2. Materials and Methods
2.1. Type of study
This was a prospective study of diagnostic accuracy, which compared the combination of pelvic MRI and 3D-EAUS versus pelvic MRI alone in the preoperative evaluation and postoperative outcomes of patients treated for perianal fistulas. Surgical examination under anesthesia was considered as the standard reference. The findings of the imaging methods were correlated with intraoperative findings in all patients. The local ethical committee of the Medical Department of Aristotle University approved the study protocol.
2.2. Sample size
A sample size of 72 patients was calculated to be sufficient to evaluate the two imaging methods, according to the findings of the meta-analysis of Muhammed R. S. Siddiqui et al. [
7] and the work of Stark and Zapf [
8] on sample size re-estimation, to avoid overfitting in diagnostic accuracy studies.
2.3. Patients
The patients of this study came from the anorectal outpatient clinic of the 3rd Surgical Department in “AHEPA” University Hospital, Thessaloniki, from April 2018 to April 2021. During this period, all candidates diagnosed after meticulous clinical examination with a fistula-in-ano were evaluated for eligibility to participate in the study protocol and 72 were chosen. All 72 patients provided written informed consent prior to their inclusion in the study.
2.4. Inclusion criteria:
Patients with primary or recurrent perianal fistulas caused by cryptoglandular infection.
2.5. Exclusion criteria:
Patients with perianal fistulas associated with:
1. Inflammatory bowel disease (IBD), especially Crohn’s disease
2. Posttraumatic etiology
3. Rectal or anal malignancy
4. Previous pelvic radiotherapy
5. Immunosuppression
6. Sexually transmitted anal disease.
2.6. Methods
The sample of 72 patients was divided into two imaging control groups. The first group included 36 patients to whom only pelvic MRI was done. The second group included 36 patients to whom both pelvic MRI and 3D-EAUS were performed. The findings of the MRI and the 3D-EAUS that were collected included:
anatomical classification of the perianal fistula (Park’s classification) [
9]
- 7.
>7. coexistence of an abscess cavity
- 8.
>8. presence of a secondary fistulous tract
- 9.
>9. clockwise location of the internal opening in the anal canal.
In some patients more than one synchronous perianal fistulas were detected and recorded separately. In cases of patients with a recent surgery for a perianal abscess, the imaging methods were performed one month after the abscess drainage and if they visualized a perianal fistula, the patient was enrolled in the study protocol.
Two weeks after the imaging methods were completed the patients were subjected to the appropriate surgical procedure for the existing perianal fistula. The same four mentioned characteristics of every fistula-in-ano found intraoperatively were also recorded. Some patients were admitted to the operating theater more than once to achieve definitive surgical treatment.
Each patient was re-examined with inspection of the perianal region and digital rectal examination at the anorectal outpatient clinic, six months after the surgical treatment was completed successfully. Two new parameters were evaluated and recorded:
complete healing of the fistula
- 10.
10. presence of fecal incontinence according to the Wexner continence scale (0-20 score) [
10].
All the collected data were finally analyzed with the proper statistical methods.
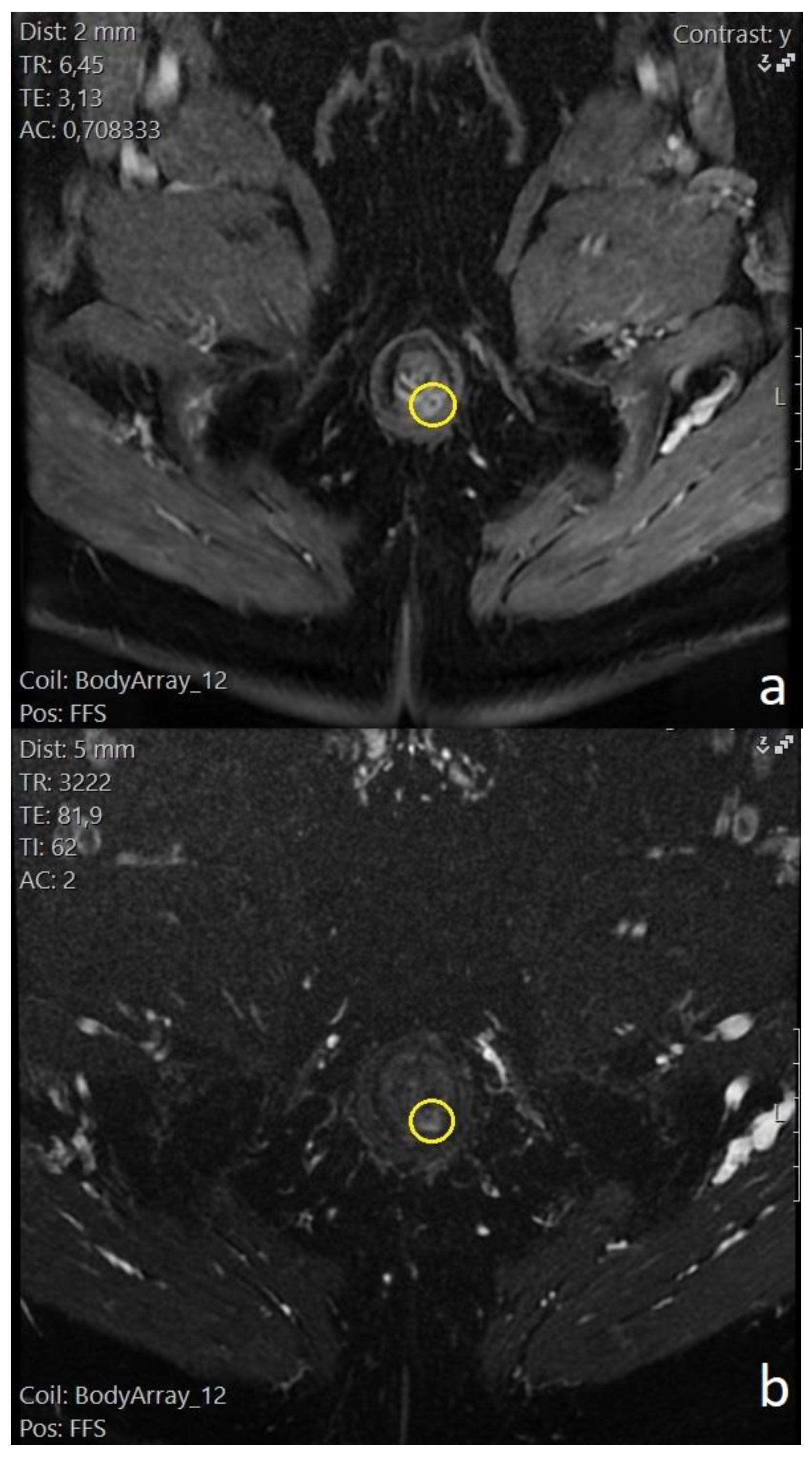
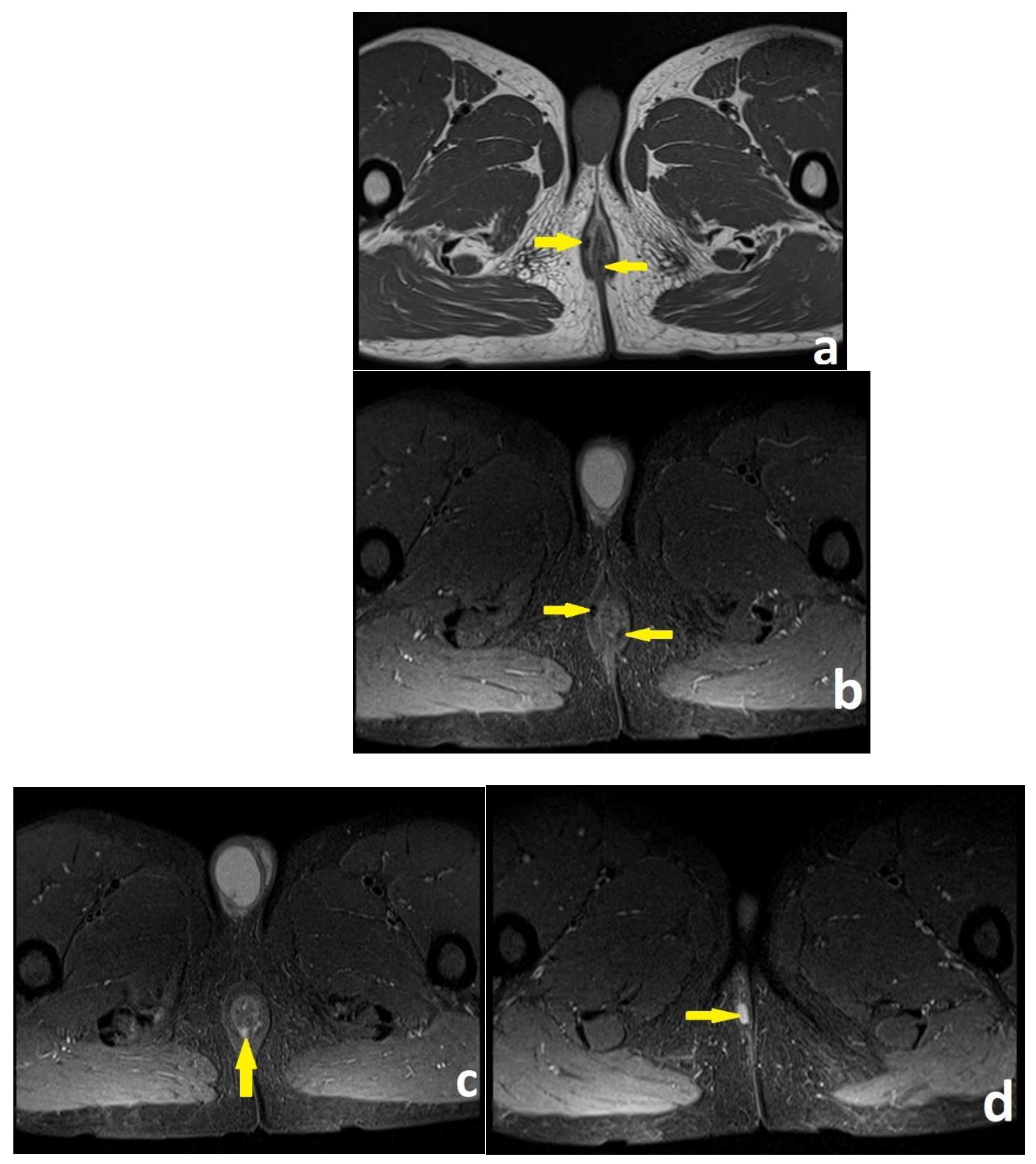
2.7. MRI
Pelvic MRI was performed on Siemens Avanto 1.5 Tesla magnet scanner. All patients were placed in supine position and external phased array body coils were used. Intravenous gadolinium was infused as a contrast media. No preparation or sedation was utilized.
The study protocol of the MR images acquired in coronal, axial, and sagittal orientation (T1-W FSE, T2-W FSE, STIR) is listed on
Supplementary Table S1.
The MR images were evaluated by one radiologist with 20 years of experience. Τhe anal sphincter muscles, levator plate and the ischiorectal fossa were evaluated with T1 sequence before and after gadolinium infusion. The lumen of the perianal fistulas and any secondary extensions or inflammatory liquid collections were visualized as hyper-intense tracts or cavities on T2 and STIR weighted images. On gadolinium-enhanced fat suppressed T1 weighted images, fistulous tracts’ wall and active granulation tissue demonstrated intense enhancement, while any fluid in the lumen was hypointense. Fibrotic scar tissue demonstrated low signal intensity on both T1 and T2 weighted images. We recorded the four mentioned characteristics in Methods chapter of all visualized perianal fistulas (
Figure 1 and
Figure 2).
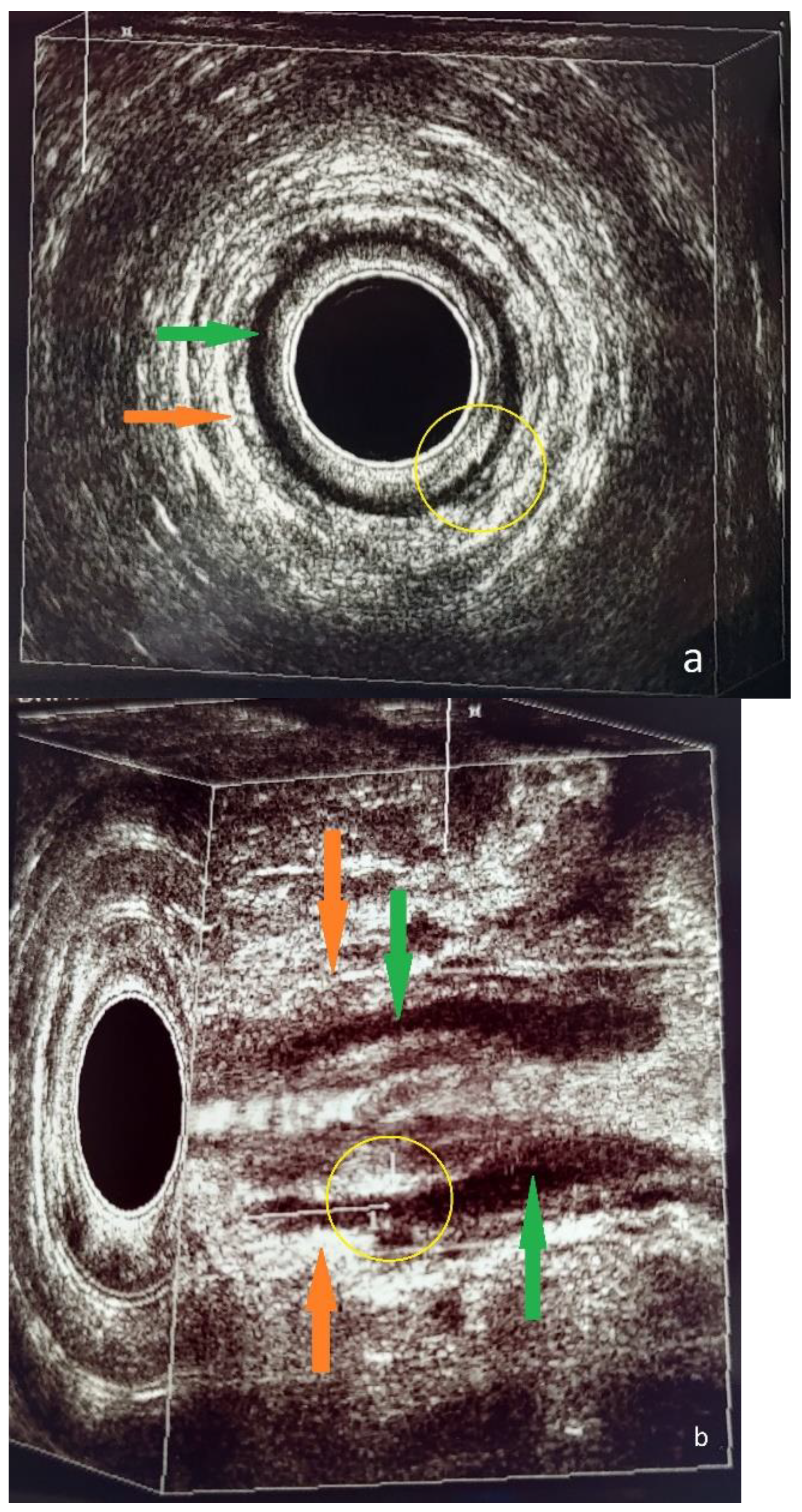
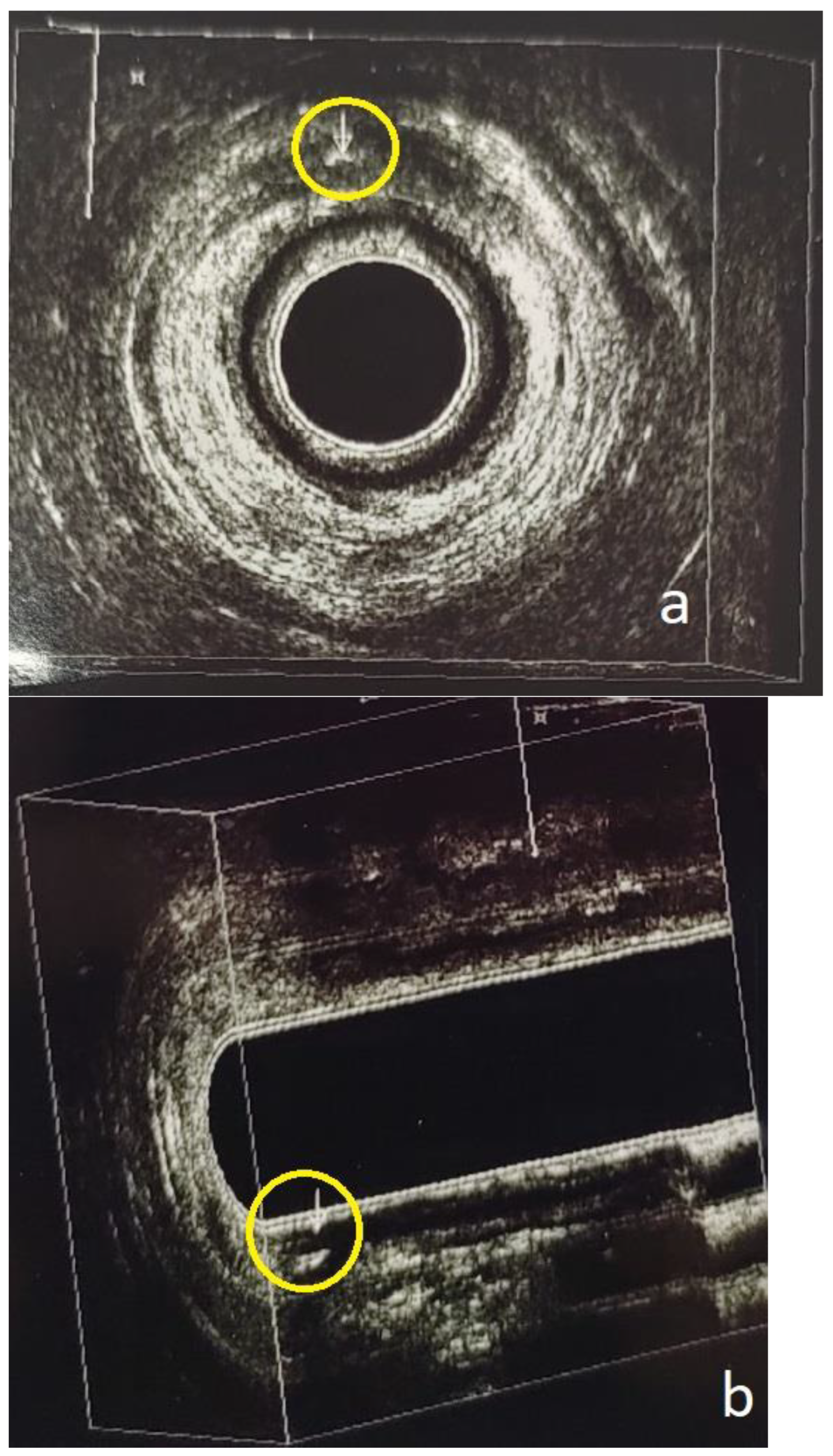
2.8.3. D-EAUS
Evaluation of all patients was performed using a Pro Focus 2202 (BK, Herlev, Denmark) endoanal ultrasound medical device, with a model 2052 anorectal transducer. The transducer was equipped with a 360° rotating head which could produce ultrasound waves with frequency range from 6 to 16 MHz and provide B-mode images. Three-dimensional reconstruction of transversal images in the coronal and sagittal planes was available with the use of specific software.
Bowel preparation was done with a fleet enema 30 minutes before the examination. The patients were placed in a left lateral position. The ultrasound probe was covered by a sterile condom, lubricated on both sides, and was gently inserted in the upper anal canal, until the U-shaped puborectalis muscle was visualized as a hyper-echoic band surrounding the posterior wall. The probe was then slowly retracted to visualize structures of the middle and lower anal canal. The internal anal sphincter (IAS) was recognized as a hypo-echoic ring in the upper and middle level. The external anal sphincter (EAS) was shown as a hyper-echoic structure in an outer level of the middle and lower anal canal.
The 3D-EAUS was performed by a colorectal surgeon with 10 years of experience in endoanal imaging, who was blinded to the results of the MRI. Hydrogen peroxide enhancement was not applied. A perianal fistula was recognized as a hypo-echoic tract that penetrated the anal sphincters or the perianal anatomical spaces and could branch into secondary extensions. The internal orifice of the fistula was shown as disruption of the IAS, according to Cho’s three criteria [
11]. A perianal abscess was visualized as a mixed hypo- and hyper-echoic region with debris and gas bubbles (
Figure 3 and
Figure 4).
2.9. Surgical procedure
Examination under anesthesia (EUA) was performed with patients in high lithotomy position and laryngeal mask airway (LMA). Bowel preparation was done with a fleet enema 30 minutes before surgery. A single dose of Metronidazole 500mg and Cefoxitin 2gr was administered intraoperatively. Surgical procedure was carried out by two colorectal surgeons with 20 and 10 years of experience respectively. The findings of the preoperative imaging (MRI alone or combination of MRI and 3D-EAUS) were studied and a surgical strategy was planned.
All external orifices of suspected perianal fistulas were examined with pliant fistula probes and infusion of H2O2. Characteristics that were examined and recorded for every fistula-in-ano found included Park’s anatomical classification, presence of a synchronous abscess cavity or a secondary-tract extension and clockwise location of the internal opening.
The perianal fistulas were categorized as intersphincteric, transsphincteric, supralevator and extrasphincteric according to Park’s classification. Other types of fistulas detected included submucosal, rectovaginal, and blind perineal. All perianal fistulas were also classified as simple and complex, according to Standard Practice Task Force (2005) and the latest American Society of Colorectal Surgeons (2022) guidelines [
2,
3,
4,
5].
Surgical procedures for the treatment of perianal fistulas included placement of a seton (vessel loop) drain, fistulotomy, Fistula Laser Closure (FiLaC), drainage of a synchronous abscess, unroofing of a secondary tract and combination of different methods.
2.10. Statistical analysis
Continuous variables were assessed for normality with the Shapiro-Wilk test and described accordingly with measures of central tendency and variation. Their differences between the two groups were assessed with a t-test or a Wilcoxon signed rank test, according to normality. Categorical variables were summarized with absolute and relative frequencies and their asymmetry between groups was assessed with chi-squared, Fisher’s test or z-test for proportions. The asymmetry between each group with the reference test was assessed with the McNemar-Bowker test of asymmetry. Diagnostic accuracy was assessed with the calculation of sensitivity, specificity, negative predictive value, positive predictive value, negative and positive likelihood ratio, and balanced accuracy. A confusion matrix with the strategy one-vs-rest was used to assess these measures for the primary outcome, since it was categorical variable with eight levels. To calculate the same measures for the second group, the combination of MRI and 3D EAUS, a Bayesian approach as described in [
12] and [
13] was utilized. It was considered that the two visualizations are connected in parallel and not serially, i.e., both are performed without a time difference that could alter the diagnosis and the performance of the second does not depend on the result of the first. Significance was held to 5% and power to 80%. All computations were run in R project for Statistical Computing, v. 4.2.1.
3. Results
A total of 72 patients with 88 fistulas were screened. Τhe first control group of pelvic MRI included 36 patients with 42 fistulas. The second control group of both pelvic MRI and 3D-EAUS included 36 patients with 46 fistulas. Six (6) patients in the MRI group and 10 in the MRI + 3D-EAUS group presented with synchronous fistulas.
The demographic characteristics recorded included sex, age, height, and weight, which were used to calculate body mass index (BMI). Male patients were 55 (76%), female patients were 17 (24%) and median age was 54 years (Interquartile Range 45-62) in the total sample. The gender ratio did not differ statistically significantly between the two groups (Pearson's Chi-squared test p-value = 0.8), nor did the age (Wilcoxon rank sum test p-value > 0.9). Similar results were yielded for height, weight, and BMI. However, it is noteworthy that the median BMI value for the entire sample was 28.6 (SD 25.6 – 32.0) (
Table 1).
Information about previous surgeries in the perianal region was collected. Primary perianal fistula was found in 17 (24%) of patients in the total sample (no statistically significant difference in proportions between groups, Pearson's Chi-squared test p-value = 0.8). History of a previous perianal abscess presented equal proportions (50%) in the MRI group, 69% ‘’Yes’’ and 31% ‘’No’’ in the MRI + 3D-EAUS group (Pearson's Chi-squared test p-value = 0.093). History of fistula recurrence did not show a statistically significant difference between the two groups (Pearson's Chi-squared test p-value = 0.4). Five patients (14%) in the MRI group and 8 patients (22%) in the MRI + 3D-EAUS group presented with recurrent perianal fistulas (
Table 1).
A statistically significant difference was observed in the ratio of simultaneous treatment for perianal abscess and fistula between the groups (Fisher's exact test p = 0.003). Twelve (12) patients (33%) in group MRI and 2 patients (5.6%) in group MRI+3D-EAUS underwent synchronous surgery for abscess and fistula. Classification of perianal fistulas into simple and complex type did not have a statistically significant difference between the two imaging control groups (Pearson's Chi-squared test p-value = 0.8). In group MRI, 19 patients (53%) presented with simple and 17 patients (47%) with complex perianal fistulas. In group MRI + 3D-EAUS, 20 patients (56%) were diagnosed with simple and 16 patients (44%) with complex fistulas (
Table 1).
Treatment of the disease with seton placement was the most common surgical procedure in the total sample of perianal fistulas (60.2%) and both imaging control groups (MRI: 54.8%, MRI + 3D-EAUS: 65.2%). Fistulotomy was the second most common procedure, with a total percentage of 27.3% (group MRI: 28.5%, group MRI + 3D-EAUS 26%). The two most regularly performed supplementary surgical procedures were perianal abscess drainage (total sample of perianal fistulas: 16%, group MRI: 28.5%, group MRI + 3D-EAUS 4.3%), and unroofing of a secondary fistulous tract (total sample of perianal fistulas: 14.8%, group MRI: 7.1%, group MRI + 3D-EAUS 21.7%).
Sixteen (16) patients in group MRI were treated with combined surgical procedures and 12 (33%) of them underwent seton placement along with perianal abscess drainage. In group MRI + 3D-EAUS, 10 patients (27.8%) were treated with both seton placement and unroofing of a secondary tract, out of 15 patients that underwent combined surgical procedures.
Overall, 49% of patients (group MRI 42%, group MRI + 3D-EAUS 56%) underwent a second surgical procedure for a definitive treatment of the disease (
Table 7). The most frequent repeat operation was seton suture change (group MRI 72.7%, group MRI + 3D-EAUS 86.7%).
3.1. Parks classification of fistulas
Assuming that the finding of a second fistula in the same patient is independent of the coexisting fistula, the frequencies of fistula types for the preoperative MRI-only group, combined imaging, and intraoperative classification are shown in
Table 2. The global symmetry test revealed no statistically significant difference between the groups, both initially and after correction for multiple comparisons. It was not possible to calculate sensitivity and specificity for supralevator fistulas in the MRI group, as there was no observation. There were few extrasphincteric, rectovaginal and perineal fistulas in each group.
The calculated diagnostic accuracy metrics are shown in . Notably, sensitivity improved in the MRI + 3D-EAUS group for transsphincteric fistulas and submucosal fistulas. Specificity improved considerably for intersphincteric and slightly for extraspincteric fistulas. Negative predictive value improved in most categories except for submucosal and rectovaginal fistulas. Balanced accuracy improved in all types of fistulas except for rectovaginal.
All values of balanced accuracy for each type of fistula were compared with z-test for proportions in both imaging control groups. Statistically significant (p < 0.05) difference was found in intersphincteric, submucosal, rectovaginal and No finding categories. The combination of imaging methods showed statistically significant higher balanced accuracy for Intersphincteric, Submucosal and No finding categories, whereas MRI alone showed statistically significant better results for Rectovaginal fistulas.
Table 3 SNMRI Sensitivity in the MRI-only group; SNadj Sensititivity in the combined MRI-3DEAUS group; SP MRI Specitifity in the MRI-only group; SPadj Specificity in the combined MRI-3DEAUS group; PPVMRI Positive predictive value in the MRI-only group; PPVadj Positive predictive value in the combined MRI-3DEAUS group; NPVMRI Negative predictive value in the MRI-only group; NPVadj Negative predictive value in the combined MRI-3DEAUS group; BAMRI Balanced accuratcy in the MRI-only group; BAadj Balanced accuratcy in the combined MRI-3DEAUS group;.
3.1.1. Transsphincteric fistulas
The diagnostic accuracy of the test combination improved in terms of sensitivity for the detection of transsphincteric fistulas, with a corresponding loss of specificity. The negative predictive value increased in the combined test, from 0.78 in the MRI group to 1.00 in the MRI + 3D-EAUS group, meaning that 100% of patients negative for transsphincteric fistula on either MRI, 3D-EAUS, or both, will indeed not suffer. The positive predictive value decreased from 0.89 to 0.71, meaning that 71% of patients with a positive MRI, or 3D-EAUS, or both, would have a transsphincteric fistula. The LR+ positive likelihood ratio, i.e., the probability of the presence of disease in patients with at least one test positive, was 2.67.
3.1.2. Intersphincteric fistulas
The diagnostic accuracy of the test combination improved in terms of specificity for the detection of intersphincteric fistulas, with a loss of sensitivity from 1.00 to 0.89. The negative predictive value remained the same on combined imaging, at the 1.00 level, so 100% of patients with negative either imaging method would not have an intersphincteric fistula. The positive predictive value remained the same, from 0.68 to 0.67, i.e., 67% of patients with at least one positive imaging method will have an intersphincteric fistula. The positive likelihood ratio LR+, i.e., the probability of disease presence in patients with a positive in at least one test was 13.3.
3.1.3. Supralevator fistulas
No supralevator fistulas were diagnosed in the MRI group. The imaging combination had a combined sensitivity of 1.00 and specificity of 1.00. The negative predictive value was 1.00 and the positive predictive value 1.00. Therefore, 100% of patients with at least one negative test will not have a supralevator fistula, while 100% of patients with at least one positive test will. This result should be interpreted with great caution, as the relevant table includes only 3 diagnosed fistulas and, furthermore, no positive examination was refuted intraoperatively. The negative likelihood ratio LR-, i.e., the probability of absence of disease in patients with a positive at least one test was 0.25.
3.1.4. Extrasphincteric fistulas
The sensitivity and specificity of extrasphincteric fistula diagnosis by MRI were 1.00 and 0.95 respectively. For the MRI + 3D EAUS group the specificity and sensitivity were 0.98 and 1.00. The negative predictive value increased to 1.00 in the combined imaging group, so 100% of patients with any negative imaging will not have an extrasphincteric fistula. The corresponding value was 0.98 for the MRI group. The positive predictive value increased from 0.33 to 0.50 in the combined imaging group.
3.1.5. Submucosal fistulas
The sensitivity of diagnosing submucosal fistulas improved in the imaging combination, from 0.40 to 0.63 while the specificity decreased from 1.00 to 0.92. The negative predictive value increased from 0.92 in the MRI group to 0.95 in the combined imaging group, meaning that for 95% of patients with even one negative test, a submucosal fistula will not be found. The positive predictive value decreased from 1.00 to 0.71, meaning that 71% of patients with at least one positive test will have a submucosal fistula. The positive likelihood ratio LR+, i.e., the probability of disease presence in patients with a positive in at least one test was 14.3.
3.1.6. Rectovaginal fistulas
Only one rectovaginal fistula was diagnosed in the MRI group, which had been visualized preoperatively with MRI. Only two rectovaginal fistulas were diagnosed in the MRI + 3D-EAUS group, of which only one was detected by 3D-EAUS and none by MRI (one was diagnosed as anterior transsphincteric). The calculated diagnostic accuracy values are not reliable for this type of fistula.
3.1.7. Perineal fistulas
Only one perineal fistula was diagnosed in the MRI group, which had been imaged preoperatively with MRI. Only two perineal fistulas were diagnosed in the MRI + 3D-EAUS group, both of which were detected by MRI and one by 3D EAUS. Estimated diagnostic accuracy values are not reliable for this type of fistula.
3.1.8. No findings
Preoperative absence of imaging findings had negative predictive value 0.92 in the MRI group and 0.97 in the MRI + 3D-EAUS group. Thirteen percent of patients with positive at least one imaging in the MRI + 3D-EAUS group would remain without findings at surgical exploration (positive predictive value 0.13). Pooled sensitivity was 0.67, compared to null in the MRI group, and specificity 0.72 versus 1.00.
3.2. Presence of a concomitant abscess cavity
Thirty-six (36) patients were screened in each imaging control group, with 42 fistulas found in the first group (MRI) and 46 in the second group (MRI+3D-EAUS).
The presence of a synchronous abscess cavity was checked in both imaging groups and it was shown that in the MRI group 16 patients had a concomitant abscess cavity and 25 did not, compared with intraoperative detection of 15 abscess cavities (
Table 4). Twelve (12) of these 15 patients had an acute abscess and underwent synchronous treatment for both the abscess and the perianal fistula (
Table 1). The remaining three patients had a residual abscess cavity after previous surgical drainage and were treated only for the perianal fistula.
In the MRI + 3D-EAUS group 6 patients had a concomitant abscess cavity on preoperative MRI imaging and 5 on preoperative 3D-EAUS. Eight (8) patients had a confirmed abscess cavity intraoperatively (
Table 4). Two (2) of these 8 patients had an acute perianal abscess (
Table 1) and the other 6 had a residual abscess cavity.
The specificity and sensitivity for the first group (MRI) were 0.96 and 1.00 respectively. Diagnostic accuracy was found to be 0.975 with 95% CI: 0.868, 0.999. The p-value (McNemar's test) was found to be almost 1. The negative predictive value was 1.00, meaning 100% of patients with a negative MRI did not have a synchronous abscess cavity, and the positive predictive value was found to be 0.94, meaning 94% of patients with a positive MRI did have a concomitant abscess cavity.
In the MRI + 3D-EAUS group the combined specificity was 1.00 and the combined sensitivity was 0.91. The negative predictive value was 0.97, i.e., 97% of patients with at least one negative test did not have an accompanying abscess cavity. The positive predictive value was 1.00, therefore 100% of patients with positive at least one imaging will be found to have an accompanying abscess cavity. The negative likelihood ratio was 0.125.
3.3. Presence of a secondary fistulous tract
The existence of a secondary fistulous tract in the MRI-only group was detected in 5 patients preoperatively and was confirmed in 3 cases intraoperatively. In the combined imaging group, 13 patients had a secondary fistulous tract identified on preoperative MRI, 7 on 3D-EAUS, and 10 had an intraoperative finding of a secondary tract.
The specificity and sensitivity for the first group (MRI) were 0.92 and 0.34 respectively. Diagnostic accuracy was found to be 0.875 with 95% CI: 0.732, 0.958. The p value (McNemar's test) was found to be almost 1. The negative predictive value was 0.94, meaning 94% of patients with a negative MRI did not have a secondary fistulous tract, and the positive predictive value was found to be 0.25, meaning 25% of patients with a positive MRI did have a secondary fistula.
In the MRI + 3D-EAUS group the combined specificity was 0.84 and the combined sensitivity was 0.91. The negative predictive value was 1.00, i.e., 100% of patients with at least one negative test did not have a secondary fistulous tract. The positive predictive value was 0.71, 71% of patients with positive at least one imaging will have a secondary fistula. The positive likelihood ratio was 7.14.
3.4. Inner orifice location
Data were recorded at each finding site clockwise to locate the internal orifice. As seen from
Table 6, most fistulas were detected at the middle-posterior wall of the anal canal (6th hour). For this reason, the remaining positions were collapsed into one category "Other location" and the absence of internal orifice remained in a separate category.
The specificity and sensitivity for locating the inner orifice at 6 hours were 0.97 and 1.00 in the MRI group, and the combined specificity and sensitivity in the MRI + 3D- EAUS group were 0.95 and 1.00, respectively. The negative predictive value of combined imaging increased to 1.00 (of single MRI localization was found to be 0.88). The positive predictive value was reduced to 95% versus 100% for imaging alone.
At the other sites, the sensitivity and specificity were 0.92 and 0.93 for the MRI-only group and 1.00 and 0.89 in the MRI + 3D-EAUS group. The negative predictive value for combined imaging increased to 100% from 96% in the MRI group, and the positive predictive value increased to 90% from 86%.
Absence of internal orifice was detected with a sensitivity of 1.00 and specificity of 0.97 in the MRI group and 1.00 and 0.81 in the MRI + 3D-EAUS group. The positive predictive value was 0.67 in the MRI group and 0.13 in the MRI + 3D-EAUS group, and the negative predictive value remained 100% in both groups.
3.5. Perianal fistula healing and fecal incontinence six months postoperatively
The relative frequencies for each of the secondary outcomes of interest are shown in
Table 7. Comparison of perianal fistulas’ healing rate was not possible, since healing was achieved in all patients at the 6-month follow-up, which was the prespecified outcome of interest. Follow-up was continued for six more months, and two fistula recurrences were detected, one in each imaging control group.
Regarding fecal incontinence, 3 patients in the MRI group and 2 in the MRI + 3D-EAUS group had mild incontinence according to the Wexner scale criteria, and the rest had no discomfort. The comparison with Fisher's exact test for the group-wise correlation matrix had a p-value > 0.9, i.e., it was not statistically significant (
Table 7).
Repeat surgery rate for definitive treatment didn’t show a statistically significant difference in proportions between the two imaging control groups (Pearson's Chi-squared test p-value = 0.2) (
Table 7).
The sample of 72 patients was also divided into a group with simple perianal fistulas (39 patients) and a group with complex perianal fistulas (33 patients). Healing rate at six months postoperatively was equal (100%) in patients of both these groups (
Table 8). Two patients were diagnosed with perianal fistula recurrence, one in the group with simple and one in the group with complex fistulas, at one year of follow-up. This was outside the prespecified period for our study.
Fecal incontinence according to the Wexner score didn’t present a statistically significant difference between the two groups (Fisher's exact test p-value > 0.9). Most patients (93% in total sample, 92% with simple fistula, 94% with complex fistula) had normal anal continence at the sixth postoperative month (
Table 8).
Patients with complex perianal fistulas had a 3.2 higher probability to undergo a repeat surgery for definitive treatment of the disease, compared to patients with simple fistulas (OR 3. 13, 95% CI 1.19 – 8.2, p-value 0.019) (
Table 8).
4. Discussion
The incidence of perianal fistulas in Europe ranges from 1.7 to 2.3 cases per 10,000 persons/year and the total prevalence in Europe is 1.69 per 10,000 population. Male to female ratio is approximately 2/1 and mean age of patients is 40 years [
2,
14,
15]. In our study, male to female ratio was approximately 3/1 and mean age was higher (54 years) for the total sample of patients (
Table 1). Obesity (BMI>25 kg/m²) is a recognized independent risk factor for perianal fistula formation [
2,
16]. This is in concordance with our study, where the median BMI value for the total sample was 28.6 kg/m² (
Table 1).
Pathogenesis of perianal fistulas is mainly associated with cryptoglandular infection, and Crohn’s disease is a second, rarer cause [
2,
17]. Most published articles that compare MRI with EAUS are heterogenous and include perianal fistulas with different pathogenesis [
2]. Maier et al included 22 patients with cryptoglandular disease and 17 patients with Crohn’s disease [
18]. Buchanan et al included 95 patients with cryptoglandular disease and 9 with Crohn’s disease [
19]. Brillantino et all included 124 patients in total. Fifteen (15) patients had a history of Crohn’s disease, 3 had a history of anorectal trauma and 1 had undergone surgery for rectal cancer [
1]. In our study we only included patients with perianal fistulas of cryptoglandular origin, which is the most common cause of the disease. Thus, our sample is homogenous, and the results of the study are more reliable and reproducible.
According to the theory of cryptoglandular infection, 40%-60% of patients treated for an acute perianal abscess will eventually develop a chronic fistula-in-ano. Previous anorectal surgery is a second independent risk factor for fistula formation and recurrence. [
2,
16,
17,
20]. The incidence of recurrence depends on the type of fistula and is highly variable, as it ranges between 7% to 50% [
21,
22]. Many published articles that compare MRI with EAUS enrolled patients with previous anorectal surgery and recurrent fistulas. Shwartz et al. included 18 (56%) patients out of 32 with at least 1 previous surgery for their perianal Crohn’s disease [
23]. Maier et al [
18] included 26 (66%) out of 39 patients and Buchanan et al [
19] enrolled 76 (73%) out of 104 patients with recurrent fistulas-in-ano. Sayeed et al included 20 (17%) out of 120 patients with previous anal operations [
24]. Maier et all detected no statistically significant correlation between the patient's history (Crohn's disease or recurrent fistula) and the diagnostic accuracy of MRI and EAUS [
18]. In our study, 43 (60%) out of 72 patients had a history of acute perianal abscess drainage and 13 (18%) out of 72 patients presented with recurrent perianal fistula (
Table 1). In total, only 15 (21%) of our total patients had a history of no previous anorectal surgery.
Other described risk factors for perianal fistula recurrence after surgical treatment include complex type of fistula-in-ano with high internal opening, multiple tracts or horseshoe extensions, failure to recognize the internal opening and inappropriate selection of the surgical procedure [
20,
21,
22]. Subsequently, the use of imaging methods with high diagnostic accuracy preoperatively is crucial for precise fistula anatomical classification and treatment, with the optimal surgical procedure [
2].
Pelvic MRI is considered the gold-standard method of imaging for perianal fistulas. It is related to statistically significant better results and prognosis after surgical treatment of fistulas-in-ano [
2]. It can offer more information than examination under anesthesia, alter the treatment strategy and reduce postoperative recurrent rates of the disease [
25,
26,
27,
28,
29,
30]. 3D-EAUS has a high diagnostic accuracy in detecting the internal opening of a fistula in-ano, plus intersphincteric and transsphincteric fistulas [
2,
7]. It can reliably facilitate the surgical planning, identify defects of the anal sphincters, and is associated with statistically significant better results in preserving anal continence postoperatively, especially in complex cases [
31,
32,
33].
Shwartz et al. compared the diagnostic accuracy of pelvic MRI, endoanal ultrasound and examination under anesthesia in 32 patients with Crohn’s disease. Thirty-nine (39) perianal fistulas and 13 abscesses were detected. The diagnostic accuracy when any 2 of the 3 mentioned tests were combined was 100% [
23]. Other published articles also suggested that if pelvic MRI and EAUS were combined preoperatively, this could improve their total diagnostic accuracy [
34,
35].
To the best of our knowledge, our article is the first study in literature which calculated measures of diagnostic accuracy for the combination of pelvic MRI and 3D-EAUS compared to pelvic MRI alone. According to our results, the combination of the two imaging methods presented adjusted sensitivity and adjusted negative predictive value 1.00 in all major categories of perianal fistulas (Transsphincteric, Intersphincteric, Supralevator, Extrasphincteric and blind Perineal). The adjusted sensitivity also improved for Submucosal fistulas (0.71 from 0.40) and for category No finding (0.67 from 0.00). The adjusted negative predictive value decreased from 1.00 to 0.95 for Submucosal and increased from 0.92 to 0.97 for category No finding (
Table 3).
The adjusted specificity improved for Intersphincteric (0.93 from 0.66) and Extrasphincteric (0.98 from 0.95) fistulas and was 1.00 for Supralevator, Rectovaginal and blind Perineal fistulas. The adjusted specificity decreased for Transsphincteric (0.63 from 0.96) and Submucosal (0.95 from 1.00) fistulas and for category No finding (0.70 from 1.00). The adjusted positive predictive value increased for Intersphincteric (0.67 from 0.33), Extrasphincteric (0.50 from 0.33) and Rectovaginal (1.00 from 0.68) fistulas and was 1.00 for Supralevator and blind Perineal fistulas. The adjusted positive predictive value decreased for Transsphincteric (0.71 from 0.89), Submucosal (0.71 from 1.00) fistulas and category No finding (0.13 from 1.00) (
Table 3).
The only meta-analysis in literature which compared the diagnostic accuracy of pelvic MRI versus EAUS in the preoperative imaging of perianal fistulas, showed equal combined sensitivity for both methods, with a value of 0.87 and comparable range. Pelvic MRI presented a combined specificity rate of 0.69 and EAUS a lower rate of 0.43 [
7]. This meta-analysis included only four articles for quantitative synthesis with a high degree of heterogeneity for reporting sensitivity and other measures of diagnostic accuracy [
18,
19,
36,
37]. In more recently published articles, the results were also contradictory. Brillantino et al reported equal value of sensitivity for MRI and peroxide enhanced 3D-EAUS (98.4%), and equal value of specificity for both imaging methods (83.3%) [
1]. Akhoundi et al, calculated the following measures of diagnostic accuracy; MRI sensitivity=76.12%, EAUS sensitivity= 87.38%, MRI specificity= 57.69%, EAUS specificity=38.46%, MRI PPV=93.88%, EAUS PPV=92.38%, MRI NPV=22.05%, EAUS NPV=26.31%, MRI accuracy=74.19%, EAUS accuracy=82.25% [
38]. In comparison to most of the previous articles, our study presented highly improved measures of diagnostic accuracy regarding the combination of pelvic MRI and 3D-EAUS.
According to the literature, pelvic MRI has a tendency for improved detection of a secondary fistulous tract and a concomitant abscess cavity. Endoanal ultrasound has a tendency for more accurate detection of the internal opening and relationship with the anal sphincters, due to their proximity to the probe [
2,
4,
7]. Buchanan et al found a statistically significant higher accuracy of MRI in detecting primary tracts (p<0.001), horseshoe extensions (p=0.003), abscess cavities (p<0.001) and internal openings (p<0.001) in comparison with EAUS and clinical examination. Nevertheless, they considered EAUS reliable for the identification of the inner orifice of a perianal fistula [
19]. Brillantino et al reported overall sensitivity of MRI and 3D-EAUS 94.4 and 80.6 respectively, in the detection of secondary extensions for simple and complex fistulas. The overall specificity of MRI and 3D-EAUS was 98.9 and 97.8 respectively in the same category. However, MRI was superior to 3D-EAUS for the detection of secondary extensions in complex perianal fistulas (p=0.041 McNemar's test). The overall sensitivity of MRI and 3D-EAUS in the identification of the internal opening was 95.8% and 97.5% respectively. The overall specificity had an equal value of 83.3% for MRI and 3D-EAUS in the same category [
1]. Sayed et al also concluded that MRI was superior to 3D-EAUS for the evaluation of secondary tracts (K-value=0.65, P<0.001). Ultrasound was found superior to MRI in the localization of the internal opening (K- value=0.44, P <0.001) [
24]. Gustafson et al was the only study which presented better results for EAUS with probing than pelvic MRI regarding secondary characteristics of perianal fistulas [
36]. In our study, the combination of pelvic MRI and 3D-EAUS showed improved sensitivity, negative and positive predictive value only in the detection of a secondary extension, whereas metrics for a synchronous abscess and the internal opening were almost equal between the two imaging control groups.
Surgical treatment of a perianal fistula is considered successful, if all fistula tracts, extensions, and purulent cavities are eliminated, and complete healing of the wound is achieved within six months after the final surgical procedure. If the healing process of a perianal fistula’s wound is not completed within six months and an external opening with fluid discharge remains, the perianal fistula is defined as persistent. Recurrence of a perianal fistula occurs within one year after definitive surgical treatment. It is defined as clinical relapse of the disease after complete healing of the surgical wound. In case the clinical relapse occurs later than one year, the disease is defined as de-novo perianal fistula [
22]. In our study, we investigated complete healing of perianal fistulas in all patients, so we set the endpoint of follow up at six months after definitive surgical treatment. The recorded rate of complete healing was 100% in all patients of both imaging control groups. Nevertheless, two patients (one from each imaging control group) were re-admitted with relapse of the disease within one year after completion of the surgical treatment. They were considered recurrent perianal fistulas outside the prespecified period of follow-up.
Surgical treatment of a perianal fistula is also considered successful if anal continence is preserved intact postoperatively. Risk factors which are associated with disruption of anal continence after surgery for perianal fistulas include pre-existing incontinence, age older than 45 years, high transsphincteric, supralevator and horseshoe type of fistula, division greater than 50% of the internal anal sphincter and division greater than 66% of the external anal sphincter [
39,
40,
41]. There are many scales of fecal incontinence described in literature, which validate the severity of different symptoms and their effect on quality of life. In our study, we used the Wexner/Cleveland Clinic Fecal Incontinence Score, which is simple and can easily be applied to a patient. It evaluates five parameters (solid stool, liquid stool or gas incontinence, usage of pads, lifestyle alteration) and each parameter is graded on a scale from 0 to 4, with a high score of 20. The Wexner score is one of the most widely adopted fecal incontinence scales, which can be utilized in clinical practice and for research purposes [
10,
42].
Abbas et al studied 179 patients treated for perianal fistulas of cryptoglandular origin. The surgical procedures performed included fistulotomy, rectal advancement flap and fistula plugging. They reported baseline stool or gas incontinence symptoms in 7.3% of the patients postoperatively [
40]. Van Koperen et al studied also 179 patients treated for perianal fistulas of cryptoglandular origin. One hundred and nine (109) patients were treated with fistulotomy for low fistulas and 70 patients were treated with rectal advancement flap for high fistulas. A high percentage (40%) of patients in both groups reported soiling postoperatively [
43]. Jayarajah et al studied 34 patients with simple cryptoglandular fistula-in-ano who were treated with surgery. The overall preoperative and postoperative rates of incontinence were 18 and 38% respectively. Nine (9) patients (27%) had deterioration of incontinence and 3 patients (9%) had an improvement [
44]. In our study, 5 patients (7%) in the total sample had symptoms of mild incontinence postoperatively. Three (3) patients (4.2%) had a Wexner score of 3 (2 in group MRI, 1 in group MRI+3D-EAUS), and 2 patients (2.8%) had a Wexner score of 4 (1 in each imaging control group). There was no statistically significant difference in fecal incontinence postoperatively between the two groups (
Table 7 and
Table 8).
Finally, complex perianal fistulas are considered a distinct category with challenging surgical treatment. Patients with Crohn’s disease may require up to 6 surgical procedures for complex fistulas [
45]. According to the literature, the optimal outcomes are achieved with sphincter-saving procedures, i.e. ligation of the intersphincteric fistulous tract (LIFT) or rectal advancement flaps, and new biological therapies, i.e. adipose derived stem-cells or mesenchymal cells, especially in patients with Crohn’s disease [
46,
47]. Burney published a case-series study of 483 patients with perianal fistulas, which reported the long-term results of surgical management. Patients with complex and recurrent perianal fistulas (18%) had to undergo up to 4 surgical operations before complete healing was achieved [
48]. In our study, patients with complex perianal fistulas also had a higher probability to undergo more than one surgical procedure to eliminate the disease, compared to patients with simple fistulas.
4.1. Study limitations:
The categories of supralevator, extrasphincteric, rectovaginal, perineal fistulas and no finding included a small number of patients. The incidence of these types of perianal fistulas was also low in recently published studies (supralevator 9.5%, extrasphincteric 0%, rectovaginal 5%) [
5,
49]. Nevertheless, values of diagnostic accuracy for the above fistulas in our study should be interpreted with great caution. Future studies of combined diagnostic accuracy for pelvic MRI and 3D-EAUS should focus on intersphincteric and transsphincteric perianal fistulas, which are the two prevalent types, or include increased number of patients for the other less common categories.
The postoperative follow-up for our patients was defined at six months. However, two cases of perianal fistula recurrence occurred later, within the first year after surgical treatment. Future studies which will record postoperative rates of perianal fistula healing and recurrence should have a follow-up period of at least 12 months.
Author Contributions
Conceptualization, N. V., C. K. (Christoforos Kosmidis), G. C., F.A.K. and I.K.; methodology, N.V., C.K. (Christoforos Kosmidis), G.C., F.A.K. and I.K .; software, F.A.K. and N.V.; validation, N. V., C. K. (Christoforos Kosmidis), F.A.K., C.E., V.L., C.M.M., C.S. and I.K.; formal analysis, N.V. and F.A.K. ; investigation, N. V., C. K. (Christoforos Kosmidis), G. C., F.A.K., A.V.K. and K.S. ; resources, N.V., C.K. (Christoforos Kosmidis), F.A.K., C.E., V.L., C.S, K.P. and K.S.; data curation, N.V., C.K. (Christoforos Kosmidis), F.A.K., C.E., V.L., C.M.M., C.S., A.V.K. and I.K. X.; writing—original draft preparation, , N.V., C.K. (Christoforos Kosmidis) and F.A.K.; writing—review and editing, N. V., C. K. (Christoforos Kosmidis), G. C., F.A.K., C.M.M., G.A., K.S. and I.K.; visualization, N.V., C.E. and V.L.; supervision, N. V., C. K. (Christoforos Kosmidis), G. C., F.A.K. and I.K. All authors have read and agreed to the published version of the manuscript.