention for CPMs when infective complications occurred. [
10]
Surgery for CPMs is indicated early after lesions’ detection and many studies exist in literature dealing with surgical treatment options (thoracotomy vs VATS) [
12,
13,
14,
15] but there is no a standardized consensus on the extension of surgical resections indicated between lobectomy and sub-lobar resections. A study by Baird et al. [
12] recommends lobectomy (Recommendation: Weakly agree) as the procedure of choice, especially when the lesion is confined to a single lobe. There are no guidelines in literature on the correct extension of surgical resection but considering the best practice, formal lobectomy is superior to segmentectomy. The present study investigates the possibility to identify a consensus among surgeons who approach these pathologies.
In our series the most of patients underwent sub-lobar resections had an average age of 4,2 years vs 12,7 years in the lobectomy group. Theoretically, it is possible to speculate that parenchyma-saving resection is the optimal choice for children, for preserving total lung capacity. Nevertheless, it should be noted that parenchyma-saving resection can be complicated by a prolonged air leak in the early postoperative period, and in patients with a residual lesion, malignant transformation as well as recurrent infections could develop during follow-up, which would necessitate a repeat operation. However, it is demonstrated that neonates and infant patients have a lung growth potential within the first years of life. [
16] Infants and children tolerate lobectomy well, so that the total lung volume and gas exchange capacity return toward normal during somatic maturation.[
7] For these reasons the ideal extent of resection is still controversial.[
17]
Both Video-thoracoscopy (VATS) and thoracotomy are described for the treatment of CPMs. VATS is the procedure of choice; it is demonstrated to be safe and effective, and it is recommended to reduce morbidity related to thoracotomy, guaranteeing cosmetic benefit, and reducing pain
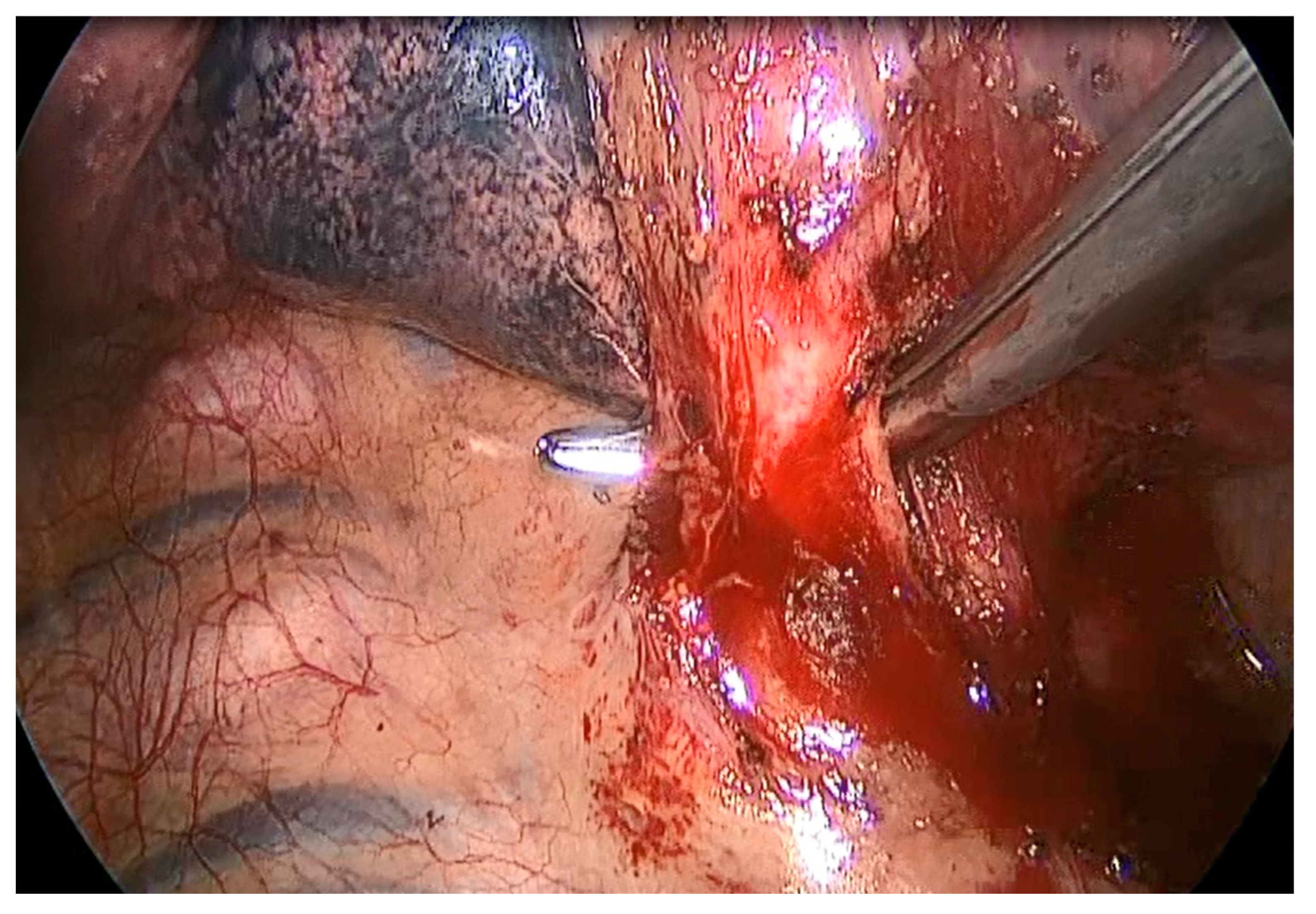
18. Thoracotomy allows easy access to hilar structures using different intercostal spaces, making easier than VATS the management of anomalous vascularization and the variable size of the lesions. Moreover, dense adhesions due by recurrent infections of the lesion can make VATS dissection more difficult and thoracotomy is sometimes required to better manage an eventual vessel injury when the aberrant or varicose bronchial arteries are not well defined by preoperative imaging (
Figure 2), so it is mandatory to consider conversion whenever necessary. In our series, VATS were performed in n=31; 62% in group A and n=16; 64% in group B in the last 10 years, reflecting the increasing surgical expertise in mini-invasive surgery over the years. Conversion was required only for two patients to manage intra-operative complications (anomalous vessel laceration; tough adhesions). No differences in outcome were found in comparison with the open access approach in the present series.
The results reported are in line with previous smaller published studies (Kim et al., Stanton et al) [
16,
17] reporting the superiority of lobectomy for the stable remission of symptoms recurrence.
Our comparing analysis showed that symptoms recurrence after surgical treatment for CPMs was lower in lobectomy group compared to sub-lobar group, with statistical significative difference (p=0.014). Even intra-operative complications (pulmonary laceration, haematoma, haemorrhage) were more frequent in the sub-lobar resections (24% vs 4%, p= 0.014). This result probably explains the longest period of chest tube permanence in group B than in group A, with statistically significative difference. There was not a significant difference in post-operative complications, surgical time or hospital stay in the two groups but there was a difference in chest tube drainage permanence that was longer in the sub-lobar group, probably due to the more frequent intra-operative complications registered in the overmentioned group.
The comparison of histopathological samples showed an increased frequency of CCAM (isolated lesion or associated to Sequestration) in the lobectomy group then in the sub-lobar resection group. Histopathological analysis represents the definitive diagnosis [19] because radiological definition is not always conclusive. In fact, contrast chest CT is considered the most accurate examination but hyperlucent lesions presuppose an overlapping spectrum and consensus and cooperation between radiologists and histopathologists are of paramount importance for the definitive diagnosis. [
20] So, prenatal imaging is not predictive of post-natal histology and surgical resection is also recommended to obtain a final diagnosis of the lesion, to distinguish isolated lesions from associated CPMs, generally related to a higher risk for infective complications and/or malignant transformation. [
21]
Analysing the causes of symptoms recurrence (presented in 8 patients, 11% of the entire population), the presence of isolated sequestration (p=0.062), intra- and postoperative complications (p=0.035), associated neoplasm at histopathological analysis (p=0.014) and sub-lobar resections (p=0.014) seemed significantly related to recurrence.
These variables were then analysed in a univariate analysis that confirmed them as potential risk factors for symptoms’ recurrence. The multivariate logistic regression confirmed the variables shown in
Table 3 as risk factors for symptoms’ recurrence.
Recurrence of symptoms was defined by the occurrence of productive cough, fever, haemoptysis related to pneumonia, bronchiolitis and/or recurrent bronchitis during the follow-up period.[
8] According to Calzolari et al. symptoms such asthma, recurrent wheeze and/or respiratory distress present after surgery are not considered recurrence of symptoms caused by the lesions; but symptoms related to the same congenital developmental abnormality that causes the development of CPMs. Patients presenting with these latter symptoms were not considered affected by recurrence after treatment. In fact, lesions may not be limited to a single lung segment, but the whole respiratory structure may be affected to differing degrees, which may result in persistent respiratory symptoms after surgery that tend to regress spontaneously.[
10]
Lobectomy is more appropriate even to prevent the rare risk of malignant transformation (rhabdomyosarcoma, pulmonary blastoma), most frequently described in isolated or associated CCAM. [
21,
22]
According to literature, patients undergoing parenchyma-saving resection are likely to have early postoperative morbidities such as recurrent pulmonary infection or prolonged air leakage, and in cases of residual lesion, even malignant transformation. [
23] The systematic review by Stanton et al. demonstrated a 15% rate of residual disease after segmental resection vs 0% with lobectomy. [
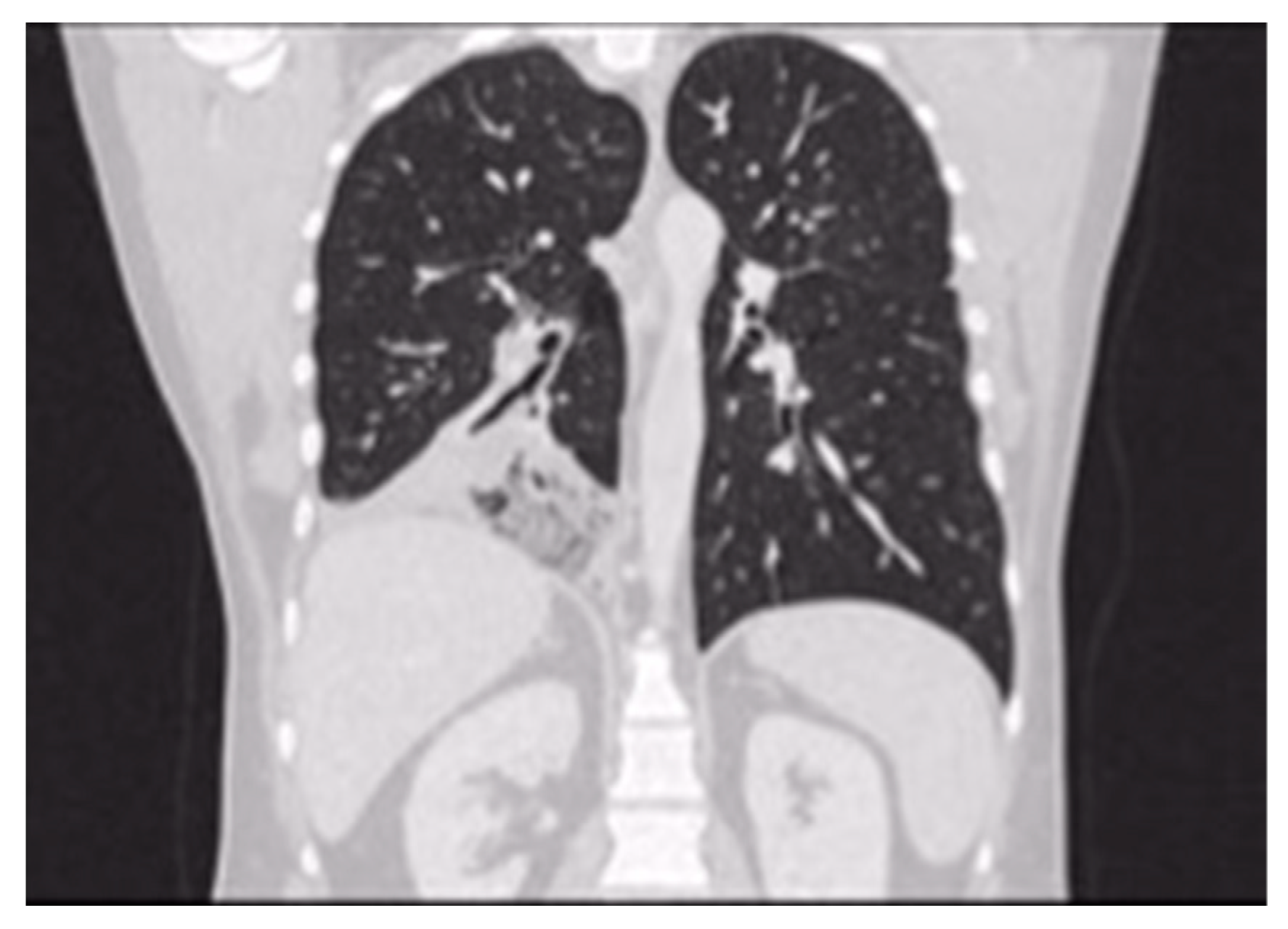
16] In our experience a patient treated for CCAM by B9 segmentectomy at the age of 13, developed successive malignant transformation 14 years later (bilaterally metastatic adenocarcinoma) in the residual right lower lobe, primarily identified by respiratory symptoms occurrence (productive coughing) and radiological evidence of lung cancer abscess (
Figure 3). In fact, performing subtotal lobectomy or segmentectomy or at worst, an atypical resection, would risk leaving lesions remnants that could later develop in lung cancer.
Our study has several limitations: data were retrospectively collected; study population was rather small and so the power of our suggestions is not so strong as to be conclusive; parenchyma-saving resection was performed in only selected cases (peripheral lesions, smaller than 3 cm diameters). However, considering the rarity of the pathology, this is one of the largest studies in literature on the topic.
A prospective, randomized controlled trial would be helpful to determine if parenchyma-saving resection could be justified in patients with localized CPMs.
5. Conclusions
Surgical excision has yet been proven to be the treatment of choice for CPMs although a general consensus on the best type of surgery is not proved. For the best of our knowledge, despite the small sample due to the rarity of the pathology described, the present multicentric study is one of the largest in literature comparing the two different surgical approaches (lobectomy vs sub-lobar resections) for CPMs.
With the limit of a small sample, retrospective work, the present study aims to demonstrate the most appropriate surgical treatment for the stable remission of CPMs in both adult and paediatric patients. in conclusion, lobectomy seems to be the treatment of choice, compared to sub-lobar resection, resulting in lower or null rate of intra- and postoperative complications, resulting in lower incidence of respiratory symptoms’ recurrence and preventing the rare risk of possible future malignant transformation.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, Beatrice Trabalza Marinucci, Cecilia Menna and Paolo Scanagatta; methodology, Beatrice Trabalza Marinucci and Cecilia Menna; software, Silvia Fiorelli; validation, Erino Angelo Rendina and Mohsen Ibrahim; formal analysis, Beatrice Trabalza Marinucci, Cecilia Menna and Silvia Fiorelli; investigation, Matteo Tiracorrendo, Giuseppe Naldi, Francesco Macchiarini and Alessandro Inserra; resources, Beatrice Trabalza Marinucci and Matteo Tiracorrendo; data curation, Beatrice Trabalza Marinucci, Cecilia Menna and Silvia Fiorelli; writing—original draft preparation, X.X.; writing—review and editing, Beatrice Trabalza Marinucci and Cecilia Menna; visualization and supervision, Erino Angelo Rendina, Paolo Scanagatta and Mohsen Ibrahim. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Sant’Andrea Hospital, La Sapienza University (protocol code 188 SA/2022, 28 September 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Conran RM, Stocker JT. Extralobar sequestration with frequently associated congenital cystic adenomatoid malformation, type 2: report of 50 cases. Pediatr Dev Pathol 1999, 2, 454–63. [Google Scholar] [CrossRef] [PubMed]
- Stocker, JT. Congenital pulmonary airway malformation: a new name and an expanded classification of congenital cystic adenomatoid malformation of the lung. Hystopathology 2002, 41, 424–31. [Google Scholar]
- Wang A, D’Amico T, Berry M. Surgical management of congenital pulmonary malformations after the first decade of life. Ann Thorac Surg 2014, 97, 1933–8. [Google Scholar] [CrossRef] [PubMed]
- Sfakianaki AK, Copel JA. Congenital cystic lesions of the lung: congenital cystic adenomatoid malformation and bronchopulmonary sequestration. Rev Obstet Gynecol 2012, 5, 85–93. [Google Scholar]
- Adzick S, Flake A, Crombleholme F. Management of congenital lung lesions. Semin Pediatr Surg 2003, 1, 10–16. [Google Scholar]
- Rashmi S, Davenport M. The argument for operative approach to asymptomatic lung lesions. Semin Pediatr Surg 2015, 24, 187–95. [Google Scholar] [CrossRef]
- Kim HK, Choi YS. Treatment of congenital cystic adenomatoid malformations: should lobectomy always be performed? Ann Thorac Surg 2008, 86, 249–53. [Google Scholar] [CrossRef]
- Trabalza Marinucci B, Maurizi G, Vanni C et al. Surgical treatment of pulmonary sequestration in adults and children: long-term results. Interact CardioVasc Thorac Surg 2020, 31, 71–77. [Google Scholar] [CrossRef]
- Lesnick BL, Davis SD. Infant pulmonary function testing. Overview of technology and practical considerations—new current procedural terminology codes effective 2010. Chest 2011, 139, 1197–202. [Google Scholar]
- Calzolari F, Braguglia A, Valfre` L et al. Outcome of infants operated on for congenital pulmonary malformations. Pediatr Pulmonol 2016, 51, 1367–72. [Google Scholar] [CrossRef]
- Andrade CF, Ferreira HPC, Fischer GB. Congenital lung malformations. J Bras Pneumol 2011, 37, 259–71. [Google Scholar]
- Baird R, Puligandla P, Laberge JM. Congenital lung malformations: Informing best practice. Seminars in Pediatr Surg 2014, 23, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Wang LM, Cao JL, Hu J. Video-assisted thoracic surgery for pulmonary sequestration: a safe alternative procedure. J Thorac Dis 2016, 8, 31–6. [Google Scholar]
- Chengwu L, Pu Q, Ma L. Video-assisted thoracic surgery for pulmonary sequestration compared with posterolateral thoracotomy. J Thorac Cardiovasc Surg 2013, 146, 557–61. [Google Scholar] [CrossRef] [PubMed]
- Esposito C, Bonnard A, Till H et al. Thoracoscopic Management of Pediatric Patients with Congenital Lung Malformations: Results of a European Multicenter Survey. Laparoendosc Adv Surg Tech 2021, 31, 355–362. [Google Scholar] [CrossRef]
- Stanton M, Njere I, Ade-Ajayi N et. Al. Systematic review and meta-analysis of the postnatal management of congenital cystic lung lesions. Journal of Pediatric Surgery 2009, 44, 1027–1033. [Google Scholar] [CrossRef]
- Morini F, Zani A, Conforti A et al. Current management of congenital pulmonary airway malformations: a “European Pediatric Surgeon’s Association” survey. Eur J Pediatr Surg 2018, 28, 1–5. [Google Scholar] [CrossRef]
- Annunziata F, Bush A, Borgia F. Congenital lung malformations: unresolved issues and unanswered questions. Front Pediatr 2019, 7, 239. [Google Scholar] [CrossRef]
- Kyncl M, Koci M, PtackovA L et al. Congenital bronchopulmonary malformation: CT histopathological correlation. Biomed Pap Med 2016, 160, 533–537. [Google Scholar] [CrossRef]
- Hirose R, Suita S, Taguchi T et al. Extralobar pulmonary sequestration mimicking cystic adenomatoid malformation in prenatal sonographic appearance and histological findings. J Pediatr Surg 1995, 30, 1390–3. [Google Scholar] [CrossRef]
- Messinger YH, Stewart DR, Priest JR et al. Pleuropulmonary blastoma: a report on 350 central pathology-confirmed pleuropulmonary blastoma cases by the International Pleuropulomonary Blastoma Registry. Cancer 2015, 121, 276–85. [Google Scholar] [CrossRef] [PubMed]
- Preziosi A, Morandi A, Galbiati F et al. Acute haemothorax and pleuropulmonary blastoma: Two extremely rare complications of extralobar pulmonary sequestration. Journal of Pediatr Surg 2022, 80, 102238. [Google Scholar]
- Muller C, Berrebi D et al. Is radical lobectomy required in congenital cystic adenomatoid malformation? Journal of pediatr Surg 2012, 47, 642–64. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).