1. Introduction
According to the World Health Organization (WHO), having sexual intercourse without contraception for more than 12 months without getting pregnant can be considered infertility [
1,
2]. Male factors, female factors and a mix of factors can all contribute to infertility. However, in the social and cultural context that advocates childbearing, women often bear more blame and pressure. Many families still blame women for infertility. About 20-30% of infertility cases are caused by a combination of male and female factors. Approximately 50% of cases of infertility is due to female factors. Male factors implicated in at least 30% [
3,
4,
5]. About 85% of infertility cases have a clear cause. That still leaves 15% of infertility unexplained [
6].
Infertility can cause stress in couples, producing feelings of sadness, panic, disappointment and so on. During infertility treatment, women may have concerns about body image, miscarriage, childbirth and more [
7]. Infertility can affect infertile couples’ mental health, family relationships and social stress [
8]. In addition, the prevalence of infertility continues to increase worldwide [
9]. Since the 21st century, infertility treatment technology has made great progress. As a result, more and more infertile couples are seeking infertility treatment. Not all infertile couples have a successful outcome, however [
10].
As the duration of infertility increases, so does the psychological stress. The effect was particularly pronounced when infertility lasted longer than eight years [
11]. Infertility can have negative social and emotional consequences for couples [
12]. Depression is one of the main mental problems associated with infertility [
13]. The rate of depression among women seeking infertility treatment was very high, at about 17%. Despite advances in assisted reproduction, nearly half of infertile couples never seek infertility treatment. Because of the high cost and fear of treatment failure [
14]. Studies have shown that infertility itself and infertility treatment are associated with poor mental health, particularly depression. The prevalence of depression was higher in infertile couples with lower incomes [
15] and those who were unsuccessful in treatment [
16]. There is a similar pattern in polygamous areas [
15]. Gender is linked to depression in infertile couples. Women have a higher prevalence of depression than men in infertile couples undergoing assisted reproduction, according to a study conducted in Turkey [
17]. Among couples who were successfully treated for infertility, those who had twins had a higher level of depression than those who had only one child [
13]. The prevention and intervention of infertile couples who are prone to depression is urgent. If not foreseen, it can lead to substance abuse and suicide. And can affect the treatment compliance of infertile couples [
16]. It is necessary to pay attention to the mental health of infertile couples and to discover the unknown factors related to depression in infertile couples. This is relevant for the 48 million couples and 186 million individuals worldwide who experienced infertility [
1].
Several factors have been found to be related to mental health difficulties among infertile couples, either general factors or specific factors related to infertility. Monthly household income in Thailand has been on the rise since 2004 [
18]. Family income affects the mental health of family members. A study in Thailand found that people with lower incomes and poorer economic conditions were at higher risk of mental problems [
19]. Therefore, it is meaningful to study income and depression in infertile couples in Thailand.
Couples who had several unsuccessful or no infertility treatments had a lower quality of life than couples who had no infertility history and had at least one child [
20]. For patients receiving infertility treatment, the higher the number of infertility treatments, the higher the risk of prenatal depression [
21]. Moreover, women who become pregnant after undergoing assisted reproductive technology have a higher risk of depression [
22]. In addition, the effect between intimate relationships and mental health goes both ways. Mental problems can affect intimate relationships and vice versa [
23]. Having a good marital relationship also has a positive impact on couples’ mental health. The marital relationship is very important to the individual. At the same time, it affects their social life [
24].
Personality is one of the determinants of mental health. People with neuroticism tend to have more negative emotions and lower emotional stability and thus lower inner strength [
25]. In addition, neuroticism is a risk factor for depression [
26]. More specifically, depression in infertile women is linked to certain personality traits [
27]. More research is needed to explain the relationship between personality traits and depression in infertile couples.
Substance abuse is found to be related to mental health problems. For example, cannabis use has been associated with anxiety, depression, and suicide. Cannabis use often precedes depression and suicidal behavior [
28]. Persistent use of multiple substances has been linked to the development of depression. It is especially higher in men [
29]. People with depression are at increased risk of suicide when they abuse substances [
30]. There is a risk of depression with early substance use, such as early use of marijuana, alcohol and other illicit drugs [
31]. Still, the relationship between substance uses and depression in infertile couples remains unknown.
Moreover, Thai people are influenced by the late King Bhumibol’s sufficiency economy concept. The philosophy of autarky economy is put forward in the practice of the living standard of Thai people. This principle can be applied to individuals, societies and states [
32]. Sufficient economy is enough to support ourselves. This philosophy, based on moderation, reasonableness and immunity, is the way to improve the happiness of life of the Thai people. Moderation means not doing too much and not doing too little. Rationality means making decisions with reason and with care. Immunity refers to the ability to cope with future changes and impacts. Sufficiency economy requires knowledge to help with planning and decision-making, as well as the virtues of honesty, wisdom, patience and perseverance. The sufficiency economy provides a good way to guide people’s lifestyles and social norms. Significantly, following the sufficiency economy can bring people happiness and improve their satisfaction in life [
33]. We can infer from this that sufficiency economy is related to mental health, which may affect depression in infertile couples.
The objective of this study was to investigate the prevalence of depression among infertile couples and the factors associated with it, as mentioned earlier. However, the factors that were examined included both non-specific and specific aspects of infertility and their relevance to the Thai population.
2. Materials and Methods
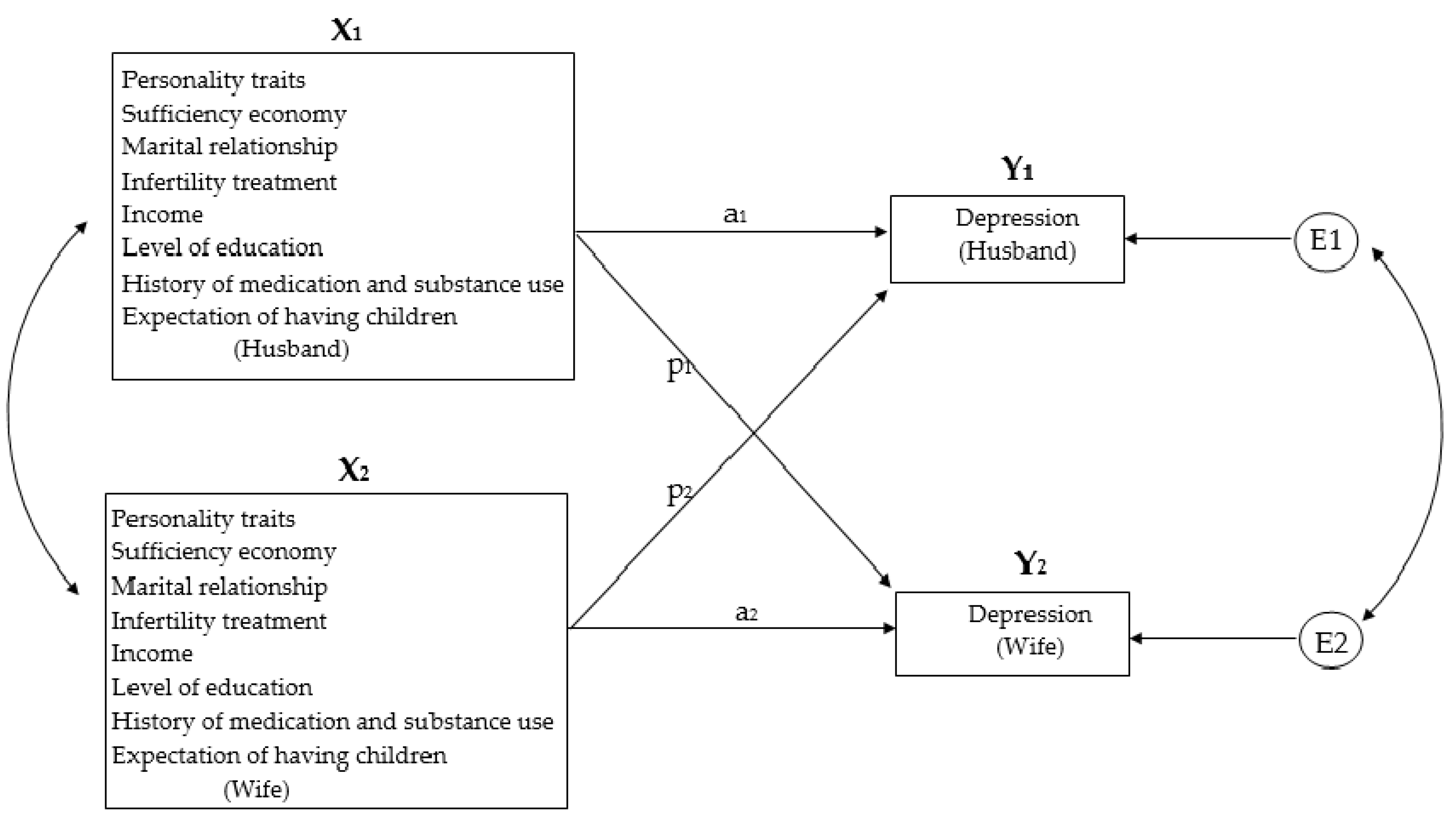
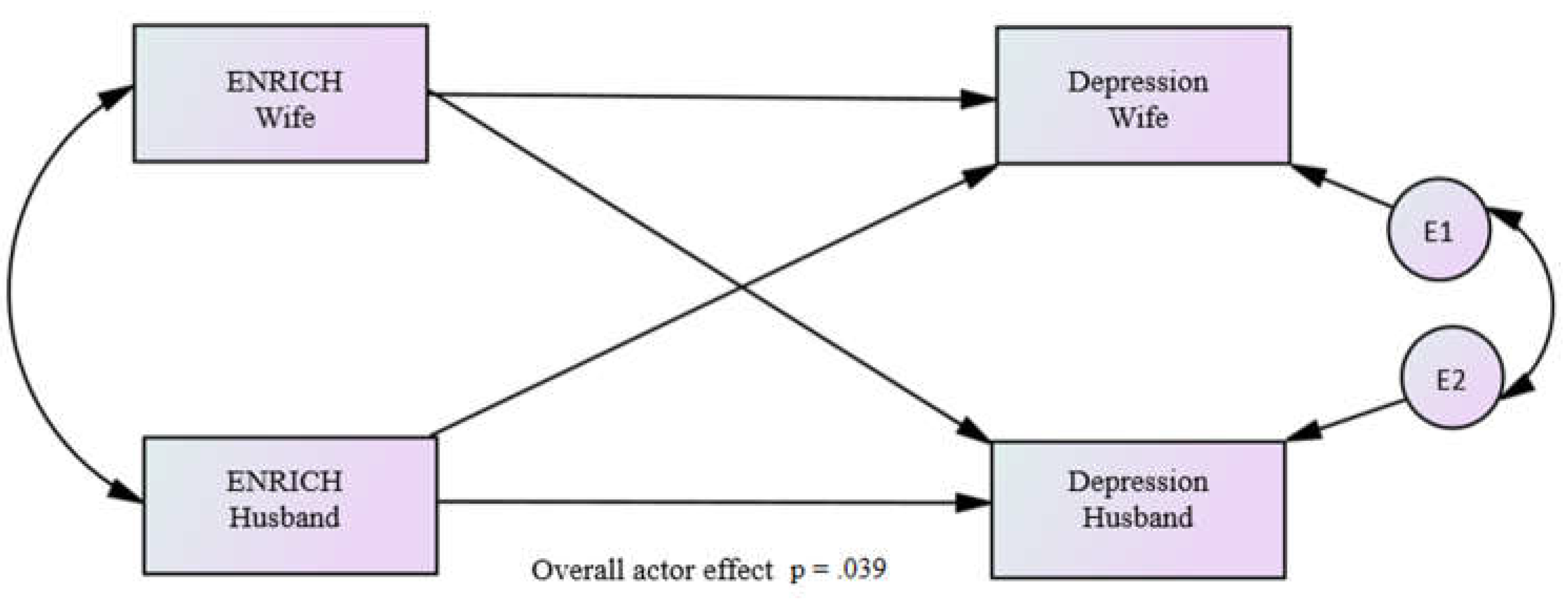
The study was designed to explore the relationship between sociodemographic factors and personal history, personality traits, marital satisfaction, sufficiency economy and depression in infertile couples, while the interaction between partners. More details can be found in
Figure 1.
Scope of the study
A cross-sectional study was conducted. The population was infertile couples who attended CMEx Fertility Center, under the Faculty of Medicine, Chiang Mai University and Chiang Mai IVF (In Vitro Fertilization) Polyclinic. A convenience sampling was carried out. This phase was conducted random days and centers. The study was run at CMEx Fertility Center under the Faculty of Medicine, Chiang Mai University and Chiang Mai IVF Polyclinic during July-August 2022.
Participants
A total of 150 infertile couples (300 participants) enrolled in the study at CMEx Fertility Center under the Faculty of Medicine, Chiang Mai University and Chiang Mai IVF Polyclinic.
Sampling
In this study, random sampling was used to reduce selection bias [
34]. The student PI and the research assistant invited participants to answer the questionnaire at CMEx Fertility Center, under the Faculty of Medicine, Chiang Mai University on Monday, Wednesday and Friday. The research team invited participants to answer the questionnaire at Chiang Mai IVF Polyclinic on Tuesday, Thursday and Weekends.
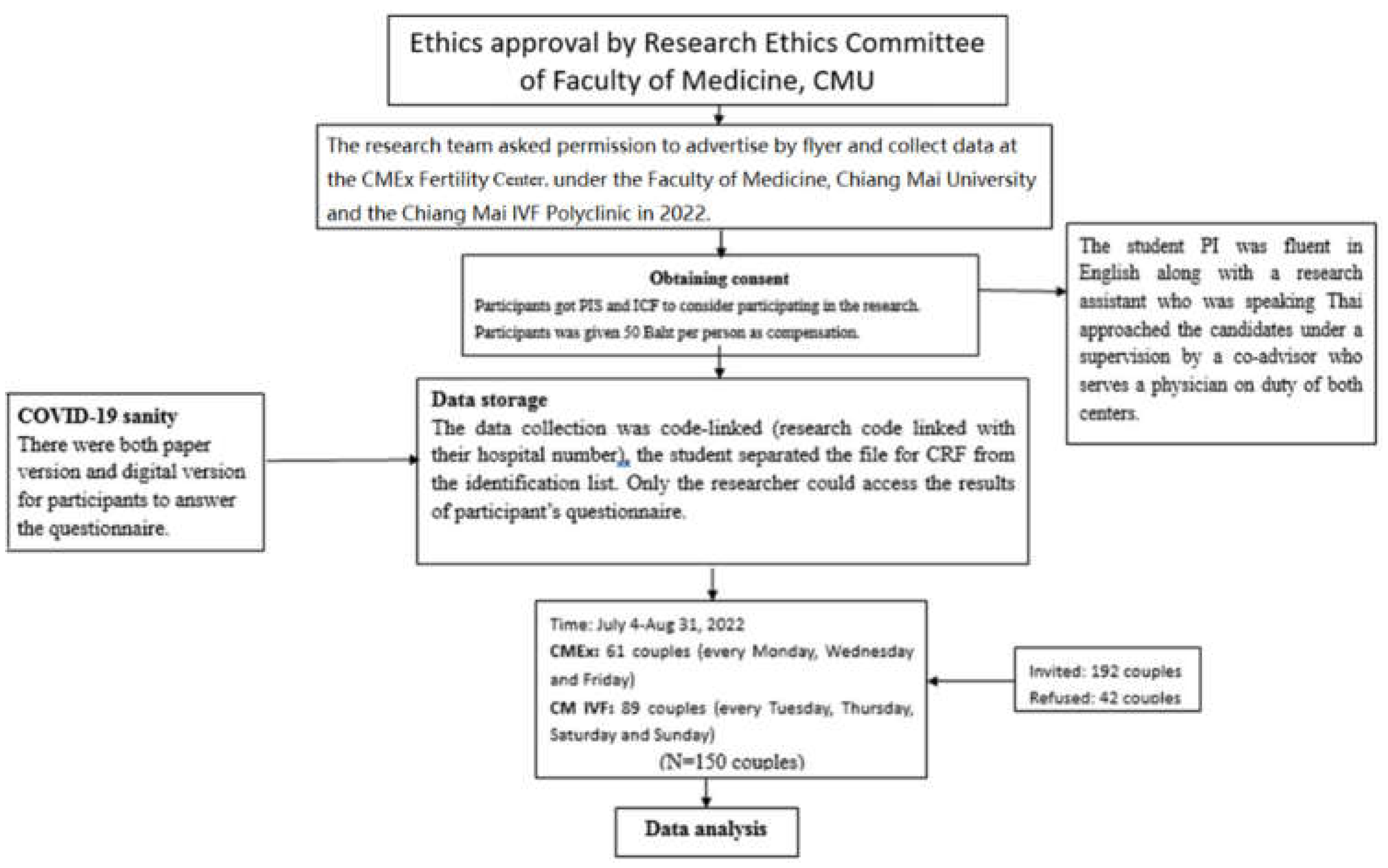
The study was approved by the Research Ethics Committee of Faculty of Medicine, Chiang Mai University. Data was collected under the supervision of the visiting physician at both centers. Participants could choose to fill out the paper version of the questionnaire or the digital version. Each member of the couple had to fill out a questionnaire separately. A questionnaire filled out by only one person is considered invalid. Data collection ended after sufficient sample size is obtained. In
Figure 2, a total of 192 couples, 150 couples were finally recruited into this study.
Measurements
The measurements were available in Thai and English. In addition, considering the situation of COVID-19, participants could choose to fill out a paper or digital version. The measurements included are as follows:
1. Sociodemographic information: The demographic information packet required basic sociodemographic information, including gender, age, education, monthly income, the expectation of having children and the number of infertility treatments, etc.
2. Outcome Inventory-21 (OI-21): OI-21 was a self-rating questionnaire used to measure levels of depression. Anxiety, somatization, and interpersonal difficulties were also measured. It was a five-point scale, ranging from 0 (Never) to 4 (Almost Always). There were 21 questions in total [
35].
3. Zuckerman-Kuhlman-Aluja Personality Questionnaire (ZKA-PQ): The short version had 40 questions. It was a four-point questionnaire, from 1 (Strongly Disagree) to 4 (Strongly Agree).The five-factor structure includes neuroticism (NE), sensation seeking (SS), extraversion (EX), activity (AC) and aggressiveness (AG) [
36].
4. ENRICH (Evaluation and Nurturing Relationship Issues, Communication and Happiness) Marital Satisfaction Scale: It had 15 questions and 5 of them were negative ratings. ENRICH scale included communication, resolve family conflicts, family roles, financial problems, free time, sexual relationship, child rearing, family and friends, and religion [
37].
5. Sufficiency Economy Scale (SES): There were 9 questions, on a seven-point scale, from 1 (Strongly Disagree) to 7 (Strongly Agree). There was a better understanding and practice for the sufficiency economy, then the higher the score [
38].
The Cronbach’s alpha of all the measurements were greater than 0.7.
Data analysis
Descriptive analyses were applied to sociodemographic data and scores of mental health outcomes, mainly in terms of frequency, percentage, mean and standard deviation.
For the difference test, the t test and the χ2 test were respectively applied according to the continuous data and the categorical data, e.g., educational level and substance use. ANOVA was used to test the differences in depression among multiple groups, e.g., the total score of depression among different groups of occupation. The correlation between variables and depression scores was checked by Pearson’s correlation and point-biserial correlation. Multiple regression was used to analyze the predictors of depression.
The interaction analysis of APIM was carried out by the multilevel modeling written by Kenny [
39]. The coefficient analysis employed t tests and Z tests. Using the standard deviations of all at once, and the standard deviations of a single parent at once. Values above
r = 0.10 were small effect sizes. Between
r = 0.30 and
r = 0.50 was a moderate effect size. Above
r = 0.50 was a large effect size [
40]. SPSS version 22 was used for data analysis. The results were statistically significant when the p-value was less than 0.05 with a 95% confidence interval.
3. Results
3.1. Sociodemographic characteristics of the participants
A total of 300 participants (150 couples) were included in the study. The sociodemographic characteristics of the participants are shown in
Table 1. The mean age of men wa slightly higher than that of women,
t (280) = 2.824, p <.01. More than a third of the participants were self-employed, or about 35.2%.
More than half of the participants had a bachelor’s degree, accounting for 58.7%. The majority of monthly income in participants was less than or equal to 760 USD. Most participants strongly agreed with the expectation of having children, at about 78.0%. The majority of the participants (46.0%) had received one infertility treatment. More than 90% of the participants did not smoke. More than half of the participants did not drink alcohol.
Regarding the prevalence of depression, it was 6.7 %, equally in males and females. No significant gender differences were observed in other sociodemographic characteristics between males and females.
3.2. Descriptive statistics and test difference
Females had significantly higher mean score of neuroticisms than males. The remaining results showed no statistically significant differences in gender (
Table 2).
3.3. Test differences between sociodemographic factors and depression
Sociodemographic factors and depression were not statistically significant among participants (
Table 3), but occupation (female only,
F (4) = 4.223, p <.01.
3.4. Pearson’s Correlation between variables and depression
Pearson’s correlation showed that aggression and neuroticism were positively correlated with depression while the expectation of having children, ENRICH marital satisfaction and sufficiency economy were negatively correlated with depression.
As with all participants, aggression and neuroticism were positively correlated with depression in male participants. ENRICH marital satisfaction was negatively correlated with depression in male participants.
Similarly, aggression and neuroticism were positively correlated with depression in female participants. Alcohol and substance use were positively correlated with depression in female participants. The expectation of having children, ENRICH marital satisfaction and sufficiency economy were negatively correlated with depression in female participants. More details are shown in
Table 4.
3.5. The multiple regression predicting depression symptom.
Regression analysis was performed for the variables correlated with depression. The results showed that neuroticism (p = .001) and marital satisfaction (p = .015) were predictors of depression in all participants. Marital satisfaction was predictor of depression in male participants, p = .030. Neuroticism was predictor of depression in female participants, p = .001 (
Table 5).
3.6. The effect of variables on the depression of the partner on APIM
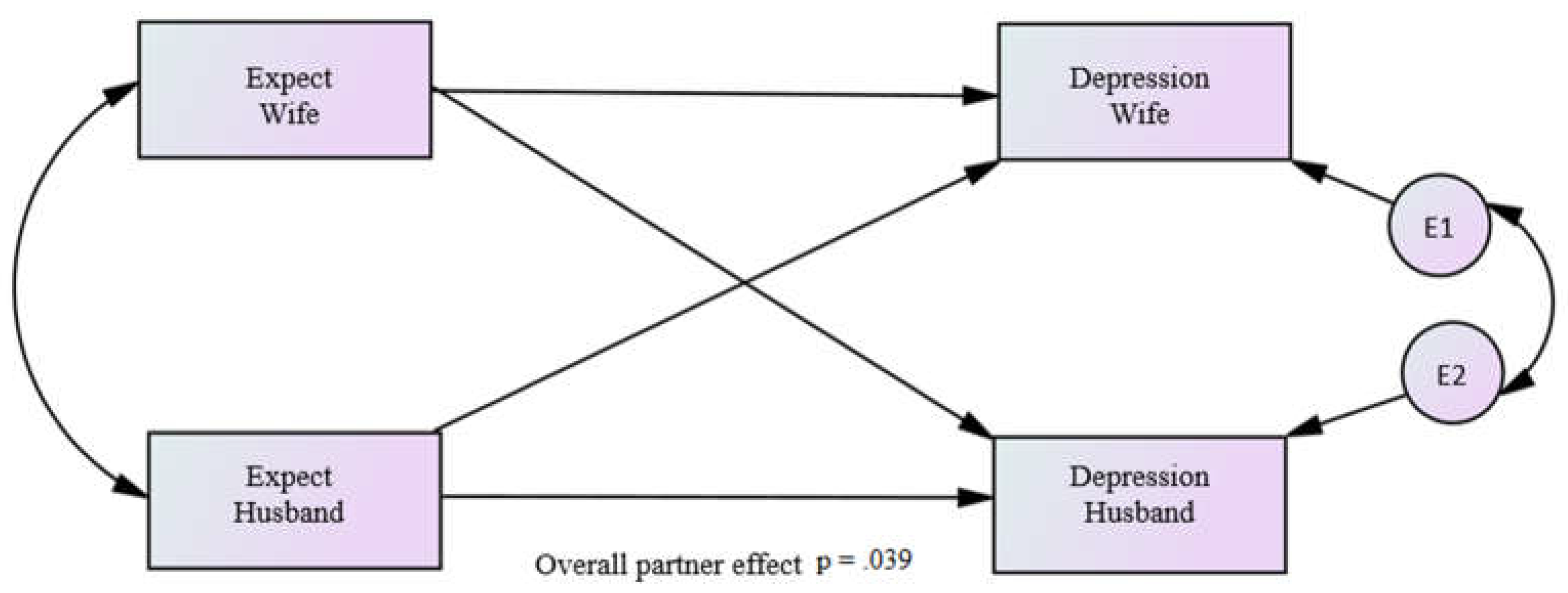
The focus of this study was the investigation of the effect of the expectation of having children, AG, NE, ENRICH and SES on depression. Both the effect of own expectation, AG, NE, ENRICH and SES (actor) and the effect of partner’s expectation, AG, NE, ENRICH and SES (partner) on depression were studied. Separate actor and partner effects were estimated for husbands(males) and wives(females), the dyad members being distinguishable by their sex. For the APIM analysis, there were a total of 148 dyads and 296 individuals with 4 individuals dropped from the analysis due to missing data on one or more variables with a total of 148 husbands and 148 wives. No other independent variables predicted depression, except for expectation of having children and neuroticism.
Regarding the expectation of having children, only the combined partner effect across both husbands and wives was significant (B= -0.323, p = .039). The standardized effect equaled -0.083 (r = -.126), which was considered a small effect size (
Figure 3).
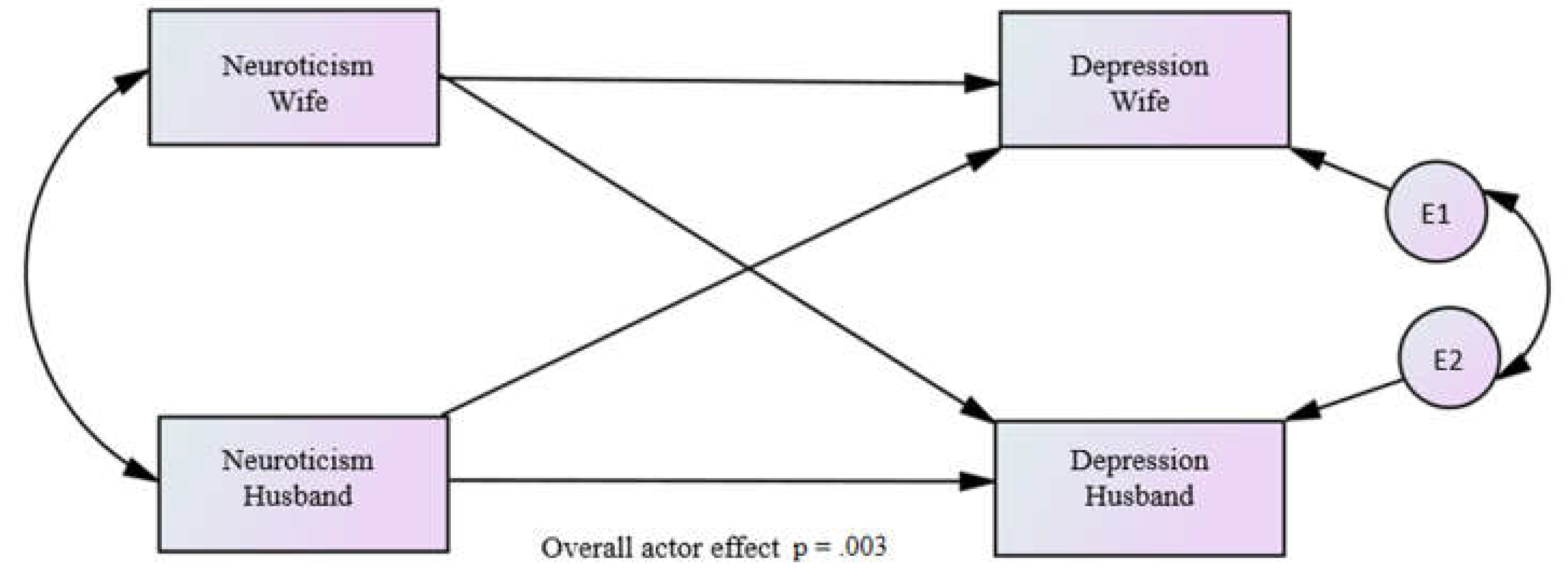
Regarding the variable of neuroticism, the combined actor effect across both husbands and wives equaled 0.092 and was statistically significant (p = .003) and the standardized effect equaled 0.166 (
r = .182 and a small effect size) (
Figure 4).
Regarding the variable of marital satisfaction, the combined actor effect across both Husbands and Wives equaled -0.022 and was statistically significant (p = .039). The standardized effect equaled -0.084 (
r = -.126), which was considered a small effect size (
Figure 5).
4. Discussion
The aim of this study was to determine the prevalence of depression and its associated factors in Thai infertile couples. In general, major depression symptoms were observed among infertile couples, even though it was not high. Unlike the other related study in India, in which the prevalence of depression was 58%, the current study revealed a lower rate of depression, at 6.7%. This may be attributed to the fact that the measurements. The present study used an outcome inventory and a self-report questionnaire, whereas the survey in India used the Hamilton Depression Rating Scale, a clinician-rated measurement [
41]. The measurement used by clinicians tends to detect the high rate of major depression rather than a self-reporting questionnaire[
42].
In line with the other related study, the current results indicated that women in couples undergoing infertility treatment had significantly higher stress, anxiety and depression scores than men[
43]. The same is true for neuroticism; our findings showed females have a higher level of neuroticism personality trait than males, and neuroticism was a strong predictor for depression [
44].
Interestingly, the expectation of having children was associated with decreased depression. It seems to be a positive rather than a negative variable. A related study showed that not having children is a risk factor for anxiety in women[
45]. We hypothesized that the fact that the expectation of having children was considered hope rather than stress because almost all participants were in the early phase of treatment. If the study is longitudinal, the expectation might become a stressor, especially for those who fail the treatment.
As expected, the sufficiency theory concept and marital satisfaction were negatively related to depression. However, neuroticism appeared to be the most potent factor for depression. This is to indicate that the intra-personal factor (personality trait-neuroticism) is more powerful than extra-personal factors.
In dyadic analysis, only three variables were predictors for depression. The actor effects were observed in marital satisfaction and neuroticism, whereas the partner effect (not actor effect) of having children was observed as a predictor for individual depression.
It is anticipated that marital satisfaction and neuroticism demonstrate to have an actor effect on depression endorsed by the related research[
45]. However, this is the first to report that the expectation (hope) of having children demonstrated the partner effect.
Clinical implication
From the present findings, some knowledge can be applied clinically. Expectations of having children should be cultivated, especially in the early phase of treatment, as it may be associated with a low incidence of depression. The personality trait of neuroticism, the strongest predictor, can be screened to prepare individuals to cope with stress or anxiety, especially when treatments are unexpectedly disappointing.
Limitations of the study
Some limitation of our research was that we invited infertile couples who sought treatment. Response and recall biases might occur because the data was collected with a self-administered questionnaire. The researchers considered social desirability bias that could occur as the participants were couples. The fact that we have not included questions about polygamy, religion and whether the couples have extramarital relationships. The cross-sectional nature of the research limited causal relationships of the outcome.
5. Conclusions
This study provided evidence of the prevalence of depression and the associated factors with depression in infertile couples. Intrapersonal factors such as neuroticism remain the strongest predictor for depression. Other related factors with infertility, i.e., marital satisfaction and expectation of having children, cannot be overlooked. Outcomes will raise awareness about mental health problems among infertile couples and guide future research for interventions—findings from our study benefit clinicians in identifying a case with such risk factors for anxiety and depression.
Author Contributions
Conceptualization, T.Y., N.W., T.W., U.S., C.S., R.J. and C.P.; methodology, T.Y., N.W., T.W., U.S., C.S., R.J. and C.P.; software, T.W.; validation, T.Y., N.W. and T.W; formal analysis, T.Y., N.W. and T.W.; investigation, T.Y., N.W. and U.S.; resources, T.Y., N.W., T.W., C.S., U.S., R.J. and C.P.; data curation, T.Y., N.W. and T.W.; writing—original draft preparation, T.Y., N.W. and T.W.; writing—review and editing, T.Y., N.W., T.W., C.S., U.S., R.J. and C.P.; visualization, T.Y., N.W. and T.W; supervision, N.W. and U.S.; project administration, N.W. and T.W.; funding acquisition, T.Y., N.W. and T.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the research ethics committee of the Faculty of Medicine, Chiang Mai University (protocol code: PSY-2565-09017)
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Faculty of Medicine, Chiang Mai University (protocol code: PSY-2565-09017 and date of approval, June 20, 2022)
Informed Consent Statement
All patients provided written informed consent to the study.
Data Availability Statement
Data not applicable.
Acknowledgments
We thank the Graduate School of Chiang Mai University for providing T.Y. with the Teaching assistant/Research assistant (TA/RA) Scholarship for 2021–2023.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Infertility. Available online: https://www.who.int/news-room/fact-sheets/detail/infertility (accessed on 11 July 2022).
- Center for Disease Control. Infertility. Available online: https://www.cdc.gov/reproductivehealth/infertility/index.htm (accessed on 11 July 2022).
- Babakhanzadeh, E.; Nazari, M.; Ghasemifar, S.; Khodadadian, A. Some of the Factors Involved in Male Infertility: A Prospective Review. Int. J. Gen. Med. 2020, 13, 29–41. [Google Scholar] [CrossRef]
- Kumar, N.; Singh, A.K. Trends of male factor infertility, an important cause of infertility: A review of literature. J. Hum. Reprod. Sci. 2015, 8, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Fainberg, J.; Kashanian, J.A. Recent advances in understanding and managing male infertility. F1000Research 2019, 8, 670. [Google Scholar] [CrossRef] [PubMed]
- Carson, S.A.; Kallen, A.N. Diagnosis and management of infertility: a review. JAMA 2021, 326, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Read, J. Sexual problems associated with infertility, pregnancy, and ageing. BMJ 2004, 329, 559–561. [Google Scholar] [CrossRef] [PubMed]
- Lei, A.; You, H.; Luo, B.; Ren, J. The associations between infertility-related stress, family adaptability and family cohesion in infertile couples. Sci. Rep. 2021, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mascarenhas, M.N.; Flaxman, S.R.; Boerma, T.; Vanderpoel, S.; Stevens, G.A. National, Regional, and Global Trends in Infertility Prevalence Since 1990: A Systematic Analysis of 277 Health Surveys. PLOS Med. 2012, 9, e1001356. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, K.; Huo, Y.; Zhou, M. The effect of infertility-related stress on Chinese infertile females’ mental health: The moderating role of marital adjustment. PsyCh J. 2019, 8, 232–239. [Google Scholar] [CrossRef]
- Dong, M.; Xu, X.; Li, Y.; Wang, Y.; Jin, Z.; Tan, J. Impact of infertility duration on female sexual health. Reprod. Biol. Endocrinol. 2021, 19, 1–10. [Google Scholar] [CrossRef]
- Thable, A.M.; Duff, E.P.; Dika, C.M. Infertility management in primary care. Nurse Pr. 2020, 45, 48–54. [Google Scholar] [CrossRef]
- Tendais, I.; Figueiredo, B. Parents’ anxiety and depression symptoms after successful infertility treatment and spontaneous conception: does singleton/twin pregnancy matter? Hum Reprod, 2016, 31, 2303–12. [Google Scholar] [CrossRef]
- Rich, C.W.; Domar, A.D. Addressing the emotional barriers to access to reproductive care. Fertil. Steril. 2016, 105, 1124–1127. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Altuwirqi, M.H.; Bukhari, M.; Abotalib, Z.; BinSalehc, S. Psychiatric disorders among infertile men and women attending three infertility clinics in Riyadh, Saudi Arabia. Ann. Saudi Med. 2015, 35, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Maroufizadeh, S.; Karimi, E.; Vesali, S.; Samani, R.O. Anxiety and depression after failure of assisted reproductive treatment among patients experiencing infertility. Int. J. Gynecol. Obstet. 2015, 130, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Yoldemir, T.; Yassa, M.; Atasayan, K. Comparison of depression between primary and secondary infertile couples. Gynecol. Endocrinol. 2020, 36, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- SRD. Average monthly income per household in Thailand from 2004 to 2020. Available online: https://www.statista.com/statistics/1030185/thailand-average-monthly-income-per-household/ (accessed on 11 July 2022).
- Assanangkornchai, S.; Nontarak, J.; Aekplakorn, W.; Chariyalertsak, S.; Kessomboon, P.; Taneepanichskul, S. Socio-economic inequalities in the association between alcohol use disorder and depressive disorder among Thai adults: a population-based study. BMC Psychiatry 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Karaca, N.; Karabulut, A.; Ozkan, S.; Aktun, H.; Orengul, F.; Yilmaz, R.; Ates, S.; Batmaz, G. Effect of IVF failure on quality of life and emotional status in infertile couples. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 206, 158–163. [Google Scholar] [CrossRef]
- Agostini, F.; Monti, F.; Paterlini, M.; Andrei, F.; Palomba, S.; La Sala, G.B. Effect of the previous reproductive outcomes in subfertile women after in vitro fertilization (IVF) and/or intracytoplasmic sperm injection (ICSI) treatments on perinatal anxious and depressive symptomatology. J. Psychosom. Obstet. Gynecol. 2018, 39, 29–37. [Google Scholar] [CrossRef]
- Gdańska, P.; Drozdowicz-Jastrzębska, E.; Grzechocińska, B.; Radziwon-Zaleska, M.; Węgrzyn, P.; Wielgoś, M. Anxiety and depression in women undergoing infertility treatment. Ginekol. Polska 2017, 88, 109–112. [Google Scholar] [CrossRef]
- Mojtabai, R.; Stuart, E.A.; Hwang, I.; Eaton, W.W.; Sampson, N.; Kessler, R.C. Long-term effects of mental disorders on marital outcomes in the National Comorbidity Survey ten-year follow-up. Chest 2017, 52, 1217–1226. [Google Scholar] [CrossRef]
- Williams, K.; Frech, A.; Carlson, D.L. Marital status and mental health. A handbook for the study of mental health: Social contexts, theories, and systems. 2010, 306–320. [Google Scholar]
- Kövi, Z.; Wongpakaran, T.; Wongpakaran, N.; Kuntawong, P.; Berghauer-Olasz, E.; Mirnics, Z. Relationship between Personality Traits and the Inner Strengths. Psychiatr Danub 2021, 33, 844–849. [Google Scholar] [PubMed]
- Wongpakaran, N.; Wongpakaran, T.; Wedding, D.; Mirnics, Z.; Kövi, Z. Role of Equanimity on the Mediation Model of Neuroticism, Perceived Stress and Depressive Symptoms. Healthcare 2021, 9, 1300. [Google Scholar] [CrossRef] [PubMed]
- Tola, E.N.; Yalcin, S.E.; Dugan, N.; Oral, B. The association of type D personality and depression with infertility in women. J. Psychosom. Obstet. Gynecol. 2020, 41, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Halladay, J.E.; et al. Cannabis Use as a Risk Factor for Depression, Anxiety, and Suicidality: Epidemiological Associations and Implications for Nurses. J Addict Nurs 2020, 31, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.C.; Patte, K.A.; Ferro, M.A.; Leatherdale, S.T. Associations between Longitudinal Patterns of Substance Use and Anxiety and Depression Symptoms among a Sample of Canadian Secondary School Students. Int. J. Environ. Res. Public Heal. 2021, 18, 10468. [Google Scholar] [CrossRef] [PubMed]
- Murthy, P.; Mahadevan, J.; Chand, P.K. Treatment of substance use disorders with co-occurring severe mental health disorders. Curr. Opin. Psychiatry 2019, 32, 293–299. [Google Scholar] [CrossRef]
- Brook, D.W.; Brook, J.S.; Zhang, C.; Cohen, P.; Whiteman, M. Drug Use and the Risk of Major Depressive Disorder, Alcohol Dependence, and Substance Use Disorders. Arch. Gen. Psychiatry 2002, 59, 1039–1044. [Google Scholar] [CrossRef]
- Mongsawad, P. The philosophy of the sufficiency economy: a contribution to the theory of development. APDJ 2012, 17, 123. [Google Scholar] [CrossRef]
- Barua, P.; Tejativaddhana, P. Impact of application of sufficiency economy philosophy on the well-being of Thai population: A systematic review and meta-analysis of relevant studies. ournal of Population and Social Studies 2019, 27, 195–219. [Google Scholar] [CrossRef]
- Stratton, S.J. Population Research: Convenience Sampling Strategies. Prehospital Disaster Med. 2021, 36, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, N.; Wongpakaran, T.; Kövi, Z. Development and validation of 21-item outcome inventory (OI-21). Heliyon 2022, 8, e09682. [Google Scholar] [CrossRef] [PubMed]
- Aluja, A.; Kuhlman, M.; Zuckerman, M. Development of the Zuckerman–Kuhlman–Aluja personality questionnaire (ZKA–PQ): A factor/facet version of the Zuckerman–Kuhlman personality questionnaire (ZKPQ). Journal of personality assessment 2010, 92, 416–431. [Google Scholar] [CrossRef] [PubMed]
- Fowers, B.J.; Olson, D.H. ENRICH Marital Satisfaction Scale: A brief research and clinical tool. Journal of Family psychology 1993, 7, 176. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T. Sufficiency Economy Scale. Available online: http://www.pakaranhome.com/index.php?lay=show&ac=article&Id=2147626282 (accessed on 11 July 2022).
- Kenny, D.A.; Ledermann, T. Detecting, measuring, and testing dyadic patterns in the actor-partner interdependence model. J Fam Psychol, 2010, 24, 359–66. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol Bull 1992, 112, 155–9. [Google Scholar] [CrossRef]
- Dadhwal, V.; et al. Depression, anxiety, quality of life and coping in women with infertility: A cross-sectional study from India. Int J Gynaecol Obstet, 2022, 158, 671–678. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T.; Wannarit, K.; Saisavoey, N.; Pinyopornpanish, M.; Lueboonthavatchai, P.; Apisiridej, N.; Ruktrakul, T.; Srichan, R.; Satthapisit, S.; et al. Level of agreement between self-rated and clinician-rated instruments when measuring major depressive disorder in the Thai elderly: a 1-year assessment as part of the THAISAD study. Clin. Interv. Aging 2014, 9, 377–382. [Google Scholar] [CrossRef]
- Abdishahshahani, M.; Torabi, M.; Kazemi, A. Investigating related factors to psychological symptoms of infertile couples undergoing assisted reproductive treatment. J Educ Health Promot 2020, 9, 21. [Google Scholar]
- Shokrkon, A.; Nicoladis, E. How personality traits of neuroticism and extroversion predict the effects of the COVID-19 on the mental health of Canadians. PLOS ONE 2021, 16, e0251097. [Google Scholar] [CrossRef]
- Zhang, L.; Shao, H.; Huo, M.; Chen, J.; Tao, M.; Liu, Z. Prevalence and associated risk factors for anxiety and depression in infertile couples of ART treatment: a cross-sectional study. BMC Psychiatry 2022, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).