1. Introduction
Since 2020, the SARS-CoV-2 pandemic has been determining a high number of COVID-19 cases with severe respiratory failure who were frequently hospitalized in Intensive Care Units (ICUs) with a well-documented concurrent rise in morbidity and mortality among them [
1]. Nevertheless, there is still limited evidence of the real impact that this pandemic had on the epidemiology of resistant microorganisms (ROs) in this setting [
2]. Some retrospective reports showed a lower incidence of infections due to ROs during the pandemic, with a less significant impact in COVID wards versus non - COVID ones [
3]. In particular, in 2021 Grasselli et al. reported bacterial infection incidence at 44.7/1000 ICU days with a 35% of ROs infections among ICU COVID patients [
4]. A 2020 case series of Cusumano et al highlighted the pivotal role on mortality of secondary bacterial infections in COVID patients [
5]. A British report showed that bacterial co-infections at admission were detected in 14% of ICU patients, whilst 85% of them were already receiving antibiotics at that stage. In addition, ICU-acquired infections were observed in 54% of patients [
6]. Langford and colleagues commented that the COVID-19 pandemic may have hastened the emergence, transmission and diffusion of antimicrobial resistance, particularly for Gram-negative organisms in hospital settings [
7]. However, the same authors reported considerable heterogeneity in both the antimicrobial resistance metrics used, and the rate of resistance reported across studies [
7]. In addition, several reports highlighted the changing epidemiology of ROs in ICUs in Europe during the different waves of COVID pandemic and, in particular, the significant increase of multidrug resistant
A. baumannii in Italian ICUs [
8,
9,
10,
11].
Aim of our study was to describe and analyze the impact of the SARS-CoV-2 pandemic on ICU microorganisms resistance patterns.
2. Materials and Methods
This is a single center retrospective study conducted in a general hospital of national relevance, highly specialized and treatment intensity organized based, located in northern Italy. The hospital has a pavilions-based structure of 458 beds, with more than 15,000 routine admissions/year and more than 8,600 medical procedures in outpatient and day surgery settings. In particular, the ICU has 8 beds, 6 of which are in an open space area and 2 in single isolated rooms. During the first pandemic wave ICU beds were initially increased up to 16 for very few months, then remained at 12 for several months and went up and down following the different waves of the COVID pandemic [
1]. All microorganisms isolated from all patients admitted to E.O. Galliera ICU from January 2018 to December 2022 were included. Their antibiotic resistance profiles were reported by our laboratory following EUCAST Guidelines [
12]. Samples were collected from the following materials: bronchoaspiration/broncholavage fluid, blood culture and central line-blood culture, urine and others (peritoneal fluid, surgical sites, etc). Microorganisms were included regardless of their nature, either infection or colonization. For any microorganism information regarding date and site of isolation, and presence or absence of antimicrobial resistance was collected.
Data were anonymously collected for all patients admitted in ICU from January 1st 2018 to December 31th 2022. Multiple isolations of the same pathogen with same resistance pattern and same site within 14 days were considered as a single sample for each patient.
3.1. Statistical Analysis
Data was collected in an excel database. A descriptive analysis was first performed. The Chi-squared test was used to assess independence between variables. A p-value of less than 0.05 was considered statistically significant. All statistical analyses were performed using Stata/SE 14.2 software (StataCorp LP, College Station, TX, USA).
3. Results
During the study period (2018-2022), a total of 1,771 microorganisms were detected in ICU, of which 221 (12.48%) had some resistant pattern (resistant organisms; ROs). In the same period 1,679 patients spent at least one day in ICU, with a total of 12,029 ICU hospitalization days. The above-mentioned microorganisms were isolated from 791 patients and were included in the study. Some patients had both ROs and non-ROs during the same stay. Their mean age was 67.97±14.33 ys (median 71) and they were mainly males (475; 60.05%) (
Table 1).
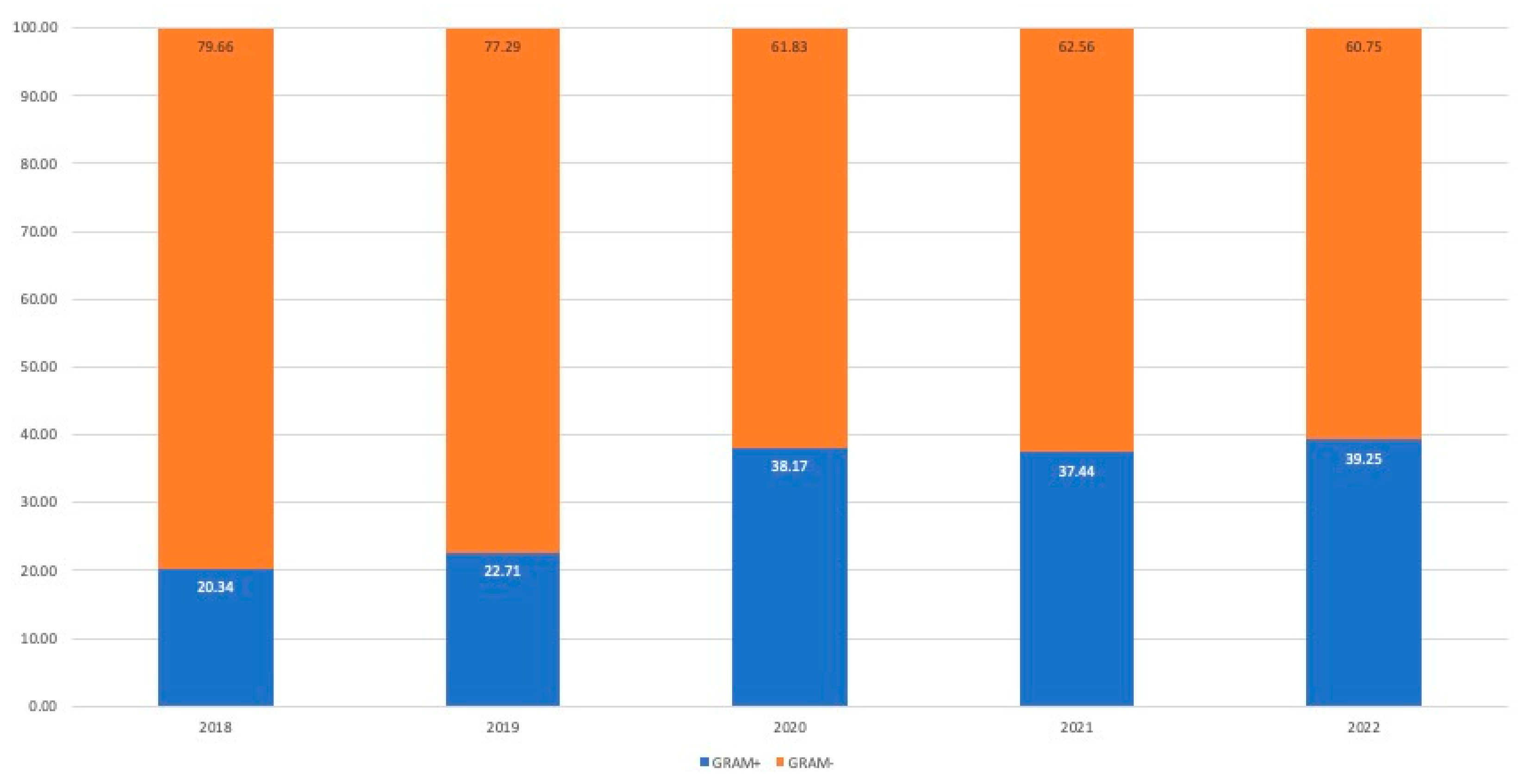
Most isolated microorganisms were Gram-negatives (67.96%), of them Enterobacteriaceae represented more than two thirds (66.21%) and non-fermenting ones were 27.93%. The most frequently detected Gram-positive microorganisms were Coagulase–negative Staphylococci (CONs) (42.20%), Enterococci (22.54%),
Staphylococcus aureus (16.47%), Streptococci (14.16%). During study years a progressive increase in the proportion of Gram-positives occurred, with a statistically significant rise between 2019 and 2020 (p<0.001) [
Figure 1].
Microorganisms were isolated from different biological materials; their proportion per cultured material is reported in
Table 2.
Regarding ROs, their absolute number increased from 35 in 2018 to 62 in 2020, and later swayed between 45 and 49. Their prevalence was between 8.02% and 14.76% of all isolated microorganisms (
Table 3).
Incidence of ROs and not-ROs changed over the study period, but this change was not statistically significant (
Table 4).
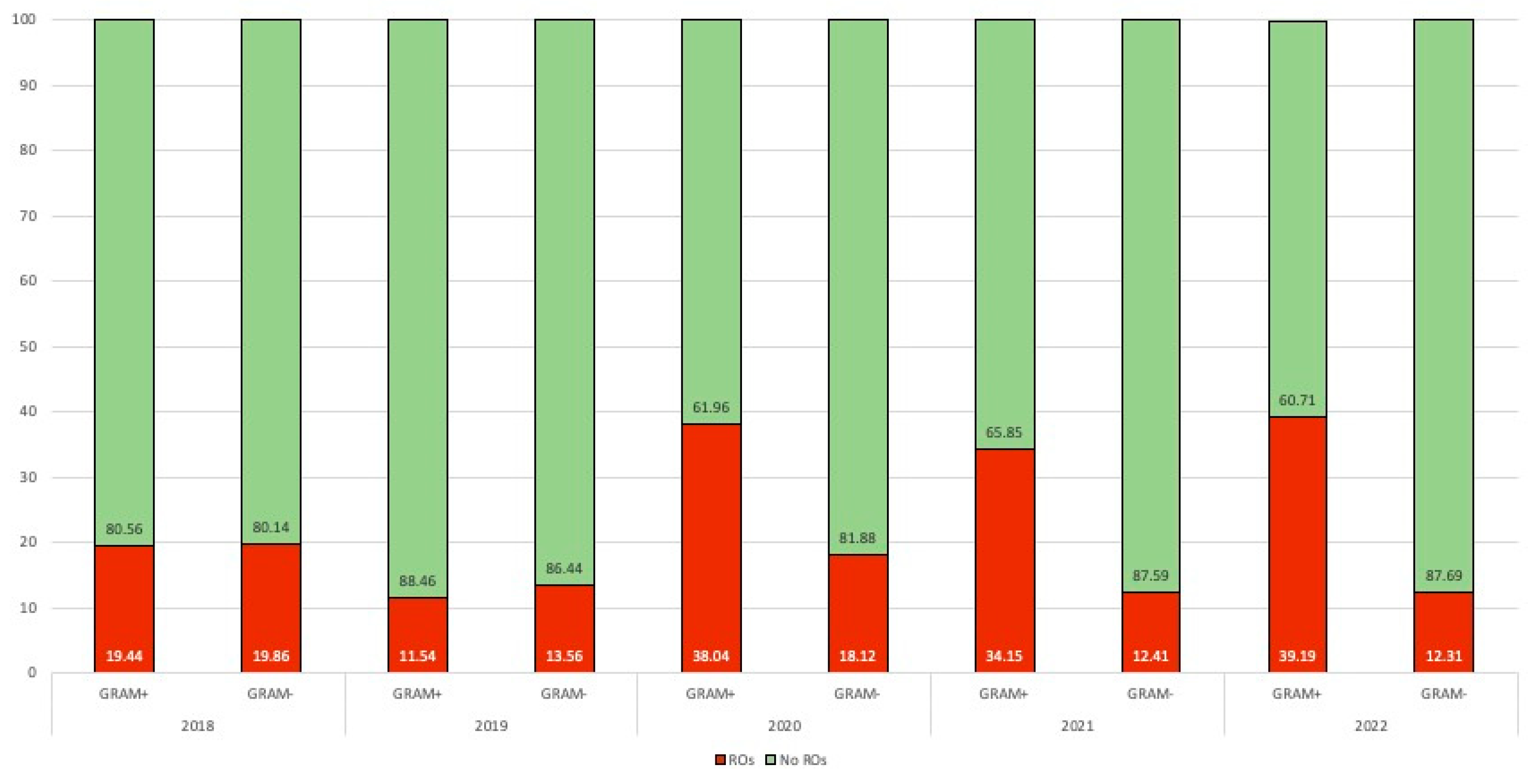
Proportion of ROs raised from 2020 especially for Gram-positives. Differently, Gram-negatives increased from 13.56% up to 18.12% in 2020, while a new slow lowering trend up to pre-pandemic levels was observed in 2021-2022 [
Figure 2].
The most frequently observed drug resistance patterns among ROs during the study period were Oxacillin 44.80%, Carbapenems 33.93% and Extended spectrum Beta-lactamase (ESBL) 16.29%.
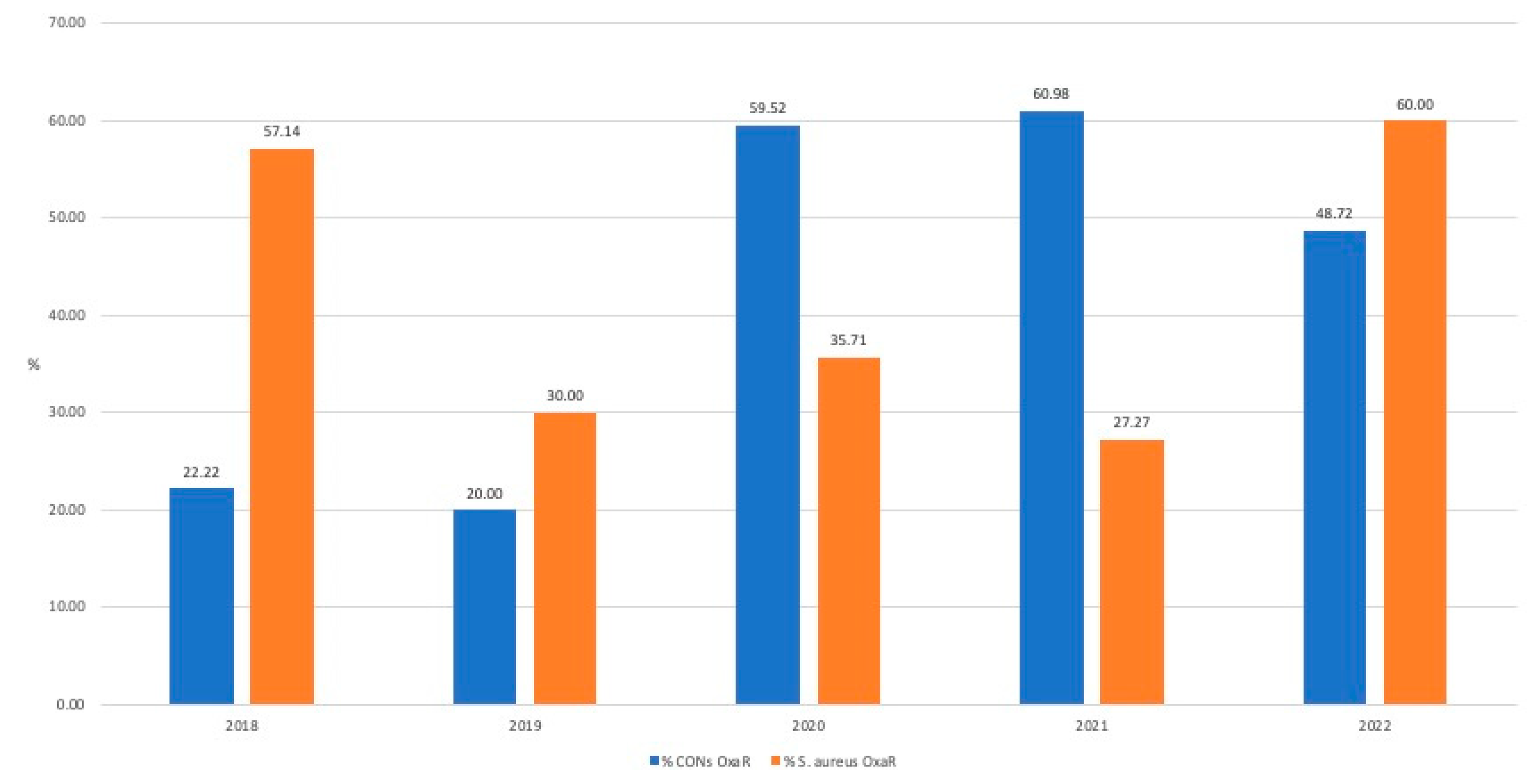
2.1. Oxacillin Resistance (Figure 3)
2.1.1. S. aureus
Few strains of S. aureus were detected during study years and, among them, prevalence of oxacillin resistance fluctuated from an initial 57.14% (4/7) in 2018, down to 30% (3/10) in 2019, then stable in 2020 (35.71%; 5/14) and in 2021 (27.7%; 3/11) and going up to 60% (9/15) in 2022.
2.1.2. Coagulase–negative Staphylococci (CONs)
Prevalence of oxacillin resistance among CONs was initially low at 22.22% (2/9) in 2018 and 20% in (3/15) in 2019. In 2020 there was a rise in the proportion of resistant strains which remained relatively stable in the following two years (2020: 59.52% (25/42); 2021: 60.98% (25/41); 2022: 48.72 % (19/39)).
A temporal correlation between increase in oxacillin resistance among CONs and SARS-CoV-2 pandemic was observed, with a statistically significant raise in 2020 (p<0.01) with a further increase in 2021 and a decrease in 2022.
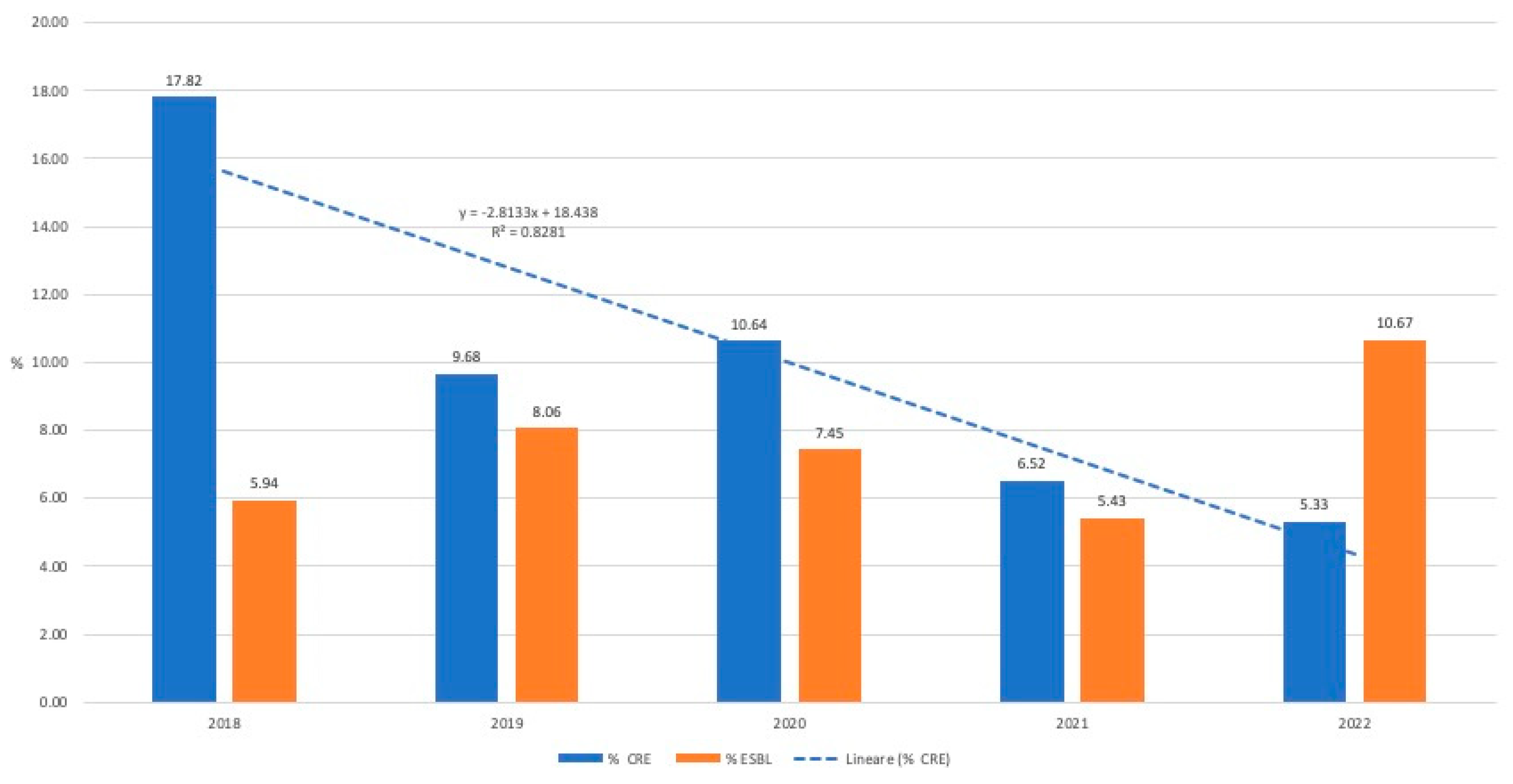
2.2. Carbapenem resistance (CR)
2.2.1. Enterobacteriaceae (Figure 4)
Proportion of carbapenem-resistant Enterobacteriaceae (CRE) dropped from 17.82% in 2019 to 5.33% in 2022, showing a not-significant lowering trend (R2=0.82) over the years.
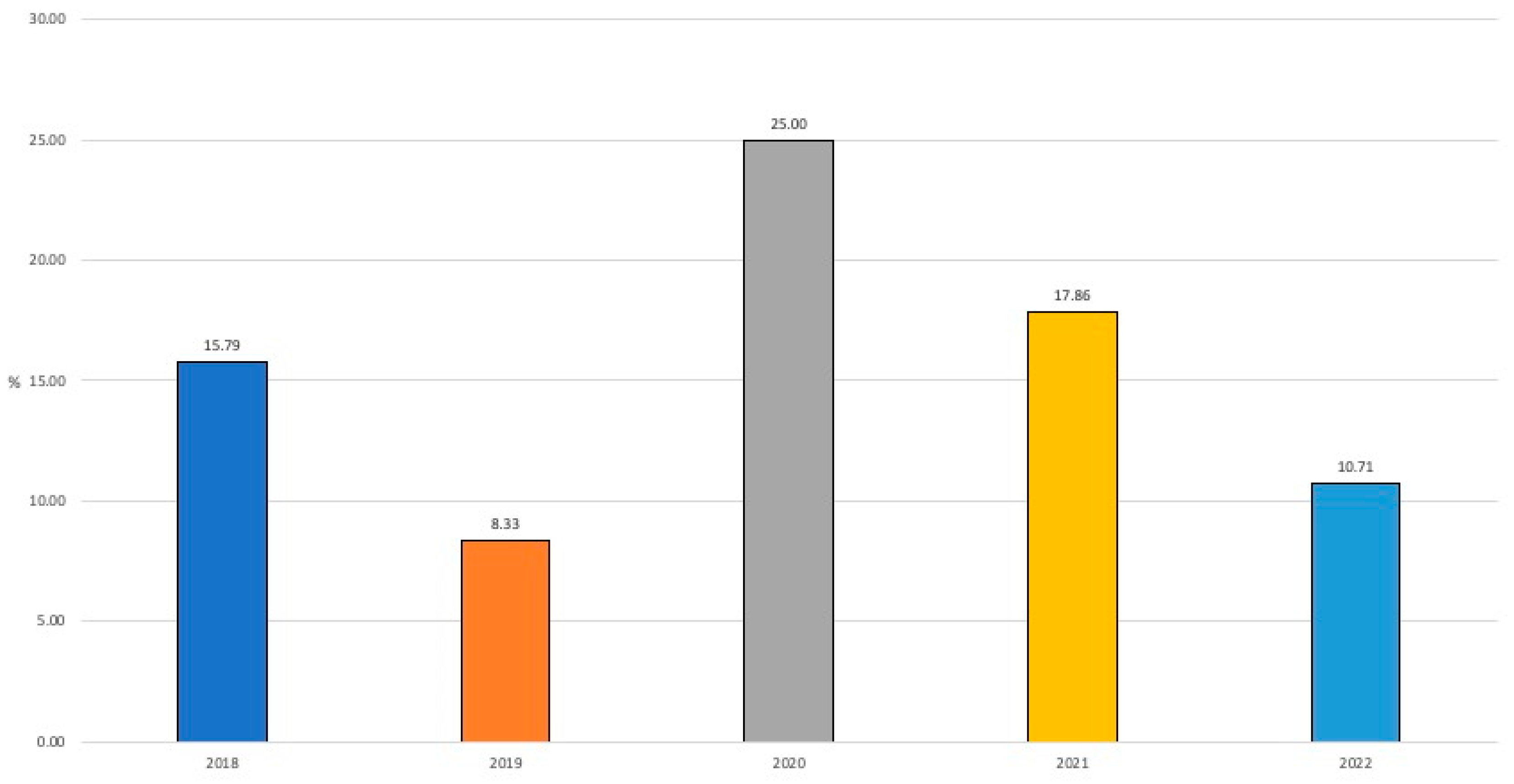
2.2.2. Non-fermenting Gram-negatives (Figure 5)
In this group, P. aeruginosa was the most frequently identified microorganism with carbapenem-resistance (20 strains in 5 years vs. 4 A. baumannii). Proportion of resistant strains went up and down during the study years: there was a drop in 2019 (8.33%) from the previous year (15.79%), then a non-statistically significant increase was observed in 2021 (25% of resistant isolates) followed by a new decrease to 10.71% in 2022.
2.2.3. K. pneumoniae
Trend in carbapenem-resistance of K. pneumoniae prevalence was the following: 15/29 (51.72%) in 2018, 5/19 (26.32%) in 2019, 7/20 (35%) in 2020, 0/9 (0%) in 2021, 2/13 (15.38%) in 2022.
2.3. ESBL
2.3.1. Enterobacteriaceae (Figure 4)
Resistant isolates in this group were rare and relatively stable over the study years: 6/101 (5.94%) in 2018; 10/124 (8.06%) in 2019; 7/94 (7.45%) in 2020; 5/92 (5.43%) in 2021 and 8/75 (10.67%) in 2022 (
Figure 3).
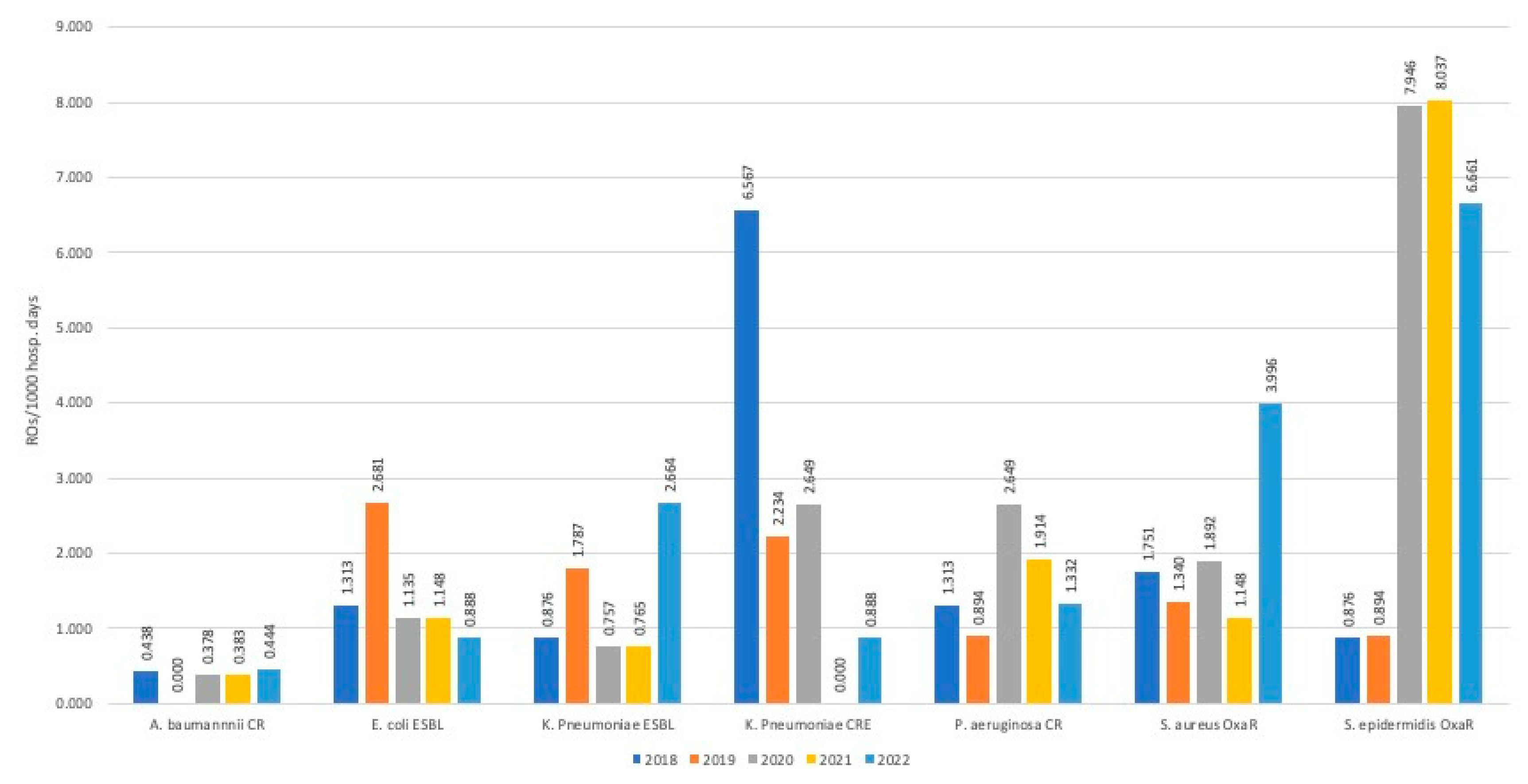
2.4. Incidence rates (Figure 6)
During study years, there was a decrease in detection of E. coli ESBL strains, which went from 2.681/1000 days of hospitalization in ICU in 2019 to 0.888/1000 ICU Days. A similar trend was observed for CR P. aeruginosa which, after an initial rise in 2019-2020 (2.649/1000 ICU days), fell to 1.332/1000 ICU days in 2022. However, both trends were not statistically significant.
Differently, for K. pneumoniae ESBL, in 2022 there was an incidence increase up to 2.664/1000 ICU days after years of stable incidence.
The highest incidence values were observed for OXA-R S. epidermidis which in 2020 was 7.946/1000 ICU days, in 2021 8.037/1000 ICU days and 6.661/1000 ICU days in 2022.
4. Discussion
The SARS-CoV-2 pandemic had a significant impact on our hospital (as in others) in terms of organization, change in infection control measures (greatest attention to respiratory transmission), type of patients in ICU (less surgical patients, more respiratory ones), but with proportions and categories of patients continuously changing in the various phases of the pandemic. This can be expected to have had an impact on the circulation of microorganisms (resistant or not), too.
In a 2022 systematic review Abubakar et al. reported that in more than 50% of the examined papers an increase in the prevalence/incidence of MRSA infections/colonizations occurred during the COVID-19 pandemic and that such increase ranged from 4.6% to 200.0% [
13]. Another retrospective analysis by Segala et al. evaluated bloodstream infections incidence in 2018-2021, i.e., in pre- and pandemic periods. They confirmed a higher risk of BSI occurrence among SARS-CoV-2 positive patients with a more pronounced risk in ICU.
S. aureus was the second pathogen in frequency and with a MRSA prevalence of more than 40% [
14]. A first consideration concerning our MRSA and MR-CONs is that, probably, this trend is related to overcrowding in ICU, massive staff turnover during this period, including not previously properly trained health care workers, with consequent insufficient hand hygiene and adherence to CVC-management bundles in first SARS-CoV-2 waves. MRSA isolates were in large majority obtained from BRA in 2018 and 2022, and from blood cultures in 2019 and 2022, differently in 2020-2021 they were all from CVC-blood cultures. Due to the increase in CVC-related infections in our ICU on the job training on CVC-management bundles and its strict monitoring were implemented since the end of 2021. This could probably partially explain the initial lowering trend observed in 2022. Unfortunately, sample size was too small for further analysis and no significant trend was identified.
Regarding Gram-negative ROs there published reports show a variable epidemiology with different emerging pathogens in different settings [
8,
9,
10,
11]. In one retrospective study, the colonization by CRE increased from 6.7% to 50 % from 2019 to 2020 [
15]. Another Italian experience of Temperoni et al. [
16] detected a high prevalence of
A. baumannii carbapenem resistant (CRAB) colonization with an infection rate of 75% (12/16). As expected, 100% of isolates of P. aeruginosa in that paper were MDR, including four carbapenem-resistant (CR) strains. Similarly, 50% of
K. pneumoniae isolates were MDR, while only 31% of isolates of
E. coli resulted in MDR. The most striking difference with our findings is the low level of resistant
A. baumannii strains in our cohort [
8,
11]. In our study isolation of ESBL pathogens was stable. A possible explanation can be found in patient features at the admission in ICU during pandemics years (younger, less comorbid, less classic risk factors for ESBL carriage at hospital admission). Our data, differently from many other studies, show that CRE isolation dropped in the study period meaning that probably, active antimicrobial stewardship initiatives and isolation bundles kept ongoing.
5. Conclusions
Although our study has some significant limitations (monocentric, small-size, observational, retrospective) a few findings merit careful consideration. Some important ROs in ICU after a first rise in incidence rates during early COVID pandemic years (2020-2021) showed a decreasing trend in 2021-2022. Observed rates reached even lower levels than pre-pandemic period (2018-2019) for
ESBL E. coli, CR
K. pneumoniae, CR
P. aeruginosa. This would suggest that the changed patient characteristics at ICU admission (younger age, less comorbidity, less surgical patients, less risk factors for ROs carriage) since the beginning of the SARS COV-2 pandemic may have impacted the observed resistance patterns. Different trends were observed for strains like Gram-negative ESBL, MRSA that after an initial lowering trends [
3,
7,
13] had a raise in 2020-2021 and 2022 possibly related to reduced infection control activities, reduced adherence to blood culture and central line-bundles and to antibiotic overtreatment in COVID patients.
In our setting, as soon as COVID pressure on ICU wards decreased, more antimicrobial stewardship activities were again in place: regular and more frequent infectious diseases (ID) specialist consultations, more frequent de-escalation and shortening of antibiotic treatment; renewed higher effort in infection control implementation strategy. The combination of these efforts was probably the main driver towards incidence reduction for most ROs in our ICU setting. This is particularly striking regarding the very low occurrence of CR-A. baumannii.
Further larger and more detailed investigations are indeed needed to better assess the real impact of SARS-CoV-2 pandemic in ROs incidence and consequently infections and related mortality in ICU.
Author Contributions
Conceptualization, Andrea Parisini; Formal analysis, Andrea Parisini, Filippo Del Puente, Marina Sartini and Emanuele Pontali; Investigation, Andrea Parisini, Silvia Boni, Elisabetta Blasi Vacca, Nicoletta Bobbio, Filippo Del Puente, Marcello Feasi, Roberta Prinapori, Maria Luisa Cristina, David Usiglio and Emanuele Pontali; Methodology, Andrea Parisini, Silvia Boni, Marina Sartini and Emanuele Pontali; Resources, Marco Lattuada; Supervision, Emanuele Pontali; Writing – original draft, Andrea Parisini, Marina Sartini and Emanuele Pontali; Writing – review & editing, Andrea Parisini, Silvia Boni, Elisabetta Blasi Vacca, Nicoletta Bobbio, Filippo Del Puente, Marcello Feasi, Roberta Prinapori, Marco Lattuada, Marina Sartini, Maria Luisa Cristina, David Usiglio and Emanuele Pontali. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to internal regulations.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sartini, M., Del Puente, F., Oliva, M., Carbone, A., Blasi Vacca, E., Parisini, A., Boni, S., Bobbio, N., Feasi, M., Battistella, A., Pontali, E., & Cristina, M. L. (2021). Riding the COVID Waves: Clinical Trends, Outcomes, and Remaining Pitfalls of the SARS-CoV-2 Pandemic: An Analysis of Two High-Incidence Periods at a Hospital in Northern Italy. Journal of clinical medicine, 10(22), 5239. [CrossRef]
- Giacobbe, D. R., Battaglini, D., Ball, L., Brunetti, I., Bruzzone, B., Codda, G., Crea, F., De Maria, A., Dentone, C., Di Biagio, A., Icardi, G., Magnasco, L., Marchese, A., Mikulska, M., Orsi, A., Patroniti, N., Robba, C., Signori, A., Taramasso, L., Vena, A., Bassetti, M. (2020). Bloodstream infections in critically ill patients with COVID-19. European journal of clinical investigation, 50(10), e13319. [CrossRef]
- Bentivegna, E., Luciani, M., Arcari, L., Santino, I., Simmaco, M., & Martelletti, P. (2021). Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. International journal of environmental research and public health, 18(3), 1003. [CrossRef]
- Grasselli, G., Scaravilli, V., Mangioni, D., Scudeller, L., Alagna, L., Bartoletti, M., Bellani, G., Biagioni, E., Bonfanti, P., Bottino, N., Coloretti, I., Cutuli, S. L., De Pascale, G., Ferlicca, D., Fior, G., Forastieri, A., Franzetti, M., Greco, M., Guzzardella, A., Linguadoca, S., … Bandera, A. (2021). Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest, 160(2), 454–465. [CrossRef]
- Cusumano, J. A., Dupper, A. C., Malik, Y., Gavioli, E. M., Banga, J., Berbel Caban, A., Nadkarni, D., Obla, A., Vasa, C. V., Mazo, D., & Altman, D. R. (2020). Staphylococcus aureus Bacteremia in Patients Infected With COVID-19: A Case Series. Open forum infectious diseases, 7(11), ofaa518. [CrossRef]
- Conway Morris, A., Kohler, K., De Corte, T., Ercole, A., De Grooth, H. J., Elbers, P. W. G., Povoa, P., Morais, R., Koulenti, D., Jog, S., Nielsen, N., Jubb, A., Cecconi, M., De Waele, J., & ESICM UNITE COVID investigators (2022). Co-infection and ICU-acquired infection in COIVD-19 ICU patients: a secondary analysis of the UNITE-COVID data set. Critical care (London, England), 26(1), 236. [CrossRef]
- Langford, B. J., So, M., Leung, V., Raybardhan, S., Lo, J., Kan, T., Leung, F., Westwood, D., Daneman, N., MacFadden, D. R., & Soucy, J. R. (2022). Predictors and microbiology of respiratory and bloodstream bacterial infection in patients with COVID-19: living rapid review update and meta-regression. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 28(4), 491–501. [CrossRef]
- Montrucchio, G., Corcione, S., Lupia, T., Shbaklo, N., Olivieri, C., Poggioli, M., Pagni, A., Colombo, D., Roasio, A., Bosso, S., Racca, F., Bonato, V., Della Corte, F., Guido, S., Della Selva, A., Ravera, E., Barzaghi, N., Cerrano, M., Caironi, P., Berta, G., … De Rosa, F. G. (2022). The Burden of Carbapenem-Resistant Acinetobacter baumannii in ICU COVID-19 Patients: A Regional Experience. Journal of clinical medicine, 11(17), 5208. [CrossRef]
- Kinross, P., Gagliotti, C., Merk, H., Plachouras, D., Monnet, D. L., Högberg, L. D., EARS-Net Study Group, & EARS-Net Study Group participants (2022). Large increase in bloodstream infections with carbapenem-resistant Acinetobacter species during the first 2 years of the COVID-19 pandemic, EU/EEA, 2020 and 2021. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin, 27(46), 2200845. [CrossRef]
- Buetti, N., Tabah, A., Loiodice, A., Ruckly, S., Aslan, A. T., Montrucchio, G., Cortegiani, A., Saltoglu, N., Kayaaslan, B., Aksoy, F., Murat, A., Akdoğan, Ö., Saracoglu, K. T., Erdogan, C., Leone, M., Ferrer, R., Paiva, J. A., Hayashi, Y., Ramanan, M., Conway Morris, A., Eurobact 2 study group (2022). Different epidemiology of bloodstream infections in COVID-19 compared to non-COVID-19 critically ill patients: a descriptive analysis of the Eurobact II study. Critical care (London, England), 26(1), 319. [CrossRef]
- Petazzoni, G., Bellinzona, G., Merla, C., Corbella, M., Monzillo, V., Samuelsen, Ø., Corander, J., Sassera, D., Gaiarsa, S., & Cambieri, P. (2023). The COVID-19 Pandemic Sparked Off a Large-Scale Outbreak of Carbapenem-Resistant Acinetobacter baumannii from the Endemic Strains at an Italian Hospital. Microbiology spectrum, 11(2), e0450522. Advance online publication. [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 13.0, 2023. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf (accessed on 7 March 2023).
- Abubakar, U., Al-Anazi, M., Alanazi, Z., & Rodríguez-Baño, J. (2023). Impact of COVID-19 pandemic on multidrug resistant gram positive and gram negative pathogens: A systematic review. Journal of infection and public health, 16(3), 320–331. [CrossRef]
- Segala, F. V., Pafundi, P. C., Masciocchi, C., Fiori, B., Taddei, E., Antenucci, L., De Angelis, G., Guerriero, S., Pastorino, R., Damiani, A., Posteraro, B., Sanguinetti, M., De Pascale, G., Fantoni, M., & Murri, R. (2023). Incidence of bloodstream infections due to multidrug-resistant pathogens in ordinary wards and intensive care units before and during the COVID-19 pandemic: a real-life, retrospective observational study. Infection, 1–9. Advance online publication. [CrossRef]
- Perez, S., Innes, G. K., Walters, M. S., Mehr, J., Arias, J., Greeley, R., & Chew, D. (2020). Increase in Hospital-Acquired Carbapenem-Resistant Acinetobacter baumannii Infection and Colonization in an Acute Care Hospital During a Surge in COVID-19 Admissions - New Jersey, February-July 2020. MMWR. Morbidity and mortality weekly report, 69(48), 1827–1831. 20 July. [CrossRef]
- Temperoni, C., Caiazzo, L., & Barchiesi, F. (2021). High Prevalence of Antibiotic Resistance among Opportunistic Pathogens Isolated from Patients with COVID-19 under Mechanical Ventilation: Results of a Single-Center Study. Antibiotics (Basel, Switzerland), 10(9), 1080. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).