Submitted:
29 May 2023
Posted:
30 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Database search
2.2. Data collection
2.3. Study registration
3. Results
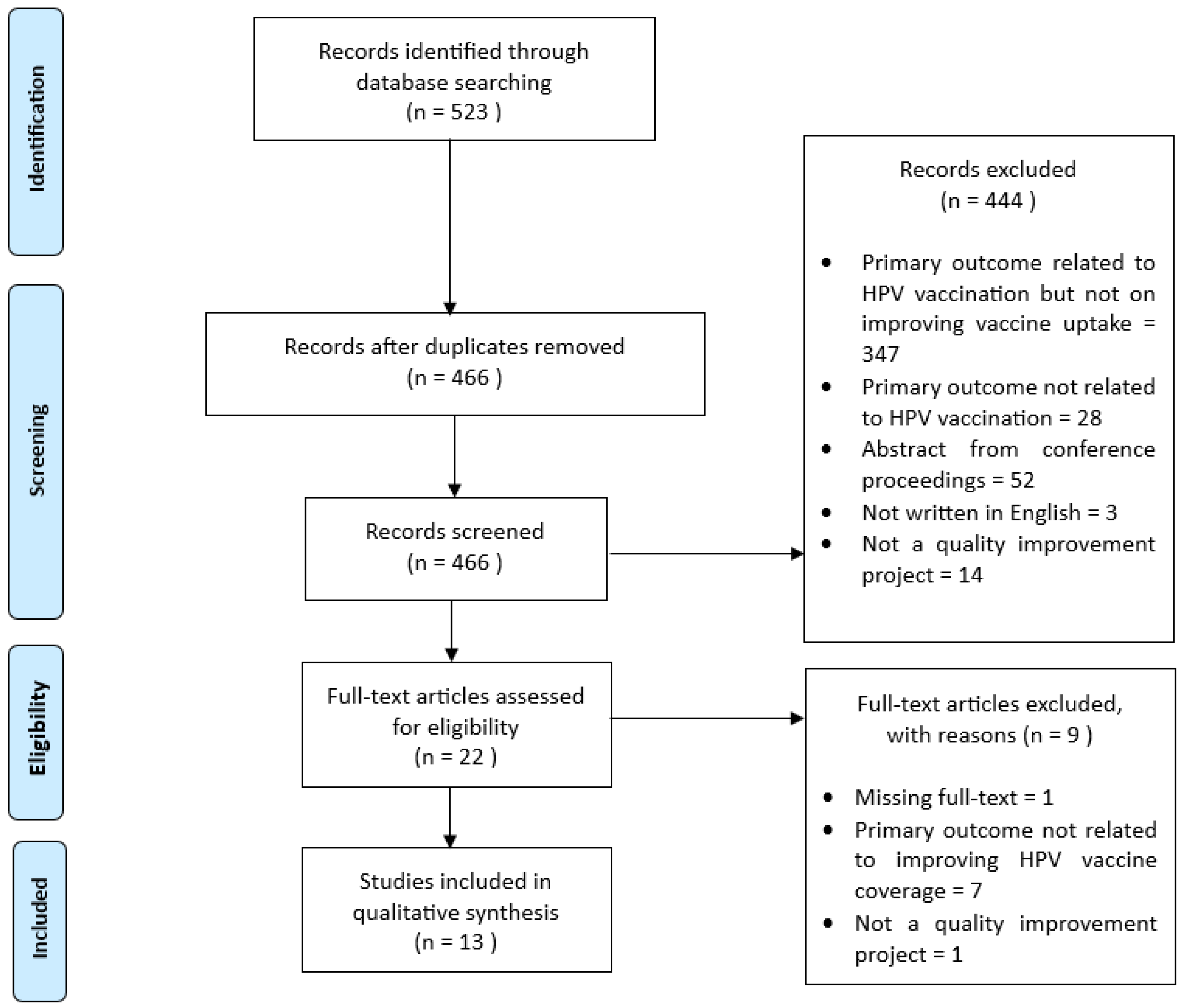
3.1. Search results
| No. | First author, year | Intervention focus group | Mode of intervention | Primary outcome | Results |
|---|---|---|---|---|---|
| 1 | Berstein, 2022 [10] | System/policy | Inclusion of HPV vaccination with other scheduled vaccines for adolescents | HPV vaccines rates among 11-12 years-old teens | HPV vaccination rate increased from 17.8% to 63.6% |
| Patients | Parents were sent pre-visit email - contains vaccine information prior to annual healthcare visit |
||||
| HCP | Initiatives to improve provider communication skills | ||||
| 2 | Davis, 2022 [1] | HCP | Educational intervention |
HPV vaccination rates in children 11−12 years old |
|
| 3 | Gilkey, 2019 [11] | HCP | An in-clinic training session (include instruction and video on effective communication) | HPV vaccination coverage among patients aged 12 to 14 years |
HPV vaccination coverage increased in the QI arm by 8.6% |
| 4 | Mackey, 2019 [12] | HCP | Reminder system for both physicians and patients | HPV vaccination coverage among patients aged 11 to 12 | The immunization rate (for the first injection) was significantly greater than baseline |
| Patients | Reminder mails to caregivers of patients aged 11-12 years | ||||
| 5 | Mathur, 2019 [13] | HCP | Four 1-hour webinars highlighting on effective communication with parents regarding the HPV vaccine. |
HPV vaccination coverage (dose 1) for all 11- and 12-year-old | Initiation of HPV vaccination increased in all participating practices (from 56.4% to 71.2%) |
| 6 | McGaffey, 2019 [14] | HCP | Periodic training on presumptive approach in HPV vaccine recommendation | HPV vaccination rate among 9-26 years-old patients (both male and female) |
|
| Patients |
|
||||
| System/policy |
|
||||
| 7 | Nissen, 2019 [15] | Patients | Implement reminder and recall system for eligible patients who were unvaccinated or with incomplete vaccination | The rate of HPV vaccine administration |
|
| HCP |
|
||||
| 8 | Oliver, 2020 [16] | HCP |
|
Impact on HPV immunization rates (HPV initiation, series completion, and missed opportunities) |
|
| 9 | Perkins, 2021 [17] | HCP |
|
Adolescent vaccination rates among adolescents who turned 13 years |
|
| 10 | Singh, 2022 [18] | Patients |
|
HPV vaccination rates among young adults |
The vaccination rate among patients who were seen in person at the clinic improved from 2.5% (1 of 40) to 46.6% (21 of 45). |
| HCP |
|
||||
| 11 | Smajlovic, 2023 [19] | Patients |
|
HPV-vaccination series completion rate to 70% among the 13-year-old patient population | The overall HPV vaccination series completion rates in increased from 27% to 65% |
| HCP | QI team provided feedback via email to providers on a 6-monthly basis to a year on the monitored HPV vaccine completion rates among 13-year-old adolescents | ||||
| System | A licensed professional-initiated protocol (LPIP) dedicated for nursing staff is triggered when an eligible patient is scheduled for a visit | ||||
| 12 | Wallace-Brodeur, 2020 [20] | HCP | Training sessions on effective recommendation for HPV vaccine, strategies to reduce MOs, and techniques on motivational interviewing |
Reduction in MOs (defined as any visit that a patient did not receive the vaccination dose despite being eligible) | LHDs reduced MOs for HPV vaccination by 25.3% |
| 13 | Zorn, 2023 [21] | HCP | Provider and staff training, with peer-to-peer coaching by QI champion | HPV initiation at age 9 and series completion rates |
|
| Setting/system | Electronic medical records support | ||||
| Patients |
|
3.2. Healthcare provider-targeted empowerment approach
3.3. Reshaping adolescents, parents, and/or caregivers’ perception on HPV vaccination
3.4. Redesigning healthcare system and policy changes
4. Discussion
5. Conclusion
Author Contributions
Funding Information
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davis, K.R.; Norman, S.L.; Olson, B.G.; Demirel, S.; Taha, A.A. A Clinical Educational Intervention to Increase HPV Vaccination Rates Among Pediatric Patients Through Enhanced Recommendations. J. Pediatr. Heal. Care 2022, 36, 589–597. [Google Scholar] [CrossRef] [PubMed]
- CDC HPV Vaccination Recommendations. Centers Dis. Control Prev. 2021, 1–2.
- Wallace-Brodeur, R.; Li, R.; Davis, W.; Humiston, S.; Albertin, C.; Szilagyi, P.G.; Rand, C.M. A Quality Improvement Collaborative to Increase Human Papillomavirus Vaccination Rates in Local Health Department Clinics. Prev. Med. (Baltim). 2020, 139, 106235. [Google Scholar] [CrossRef]
- Pingali, C.; Yankey, D.; Elam-Evans, L.D.; Markowitz, L.E.; Williams, C.L.; Fredua, B.; McNamara, L.A.; Stokley, S.; Singleton, J.A. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13-17 Years — United States, 2020. MMWR Recomm. Reports 2021, 70, 1184–1190. [Google Scholar] [CrossRef] [PubMed]
- Austin, B.; Morgan, H. Improving Human Papillomavirus Vaccine Uptake in the Family Practice Setting. J. Nurse Pract. 2019, 15, e123–e125. [Google Scholar] [CrossRef]
- Mitchell, K.; Saraiya, M.; Bhatt, A. Increasing HPV Vaccination Rates Through National Provider Partnerships. J. Women’s Heal. 2019, 28, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia Action Plan - Towards the Elimination of Cervical Cancer in Malaysia 2021-2030; Abdul Samad, S., Ed.; 1st ed.; Ministry of Health, Malaysia: Putrajaya, 2021. Ministry of Health, Malaysia: Putrajaya.
- Gilkey, M.B.; Bednarczyk, R.A.; Gerend, M.A.; Kornides, M.L.; Perkins, R.B.; Saslow, D.; Sienko, J.; Zimet, G.D.; Brewer, N.T. Getting Human Papillomavirus Vaccination Back on Track: Protecting Our National Investment in Human Papillomavirus Vaccination in the COVID-19 Era. J. Adolesc. Heal. 2020, 67, 633–634. [Google Scholar] [CrossRef]
- Schneiter, M.; Rositch, A.; Levinson, K.; Stone, R.; Fader, A.; Ferriss, J.; Wethington, S.; Beavis, A. The Gynecologic Oncologist as the HPV Champion: Missed Opportunities for Cancer Prevention. Gynecol. Oncol. 2021, 162, S292–S293. [Google Scholar] [CrossRef]
- Bernstein, T.A.; Broome, M.; Millman, J.; Epstein, J.; Derouin, A. Promoting Strategies to Increase HPV Vaccination in the Pediatric Primary Care Setting. J. Pediatr. Heal. Care 2022, 36, e36–e41. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Parks, M.J.; Margolis, M.A.; McRee, A.-L.; Terk, J. V Implementing Evidence-Based Strategies to Improve HPV Vaccine Delivery. Pediatrics 2019, 144. [Google Scholar] [CrossRef]
- Mackey, J.K.; Thompson, K.; Abdulwahab, A.; Huntington, M.K. A Simple Intervention to Increase Human Papillomavirus Vaccination in a Family Medicine Practice. S. D. Med. 2019, 72, 438–441. [Google Scholar] [PubMed]
- Mathur, M.; Campbell, S. Statewide Pediatric Quality Improvement Collaborative for HPV Vaccine Initiation. Wis. Med. J. 2019, 118, 42–43. [Google Scholar]
- McGaffey, A.; Lombardo, N.P.; Lamberton, N.; Klatt, P.; Siegel, J.; Middleton, D.B.; Hughes, K.; Susick, M.; Lin, C.J.; Nowalk, M.P. A “Sense”-Ational HPV Vaccination Quality Improvement Project in a Family Medicine Residency Practice. J. Natl. Med. Assoc. 2019, 111, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Nissen, M.; Kerkvliet, J.L.; Polkinghorn, A.; Pugsley, L. Increasing Rates of Human Pipillomavirus Vaccination in Family Practice: A Quality Improvement Project. S. D. Med. 2019, 72, 354–360. [Google Scholar] [PubMed]
- Oliver, K.; McCorkell, C.; Pister, I.; Majid, N.; Benkel, D.H.; Zucker, J.R. Improving HPV Vaccine Delivery at School-Based Health Centers. Hum. Vaccines Immunother. 2019, 15, 1870–1877. [Google Scholar] [CrossRef]
- Perkins, R.B.; Foley, S.; Hassan, A.; Jansen, E.; Preiss, S.; Isher-Witt, J.; Fisher-Borne, M. Impact of a Multilevel Quality Improvement Intervention Using National Partnerships on Human Papillomavirus Vaccination Rates. Acad. Pediatr. 2021, 21, 1134–1141. [Google Scholar] [CrossRef]
- Singh, C. Increasing Knowledge of Human Papillomavirus Among Young Adults. J. Nurse Pract. 2022, 18, 618–621. [Google Scholar] [CrossRef]
- Smajlovic, A.; Toth, C.D. Quality Improvement Project to Increase Human Papillomavirus Two-Dose Vaccine Series Completion by 13 Years in Pediatric Primary Care Clinics. J. Adolesc. Heal. 2023. [Google Scholar] [CrossRef]
- Wallace-Brodeur, R.; Li, R.; Davis, W.; Humiston, S.; Albertin, C.; Szilagyi, P.G.; Rand, C.M. A Quality Improvement Collaborative to Increase Human Papillomavirus Vaccination Rates in Local Health Department Clinics. Prev. Med. (Baltim). 2020, 139, 106235. [Google Scholar] [CrossRef]
- Zorn, S.; Darville - Sanders, G.; Vu, T.; Carter, A.; Treend, K.; Raunio, C.; Vasavada, A. Multi-Level Quality Improvement Strategies to Optimize HPV Vaccination Starting at the 9-Year Well Child Visit: Success Stories from Two Private Pediatric Clinics. Hum. Vaccines Immunother. 2023, 19, 1–11. [Google Scholar] [CrossRef]
- Austin, B.; Morgan, H. Improving Human Papillomavirus Vaccine Uptake in the Family Practice Setting. J. Nurse Pract. 2019, 15, e123–e125. [Google Scholar] [CrossRef]
- Bernstein, T.A.; Broome, M.; Millman, J.; Epstein, J.; Derouin, A. Promoting Strategies to Increase HPV Vaccination in the Pediatric Primary Care Setting. J. Pediatr. Heal. Care 2022, 36, e36–e41. [Google Scholar] [CrossRef] [PubMed]
- McGaffey, A.; Lombardo, N.P.; Lamberton, N.; Klatt, P.; Siegel, J.; Middleton, D.B.; Hughes, K.; Susick, M.; Lin, C.J.; Nowalk, M.P. A “Sense”-Ational HPV Vaccination Quality Improvement Project in a Family Medicine Residency Practice. J. Natl. Med. Assoc. 2019, 111, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Singh, C. Increasing Knowledge of Human Papillomavirus Among Young Adults. J. Nurse Pract. 2022, 18, 618–621. [Google Scholar] [CrossRef]
- Nissen, M.; Kerkvliet, J.L.; Polkinghorn, A.; Pugsley, L. Increasing Rates of Human Pipillomavirus Vaccination in Family Practice: A Quality Improvement Project. S. D. Med. 2019, 72, 354–360. [Google Scholar]
- Zorn, S.; Darville - Sanders, G.; Vu, T.; Carter, A.; Treend, K.; Raunio, C.; Vasavada, A. Multi-Level Quality Improvement Strategies to Optimize HPV Vaccination Starting at the 9-Year Well Child Visit: Success Stories from Two Private Pediatric Clinics. Hum. Vaccines Immunother. 2023. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.R.; Norman, S.L.; Olson, B.G.; Demirel, S.; Taha, A.A. A Clinical Educational Intervention to Increase HPV Vaccination Rates Among Pediatric Patients Through Enhanced Recommendations. J. Pediatr. Heal. Care 2022, 36, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Handayani, P.W.; Hidayanto, A.N.; Budi, I. User Acceptance Factors of Hospital Information Systems and Related Technologies: Systematic Review. Informatics Heal. Soc. Care 2018, 43, 401–426. [Google Scholar] [CrossRef]
- Askelson, N.M.; Ryan, G.; Seegmiller, L.; Pieper, F.; Kintigh, B.; Callaghan, D. Implementation Challenges and Opportunities Related to HPV Vaccination Quality Improvement in Primary Care Clinics in a Rural State. 2019, 44, 790–795. [Google Scholar] [CrossRef]
- Perkins, R.B.; Brogly, S.B.; Adams, W.G.; Freund, K.M. Correlates of Human Papillomavirus Vaccination Rates in Low-Income, Minority Adolescents: A Multicenter Study. J. Women’s Heal. 2012, 21, 813–820. [Google Scholar] [CrossRef]
- Hirth, J. Disparities in HPV Vaccination Rates and HPV Prevalence in the United States: A Review of the Literature. Hum. Vaccines Immunother. 2019, 15, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Davidoff, F.; Batalden, P.; Stevens, D.; Ogrinc, G.; Mooney, S. Publication Guidelines for Quality Improvement in Health Care: Evolution of the SQUIRE Project. In Proceedings of the Quality and Safety in Health Care; BMJ Publishing Group Ltd, October 1 2008; Vol. 17, pp. i3–i9.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





