Submitted:
12 May 2023
Posted:
15 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Ethics Approval
2.3. Consultation Models
2.4. Variables
2.5. Statistics
3. Results
3.1. Sample Overview and Outcomes
3.2. Outcomes after E-Consultation Implementation
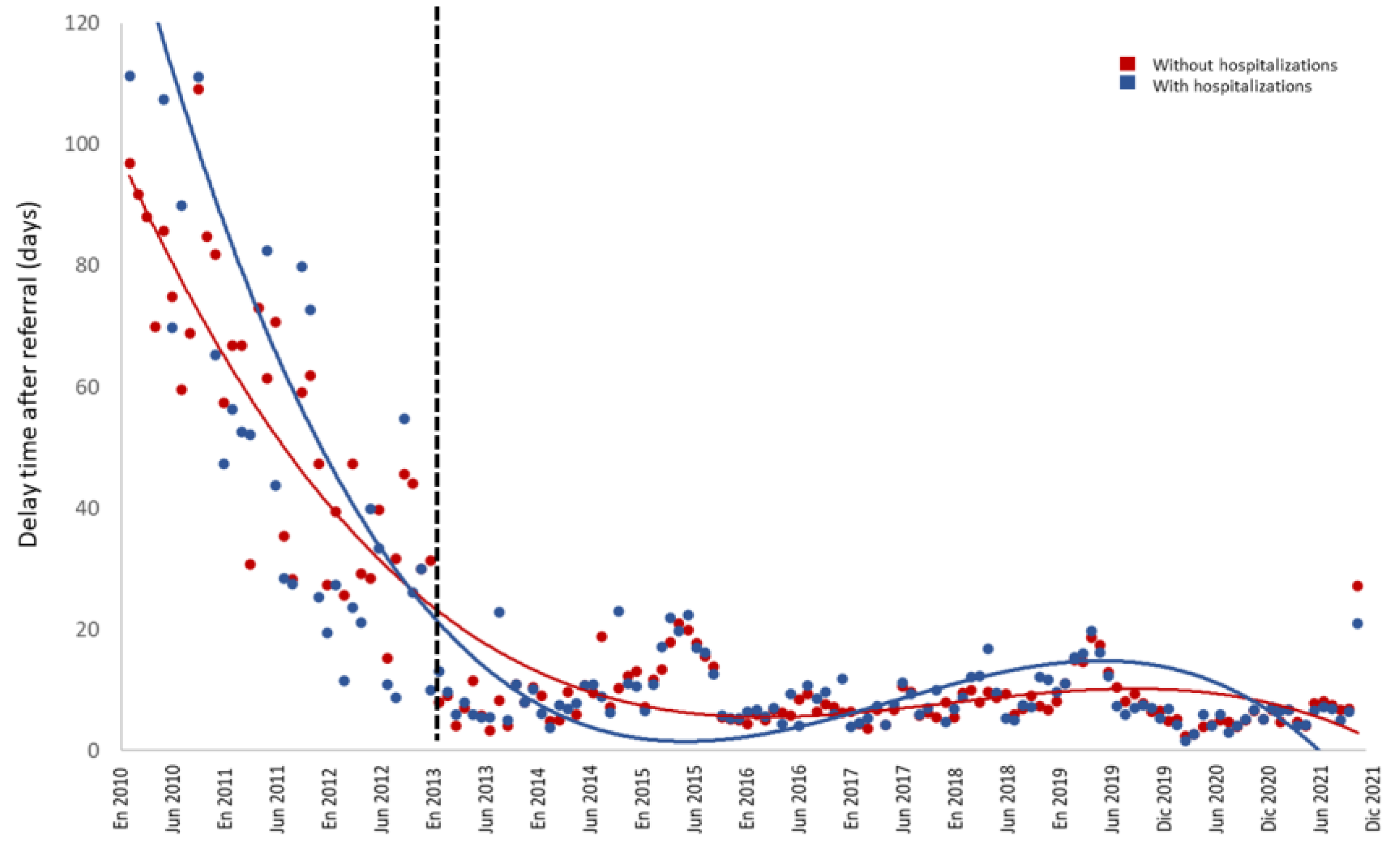
3.2.1. Delay from PCP Referral to Cardiology Consultation
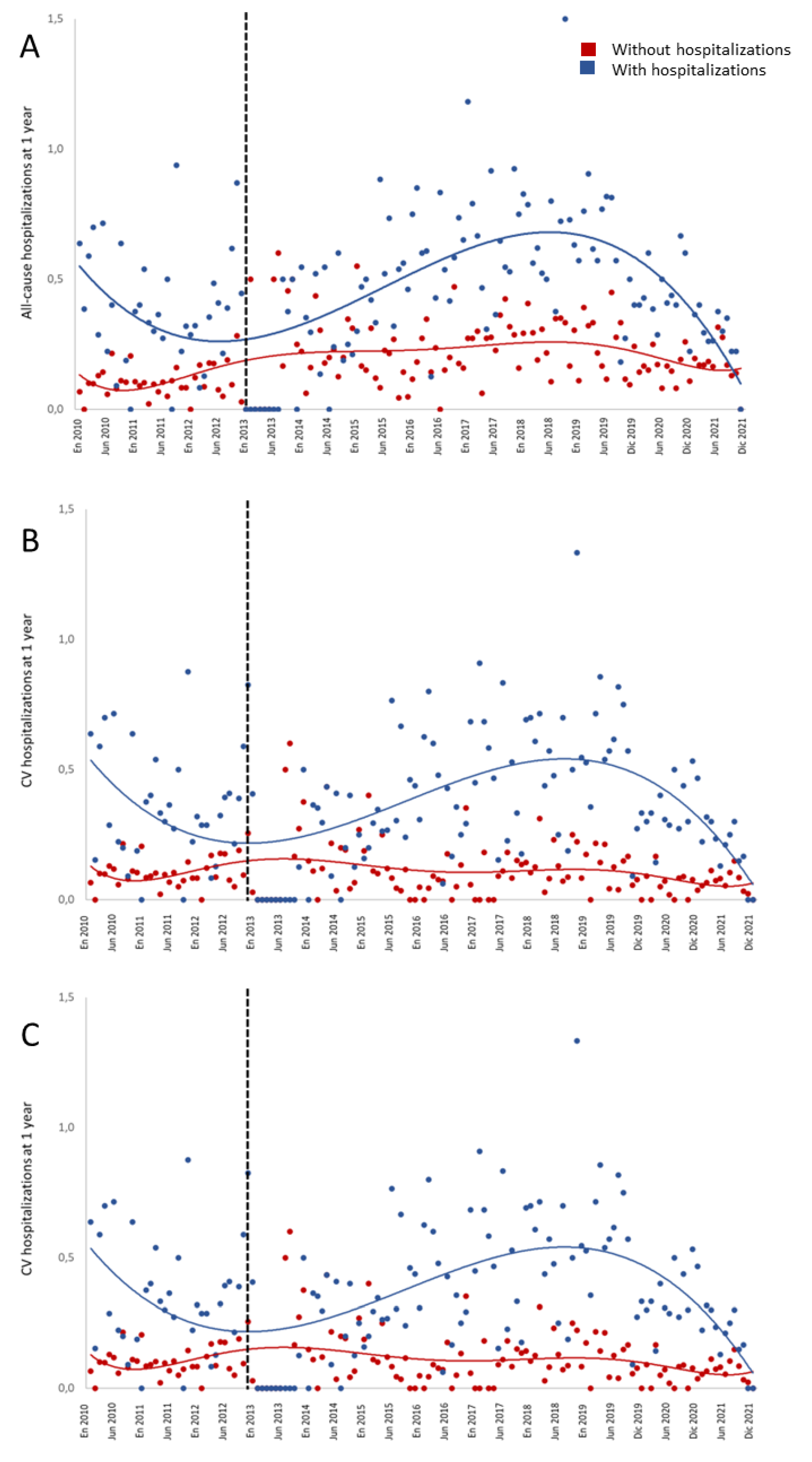
3.2.2. Hospital Admissions at 1-Year After Consultation
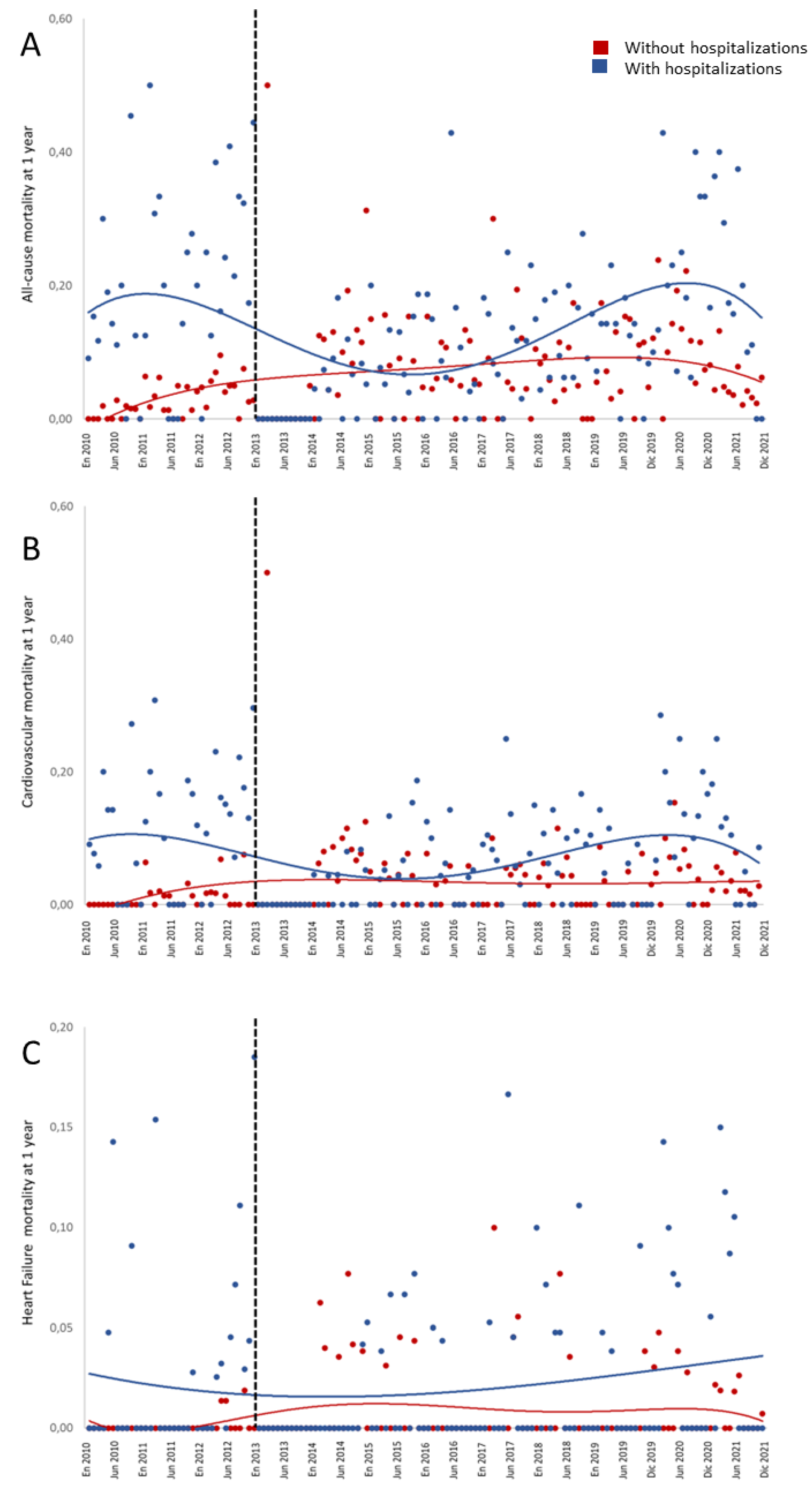
3.2.3. Mortality at 1-Year After Consultation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur Heart J 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Comin-Colet, J.; Calero-Molina, E.; Corbella, X.; Muñiz, J.; San Saturnino, M.; Ibarrola, C.; Comín-Colet, J.; Alcober, L.; Calero-Molina, E.; Cobo, M.; et al. Recomendaciones Para Desarrollar Modelos Asistenciales de Atención al Paciente Con Insuficiencia Cardiaca (Proyecto MAIC): Estudio Delphi. J Healthc Qual Res 2022, 37, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.; Enjuanes, C.; Calero-Molina, E.; Hidalgo, E.; José, N.; Calvo, E.; Verdú-Rotellar, J.M.; Garcimartín, P.; Chivite, D.; Formiga, F.; et al. Effectiveness of Telemedicine in Patients with Heart Failure According to Frailty Phenotypes: Insights from the ICOR Randomised Controlled Trial. Eur J Intern Med 2022, 96, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.; Enjuanes, C.; Calero-Molina, E.; Hidalgo, E.; José-Bazán, N.; Ruiz, M.; Verdú-Rotellar, J.M.; Garcimartín, P.; Jiménez-Marrero, S.; Garay, A.; et al. Usefulness of Telemedicine-Based Heart Failure Monitoring According to ‘EHealth Literacy’ Domains: Insights from the ICOR Randomized Controlled Trial. Eur J Intern Med 2022, 101, 56–67. [Google Scholar] [CrossRef]
- González-Franco, Á.; Cerqueiro González, J.M.; Arévalo-Lorido, J.C.; Álvarez-Rocha, P.; Carrascosa-García, S.; Armengou, A.; Guzmán-García, M.; Trullàs, J.C.; Montero-Pérez-Barquero, M.; Manzano, L. Morbidity and Mortality in Elderly Patients with Heart Failure Managed with a Comprehensive Care Model vs. Usual Care: The UMIPIC Program. Revista Clínica Española (English Edition) 2022, 222, 123–130. [Google Scholar] [CrossRef]
- Jackevicius, C.A.; de Leon, N.K.; Lu, L.; Chang, D.S.; Warner, A.L.; Mody, F.V. Impact of a Multidisciplinary Heart Failure Post-Hospitalization Program on Heart Failure Readmission Rates. Annals of Pharmacotherapy 2015, 49, 1189–1196. [Google Scholar] [CrossRef]
- Tuckson, R. V; Edmunds, M.; Hodgkins, M.L. Telehealth. New England Journal of Medicine 2017, 377, 1585–1592. [Google Scholar] [CrossRef]
- Rey-Aldana, D.; Cinza-Sanjurjo, S.; Portela-Romero, M.; López-Barreiro, J.L.; Garcia-Castelo, A.; Pazos-Mareque, J.M.; Mazón-Ramos, P.; González-Juanatey, J.R. Programa de Consulta Electrónica Universal (e-Consulta) de Un Servicio de Cardiología. Resultados a Largo Plazo. Rev Esp Cardiol 2022, 75, 159–165. [Google Scholar] [CrossRef]
- Cinza Sanjurjo, S.; Mazón Ramos, P.; Iglesias Álvarez, D.; Rey Aldana, D.; Portela Romero, M.; González-Juanatey, J.R. Consulta Electrónica (e-Consulta) Para Pacientes Con Insuficiencia Cardiaca. Resultados a Largo Plazo. Rev Esp Cardiol 2022, 75, 93–95. [Google Scholar] [CrossRef]
- Mazón-Ramos, P.; Cinza-Sanjurjo, S.; Garcia-Vega, D.; Portela-Romero, M.; Sanmartin-Pena, J.C.; Rey-Aldana, D.; Martínez Monzonís, A.; Espasandín-Domínguez, J.; Gude-Sampedro, F.; González-Juanatey, J.R. A Clinician-to-Clinician Universal Electronic Consultation Programme at the Cardiology Department of a Galician Healthcare Area Improves Healthcare Accessibility and Outcomes in Elderly Patients. European Heart Journal - Digital Health 2023. [Google Scholar] [CrossRef]
- Rey-Aldana, D.; Mazón-Ramos, P.; Portela-Romero, M.; Cinza-Sanjurjo, S.; Alvarez-Alvarez, B.; Agra-Bermejo, R.; Rigueiro-Veloso, P.; Espasandín-Domínguez, J.; Gude-Sampedro, F.; González-Juanatey, J.R. Longer-Term Results of a Universal Electronic Consultation Program at the Cardiology Department of a Galician Healthcare Area. Circ Cardiovasc Qual Outcomes 2022, 15, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Alcoberro, L.; Moliner, P.; Vime, J.; Jiménez-Marrero, S.; Garay, A.; Yun, S.; Pons-Riverola, A.; Ramos-Polo, R.; Ras-Jiménez, M.; Tajes, M.; et al. Breaking the 30-Day Barrier: Long-Term Effectiveness of a Nurse-Led 7-Step Transitional Intervention Program in Heart Failure. PLoS One 2023, 18, e0279815. [Google Scholar] [CrossRef] [PubMed]
- Van Spall, H.G.C.; Lee, S.F.; Xie, F.; Oz, U.E.; Perez, R.; Mitoff, P.R.; Maingi, M.; Tjandrawidjaja, M.C.; Heffernan, M.; Zia, M.I.; et al. Effect of Patient-Centered Transitional Care Services on Clinical Outcomes in Patients Hospitalized for Heart Failure. JAMA 2019, 321, 753. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Bailón, M.; Comín-Colet, J. Towards a Comprehensive and Multidisciplinary Care in Heart Failure. Revista Clínica Española (English Edition) 2022, 222, 174–175. [Google Scholar] [CrossRef] [PubMed]
- Baecker, A.; Meyers, M.; Koyama, S.; Taitano, M.; Watson, H.; Machado, M.; Nguyen, H.Q. Evaluation of a Transitional Care Program After Hospitalization for Heart Failure in an Integrated Health Care System. JAMA Netw Open 2020, 3, e2027410. [Google Scholar] [CrossRef]
- Krzesiński, P.; Jankowska, E.A.; Siebert, J.; Galas, A.; Piotrowicz, K.; Stańczyk, A.; Siwołowski, P.; Gutknecht, P.; Chrom, P.; Murawski, P.; et al. Effects of an Outpatient Intervention Comprising Nurse-led Non-invasive Assessments, Telemedicine Support and Remote Cardiologists’ Decisions in Patients with Heart Failure (AMULET Study): A Randomised Controlled Trial. Eur J Heart Fail 2022, 24, 565–577. [Google Scholar] [CrossRef]
- Lawson, C.A.; Lam, C.; Jaarsma, T.; Kadam, U.; Stromberg, A.; Ali, M.; Tay, W.T.; Clayton, L.; Khunti, K.; Squire, I. Developing a Core Outcome Set for Patient-Reported Symptom Monitoring to Reduce Hospital Admissions for Patients with Heart Failure. European Journal of Cardiovascular Nursing 2022, 21, 830–839. [Google Scholar] [CrossRef]
- Salzano, A.; D’Assante, R.; Stagnaro, F.M.; Valente, V.; Crisci, G.; Giardino, F.; Arcopinto, M.; Bossone, E.; Marra, A.M.; Cittadini, A. Heart Failure Management during the COVID-19 Outbreak in Italy: A Telemedicine Experience from a Heart Failure University Tertiary Referral Centre. Eur J Heart Fail 2020, 22, 1048–1050. [Google Scholar] [CrossRef]
- Sammour, Y.; Spertus, J.A.; Austin, B.A.; Magalski, A.; Gupta, S.K.; Shatla, I.; Dean, E.; Kennedy, K.F.; Jones, P.G.; Nassif, M.E.; et al. Outpatient Management of Heart Failure During the COVID-19 Pandemic After Adoption of a Telehealth Model. JACC Heart Fail 2021, 9, 916–924. [Google Scholar] [CrossRef]
- Xu, H.; Granger, B.B.; Drake, C.D.; Peterson, E.D.; Dupre, M.E. Effectiveness of Telemedicine Visits in Reducing 30-Day Readmissions Among Patients With Heart Failure During the COVID-19 Pandemic. J Am Heart Assoc 2022, 11. [Google Scholar] [CrossRef]
- Yun, S.; Enjuanes, C.; Calero, E.; Hidalgo, E.; Cobo, M.; Llàcer, P.; García-Pinilla, J.M.; González-Franco, Á.; Núñez, J.; Morales-Rull, J.L.; et al. Study Design of Heart Failure Events Reduction with Remote Monitoring and EHealth Support (HERMeS). ESC Heart Fail 2020, 7, 4448–4457. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Marrero, S.; Yun, S.; Cainzos-Achirica, M.; Enjuanes, C.; Garay, A.; Farre, N.; Verdú, J.M.; Linas, A.; Ruiz, P.; Hidalgo, E.; et al. Impact of Telemedicine on the Clinical Outcomes and Healthcare Costs of Patients with Chronic Heart Failure and Mid-Range or Preserved Ejection Fraction Managed in a Multidisciplinary Chronic Heart Failure Programme: A Sub-Analysis of the ICOR Randomized Trial. J Telemed Telecare 2020, 26, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Silva-Cardoso, J.; Juanatey, J.R.G.; Comin-Colet, J.; Sousa, J.M.; Cavalheiro, A.; Moreira, E. The Future of Telemedicine in the Management of Heart Failure Patients. Card Fail Rev 2021, 7. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, A.; Cartledge, S. The Effect of Telemedicine in Heart Failure Based on Frailty Phenotypes. Eur J Intern Med 2022, 96, 44–45. [Google Scholar] [CrossRef]
- Mazón-Ramos, P.; Cinza-Sanjurjo, S.; Garcia-Vega, D.; Portela-Romero, M.; Rodríguez-Mañero, M.; Rey-Aldana, D.; Morandeira, A.P.; Lage-Fernández, R.; Gude-Sampedro, F.; González-Juanatey, J.R. The Impact of Inter-clinician Electronic Consultation in Patients Diagnosed with Atrial Fibrillation in Primary Care. Eur J Clin Invest 2023, 53. [Google Scholar] [CrossRef]
| Total | Without previous hospitalizations | With previous hospitalizations | p | |
|---|---|---|---|---|
| 6,444 | 4,214 | 2,230 | ||
| Agea (years) | 77.7 (9.7) | 77.6 (9.7) | 77.9 (9.8) | 0.267 |
| Women (%) | 49.6% | 51.5% | 46.0% | <0.001 |
| Comorbidities | ||||
| Arterial hypertension (%) | 78.8% | 79.7% | 77.0% | 0.013 |
| Diabetes mellitus (%) | 34.5% | 31.1% | 40.9% | <0.001 |
| Ischemic heart disease (%) | 20.7% | 19.9% | 22.2% | 0.036 |
| Atrial fibrillation (%) | 44.9% | 46.3% | 42.2% | 0.002 |
| Cerebrovascular disease (%) | 8.5% | 8.3% | 8.9% | 0.380 |
| Peripheral arterial disease (%) | 7.3% | 6.7% | 8.5% | 0.008 |
| Consultation model. Periods | <0.001 | |||
| In-person consultation | 35.6% | 40.3% | 26.9% | |
| e-Consult | 64.4% | 59.7% | 73.1% | |
| E-consultation resolution | ||||
| e-consult solves (%) | 17.7% | 17.0% | 18.8% | 0.171 |
| 1 single-act consultation (%) | 39.7% | 39.8% | 39.6% | |
| Follow-up visits (%) | 42.6% | 43.2% | 41.6% | |
| Delay to in-person consultation | ||||
| Time to answera (days) | 25.0 (53.5) | 27.2 (53.9) | 21.0 (52.5) | <0.001 |
| <8 days (%) | 50.3% | 46.4% | 57.7% | <0.001 |
| 8-14 days (%) | 16.0% | 16.0% | 15.9% | |
| 15-30 days (%) | 16.1% | 17.5% | 13.5% | |
| >30 days (%) | 17.6% | 20.0% | 13.0% | |
| Healthcare activity | ||||
| Cardiovascular testa,b | 1.56 (2.29) | 1.52 (2.29) | 1.63 (2.29) | 0.053 |
| Emergency department consultationsa,b (1-year) | 3.7 (5.8) | 3.92 (6.21) | 3.21 (5.06) | <0.001 |
| Emergency department consultationsb (%) | 69.7% | 68.1% | 72.9% | <0.001 |
| Hospitalizationsb | ||||
| All-cause hospitalizationsb (%) | 22.0% | 15.2% | 34.9% | <0.001 |
| CV hospitalizationsb (%) | 14.9% | 8.3% | 27.3% | <0.001 |
| HF-related hospitalizationsb (%) | 9.3% | 2.4% | 22.4% | <0.001 |
| Deathsb | ||||
| All-cause deathsb (%) | 9.4% | 6.3% | 15.2% | <0.001 |
| CV deathsb (%) | 4.8% | 2.8% | 8.6% | <0.001 |
| HF-related deathsb (%) | 1.3% | 0.7% | 2.5% | <0.001 |
| Death causesc | ||||
| Ischemic cardiopathy (%) | 10.2% | 9.9% | 10.6% | <0.001 |
| HF (%) | 14.2% | 12.2% | 16.5% | |
| Cancer (%) | 11.5% | 14.6% | 7.9% | |
| Valvulopathy (%) | 4.7% | 4.7% | 4.6% | |
| Ischemic stroke (%) | 3.2% | 3.1% | 3.2% | |
| COPD (%) | 4.1% | 4.7% | 3.4% | |
| Chronic kidney disease (%) | 1.6% | 2.3% | 0.7% | |
| Respiratory infection (%) | 2.2% | 2.1% | 2.4% | |
| Atrial Fibrillacion (%) | 3.3% | 3.1% | 3.6% | |
| Haemorrhagic stroke (%) | 0.9% | 0.8% | 1.1% | |
|
aMean ± (standard deviation). b1st year after the e-consultation. cPercentages over the total number of deaths. dStatistics: chi-square test, statistical significance at p<0.05. CV: cardiovascular; HF: heart failure; COPD: chronic obstructive pulmonary disease | ||||
| HF-r hospitalization | CV hospitalization | All-cause hospitalization | HF-r mortality | CV mortality | All-cause mortality | ||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Age | 1.01 (1.00-1.02) | 0.999 (0.992-1.007) | 1.00 (0.99-1.01) | 1.12 (1.09-1.16) | 1.08 (1.06-1.09) | 1.07 (1.06-1.09) | |
| Gender (men) | 1.26 (1.05-1.52) | 1.17 (1.01-1.35) | 1.15 (1.01-1.30) | 0.99 (0.64-1.56) | 1.14 (0.89-1.46) | 1.58 (1.31-1.89) | |
| Comorbidities | |||||||
| Arterial hypertension | 0.77 (0.62-0.96) | 0.83 (0.70-0.98) | 0.86 (0.74-0.99) | 0.65 (0.40-1.08) | 0.81 (0.61-1.07) | 0.66 (0.54-0.88) | |
| Diabetes mellitus | 0.89 (0.74-1.08) | 1.08 (0.93-1.25) | 1.09 (0.96-1.25) | 1.25 (0.78-2.01) | 0.99 (0.77-1.29) | 0.99 (0.82-1.19) | |
| Ischemic cardiopathy | 1.11 (0.89-1.38) | 1.40 (1.18-1.66) | 1.18 (1.02-1.37) | 0.70 (0.39-1.28) | 1.14 (0.85-1.52) | 1.13 (0.91-1.40) | |
| Atrial fibrillation | 1.24 (1.03-1.48) | 1.02 (0.88-1.18) | 0.97 (0.86-1.10) | 0.83 (0.53-1.30) | 0.78 (0.61-0.99) | 0.81 (0.68-0.97) | |
| Cerebrovascular disease | 0.87 (0.63-1.21) | 1.23 (0.96-1.16) | 1.19 (0.96-1.48) | 1.48 (0.77-2.87) | 1.03 (0.68-1.55) | 0.86 (0.63-1.19) | |
| Peripheral arterial disease | 0.98 (0.70-1.37) | 0.95 (0.72-1.24) | 1.05 (0.83-1.32) | 1.48 (0.69-3.20) | 1.67 (1.12-2.50) | 1.49 (1.09-2.03) | |
| HF-related previous hospitalizations | |||||||
| Without hospitalizations | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| With hospitalizations | 11.97 (9.54-15.01) | 4.05 (3.50-4.70) | 2.69 (2.38-3.05) | 3.32 (2.11-5.23) | 3.11 (2.44-3.95) | 2.60 (2.18-3.11) | |
| Cardiology assitance | |||||||
| Emergency assistance | 1.05 (1.03-1.07) | 1.04 (1.03-1.05) | 1.05 (1.03-1.06) | 0.96 (0.89-1.03) | 0.89 (0.85-0.93) | 0.92 (0.89-0.95) | |
| Delay time | |||||||
| 0-7 days (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 8-14 days | 1.23 (1.01-1.49) | 1.18 (1.01-1.37) | 1.13 (0.99-1.30) | 2.76 (1.60-4.77) | 2.04 (1.57-2.66) | 1.81 (1.49-2.20) | |
| 15-30 days | 0.93 (0.68-1.26) | 1.02 (0.80-1.30) | 1.12 (0.91-1.38) | 2.19 (0.89-5.39) | 1.62 (1.05-2.51) | 1.60 (1.18-2.18) | |
| >30 days | 1.04 (0.72-1.49) | 1.09 (0.82-1.44) | 1.13 (0.87-1.46) | 1.83 (0.51-6.50) | 1.07 (0.62-1.82) | 1.22 (0.84-1.79) | |
| Assitance model | |||||||
| Econsult (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| In-person consultation | 1.24 (0.96-1.61) | 1.20 (0.97-1.48) | 2.53 (2.11-3.11) | 0.61 (0.34-1.11) | 0.36 (0.26-0.50) | 0.44 (0.34-0.56) | |
|
In bold: statistically significant factors (p<0.05) Abbrevations: OR: odds ratio; CI: confidence interval; CV, cardiovascular; HF, heart failure; HF-r, heart failure-related |
|||||||
| HF-r hospitalization | CV hospitalization | All-cause hospitalization | HF-r mortality | CV mortality | All-cause mortality | ||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Age | 1.01 (1.00-1.02) | 1.00 (0.99-1.01) | 1.00 (0.99-1.01) | 1.16 (1.11-1.22) | 1.07 (1.05-1.09) | 1.07 (1.05-1.09) | |
| Gender (men) | 1.09 (0.89-1.35) | 1.03 (0.85-1.26) | 1.02 (0.85-1.23) | 1.09 (0.62-1.91) | 1.04 (0.76-1.43) | 1.48 (1.15-1.92) | |
| Comorbidities | |||||||
| Arterial hypertension | 0.84 (0.66-1.08) | 0.85 (0.68-1.07) | 0.79 (0.64-0.99) | 0.73 (0.38-1.39) | 0.88 (0.61-1.28) | 0.69 (0.52-0.93) | |
| Diabetes mellitus | 0.75 (0.60-0.93) | 0.84 (0.68-1.02) | 0.89 (0.73-1.07) | 1.29 (0.71-2.32) | 1.02 (0.73-1.42) | 0.88 (0.67-1.14) | |
| Ischemic cardiopathy | 1.08 (0.84-1.38) | 1.30 (1.03-1.63) | 1.20 (0.97-1.49) | 0.64 (0.30-1.36) | 1.12 (0.77-1.63) | 1.18 (0.88-1.58) | |
| Atrial fibrillation | 1.26 (1.02-1.55) | 1.09 (0.90-1.33) | 1.02 (0.85-1.22) | 0.77 (0.43-1.36) | 0.65 (0.47-0.91) | 0.81 (0.63-1.05) | |
| Cerebrovascular disease | 0.99 (0.70-1.42) | 1.07 (0.77-1.49) | 1.23 (0.90-1.67) | 1.09 (0.45-2.68) | 0.76 (0.43-1.34) | 0.79 (0.51-1.23) | |
| Peripheral arterial disease | 1.01 (0.69-1.46) | 0.91 (0.64-1.29) | 0.99 (0.72-1.36) | 1.40 (0.52-3.76) | 1.65 (0.99-2.75) | 1.63 (1.08-2.46) | |
| Cardiology assitance | |||||||
| Emergency assistance (1 year) | 1.06 (1.04-1.08) | 1.05 (1.03-1.08) | 2.33 (1.77-3.07) | 0.97 (0.89-1.05) | 0.92 (0.88-0.96) | 0.93 (0.89-0.95) | |
| Delay time | |||||||
| 0-7 days (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 8-14 days | 1.36 (1.09-1.69) | 1.32 (1.08-1.62) | 1.23 (1.01-1.48) | 2.53 (1.31-4.87) | 1.71 (1.22-2.41) | 1.74 (1.34-2.27) | |
| 15-30 days | 0.92 (0.64-1.31) | 0.85 (0.61-1.19) | 0.92 (0.68-1.25) | 2.82 (0.94-8.45) | 2.38 (1.37-4.14) | 1.87 (1.21-2.89) | |
| >30 days | 0.81 (0.52-1.27) | 0.84 (0.56-1.26) | 0.94 (0.64-1.39) | 1.62 (0.34-7.75) | 0.71 (0.34-1.49) | 0.91 (0.52-1.57) | |
| Assitance model | |||||||
| Econsult (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| In-person consultation | 1.52 (1.12-2.06) | 1.53 (1.16-2.03) | 2.33 (1.77-3.07) | 2.59 (1.32-5.05) | 4.04 (2.75-5.93) | 4.19 (3.05-5.75) | |
|
In bold: statistically significant factors (p<0.05) Abbrevations: OR: odds ratio; CI: confidence interval; CV, cardiovascular; HF, heart failure; HF-r, heart failure-related |
|||||||
| HF-r hospitalization | CV hospitalization | All-cause hospitalization | HF-r mortality | CV mortality | All-cause mortality | ||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Age | 1.00 (0.98-1.02) | 0.99 (0.98-1.01) | 1.00 (0.99-1.01) | 1.07 (1.02-1.12) | 1.08 (1.05-1.11) | 1.08 (1.06-1.10) | |
| Gender (men) | 2.16 (1.41-3.31) | 1.38 (1.10-1.73) | 1.29 (1.08-1.54) | 0.90 (0.43-1.90) | 1.40 (0.95-2.04) | 1.81 (1.39-2.36) | |
| Comorbidities | |||||||
| Arterial hypertension | 0.55 (0.35-0.86) | 0.79 (0.61-1.04) | 0.96 (0.77-1.19) | 0.54 (0.24-1.22) | 0.82 (0.53-1.28) | 0.68 (0.50-0.91) | |
| Diabetes mellitus | 1.82 (1.21-2.75) | 1.57 (1.25-1.97) | 1.38 (1.15-1.65) | 1.28 (0.58-2.83) | 1.02 (0.66-1.52) | 1.22 (0.92-1.61) | |
| Ischemic cardiopathy | 1.26 (0.80-1.98) | 1.59 (1.24-2.05) | 1.22 (0.99-1.51) | 0.85 (0.32-2.28) | 1.22 (0.77-1.93) | 1.12 (0.81-1.54) | |
| Atrial fibrillation | 1.01 (0.67-1.51) | 0.89 (0.71-1.12) | 0.93 (0.78-1.11) | 1.01 (0.48-2.09) | 1.01 (0.69-1.47) | 0.83 (0.64-1.08) | |
| Cerebrovascular disease | 0.40 (0.15-1.10) | 1.45 (1.02-2.06) | 1.17 (0.87-1.58) | 2.29 (0.85-6.22) | 1.57 (0.87-2.83) | 0.97 (0.60-1.56) | |
| Peripheral arterial disease | 0.81 (0.37-1.79) | 1.03 (0.69-1.56) | 1.17 (0.84-1.61) | 1.74 (0.50-5.99) | 1.74 (0.89-3.37) | 1.38 (0.85-2.25) | |
| Cardiology assitance | |||||||
| Emergency assistance (1 year) | 1.04 (1.01-1.06) | 1.02 (1.00-1.04) | 1.04 (1.03-1.06) | 0.99 (0.85-1.14) | 0.86 (0.78-0.95) | 0.94 (0.89-0.98) | |
| Delay time | |||||||
| 0-7 days (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 8-14 days | 0.85 (0.54-1.36) | 0.99 (0.77-1.27) | 0.99 (0.81-1.21) | 2.38 (0.82-6.89) | 2.51 (1.54-4.09) | 1.58 (1.15-2.16) | |
| 15-30 days | 0.91 (0.49-1.68) | 1.20 (0.85-1.69) | 1.26 (0.95-1.67) | 1.16 (0.21-6.52) | 0.92 (0.41-2.08) | 1.36 (0.85-2.18) | |
| >30 days | 1.55 (0.85-2.86) | 1.31 (0.89-1.92) | 1.29 (0.90-1.82) | 1.74 (0.16-19.47) | 2.18 (0.85-5.57) | 1.87 (1.02-3.43) | |
| Assitance model | |||||||
| Econsult (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| In-person consultation | 0.84 (0.49-1.46) | 1.03 (0.75-1.42) | 3.15 (2.37-4.20) | 0.34 (0.07-1.77) | 1.48 (0.78-2.81) | 0.85 (0.55-1.32) | |
|
In bold: statistically significant factors (p<0.05) Abbrevations: OR: odds ratio; CI: confidence interval; CV, cardiovascular; HF, heart failure; HF-r, heart failure-related |
|||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





