1. Introduction
The Cognitive–Attentional Syndrome (CAS) is a core concept in the theoretical model of metacognitive therapy for psychological disorders [
1]. The Self-regulatory Executive Function model (S-REF) [
2,
3] considers inflexible and recurrent patterns of thinking in response to negative thoughts, feelings, and beliefs as the proximal cause of such disorders. The CAS is a set of symptoms associated with this maladaptive style of processing and is considered a transdiagnostic feature of psychopathology. It consists of perseverative and negative thinking (worry or rumination), threat monitoring, and unhelpful, paradoxically inefficient coping strategies used to deal with the first two aspects, such as thought suppression or avoidance.
CAS is hypothesized to develop due to underlying maladaptive metacognitions, which include positive and negative beliefs about thinking (i.e., metacognitive beliefs) [
1,
4,
5]. For example, holding the belief that worrying keeps one safe (positive metacognitive belief) predisposes a person to worrying in response to a negative thought about potential danger. Furthermore, holding the belief that worrying will ruin one’s health (negative metacognitive belief) leads to a persistence of worrying because the person uses unhelpful strategies such as thought suppression to interrupt the process. The S-REF model posits that in all situations in which there is a discrepancy between self-relevant goals (outer circumstances and mental states) and perceived goals, Self-regulatory Executive Function becomes activated. This process might be accompanied by CAS activation and, therefore, negative emotions, self-appraisal, and sense of threat. While, in most people, periods of CAS activation are brief or non-existent, some will experience a vicious circle of prolonged CAS activation. For example, a person with health-related anxiety during the COVID-19 pandemic engages in negative repetitive thoughts about health-related issues due to positive metacognitive beliefs (e.g., “thinking about it will help me prepare”). Consequently, this person may find that they are devoting excessive amounts of time to worry. This observation may trigger worrying about worrying due to negative metacognitive beliefs about uncontrollability and negative consequences of worrying (e.g., “I cannot stop these thoughts and I will lose my mind”). Strategies such as attempting to suppress thoughts will probably lead to greater preoccupation with these thoughts, meaning that CAS is likely to continue to occur.
This process is understood in the S-REF model as the cause of emotional and other psychiatric disorders and their core, common component. Numerous studies confirm that maladaptive metacognitive beliefs and symptoms of CAS are positively associated with a wide range of psychological and behavioral problems, including emotional disorders such as depression, anxiety, and stress, as well as trauma-related disorders such as adjustment disorder (AjD) and posttraumatic stress disorder (PTSD) [
6,
7,
8,
9].
The aim of this study was to examine the association between symptoms of CAS and stress- and trauma-related psychopathology in the context of the COVID-19 pandemic, which is perceived as a highly stressful situation by most people [
10]. To date, there have been many publications on the prevalence of emotional disorders obtained in studies conducted during the current pandemic. For example, in a web-based survey conducted by Rossi et al. [
11], rates of different mental health outcomes were assessed in the Italian general population three to four weeks into lockdown measures after the outbreak of the pandemic. Almost a quarter (23%) of respondents reported symptoms of adjustment disorder, 37% reported posttraumatic stress symptoms, 22% high perceived stress, 21% anxiety, and 17% depression. In many other studies conducted in the first and subsequent months of the pandemic, increased rates of anxiety, depressive symptoms, and stress-related symptoms were found as well [
12,
13,
14,
15]. These symptoms seemed to persist throughout the pandemic. Given the wide range of mental health symptoms observed as outcomes of the pandemic, we decided to test whether CAS – a transdiagnostic factor and the main mechanism behind the persistence of psychopathology according to metacognitive theory – predicted symptoms of various emotional disorders in the first months of the pandemic or three months later. In particular, we focused on symptoms of adjustment disorder and traumatic stress, but additionally on other symptoms frequently included in studies on mental health during the pandemic (i.e., generalized anxiety and depression).
2. Materials and Methods
2.1. Participants
The total sample for this study consisted of 1,792 participants who were recruited online via social media (Facebook). They participated voluntarily and no financial or material reward was offered. Ethical approval for the study was granted by the Ethics Committee of the Faculty of Psychology at the [blinded for peer review]. The study was conducted via the internet using the Qualtrics platform. Participants had to be aged 18 years or older at the time of the survey; a total of 50 people were excluded from the study due to being under 18 years and 51 were excluded due to partial completion of the questionnaires, so the analysis ultimately included 1,693 participants. No other exclusion criteria were applied. The majority of respondents (78%) were female (21% men, and 1% intergender or non-binary) and the mean age of the sample was 31.23 years (SD=9.60, range 18–78 years).
The data was collected at two time points. The first wave took place from March 25th to April 30th 2020, three weeks after identification of the first coronavirus-infected patient in Poland, at the time when the state of epidemic had just been announced and the lockdown restrictions were introduced. It was therefore the time of the greatest restrictions, consisting of, for example, the closure of educational institutions, the closure of borders to air and rail traffic, prohibition of travel without due need, etc. After consenting, participants completed the online survey, which lasted about 25 minutes; if they agreed to participate in the second measurement, they were asked to provide an email address.
The second time point of the study was three months after the first wave; the data was collected from 3th July to 11th August 2020. In total, 418 people responded in the second wave, but only 362 answered questions. As in the first wave, most participants (78%) were female (20% men, and 1% intergender or non-binary) and the mean age of the sample was 30.40 years (SD=8.39, range 18–66 years). At the beginning of June, the rate of new infections was 300 people a day. In July, however, there was a sharp increase in new infections, with the rate doubling to about 650 infections per day. The rapid increase was related to the ongoing parliamentary elections and increased holiday tourism, during which, among other things, little attention was paid to maintaining social distancing and wearing masks.
2.2. Measures
The first part of the online survey included the measurement of sociodemographic variables (gender, age, relationship status, employment status, years of education, possibility of remote work). Then, respondents provided answers on self-report questionnaires:
Cognitive–Attentional Syndrome:
The Cognitive–Attentional Syndrome Questionnaire (CAS-1) [
1,
4] questionnaire consists of 16 items. The first two are questions concerning the frequency of rumination and worry as well as concentration on threats. A further six items concern maladaptive behaviors used to cope with negative emotions and/or thoughts, such as thought and situation avoidance, drinking or substance abuse, and attempts to control thoughts or emotions. The last eight items concern positive and negative metacognitive beliefs core to Cognitive–Attentional Syndrome (e.g., “worrying too much could harm me” or “worrying helps me cope”). The results of the questionnaire were calculated as in previous papers [
4,
16]. The total results can range from 0 to 128, where a higher result indicates a greater level of Cognitive–Attentional Syndrome. The Polish version has good psychometric properties; in the current study Cronbach’s alpha was .83.
Impaired Functioning:
The Work and Social Adjustment Scale (WSAS) [
17] is a short questionnaire used to measure impaired functioning. It consists of five items with a nine-point scale (0 indicates
no impairment at all and 8 indicates
severe impairment). Possible scores range from 0 to 45. Based on the results [
17], it is possible to distinguish three levels of functioning: 1–10 points: mild functional impairment; 11–20: moderately severe functional impairment; 21+: severe functional impairment. The original English version of the WSAS was translated into Polish with the use of the back translation procedure. The Polish version of the scale exhibited satisfactory internal consistency of scores in the current sample (α=.80).
Symptoms of Adjustment Disorder:
The Adjustment Disorder – New Module 20 (ADNM-20) [
18,
19] is a questionnaire that measures symptoms of adjustment disorder. The ADNM-20 consists of two parts: a list of stressors and an item symptom list. The list of stressful events comprises a wide range of experiences (19 potential stressors; e.g., financial problems, divorce, serious illness), and requires reference to the event that was the most aggravating in the last six months. For the purpose of the study, the COVID-19 pandemic was also added to this list. The symptom list section measures the symptoms in response to the most distressing event(s) the respondent has experienced. The ADNM-20 was developed to more closely align with the ICD-11 guidelines for AjD and this is reflected in its focus on the two core symptom clusters of Preoccupation (four items) and Failure to Adapt (four items) [
20]. However, it also includes the four associated symptom clusters of Avoidance (four items), Depression (three items), Anxiety (two items), and Impulsivity (three items). All items are answered on a four-point Likert scale with possible scores ranging from 20 to 80. The questionnaire consists of six subscales: Preoccupation, Failure to Adapt, Avoidance, Depressive Mood, Anxiety, and Impulsivity. Preoccupation and Failure to Adapt are the core symptoms of AjD and can be considered together as one subscale (AjD-C). Avoidance, Depressive Mood, Anxiety, and Impulsivity are accessory symptoms and can also be considered together as one subscale (AjD-AS). The Polish version of the ADNM-20 has excellent internal consistency, with α=.91 [
10].
Traumatic Stress:
The International Trauma Questionnaire (ITQ) [
21] is a self-report measure of ICD-11 PTSD symptoms. Respondents complete the ITQ in relation to the most traumatic event they have experienced before answering questions about symptoms. In the current study, they were also given the option of referring to their experience of the COVID-19 pandemic. The PTSD items in the ITQ are completed with reference to how much the respondent has been bothered by each symptom in the past month and are accompanied by three items measuring functional impairment caused by these symptoms. All items are answered on a five-point Likert scale, with possible scores ranging from 0 to 24. A symptom is considered present where a score of ≥ 2 (
moderately) is achieved. PTSD diagnosis requires traumatic exposure, at least one symptom present from each symptom cluster (Re-experiencing, Avoidance, and Sense of Threat), and endorsement of at least one indicator of functional impairment. The psychometric properties of the ITQ have been examined in both clinical and general population samples [
22]. The measure is available in many language versions, including Polish (
www.traumameasuresglobal.com/itq). The internal consistency of the PTSD item scores in the current sample was very good (
α=.90).
Depression: Additionally, nine symptoms of depression were measured using the
Patient Health Questionnaire-9 (PHQ-9) [
23,
24], available from the MAPI Research Institute, (
www.phqscreeners.com). Respondents indicate how often they have been bothered by each symptom over the last two weeks using a four-point Likert scale. Possible scores range from 0 to 27, with higher scores indicating higher levels of depression. A cut-off score of 15 was used to identify participants likely to meet the criteria for depressive disorder, in accordance with the results of the meta-analysis of Manea et al. [
25]. PHQ-9 scores have very good psychometric properties, showing excellent internal consistency in the current sample (
α=.93).
Generalized Anxiety: Symptoms of generalized anxiety were measured using the
Generalized Anxiety Disorder 7-item Scale (GAD-7) [
26]. Like the PHQ-9, respondents indicate how often they have been bothered by each symptom over the last two weeks on a four-point Likert scale. Possible scores range from 0 to 21, with higher scores indicating higher levels of anxiety. The cut-off point for the scale is ≥10 points [
27]. The GAD-7 has been shown to be a reliable and valid measure in multiple studies; the Polish translation of the scale is available from the MAPI Research Institute
(www.phqscreeners.com). The internal consistency of the scores for the current sample was excellent (
α=.92).
2.3. Statistical Analyses
In the first step, descriptive statistics and a series of paired-samples
t-tests with Hedges’
g [
28] were performed using IBM
’s SPSS 28. Following the guidelines for managing missing data in longitudinal studies [
29], attrition analysis was performed. Student’s
t-test was used to investigate differences in the severities of measured symptoms of disorders between the two waves of study. For further investigation, structural equation modeling (SEM) was conducted in Mplus 8.5 [
30] in order to determine relations between stressors, Cognitive–Attentional Syndrome, impaired functioning, and symptoms of: depression, generalized anxiety, AjD, and PTSD. The recommendations of Hu and Bentler [
31] were used to determine the goodness of fit of the data to the model. The following parameters were taken into account, in accordance with the most commonly-used standards: RMSEA<.08 means acceptable fit and <.05 means good fit; CFI>.90 and TLI>.90 means acceptable fit, and CFI and TLI>.95 means good fit; SRMR should be<.08.
3. Results
3.1. Descriptive Statistics and Attrition Analysis
Descriptive statistics and the prevalence of disorders are shown in
Table 1. Attrition analysis was performed using Little
’s MCAR test on variables associated with psychopathology. The percentage of missing data ranged from 78.6% to 88.2%; due to high levels, no data imputation technique was introduced and partial responses were used for t-test analyses. Little
’s MCAR test was insignificant, χ
2(27)=24.60, p=.579, and we therefore concluded that missing data were randomly distributed.
3.2. Changes in the Severity of Symptoms
One of the purposes of this study was to examine changes in the severities of symptoms over time. A series of paired-samples t-tests were conducted to compare the number of stressors, symptoms of PTSD and adjustment disorder, depression, generalized anxiety, CAS, and impaired functioning between the two time points. There were significant differences in PTSD scores: Re-experiencing (MT1=2.93, SDT1=2.55, MT2=4.86, SDT2=2.48, t(286)=-12.86, p=<.001, Hedges’ g=-.76, 95% CI [-.90,-.63]), Avoidance (MT1=3.77, SDT1=2.62, MT2=5.53, SDT2=2.62, t(286)=-11.91, p=< .001, g=-.67, 95% CI[-.80,-.63]), and Sense of Threat (MT1=3.70, SDT1=2.72, MT2=5.37, SDT2=2.77, t(286)=-11.52, p=<.001, g=-.61, 95% CI[-.72,-.49]), core symptoms of AjD (MT1=21.65, SDT1=6.43, MT2=20.11, SDT2=6.67, t(329)=4.91, p=<.001, g=.23, 95% CI[.14,.33]), accessory symptoms of AjD (MT1=31.95, SDT1=8.98, MT2=29.98, SDT2=9.68, t(329)=4.45, p=<.001, g=.21, 95% CI [.12,.30]), Depression (MT1=11.43, SDT1=6.73, MT2=10.05, SDT2=6.55, t(278)=4.78, p=<.001, g=.21, 95% CI [.12,.30]), Generalized Anxiety (MT1=9.55, SDT1=6.10, MT2=7.71, SDT2=65.71, t(365)=4.46, p=<.001, g=.31, 95% CI [.21,.41]), and Impaired Functioning (MT1=20.97, SDT1=9.12, MT2=18.23, SDT2=10.54, t(361)=5.73, p=<.001, g=.28, 95% CI [.18,.37]). The following were statistically insignificant: changes in numbers of stressors (MT1=5.49, SDT1=2.42, MT2=5.42, SDT2=2.50, t(359)=.64, p=.522) and level of Cognitive–Attentional Syndrome (MT1=75.65, SDT1=20.33, MT2=73.96, SDT2=21.23, t(278)=1.73, p=.085). The results of this study indicate that there was a statistically significant difference between severity of symptoms AjD, depression, generalized anxiety and impaired functioning between the two time points: their intensities decreased over time. In contrast, PTSD symptoms worsened between measurements.
3.3. Structural Equation Modeling
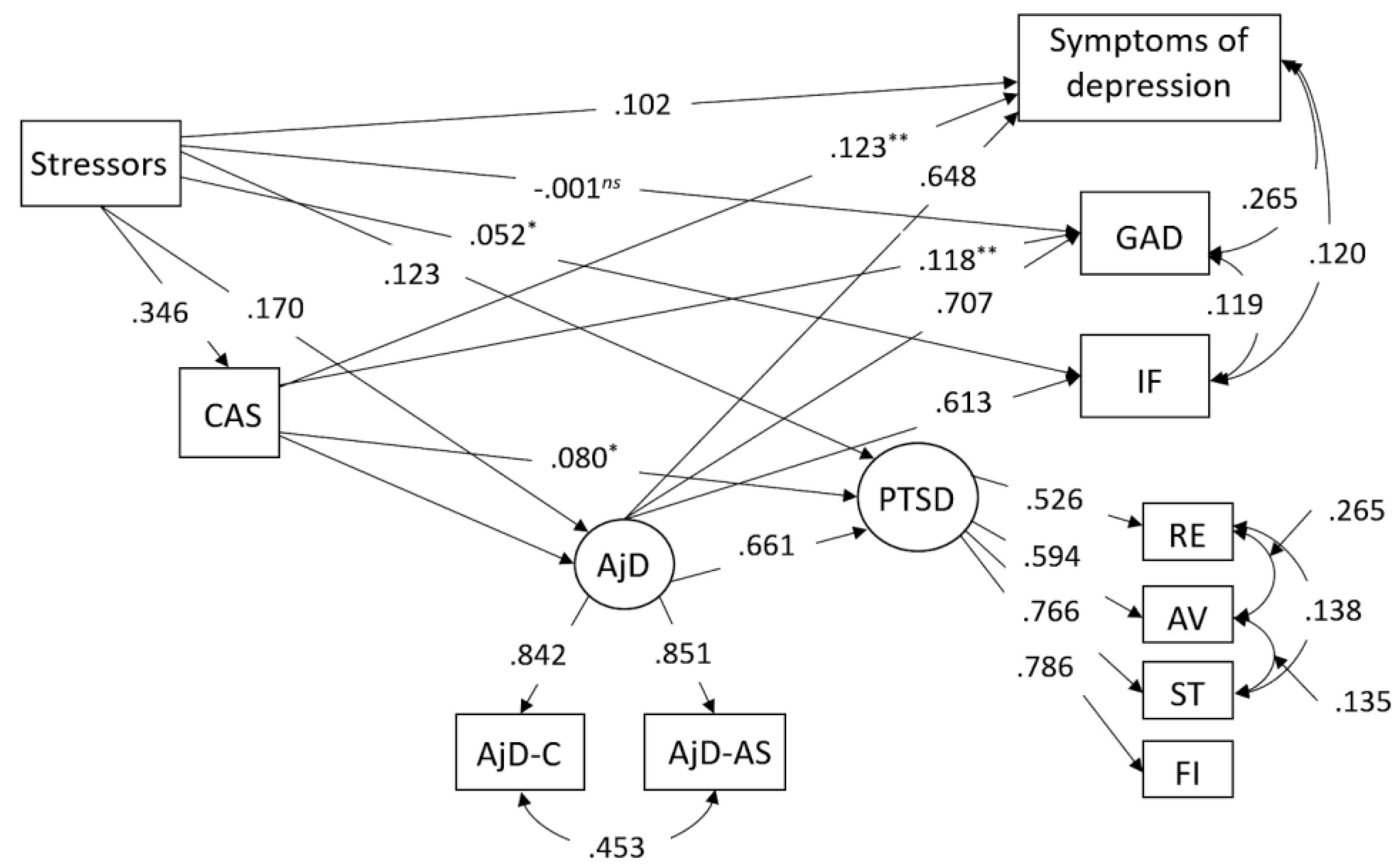
The multiple-mediator SEM model was checked with a maximum likelihood estimator (ML) with 1,000 bootstrap re-samples. The proposed model of the relationship between the variables at first measurement (see
Figure 1) showed good model fit indicators: χ
2(28)=186.155, p=<.001; CFI = .984; TLI = .969; RMSEA = .058 (90% CI [.050, .066]; p = .049); SRMR = .020. In addition, indirect effects were analyzed between traumatic events and PTSD included other variables. The results are shown in
Table 2. Cognitive–Attentional Syndrome and AjD were responsible for partial mediation in the relationship between stressors and other studied symptoms.
Figure 1.
Structural equation model for T1. All paths except marked have p<.001.
Figure 1.
Structural equation model for T1. All paths except marked have p<.001.
Notes: CAS – Cognitive–Attentional Syndrome, AjD – adjustment disorder, AjD-C – core symptoms of AjD, AjD-AS – accessory symptoms of AjD, GAD – symptoms of generalized anxiety, RE – re-experiencing, AV – avoidance, ST – sense of threat, IF – impaired functioning, FI – PTSD functional impairment, *p<.05, **p<.01, ns–non significant.
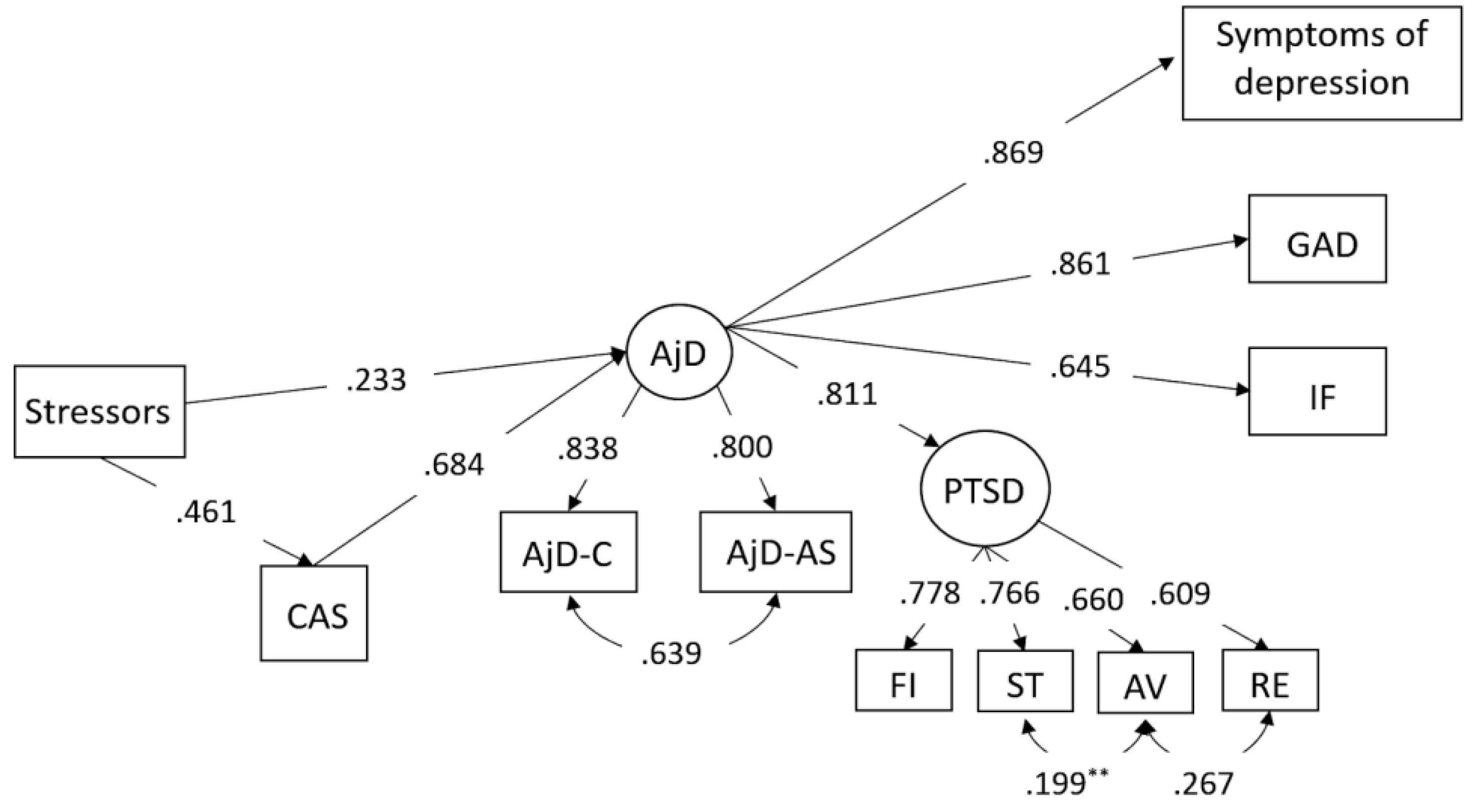
The T1 model was also used for the second measurement. Model fit indicators remained at an acceptable level: χ
2(28)=81.748, p=<.001; CFI=.976; TLI=.952; RMSEA=.073 (90% CI [.055,.092]; p=.020); SRMR=.029. However, not all paths in the model were statistically significant. After removing them (see
Figure 2), the model’s fit indicators improved slightly: χ
2(39)=98.023, p=<.001; CFI=.973; TLI=.962; RMSEA=.065 (90% CI [.049,.081]; p=.061); SRMR=.033. According to simulations performed on the fit indicators, a value of ∆CFI smaller than or equal to -.01 indicates that the null hypothesis of invariance should not be rejected [
32]. This confirms that the proposed models differ from each other.
Figure 2.
Structural equation model for T2. All paths except those marked have p<.001.
Figure 2.
Structural equation model for T2. All paths except those marked have p<.001.
Notes: CAS – Cognitive–Attentional Syndrome, AjD – Adjustment Disorder, AjD-C – core symptoms of AjD, AjD-AS – accessory symptoms of AjD, GAD – symptoms of Generalized Anxiety, RE – Re-experiencing, AV – Avoidance, ST – Sense of Threat, IF – Impaired Functioning, FI – PTSD functional impairment, **p<.01.
Table 2.
Indirect effects.
Table 2.
Indirect effects.
| Effects |
T1
Estimate |
T2
Estimate |
| 90% CI |
p |
90% CI |
p |
| Stressors –> CAS –> PTSD |
.028
.006–.050 |
.038 |
.070
-.012–.152 |
.162 |
| Stressors –> AjD –> PTSD |
.112
.085–.139 |
<.001 |
.145
.071–.219 |
.001 |
| Stressors –> CAS –> AjD –> PTSD |
.153
.128–.178 |
<.001 |
.211
.137–.284 |
<.001 |
| Stressors –> AjD –> IF |
.104
.080–.128 |
<.001 |
.124
.061–.186 |
.001 |
| Stressors –> CAS –> AjD –> IF |
.142
.123–.161 |
< 001 |
.180
.129–.231 |
<.001 |
| Stressors –> AjD –> Depression Symptoms |
.110
.083–.137 |
<.001 |
.174
.076–.272 |
.003 |
| Stressors –> CAS –> Depression Symptoms |
.042
.020–.065 |
.002 |
.025
-.076–.127 |
.681 |
| Stressors –> CAS –> AjD –> Depression Symptoms |
.150
.124–.150 |
<.001 |
.254
.149–.359 |
<.001 |
| Stressors –> CAS –> GAD |
.041
.021–.061 |
.001 |
.016
-.059–.091 |
.730 |
| Stressors –> AjD –> GAD |
.120
.091–.149 |
<.001 |
.168
.079–.257 |
.002 |
| Stressors –> CAS –> AjD –> GAD |
.164
.139–.189 |
<.001 |
.244
.158–.330 |
<.001 |
4. Discussion
According to the metacognitive theory of psychopathology, Cognitive–Attentional Syndrome (CAS) is the main factor in the development and maintenance of symptoms, including those that appear as the result of exposure to stress and trauma [
10]. This assumption has been confirmed in many previous studies. The main aspect of CAS is extended negative thinking, in the forms of worry or rumination. In our study, we aimed to answer the question of whether CAS predicted symptoms of stress and trauma related disorders in the course of the COVID-19 pandemic, which was perceived as a highly stressful situation by the majority of respondents [
10]. This study had a longitudinal design with two time points: at the beginning of the pandemic and three months later. Therefore, we analyzed the hypothesized model with reference to these two measurement points that assumed that CAS played a key role in predicting symptoms of psychopathology.
The first measurement included a large sample of adult Poles recruited through the internet in the first phase of COVID-19 pandemic (i.e., in the middle of March and April 2020). The tested model revealed that the CAS was predictive of all included symptomatology – adjustment disorder, posttraumatic stress disorder, depression, and generalized anxiety. However, it was not predictive of symptoms of impaired functioning measured by the Work and Social Adjustment Scale. Stressors included in the Adjustment Disorder – New Module 20 scale were predictive for CAS, which was a mediator between these events and AjD, PTSD, as well as impaired functioning and depressive symptoms. Cognitive–Attentional Syndrome in the first wave was also a direct predictor of all disorders included in the study. In other words, the symptoms of CAS intensified the symptoms of these disorders. This result may be treated as a confirmation of other findings revealing that life stressors are important risk factors for psychopathology in general, but also that AjD is a disorder specifically related to stress, because the more stressors, the more intense the internal cognitive-emotional processing in the form of worrying/rumination – the core symptom of AjD.
It is worth considering the context of the pandemic at the time the measurements took place. The government of Poland announced the first restrictions on the 11th of March 2020 (closure of all municipal institutions, schools, and childcare facilities, and the banning of all mass events or even going to the woods), and on March 20th the state of epidemic was officially announced. Mandatory government measures followed soon after, with the temporary closure of all non-essential services and additional physical distancing measures, etc. Our study started on the 25th of March – immediately after the introduction of these strict restrictions. Thus, the findings of the study at the first time point can be interpreted in the context of the pandemic as the result of an ongoing process of adaptation to the early phase of this unknown situation, which was somewhat naturally associated with an increased state of stress and anxiety, resulting in an increase of all symptoms of psychopathology.
The pandemic situation was somewhat different at the time of the second measurement: around this time, there was an increase in new infections due to the loosening of the restrictions (July 2020). However, this was also the holiday season, and this significant increase might be also explained by fatigue with the previous strict restrictions that had finally been lifted. The data from that time confirms that CAS mediated between reported stressors and symptoms of adjustment disorder. However, in this model it was AjD that mediated the relationship between both stressors and CAS with co-occurring symptoms of other disorders (PTSD, depression, and generalized anxiety). A significant increase of AjD symptoms predicted the severity of other symptoms, which indicates that intense stress and disturbances in adjustment were a dominant feature in the picture of psychopathology at that time. This means that extended negative thinking, which is the core aspect of CAS and also one of the main symptoms of AjD, was not only significantly increased, but also a leading cause of general symptom aggravation. Despite the decrease in the intensity of AjD symptoms between waves, it became a significant predictor of other psychopathology symptoms at both time points, except for traumatic stress. The reduced intensity of symptoms may be related to getting used to the unique situation and gradually becoming better at coping with it. However, symptoms of PTSD might be specific against other symptoms that co-occur in reaction to prolonged stressful situations or increased between two time points as a result of cumulative (traumatic) stress.
The main limitation of the study is, of course, the significant reduction in the number of participants at the second time point, which restricted the possible statistical analyses. Moreover, recruitment in our study relied on voluntary participation through social networks. For this reason, there may be an important selection bias against people who do not use social networks, as well as self selection, resulting in the highly unbalanced gender ratio (the much higher proportion of women) and predominance of young adults. An additional factor related to the respondents was a significant representation of people working from home offices. Furthermore, the survey was based on self-report assessments, not interview-based measures. Therefore, the rates of mental health outcomes obtained in this study should be interpreted with caution.
5. Conclusions
The results of this study confirm the mediating role of Cognitive–Attentional Syndrome between reported stressors and symptoms of emotional disorders (adjustment disorder, traumatic stress, generalized anxiety, and depression) in the context of the initial phase of the COVID-19 pandemic. It confirms also that this situation was highly stressful for many people, as indicated by the symptoms of stress and trauma-related disorders; however, even in the initial phase, including the first months after the outbreak of the pandemic, changes in symptoms were observed: symptoms decreased with time and in specific contexts, such as the loosening of restrictions and the onset of the holiday season.
Funding
This work was supported by the Faculty of Psychology, University of Warsaw, from the funds awarded by the Ministry of Science and Higher Education in the form of a subsidy for the maintenance and development of research potential in 2022 and in 2023 (501-D125-01-1250000 zlec. 5011000228 and ….).
Institutional Review Board Statement
The study was approved by Ethical Committee of the Faculty of Psychology, University of Warsaw, on 2nd July 2020 (approval code n° 6/7/2020). In accordance with the Helsinki Declaration, patients provided written informed consent to participate in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be made available by the corresponding author upon request.
Acknowledgments
The authors would like to thank Szymon Szumiał (Faculty of Management, University of Warsaw) for supervision of statistical analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wells A. Metacognitive therapy for anxiety and depression. New York: Guilford Press; 2009.
- Wells, A.; Matthews, G. Attention and emotion: A clinical perspective. Hove Lawrence Erlbaum, UK; 1994.
- Wells A; Matthews G. Modeling cognition in emotional disorder: The S-REF model. Behav. Res. Ther. 1996; 34(11):881–8. [CrossRef]
- Kowalski, J.; Dragan, M. Cognitive-attentional syndrome – The psychometric properties of the CAS-1 and multi-measure CAS-based clinical diagnosis. Compr. Psychiatry 2019; 91:13-21. [CrossRef]
- Capobianco, L.; Nordahl, H. A brief history of metacognitive therapy: From cognitive science to clinical practice. Cogn. Behav. Pract. 2023; 30(1):45-54, . [CrossRef]
- Sun, X.; Zhu, C.; So, S.H.W. Dysfunctional metacognition across psychopathologies: A meta-analytic review. Eur Psychiatry 2017; 45:139-153. [CrossRef]
- Gkika, S.; Wittkowski, A.; Wells, A. (2017). Social cognition and metacognition in social anxiety: a systematic review. Clin. Psychol. Psychother. 25, 10–30. [CrossRef]
- Brown, R.L. et al. The metacognitive model of post-traumatic stress disorder and metacognitive therapy for post-traumatic stress disorder: A systematic review. Clin. Psychol. Psychother. 2022; 29(1):131-146. [CrossRef]
- Dragan, M.; Kowalski, J. Childhood adversities and psychopathology in participants with high and low severity of cognitive-attentional syndrome symptoms. Eur. J. Trauma Dissociation 2020: 4:100112. [CrossRef]
- Dragan, M.; Grajewski, P.; Shevlin, M. Adjustment disorder, traumatic stress, depression and anxiety in Poland during an early phase of the COVID-19 pandemic. Eur. J. Psychotraumatol 2021; 12(1):1860356. [CrossRef]
- Rossi, R. et al. Stressful life events and resilience during the COVID-19 lockdown measures in Italy: association with mental health outcomes and age. Front. Psychiatry 2021; 12:635832. [CrossRef]
- Hyland, P. et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020; 142(3):249-256. [CrossRef]
- Shevlin, M. et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych open 2020; 6(6): e125. [CrossRef]
- Gambin, M. et al. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland. Specific predictors and differences in symptoms severity. Compr. Psychiatry 2021; 105:152222. [CrossRef]
- Olff, M. et al. Mental health responses to COVID-19 around the world. Eur. J. Psychotraumatol 2021; 12(1):1929754.
- Fergus, T.A., Bardeen, J.R., Orcutt, H.K. Attentional control moderates the relationship between activation of the cognitive attentional syndrome and symptoms of psychopathology. Personal. Individ. Differ. 2012; 53(3): 213-217. [CrossRef]
- Mundt, J. C.; Marks, I. M.; Shear, M. K.; Greist, J. M. The Work and Social Adjustment Scale: A simple measure of impairment in functioning. Br. J. Psychiatry 2002; 180:461–464. [CrossRef]
- Einsle, F.; Köllner, V.; Dannemann, S.; Maercker, A. Development and validation of a self-report for the assessment of adjustment disorders. Psychol. Health Med. 2010; 15:584–595. [CrossRef]
- Lorenz, L.; Bachem, R. C.; Maercker, A. The Adjustment Disorder–New Module 20 as a screening instrument: Cluster analysis and cut-off values. Int. J. Occup. Environ. Med. 2016; 7:215-220. [CrossRef]
- Shevlin, M. et al. Measuring ICD-11 adjustment disorder: The development and initial validation of the International Adjustment Disorder Questionnaire. Acta Psychiatr. Scand. 2020; 141(3):265-274. [CrossRef]
- Cloitre, M.; Shevlin, M.; Brewin, C. R.; Bisson, J. I.; Roberts, N. P.; Maercker, A.; Karatzias T.; Hyland, P. The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr. Scand. 2018; 138:1-11. [CrossRef]
- Redican, E. et al. The latent structure of ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD in a general population sample from USA: a factor mixture modelling approach. J. Anxiety Disord. 2022; 85:102497. [CrossRef]
- Kroenke, K.; Spitzer, R. L.; Williams, J. B. W. The PHQ-9. J. Gen. Intern. Med. 2001; 16:606–613.
- Kokoszka, A.; Jastrzębski, A.; Obrębski, M. Psychometric properties of the Polish version of Patient Health Questionnaire-9. Psychiatria 2016; 13:187–193.
- Manea, L.; Gilbody, S.; McMillan, D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen. Hospit. Psychiatr. 2015; 37:67–75. [CrossRef]
- Spitzer, R. L.; Kroenke, K.; Williams, J. B. W.; Löwe, B. A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med. 2006; 166:1092.
- Rutter, L. A.; Brown, T. A. Psychometric properties of the Generalized Anxiety Disorder Scale-7 (GAD-7) in outpatients with anxiety and mood disorders. J. Psychopathol. Behav. Assess. 2016; 39:140–146. [CrossRef]
- Lin, L.; Aloe, A. M. Evaluation of various estimators for standardized mean difference in meta-analysis. Stat. Med. 2021; 40(2):403–426. [CrossRef]
- Nicholson, J. S.; Deboeck, P. R.; Howard, W. Attrition in developmental psychology: A review of modern missing data reporting and practices. Int. J. Behav. Dev. 2017; 41(1):143–153.
- Muthén, L. K.; Muthén, B. O. MPlus user’s Guide 8th version (March). Los Angeles: Authors; 2017.
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999; 6(1):1–55. [CrossRef]
- Cheung, Gordon W.; Rensvold, Roger B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Modeling 2002; 9(2):233–255.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).