1. Introduction
In recent weeks, general surgeons have been closely monitoring a concerning trend in the medical field - an increase in the diagnosis of mucocele appendix cases [
1]. A mucocele appendix is a condition that occurs when the appendix becomes enlarged due to a buildup of mucus in the organ. While this condition is rare, it can be potentially life-threatening if left untreated [
1].
Mucocele appendix is a relatively uncommon condition, but it is one that we are seeing more frequently. We believe that the increase in cases may be due to the growing use of advanced imaging techniques, which allows us to diagnose the condition more accurately [
2].
Symptoms of a mucocele appendix can range from mild discomfort to severe pain in the abdomen. In some cases, patients may experience nausea, vomiting, diarrhea, and fever. If left untreated, patients may develop serious complications such as peritonitis, which is inflammation of the lining of the abdomen [
3].
While the exact cause of a mucocele appendix is not understood, general surgeons believe that it is related to inflammation or obstruction of the appendix. Treatment options for a mucocele appendix can vary, depending on the severity of the case [
4]. Surgery from simple appendectomy to right hemicolectomy may be necessary, or medication may be prescribed to manage symptoms [
5]. In this study, we reported a rare case with mucocele of the appendix in Golestan Hospital of Ahwaz.
2. Case Presentation
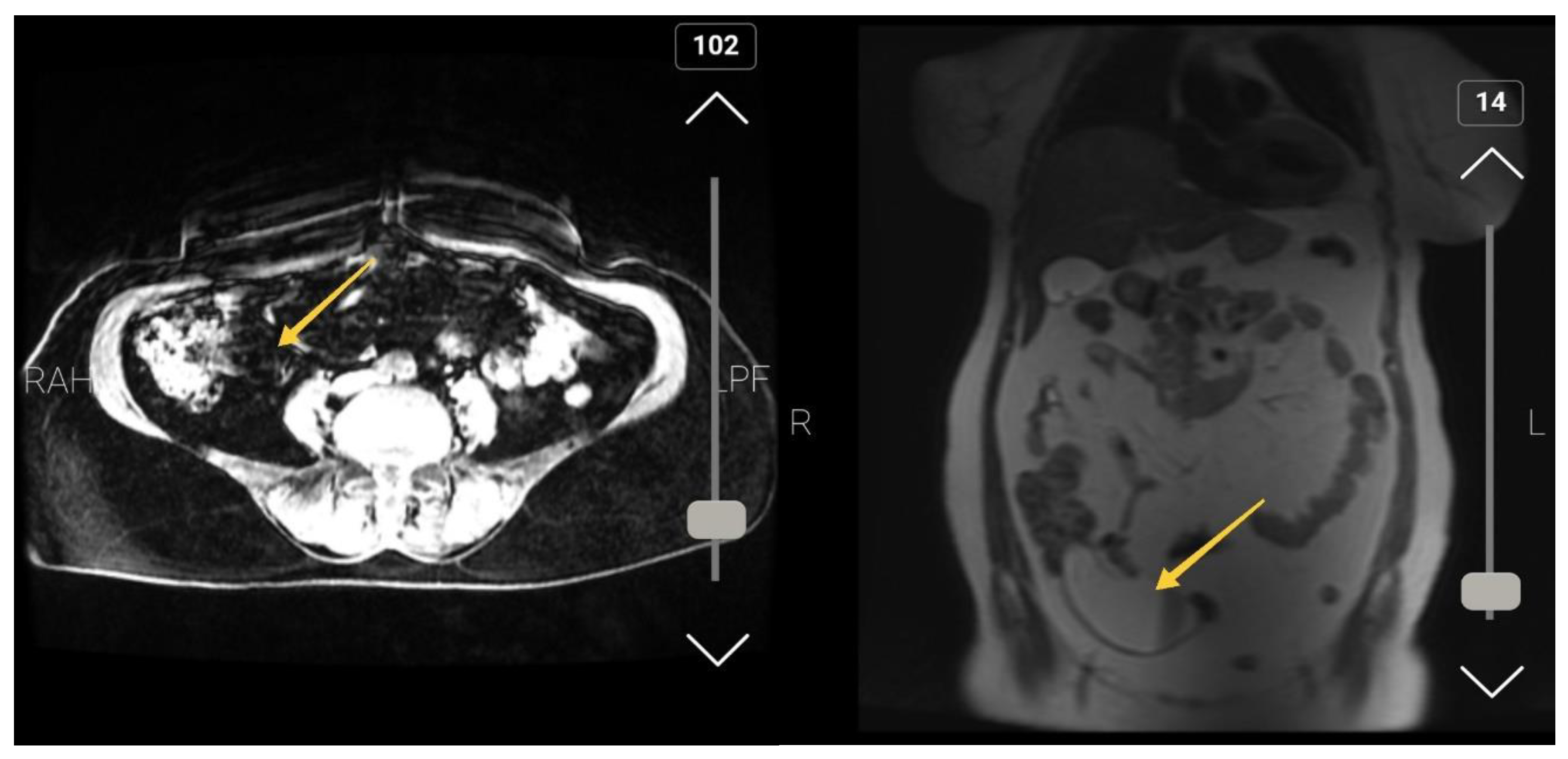
A 60-year-old female with a seven-month history of right lower quadrant pain aggravate in the last two weeks presented to the surgery emergency department of Golestan Hospital of Ahwaz. The patient mentioned weakness, fatigue, and decreased appetite from three month ago but didn't say any history of nausea, vomiting, or weight loss. She was afebrile at admission. The past medical history, past surgical history, family history, drug history and habitual history were negative. A physical exam showed tenderness and rebound tenderness in the RLQ (McBurney’s point), but Rovsing's sign was negative. other clinical examinations were normal. The patient’s WBC count was 13400 (Neutrophil=82 %), Hemoglobin= 12.3, and had normal urine analysis. In her medical records (Abdomen CT-Scan with and without IV contrast), fluid signal tubular mass measured 105 * 37 mm in RLQ is noted suggested for mucocele appendicitis (
Figure 1). After admission, she became NPO (Nothing by Mouth), and after antibiotic therapy (Ceftriaxone and metronidazole IV) and hydration (1/3, 2/3 1/3-2/3 intravenous fluid) and pack cell reservation she candidate for surgical management. Appendectomy was performed through McBurney incision and the base of the appendix was free, no lymphadenopathy was seen (
Figure 2).
There was no postoperative side effect. Two days later the patient was discharged and after fallow-up, the pathology was mucocele of the appendix with mucin-secreting mucosal hyperplasia.
3. Discussion
We were surprised to find this case in Golestan Hospital, which is the trauma center in the southwest of the country. The appendiceal mucocele describes a mucus-filled appendix that could be neoplastic or nonneoplastic pathologies (mucosal hyperplasia, simple cysts, mucinous cystadenomas, mucinous cystadenocarcinoma) [
6].
Appendiceal mucoceleis commonly seen after fifth decade that is similar to result of our studty.
The typical form is incidental; however, presentation with appendicitis signs and symptoms occurs in more than 30 % of cases [
7]. the case of our study had RLQ pain but it wasn't acute. From Alvardo criteria, our patient had RLQ tenderness (2 Score), Rebound tenderness (1 Score), Fever of more than 99.1 degrees of Fahrenheit (1 Score), and Leukocytosis >10,000 (1 Score).
On imaging findings for the neoplastic process, we expect round-encapsulated cystic mass with irregular walls and soft tissue thickening that is similar to our study that tubular mass measured 105 * 37 mm.
Careful imaging for the presence of ascites, peritoneal disease, and hepatic surface scalloping is important in the initial evaluation [
8].
All people over 50 years of age with right lower quadrant pain should undergo a CT scan of the abdomen (Like our patents). With colonoscopy, an orifice of the appendix can be elevated, and yellowish mucous secretions can be seen [
9].
In addition, synchronous and metachronous tumors can be identified. A reliable diagnosis based on the combination of imaging and surgical excision. in our study, the imaging finding was adapted to surgical findings. avoidance of mucocele rupture is important during surgery because the intraperitoneal spread of neoplastic cells and caused pseudomyxoma peritonei [
10].
The certain treatment of mucocele is surgery, if it has benign causes, a simple appendectomy (McBurney incision) is enough that is similar to our study, but for the treatment of adenocarcinoma cyst, a right hemicolectomy is recommended [
11].
Colorectal, ovarian, and endometrial cancers can coexist in the setting of appendiceal mucoceles, and careful examination of intra-abdominal structures. In our patient, the mucocele was not perforated (no secretion into the peritoneal cavity), there was no pathological process at the base of the appendix (negative resection margin), and regional lymph nodes were negative [12]. Therefore, only appendectomy was performed, which is sufficient surgery in such a case.
4. Conclusions
An appendiceal mucocele is a rarely. Appendiceal tumors have a low prevalence; But due to the nature of these tumors, which can also be malignant, they should be given importance and careful follow-up is mandatory. Correct diagnosis is necessary to prevent complications during and after the operation. As the Surgical community continues to learn more about this condition, it is essential that patients remain informed and proactive about this situation. With timely diagnosis and treatment, mucocele appendix can be successfully managed and treated.
Acknowledgments
We thank for patient for her consent to publish the case report. The authors would like to give a special thank you to the colleagues at Golestan Hospital, Joundishapour faculty of Medical Sciences, for his guidance and encouragement.
Conflicts of Interest
The authors declared no conflict of interest
References
- Singh, MP. A general overview of mucocele of appendix. Journal of Family Medicine and Primary Care. 2020, 9, 5867. [Google Scholar] [CrossRef] [PubMed]
- Vyas J, Badgurjar M, Saxena P, Parihar S, Thakor P. Prudent planning in management of mucocele of appendix. International Journal of Surgery Case Reports. 2021, 81, 105766. [Google Scholar] [CrossRef] [PubMed]
- Hassan Y, Wani IA, Farooq SI. Mucocele of appendix: A rare cause of surgical abdomen. Medical Journal of Babylon. 2022, 19, 89. [Google Scholar] [CrossRef]
- Knol ME, de Leede EM, van Beurden A. Torsion of a mucocele of the veriform appendix: report of a case. Journal of Surgical Case Reports. 2020, 2020, rjaa442. [Google Scholar] [CrossRef] [PubMed]
- Jelev G, Vassilev I, Usheva S, Yanev T, Sedloev T. А case of a mucocele of the appendix–A diagnostic and therapeutic dilemma. International Journal of Surgery Case Reports. 2023, 105, 108082. [Google Scholar] [CrossRef] [PubMed]
- Derbal S, Klapczynski C, Charissoux A, Durand Fontanier S, Taibi A. Management of mucocele of the appendix with peritoneal dissemination in pregnant women: a case report and literature review. Acta Chirurgica Belgica. 2021, 27, 1–7. [Google Scholar]
- Gayathre SP, Rajeswaran T. Mucocele of appendix unmasking appendiceal neoplasm. International Surgery Journal. 2023, 10, 766–9. [Google Scholar] [CrossRef]
- Aggarwal N, Bhargava A. Appendiceal mucocele secondary to torsion in an asymptomatic patient. Journal of Surgical Case Reports. 2019, 2019, rjz241. [Google Scholar] [CrossRef] [PubMed]
- Daspin D, Khalkho VM, Gnanaprakasam F, Krishnaswami M. Mucocele of Appendix-A Detailed Case Report. Journal of Evolution of Medical and Dental Sciences. 2019, 8, 3182–5. [Google Scholar] [CrossRef]
- Jelev G, Vassilev I, Usheva S, Yanev T, Sedloev T. А case of a mucocele of the appendix–A diagnostic and therapeutic dilemma. International Journal of Surgery Case Reports. 2023, 105, 108082. [Google Scholar] [CrossRef] [PubMed]
- Khan A, AlSubaie RS, Saleh AA, Khan IV A, AlSubaie R. Mucocele of the Appendix: A Case Report and Review of Literature. Cureus. 2023, 15. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).