1. Introduction
Population ageing is increasing exponentially. In 2030, 1 in 6 individuals in the world will be over 65 years. It is estimated that in 2050, 2 billion people will be over 65 years [
1] and the number of individuals over 80 years will triple between 2020 and 2050, reaching 426 million people [
2]. All of this has several implications for health and social care planning [
3].
The most complex expression of population ageing is frailty, that can be defined as a state of vulnerability to poor recovery after an stressor event, leading to an increased risk of disability, hospitalization and mortality [
3]. This increased vulnerability is specially revealed under several circumstances, like acute illnesses and hospitalization [
4]. Consequently, frailty is a multifactorial syndrome with a high impact on patient´s health and is associated with delirium, disability, long-stay hospitalization, institutionalization and mortality [
5]. Hence, frail elderly patient are usually high costs-high needs patients, requiring a high degree of attention by healthcare systems [
6], and are a growing group in hospital Emergency Departments (ED) [
7].
. Frailty assessment is a keystone in geriatric care and is of paramount importance to address the elderly population heterogeneity. Different authors suggest to use frailty assessment as an equivalence for biological age, as opposed to chronological age, which provides little value in clinical decision making [
8,
9]. A large number of tools have been proposed for frailty assessment, but each of them have specific characteristics and limitations, since they were validated in different healthcare settings [
10]. Most commonly used scales differ in the number and type of deficits assessed, their validation environment, and the time and expertise required to be applicated [
11].
Moreover, frailty is common in older patients in hospital wards and hospital ED, with reported prevalence rates between 21 and 62%. It is often related with non-specific symptoms, which are accompanied by a constellation of factors (physical, psychological, nutritional, pharmacological, functional and social) that must be properly identified and assessed to provide specific, tailored, and effective care in emergency department [
12,
13,
14].
Multidisciplinary approach to frail patients should provide a Comprehensive Geriatric Assessment (CGA). CGA is the tool that allows a better understanding of the diverse and specific needs of the elderly at each stage of the care process, and an appropriate planning of their care [
3,
15]. Despite this, the concepts of frailty identification and CGA are not commonly performed in the ED [
16,
17,
18,
19,
20,
21,
22]. Cited barriers included feasibility of tools in the time pressured ED environment, lack of formal clinical frailty guidelines for the ED.
Short Stay Units (SSU) are ED supportive hospitalization units, that have demonstrated to be useful in avoiding or reducing overnight stays and days of admission [
23,
24,
25]. The admission criteria, which are usually common to all of them, include patients with medical pathology, a clear diagnosis, and a stable condition not requiring close monitoring or invasive treatment, and with an expected hospitalization period lasting less than 72 hours [
24,
25]. Over the years, admitted population in SSU has presented a significant change, as a result of population aging, although the admission criteria have not changed [
26]. SSU admitted patients are older, have more comorbidities and polypharmacy, and thus it seems necessary to include new strategies to identify risks in vulnerable individuals, while keeping hospital stays as short as possible. Frailty assessment may be useful, but there are no current recommendations on the best tool to apply for frailty screening in these units. The Fragile-VIG index (FI-VIG) is a frailty index (FI) developed by Amblàs et al. (C3RG, Chronicity Research Group of Central Catalonia), which offers both the possibility of doing a rapid CGA of individuals and calculating their grade of frailty, and which was initially validated in a cohort of patients over 85 years of age in a Acute Geriatric Unit (UGA) [
11,
27]. The index consists in a 22-item deficit rating scale. As the authors say, the results describes as a simple, quick tool (it’s completed in 5-10 minutes), with excellent discriminative and predictive capacity in relation to mortality, and performs a multidimensional assessment of the patient.
The scale has subsequently been validated in the context of intermediate care or health care hospitals [
28,
29] as well as in the community setting, with the same results. The authors keep it available in different languages and free of charge at
https://www.c3rg.com/index-fragil-vig.
The aim of our study is to analyze the utility of FI-VIG in a new scenario, a ED SSU, and its performance to properly identify groups of patients with different grades of frailty and mortality risk.
2. Materials and Methods
An observational, single-center, prospective, cohort study was done in the short stay unit (SSU) of the Emergency Department of the Hospital de la Santa Creu i Sant Pau, a tertiary and university, urban, with 550-bed center. The SSU has 36 beds, reporting to the ED, with 2,243 admissions during 2021.
The study was approved by the Clinical Research Ethics Committee under sponsor code IIBSP-FRA-2020-74. The CEIC considered the request for informed consent unnecessary because it was a registry of a validated scale and a non-interventional study. All patients admitted to the SSU over 65 years between March 1, 2021 until April 30, 2021 and were consecutively included. Only patients admitted for end-of-life care treatment were excluded. After admission, patients were followed up for one year. Follow-up was by consultation of the Shared Health Record of Catalonia (HC3) and a 12-month telephone call to the patient or career. There was no loss to follow-up.
The research team consisted of two attending physicians from ED, SSU chief-nurse and 4 nurses. FI-VIG support was used. After initial training by the principal investigator, one of the nurses assessed IF-VIG within the first 24 hours of admission taking into account, as determined by the index, the patient's situation in the 30 days before to admission.
Based on the FI-VIG
https://en.c3rg.com/index-fragil-vig, patients were categorized into non-frail (< 0.2), initial frailty (0.2 - 0.36), intermediate frailty (0.36 - 0.55) and advanced frailty (> 0.55).
The study variables were demographic and administrative data (date of birth, sex, date of admission to the short-stay unit, discharge date from the unit, reason for discharge); clinical data (comorbidities, functional and cognitive status, social status, geriatric syndromes).
Following the methodology recommended by the authors of the scale, the binary variables were scored as "0" absence and "1" presence of deficits. Money management, telephone use and medication management were assessed as instrumental activities of daily living. Weight loss of more than 5% was assessed as a nutritional marker; presence of depressive syndrome, insomnia and anxiety as emotional markers and presence of social vulnerability as a social marker. The presence of pain and dyspnea were considered as symptoms with severity criteria. Delirium, falls, ulcers, polypharmacy and dysphagia were assessed as geriatric syndromes. Finally, the existence of chronic diseases was recorded as "1", and in case of advanced chronic disease according to the NECPAL test, 2 points were assigned. In relation to ordinary variables, the Barthel index was used in 4 categories according to absence of dependence, mild, moderate-severe and severe dependence. Cognitive impairment was classified as 0 points no impairment, 1 point mild/moderate impairment and 2 points severe/very severe impairment. Mortality was monitored at admission, at 1 month, 6 months and 1 year through HC3 and telephone calls at 1 year.
The result of the FI-VIG of each patient was not communicated to the healthcare team, so as not to modify clinical practice or perform any intervention at this stage of the study.
Categorical variables were described as frequency and percentage of available data, while quantitative variables were described as mean and standard deviation (SD). Descriptive statistics of the variables analyzed were performed using SPSS. Statistical significance (95% confidence interval/p < 0.05) for the variables between patients alive/death was determined by means of mean contrasts (for quantitative variables) and proportion contrasts (for qualitative variables). For survival analysis, the log-rank test was used to compare survival curves according to the FI-VIG value and ROC curve analysis to determine the prognostic capacity of FI-VIG for mortality code.
3. Results
3.1. Descriptive Analysis of the Cohort
Of the 501 patients admitted to the SSU during the study period, 323 were over 65 years. Of these, 21 had been admitted for end-of-life care, and were excluded. A total of 302 patients were included, whose mean age was 82.62 years, 56% were women (n=169). Five percent of the patients (n=15) lived in a nursing home.
A total of 60.9% of patients were independent for basic activities of daily living (ADLs, n=184). Mild-moderate dependence for ADLs was observed in 23.5% (n=71), moderate-severe in 10.3% of patients (n=31) and absolute dependence in 5.3% (n=16). Mild-moderate cognitive impairment GDS<5 (n=44) and moderate-severe cognitive impairment GDS>6 (n=6) accounted for 14.6% of patients. The data are presented in
Table 1. In-hospital mortality of the cohort was 3% (n=9), at 1 month 12.3% (n=37), at 6 months 20.6% (n=62) and at 1 year 23.2% (n=70).
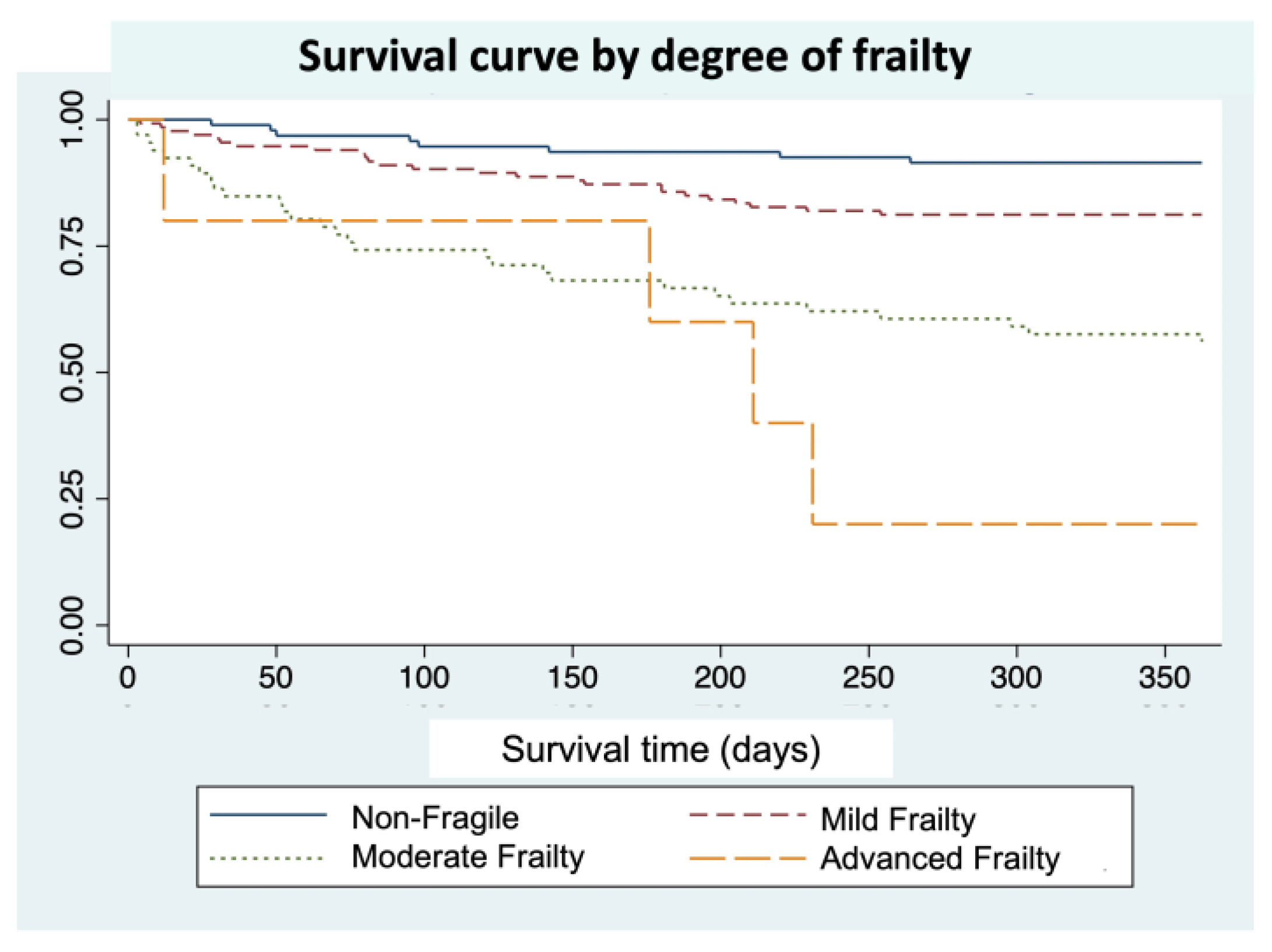
Of the 302 patients included, 128 (42.4%) were categorized as non-fragile and 174 (57.6%) were categorized overall as fragile. Of these, 111 (36.8%) had initial frailty, 52 (17.2%) had intermediate frailty and 11 (3.6%) had advanced frailty.
3.1. Time of Test Execution
The mean running time of the index was 7 minutes per patient.
3.3. Mortality Analysis
Table 2 shows the differences in the percentage of mortality between frailty groups. In non-fragile patients, no death was detected during admission compared to 5.2% (n=9) in fragile patients (p=0.012). At 30 days, mortality was 6.3% (n=8) in non-fragile patients vs 16.7% (n=29) in fragile patients (p=0.007); at 6 months, 10.2% (n=13) in non-fragile patients vs 28.2% (n=49) in fragile patients (p=0.001) and at 1 year, it was 12.5%(n=16) in non-fragile vs 31% (n=54) in fragile patients (p=0.001).
Figure 1 shows the results of the analysis of the correlation between mortality and FI-VIG by means of the log-rank test comparing the survival curves according to the IF-VIG value, discretized by the previously mentioned intervals.
3.4. Model Usefulness
A ROC analysis was performed at 12 months to check the usefulness of the model in the population studied. The ROC area under the curve was 0.7120 (95%CI 0.6423 - 0.7816).
4. Discussion
Our work shows that FI-VIG is a reliable and accurate tool for frailty screening in SSU, with a similar performance to that demonstrated in other settings. FI-VIG correlates frailty status with mortality, and our study shows that this correlation is still valid for a SSU setting.
It is well known that frailty status leads to progressively higher mortalities during hospital admission, as well as at 30 days, 6 months and 1 year after discharge. Although the SSU admitted patients showed different characteristics when compared with the population in which the FI-VIG was initially validated, the results of this study demonstrate that the FI-VIG is also applicable in this population. Although the results of the ROC curve are relatively lower than those obtained in the pivotal study, FI-VIG scale still offers a great discriminatory capacity between the different degrees of frailty. Furthermore, its performance mean time was 7 minutes, which confirms that it is a feasible, easy-to-use scale in a SSU setting.
Systematically measuring frailty is undoubtfully useful in patient management [
28] and in SSU, FI-VIG turned out to be an accurate tool, that should be incorporated in clinical practice. FI-VIG assigns to each patient a numerical score, allowing its categorization in different frailty degrees, which in turn correlate well with mortality. In addition, as it is a multidimensional scale, it is able to detect several deficits in frail patients, that can be used as the base of a reglementary CGA [
11,
26]
Frailty assessment during SSU admission allows prompt patient referral to expert teams in order to initiate interventions focused on reversing or preventing secondary risks. By doing this, it improves the prevention of incidental geriatric syndromes during admission in frail individuals, as an specific care plan can be early designed (early mobilization, identification and correct management of delirium, prevention of constipation and falls, careful pain management, avoidance of medication-related risks and initiation of pharmaceutical care programs [
31] among others). Finally, by frailty stratification, FI-VIG offers the chance of tailored interventions and therapeutic intensity for this patients [
32,
33].
Given the growing importance of frailty as an expanding public health problem, interventions like FI-VIG application in order to deliver an integrated care to older people across different settings could make acute and community care more responsive for all patients.
In our study, mean cohort age was 82.6 years, and almost 40% of patients had some degree of disability and 16.5% had dementia. As in other SSU in our country, the population is selected a priori by the criteria that determine the decision of admission to this unit, and the demographic characteristics of our cohort are similar to those reported in the literature in recent works [
34]. Through FI-VIG application, we were able to determine that 57.6% of the patients in our SSU had some frailty degree, being most of them classified as mild (63.8%) or moderately (29.9%) frail. These data are relevant since we have not found similar studies describing frailty features in a SSU in our country. Despite being a previously selected population, with an expected short hospital stay, our study revealed that in our SSU there was a large group of frail individuals in whom FI-VIG performance could offer a great opportunity for tailored interventions.
We identified remarkable limitations in our study. It is a single-center study, and contains a low number of patients with advanced frailty, probably due to the narrow admission criteria in a SSU. Furthermore, it doesn’t considers the concomitant diseases as factors that may influence in the survival rate. However, it has several strengths: it was designed as a prospective study, we recruited a large number of patients, and frailty assessment was performed by a small, highly-trained research team.
5. Conclusions
In conclusion, FI-VIG is a valid tool for systematic frailty identification in a SSU. In this setting, it keeps a good feasibility as well as diagnostic test accuracy, and allows early risk stratification, prompt CGA and tailored, specific interventions for each patient.
Author Contributions
Conceptualization, Mireia Puig and Josep Ris; methodology, Miguel Rizzi and Josep Anton Montiel.; software, Miguel Rizzi and José Alberto Santos.; validation, Marta Blázquez, Josep Anton Montiel and Leopoldo Higa; formal analysis, José Alberto Santos and Miguel Rizzi.; investigation, Marta Blázquez, Josep Anton Montiel, Belén Acosta, Elena Gonzalez, Rosario Fraile, David Figueroa, Iván Agra y Sergio Herrera; data curation, José Alberto Santos, Miguel Rizzi.; writing—original draft preparation, Marta Blázquez, Mireia Puig.; writing—review and editing, all.; supervision, Josep Anton Montiel, Josep Ris, Mireia Puig.; project administration, Josep Anton Montiel.; funding acquisition, Josep Anton Montiel. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by by the Hestia Chair in Integrated Social and Health Care 2020.
Acknowledgments
We thank Dr. Jordi Amblàs Novellas for his review of this manuscript. Dr. Amblàs is Associate Professor at UVic-UCCC, Director of Strategy at l'Agència d'Integració Social i Sanitària (Departament de Salut) and Head of the Central Catalonia Chronicity Research Group (C3RG) & Centre for Health and Social Care Research (CESS).
Conflicts of Interest
The authors declare no conflict of interest.
References
- United Nations Population Division. The World at Six Billion. United Nations Publ.:1-63.
- World Health Organization, Ageing and health report. Retreived 19th september 2021. Link: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. W: 2018, 2018.
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Mitnitski, A.; Rockwood, K. Prevalence and 10-Year Outcomes of Frailty in Older Adults in Relation to Deficit Accumulation. J. Am. Geriatr. Soc. 2010, 58, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Theou, O.; Campbell, S.; Malone, M.L.; Rockwood, K. Older Adults in the Emergency Department with Frailty. Clin. Geriatr. Med. 2018, 34, 369–386. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, D.; Chernof, B.; Fulmer, T.; Lumpkin, J.; Selberg, J. Caring for High-Need, High-Cost Patients — An Urgent Priority. New Engl. J. Med. 2016, 375, 909–911. [Google Scholar] [CrossRef] [PubMed]
- Brousseau, A.-A.; Dent, E.; Hubbard, R.; Melady, D.; Émond, M.; Mercier. ; Costa, A.P.; Gray, L.C.; Hirdes, J.P.; Dey, A.B.; et al. Identification of older adults with frailty in the Emergency Department using a frailty index: results from a multinational study. Age Ageing 2017, 47, 242–248. [Google Scholar] [CrossRef]
- Ji, L.; Jazwinski, S.M.; Kim, S. Frailty and Biological Age. Ann. Geriatr. Med. Res. 2021, 25, 141–149. [Google Scholar] [CrossRef]
- Turner, G.; Clegg, A. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing 2014, 43, 744–747. [Google Scholar] [CrossRef]
- Boreskie, K.F.; Hay, J.L.; Boreskie, P.E.; Arora, R.C.; Duhamel, T.A. Frailty-aware care: giving value to frailty assessment across different healthcare settings. BMC Geriatr. 2022, 22, 1–12. [Google Scholar] [CrossRef]
- Amblàs-Novellas, J.; Martori, J.C.; Espaulella, J.; Oller, R.; Molist-Brunet, N.; Inzitari, M.; Romero-Ortuno, R. Frail-VIG index: a concise frailty evaluation tool for rapid geriatric assessment. BMC Geriatr. 2018, 18, 1–12. [Google Scholar] [CrossRef]
- Simon, N.; Jauslin, A.; Bingisser, R.; Nickel, C. Emergency presentations of older patients living with frailty: Presenting symptoms compared with non-frail patients. Am. J. Emerg. Med. 2022, 59, 111–117. [Google Scholar] [CrossRef]
- Djärv, T.; Castrén, M.; Mårtenson, L.; Kurland, L. Decreased general condition in the emergency department. Eur. J. Emerg. Med. 2015, 22, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Fehlmann, C.A.; Nickel, C.H.; Cino, E.; Al-Najjar, Z.; Langlois, N.; Eagles, D. Frailty assessment in emergency medicine using the Clinical Frailty Scale: a scoping review. Intern. Emerg. Med. 2022, 17, 2407–2418. [Google Scholar] [CrossRef] [PubMed]
- Lucke, J.A.; Mooijaart, S.P.; Heeren, P.; Singler, K.; McNamara, R.; Gilbert, T.; Nickel, C.H.; Castejon, S.; Mitchell, A.; Mezera, V.; et al. Providing care for older adults in the Emergency Department: expert clinical recommendations from the European Task Force on Geriatric Emergency Medicine. Eur. Geriatr. Med. 2021, 13, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Elliott, A.; Taub, N.; Banerjee, J.; Aijaz, F.; Jones, W.; Teece, L.; van Oppen, J.; Conroy, S. Does the Clinical Frailty Scale at Triage Predict Outcomes From Emergency Care for Older People? Ann. Emerg. Med. 2020, 77, 620–627. [Google Scholar] [CrossRef]
- Kaeppeli, T.; Rueegg, M.; Dreher-Hummel, T.; Brabrand, M.; Kabell-Nissen, S.; Carpenter, C.R.; Bingisser, R.; Nickel, C.H. Validation of the Clinical Frailty Scale for Prediction of Thirty-Day Mortality in the Emergency Department. Ann. Emerg. Med. 2020, 76, 291–300. [Google Scholar] [CrossRef]
- Rosenbaum, L. Facing Covid-19 in Italy — Ethics, Logistics, and Therapeutics on the Epidemic’s Front Line. New Engl. J. Med. 2020, 382, 1873–1875. [Google Scholar] [CrossRef]
- Jørgensen, R.; Brabrand, M. Screening of the frail patient in the emergency department: A systematic review. Eur. J. Intern. Med. 2017, 45, 71–73. [Google Scholar] [CrossRef]
- Elliott, A.; Phelps, K.; Regen, E.; Conroy, S.P. Identifying frailty in the Emergency Department—feasibility study. Age Ageing 2017, 46, 840–845. [Google Scholar] [CrossRef]
- Lewis, E.T.; Dent, E.; Alkhouri, H.; Kellett, J.; Williamson, M.; Asha, S.; Holdgate, A.; Mackenzie, J.; Winoto, L.; Fajardo-Pulido, D.; et al. Which frailty scale for patients admitted via Emergency Department? A cohort study. Arch. Gerontol. Geriatr. 2018, 80, 104–114. [Google Scholar] [CrossRef]
- O’caoimh, R.; Costello, M.; Small, C.; Spooner, L.; Flannery, A.; O’reilly, L.; Heffernan, L.; Mannion, E.; Maughan, A.; Joyce, A.; et al. Comparison of Frailty Screening Instruments in the Emergency Department. Int. J. Environ. Res. Public Heal. 2019, 16, 3626. [Google Scholar] [CrossRef]
- Cosco, T.D.; Best, J.; Davis, D.; Bryden, D.; Arkill, S.; van Oppen, J.; Riadi, I.; Wagner, K.R.; Conroy, S. What is the relationship between validated frailty scores and mortality for adults with COVID-19 in acute hospital care? A systematic review. Age Ageing 2021, 50, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Puig-Campmany, M.; Blázquez-Andion, M.; Ris-Romeu, J. Aprender, desaprender y reaprender para asistir ancianos en urgencias : el secreto del cambio. Emergencias 2020, 32, 122–130. [Google Scholar]
- Alonso, G.; Escudero, J.M. La unidad de corta estancia de urgencias y la hospitalización a domicilio como alternativas a la hospitalización convencional. An. del Sist. Sanit. de Navar. 2010, 33, 97–106. [Google Scholar] [CrossRef]
- Sánchez-Marcos, C.; Jacob, J.; Llorens, P.; Rodríguez, B.; Martín-Sánchez, F.; Herrera, S.; Castillero-Díaz, L.; Herrero, P.; Gil, V. ; Miró, Análisis de la efectividad y seguridad de las unidades de estancia corta en la hospitalización de pacientes con insuficiencia cardíaca aguda. Propensity Score UCE-EAHFE. 2022, 222, 443–457. [Google Scholar] [CrossRef]
- González Armengol JJ, Fernández Alonso C, Martín Sánchez FJ, et al. Actividad de una unidad de corta estancia en urgencias de un hospital terciario: cuatro años de experiencia. Emergencias Rev la Soc Española Med Urgencias y Emergencias 2009, 21, 87–94. [Google Scholar]
- Amblàs-Novellas, J.; Torné, A.; Oller, R.; Martori, J.C.; Espaulella, J.; Romero-Ortuno, R. Transitions between degrees of multidimensional frailty among older people admitted to intermediate care: a multicentre prospective study. BMC Geriatr. 2022, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Amblàs-Novellas, J.; Martori, J.C.; Brunet, N.M.; Oller, R.; Gómez-Batiste, X.; Panicot, J.E. Índice frágil-VIG: diseño y evaluación de un índice de fragilidad basado en la Valoración Integral Geriátrica. Revista Española de Geriatría y Gerontología 2016, 52, 119–127. [Google Scholar] [CrossRef]
- Zamora-Sánchez, J.J.; Zabaleta-Del-Olmo, E.; Gea-Caballero, V.; Julián-Rochina, I.; Pérez-Tortajada, G.; Amblàs-Novellas, J. Validez convergente y discriminativa del índice Frágil-VIG con la escala de Braden en personas atendidas en atención domiciliaria. Revista Española de Geriatría y Gerontología 2022, 57, 71–78. [Google Scholar] [CrossRef]
- van Dam, C.S.; Hoogendijk, E.O.; Mooijaart, S.P.; Smulders, Y.M.; de Vet, R.C.; Lucke, J.A.; Blomaard, L.C.; Otten, R.H.; Muller, M.; Nanayakkara, P.W.; et al. A narrative review of frailty assessment in older patients at the emergency department. Eur. J. Emerg. Med. 2021, 28, 266–276. [Google Scholar] [CrossRef]
- Juanes, A.; Garin, N.; Mangues, M.A.; Herrera, S.; Puig, M.; Faus, M.J.; Baena, M.I. Impact of a pharmaceutical care programme for patients with chronic disease initiated at the emergency department on drug-related negative outcomes: a randomised controlled trial. Eur. J. Hosp. Pharm. 2017, 25, 274–280. [Google Scholar] [CrossRef]
- Amblàs-Novellas, J.; A Murray, S.; Espaulella, J.; Martori, J.C.; Oller, R.; Martinez-Muñoz, M.; Molist, N.; Blay, C.; Gómez-Batiste, X. Identifying patients with advanced chronic conditions for a progressive palliative care approach: a cross-sectional study of prognostic indicators related to end-of-life trajectories. BMJ Open 2016, 6, e012340. [Google Scholar] [CrossRef] [PubMed]
- Richard Espiga, F.; Mòdol Deltell, J.M.; Martín-Sánchez, F.J.; Fernández Sierra, A.; Fernández Pérez, C.; Pastor, A.J. Impacto de la creación de una unidad de corta estancia (UCE) dependiente orgánicamente de urgencias en la gestión clínica y la calidad asistencial hospitalaria. Emergencias 2017, 29, 147–153. [Google Scholar] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).