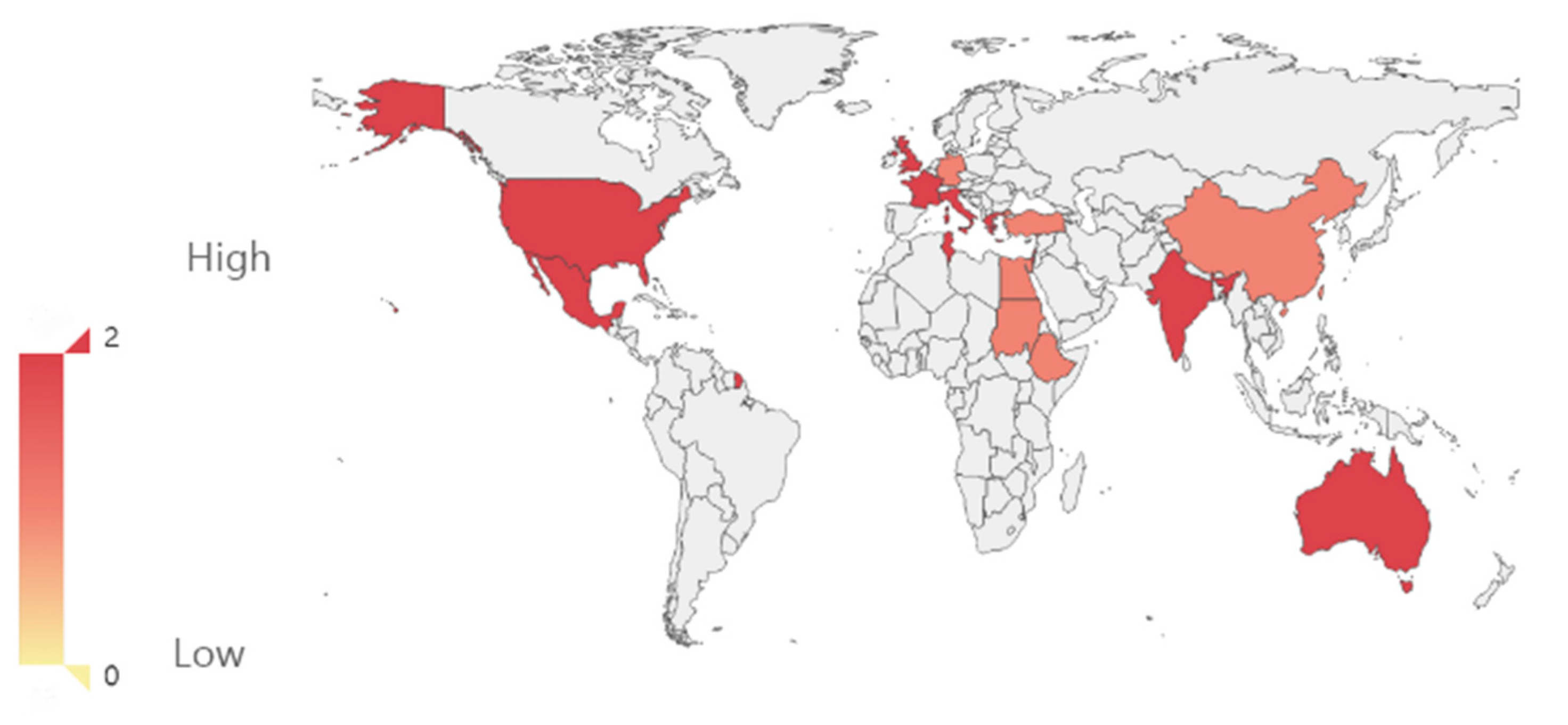
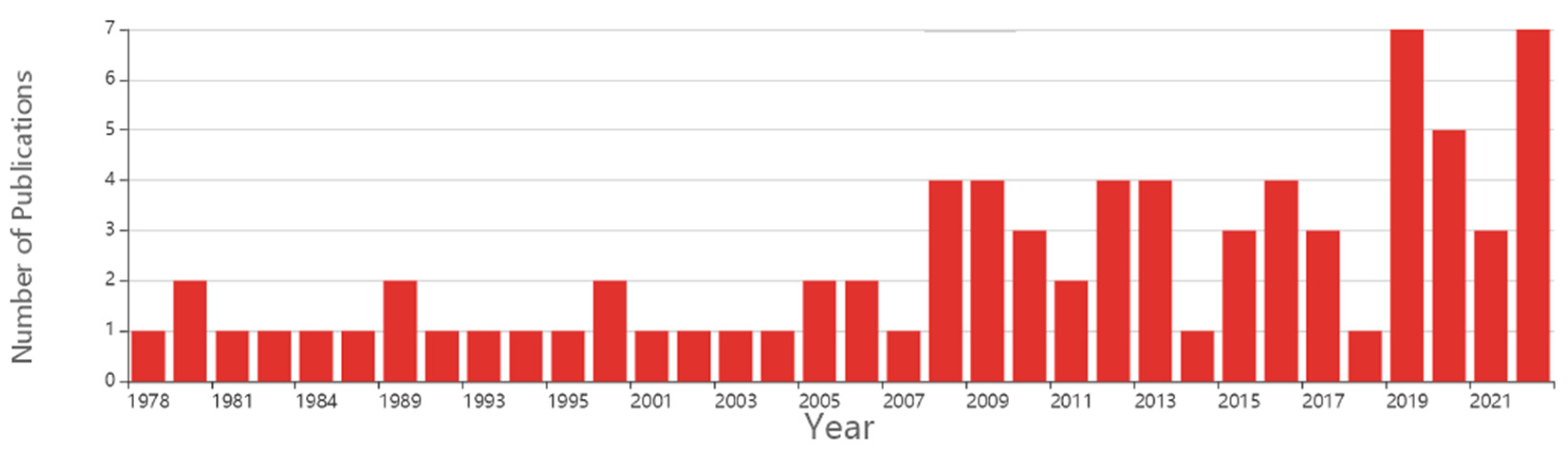
1. Introduction
The cavovarus foot is an acquired foot deformity with an incidence of about 1:100,000. It is caused by progressive forefoot pronation, resulting in a high-arched medial and middle foot shape and a compensatory varus of the hindfoot [
1] (
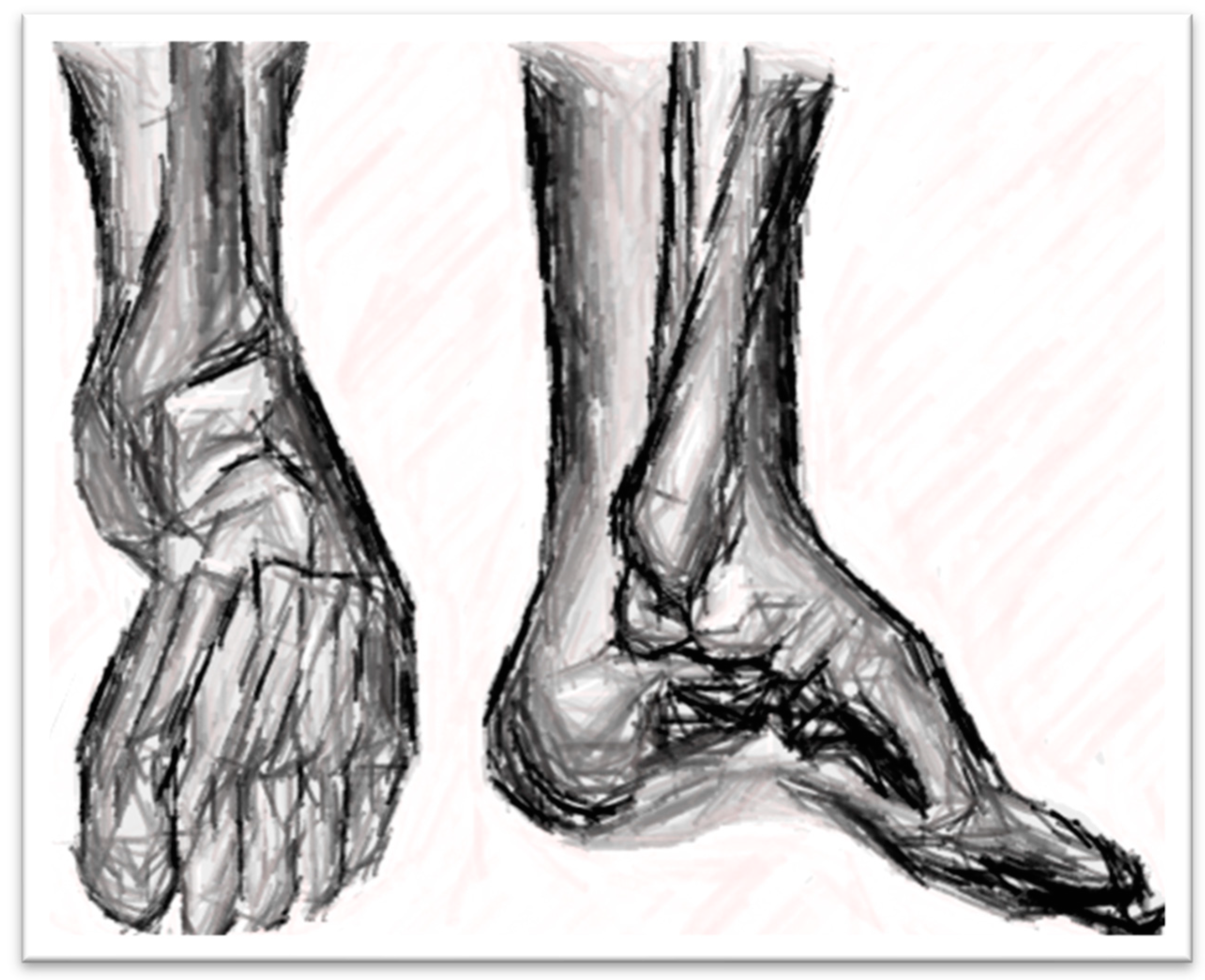
figure 1^
2). The etiology of the cavovarus foot is complicated. According to the current research, the main factor leading to a cavovarus foot is the imbalance of muscle strength. The most common pathogenic factor is hereditary motor sensory neuropathy, found in 66% of children with hyper arch malformation [
2]. Other factors include myelomeningocele, poliomyelitis, residual malformation of horseshoe feet, post-traumatic cavovarus feet, etc. [
3,
4]. cavovarus is not a single planar deformity but a three-dimensional planar deformity of the foot. Foot deformities are complex, requiring careful medical history, physical examination, and imaging analysis to evaluate children's cavovarus deformity in the foot fully.
The cavovarus foot mainly manifests as muscle weakness, limited dorsiflexion of the ankle joint, progressive increase of the foot's medial arch, and secondary varus deformity of the hindfoot, resulting in ankle instability and uncomplicated sprain during walking. In severe cases, the first and fifth metatarsal bones may appear as skin ulcers due to long-term wear [
5]. When the child has claw toe deformity due to friction with the shoe, the back of the toe may also appear callose or have skin ulcers. Children often have difficulty carrying out daily activities, affecting their mental health development; these manifestations and behaviors are the main reasons children and their families visit the hospital. The cavovarus foot is more harmful to children, especially the deformity has a progressive trend of cavovarus foot deformity, will eventually lose the ability to walk. Therefore, early intervention and treatment of cavovarus can block or delay the progression of the disease and ultimately avoid or delay joint fusion surgery in children. However, according to the current study, the long-term treatment effect of these children is quite different due to the complexity of the cavovarus foot deformity. A complete evaluation of cavovarus before treatment is the basis for treating cavovarus. The Coleman test is most commonly used to determine the foot's flexibility. The medial side of the foot was suspended in the air, the lateral side was placed on a 2.5cm wooden block, and the anterolateral X-ray film of the foot was taken. The alignment of the forefoot was restored to normal, and the deformity of the cavovarus was corrected, proving that only soft tissue could be performed [
5,
6]. If the alignment of the front foot does not return to normal, osteotomy of the front foot should be performed. If the back foot cannot be corrected, osteotomy of the calcaneus should be performed. Mark et al. [
35] extended the affected limb of the child to correct the forefoot's cavovarus and subtalar joint artificially. If correct, it would be flexibility, which the author believed was more reliable than Coleman's test. However, the Coleman test is more objective, and that radiographic evaluation is essential in assessing cavovarus foot deformities, with standard standing weight-bearing front and side views of the foot taken.
2. Clinical manifestations
The cavovarus foot mainly manifests as muscle weakness, limited dorsiflexion of the ankle joint, progressive increase of the foot's medial arch (
Figure 3), and secondary varus deformity of the hindfoot, resulting in ankle instability and uncomplicated sprain during walking. In severe cases, callose may appear in the skin of the first and fifth metatarsal bones due to long-term wear [
5]. These manifestations are the main reasons children and their families visit the hospital. When the child has claw toe deformity due to friction with the shoe, the back of the toe may also appear callose or have skin ulcers.
The clinical examination of the foot should begin with gait analysis and observe the morphology of the foot at various stages of the gait cycle. Foot balance is achieved by creating a balanced tripod where the center of pressure is placed so that pain does not occur. These points include the heel, medial front foot, and lateral front foot. Patients with neuromuscular cavovarus often have an underlying muscle imbalance, resulting in loss of tripod structure, increased foot pressure, subsequent gait changes, foot pain, and wear. Due to the high arch of the foot, force line deviation, and muscle force imbalance, the forefoot and middle foot are stiff, and the back extension and internal and external rotation cannot be good during walking [
5].In the process of toe shedding, the high arch of the middle foot is significantly increased due to the overextended metatarsophalangeal joint and the hoist effect of plantar fascia [
26].
More clinical information can also be obtained by visiting patients. The patient's feet should be shoulder-width apart, and the medial boundaries of the feet should be parallel to each other to offset the difference caused by the rotation of the lower extremities [
28]. Slight limb length differences or asymmetrical foot size may result from neuromuscular lesions. A posteromedial incision may indicate previous surgical treatment of the malformation. There is a history of reduction and fixation of the fracture, suggesting that the cavovarus deformity may be caused by trauma. The sole's wear degree can understand the foot's force distribution and assist in diagnosing cavovarus foot deformity. A view of the patient's foot from the normal front can be used to assess a forefoot-driven cavovarus foot deformity. Forefoot-driven high arches are plantar flexion and pronation deformity of the forefoot relative to the middle foot, accompanied by a compensatory posterior varus deformity to improve the stress distribution of the plantar. An imbalance of muscle strength between the peroneal longus tendon and the anterior tibial tendon can aggravate the metatarsal flexion deformity of the first metatarsal bone [
30]. Cavovarus deformity can also be caused by hind feet, but Cavovarus deformity caused by hind feet is more common than high arches deformity caused by forefeet Rare. Usually, the heel should be positioned at the calf's midline due to the calcaneus's valgus position. When the hind foot is varus, the heel is on the inside of the midline of the calf. In patients with Cavovaruss foot deformity caused by the hind foot, the gastrocnemius muscle strength is weakened, which can lead to a distinct vertical calcaneus. Current studies have shown that several neurological diseases are related to calcaneal Cavovarus foot deformity, including poliomyelitis, iatrogenic injury after cerebral palsy treatment, spinal deformity, and intraspinal etiology [
29].
During a physical examination, the foot and ankle joints should be palpated while the patient is seated. Careful physical examination revealed plantar pressure distribution in Cavovarus foot deformity, with the first metatarsal head being the most common site of pain [
17]. Palpation of the bases of the fourth and fifth metatarsals may indicate stress fractures or stress pain [18.19]. A history of unhealed proximal lateral metatarsal fractures also requires examining the metatarsal base [
38]. Palpation of the medial plantar fascia may reveal pain or stiffness, and pain in the lateral fibula may be due to peroneal tendinopathy. The severity of the deformity can be assessed by assessing the range of motion of individual joints throughout the foot and ankle. The range of motion of the active and passive ankle joints should be assessed while sitting—inability to dorsiflexion the ankle joint, usually due to Achilles tendon contracture in the back foot. Partial ankle flexion without dorsiflexion indicates a combination of gastrocnemius and plantar contracture. Limitation of ankle dorsiflexion may also result from an impingement of the anterior medial ankle of the talus during dorsiflexion. A foot examination can rule out the presence of arthritis [
33]. Patients should raise the heel of one or both legs to assess subtalar joint flexibility. The flexibility of the subtalar joint reduces the likelihood of arthritis in the rear foot when the calcaneus can be valgus when the foot follows the ground and varus when the heel is raised. The Kelikian test can be used to evaluate the flexibility of paw toe deformity in the metatarsophalangeal joint. Passive overextension of the metatarsal head can tense the plantar fascia and correct flexible paw toe deformity. If the claw toe deformity cannot be corrected, then the claw toe deformity is rigid. In general, passively correctable deformities can be corrected by tendon transfer, whereas rigid deformities require osteotomy [
36].
A neurophysical examination is also essential to evaluate the deformity of the high arches. Neurological examination may indicate an underlying systemic peripheral neuropathy or central nervous system lesion resulting in a Cavovarus foot deformity. Patients with severe bilateral Cavovarus foot deformity and claw toe deformity should undergo electromyographic testing to determine the presence of peripheral nerve disorders such as Charcot-Marie-Tooth(CMT) disease. One study found that the incidence of CMT in patients with bilateral Cavovarus foot deformity was 78%[
35].In addition, the incidence of CMT in families with a positive family history can reach 91%. Patients with CMT often have intrinsic muscle weakness, most evident in the first intermetacarpal muscle of the hand. Abnormal reflexes and upper motor neuron signs such as Babinski's and Hoffman's may indicate central nervous system etiology.
In the second decade of life, hereditary ataxia patients manifest progressive hyper arches. The clinical triad of hereditary ataxia involves ataxia, Babinski positives, and the absence of reflexes. Individuals with cerebral palsy can develop a varus Cavovarus foot deformity accompanied by anterior tibial muscular spasm. Examining the spine focuses mainly on determining whether there is a field on the back of the spine, such as hair development in the spine region of the back, a dip on the surface of the skin, or a bulge on the surface of the skin. These abnormalities may indicate an underlying developmental disorder of the spine and should be refined by spinal MRI imaging. Asymmetrical or rapidly progressing hyper arch deformities also require spinal imaging to rule out intramural lesions such as intramural tumors or tetragonal spinal cord [
25,
27,
28].
Muscle strength assessment provides the theoretical basis for implementing muscle balance techniques. The current muscle strength grading system is the Medical Research Council (MRC). The MRC system classifies muscle strength into five levels, as follows: 1: muscle contraction can be detected; Level 2: Muscle activity can cause the joint to move in the plane, but not against gravity movement; Level 3: Muscle contraction can resist gravity, but not resistance; Level 4: can partially resist resistance; Stage 5: Muscle contractions can fully resist resistance activities. Usually, patients with CMT affect the internal muscles of the foot first because the longer peripheral nerves are affected first. The weakness of the anterior tibialis muscle and the relative strength of the fibula longus lead to the first metatarsal sags, and the forefoot pronation leads to the deformity of the Cavovarus foot. The anterior tibialis muscle becomes weaker, resulting in a reduction in the foot's dorsiflexion and plantarflexion. The tendons of the tibialis posterior are more potent than those of the peroneus brevis, enabling adduction and varus of the middle foot [
29,
30,
31]. Weakness of the gastrocnemius muscle in poliomyelitis can lead to posterior varus deformity. People with polio may have limb weakness and limb length differences but not intrinsic muscle weakness of the foot. Cerebral palsy patients often have muscle spasms of the anterior tibial muscle and rigid claw toe deformity [
30].
3. Imaging evaluation
The evaluation of plain radiographs is very important for evaluating Cavovarus foot deformity (
Figure 3). The standard anteroposterior and lateral weight-bearing radiographs taken before and after surgery are an essential imaging basis for observing the postoperative efficacy of patients. Before the foot stand weight can measure, the foot deformity rate is side a little while the Meary Angle (from the first metatarsal bone and attachment Angle), standard Meary Angle of 0 ± 5 °, prompt the axis of the talus and the axis of the first metatarsal in the same line. Meary Angle >5° indicates metatarsal flexion of the first metatarsal bone. The Meary Angle of the Cavovarus foot is 18° on average. Deformities of the hind foot were assessed by measuring calcaneal Pitch Angle and Hibb Angle on standing weight-bearing lateral radiographs. The Pitch Angle of calcaneal bone is the Angle between the horizontal line between calcaneal bone and the ground and the axis of calcaneal bone. The standard Pitch Angle of calcaneal bone is 22°, and the Pitch Angle of calcaneal bone >30° indicates that the Cavovarus deformity comes from the hindfoot. The Hibb Angle is the Angle between the calcaneus axis and the first metatarsal bone, which is generally less than 45°, and the Hibb Angle of Cavovarus deformity is generally greater than 90°. Bilateral standing anterioradiography can be used to understand coronal deformities. The overlap between metatarsal bones indicates pronation of the forefoot, and the Angle between the talus and calcaneus is greater than 7°, indicating adduction deformity of the forefoot [
6]. These indicators are suitable imaging parameters to evaluate the deformity's location, degree, and progression. It is also the exact measurement index of orthopedic effect in postoperative follow-up.
4. Treatment of Cavovarus
4.1. Conservative treatment
Authors should discuss the results and how they can be interpreted in perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
The treatment of Cavovarus depends mainly on the severity of the deformity and can be treated conservatively for mild or early detection of Cavovarus. However, the effectiveness of conservative treatment is controversial, and several recent studies have shown better outcomes in younger children. Pin et al. reported that the therapeutic effect of a brace on Cavovarus caused by cerebral palsy was poor [
7].
Maas et al. [
8] studied the application of knee-ankle-foot braces to prevent a reduced range of motion and found that children generally could not tolerate the treatment and could not stop the progression of the disease. Astory et al. [
9] reported that through conservative treatment, after 4-5 years of follow-up, 65% of the children achieved good results, and finally, the operation was delayed or even avoided. For children with Cavovarus caused by CMT, it is mainly due to muscle imbalance. Injecting botox into the muscles with strong muscles may weaken these muscles with strong muscles. Burns et al. [
10] injected 7iu/kg botox into the posterior tibial tendon and the peroneus longus muscle, and after 2 years of treatment, there was no significant change compared with the contralateral foot.
Similarly, Tiffreau et al. [
11] injected 50iu of botox into the posterior tibialis tendon and showed some improvement after 6 months of treatment. Thus, botox injection has no apparent effect on treating Cavovarus. Conservative treatment ultimately fails due to the progression of pain. Although conservative treatment has certain limitations, it can be used as an auxiliary orthosis after surgery to maintain the postoperative foot orthosis of children.
4.2. Surgical Treatment
4.2.1. Release of the plantar fascia
Plantar fascia plays an essential role in the formation and development of Cavovarus in the surgical treatment of children. If the metatarsophalangeal joint is overextended, the plantar fascia will tighten, and the arch will increase. Plantar fascia contracture will be secondary to the overextended metatarsophalangeal joint, causing arch elevation. Therefore, if the patient has a contracture of the plantar fascia, it should be released. A simple plantar fascia release can achieve the therapeutic effect for Cavovarus with mild deformity. Plantar fascia release surgery should be performed even if bone surgery is required. Therefore, plantar fascia release combined with osteotomy is currently the most widely used surgical method. In younger children, single plantar fascia release may result in flat feet. Open plantar fascia release and postoperative plaster fixation are recommended for moderate to severe Cavovarus. Plantar fascia release is essential to most Cavovarus foot treatments, especially in children with CMT; the plantar fascia will have a contracture. Kwon et al. [
12] adopted plantar fascia release combined with a first metatarsal osteotomy, and the plantar pressure of the children was significantly improved after surgery. In a recent study, Sanpera et al. [
13] used plantar fascia release combined with the first metatarsal epiphyseal block, and after 28 months of follow-up, the Cavovarus deformity was well corrected. Therefore, it is recommended that most children should release the plantar fascia during the surgical treatment.
4.2.2. Tendon transposition
Most children with Cavovarus deformity have intrinsic neuromuscular lesions, which require intraoperative adjustment of muscle strength to achieve a new balance of muscle strength to prevent the recurrence of the deformity. However, the efficacy after tendon transposition is challenging to predict and requires careful preoperative evaluation by the surgeon.
The tendons that play a significant role in causing the deformity of Cavovarus are the peroneus longus and peroneus brevis, the tibialis anterior, and the tibialis posterior. Due to the imbalance of internal muscle strength in children with Cavovarus, the strength of the peroneus longus is expected, the strength of the anterior tibialis muscle is weakened or paralyzed, and the peroneus longus loses the antagonism of the anterior tibialis muscle, resulting in the first metatarsal sags. The drop of the first metatarsal increases the longitudinal arch of the medial foot, leading to a deformity of the Cavovarus foot. A similar mechanism occurs in the peroneus brevis and the tibialis tendon. A weakened peroneus brevis muscle and a normal or still strong posterior tibialis tendon can lead to a varus deformity.[
22] Transfer of the peroneal longus to the peroneal brevis is usually performed with bone surgery. It eliminates plantar flexion of the peroneus longus near the first metatarsal, strengthens the valgus of the peroneus Breus, and indirectly improves the function of the tibialis anterior. In children with CMT, the strength of the tibialis anterior dorsalis extension of the ankle joint is weak. Therefore, the relative strength of the tibialis posterior muscle is too strong, leading to varus deformity of the hindfoot [
22,
25,
26].In this case, transferring the posterior tibialis tendon to the anterior tibialis tendon may help the patient realize the ankle joint better and help indirectly correct the posterior varus deformity. Currently, the procedure described by Hsu and Hoffer [
14] for transposition of the posterior tibial tendon consists mainly of four steps: (1) Complete dissection of the posterior tibial tendon from the scaphoid; (2) Create a complete opening on the medial side of the distal tibia to free the posterior tibial tendon completely; (3) The posterior tibial tendon was transferred from the medial incision to the anterior incision, and it was divided into two bundles; (4) The tendon was separated into two bundles, one of which was attached to the lateral cuneus and the other to the peroneus brevis. This kind of operation not only strengthens the strength of the dorsalis extension but also strengthens the strength of the valgus and has a noticeable effect on the orthosis of the Cavovarus deformity. Dreher et al. [
15] divided the posterior tibialis tendon into two bundles, one fixed on the anterior tibialis muscle and the other on the peroneus brevis muscle, significantly improving the range of motion of the ankle joint and achieving a satisfactory postoperative effect.
Invert toe deformity is a concomitant deformity of Cavovarus resulting from arch elevation and muscle imbalance. The Jones operation is currently recognized as a surgical intervention for inverted toe deformities. The procedure involves the transfer of the long and short bunions to the first metatarsal head and, in the presence of Achilles tendon contracture, Achilles tendon lengthening [
16,
28]. However, this surgical method only restricts muscle force redistribution between soft tissues. For existing bone changes, simple soft tissue surgery usually cannot achieve an ideal orthopedic effect, and soft tissue surgery combined with bone surgery is needed to achieve a better orthopedic effect. Therefore, subsequent scholars improved the surgical method. Based on soft tissue surgery, combined with interdigital joint fusion and dorsiflexion proximal first metatarsal osteotomy, the first metatarsal sagging deformity was corrected while correcting the inverted toe deformity of the forefoot. This operation is based on the orthosis of the Cavovarus and is usually performed as a combined operation.
During a mean follow-up of 42 months, Breusch and colleagues reported that 51 patients (81 feet) who underwent Jones tendon transposition had an excellent rate of 86%, most of which were neurogenic Cavovarus malformations [
16].
Erickson et al. [
17] treated 19 patients with CMT with an average age of 12 years using plantar fascia release, tibia-posterior tendon transposition, Jones tendon transposition, and Achilles tendon lengthening. After 2.6 years of follow-up, the patients showed improvements in imaging and gait, and the pressure distribution in the first metatarsal bone was improved, but the plantar pressure was not completely normal. Therefore, according to current studies, the orthotic effect and maintenance of the orthotic effect of soft tissue surgery for children with CMT are limited. Therefore, soft tissue surgery is usually unable to achieve and maintain a good effect for children with CMT, and osteotomy surgery should be added to ensure efficacy.
4.2.3. First metatarsal osteotomy
The metatarsal flexion of the first metatarsal bone increases the longitudinal arch of the medial foot. The aggravation of the metatarsal flexion deformity of the first metatarsal bone leads to the progression of the Cavovarus foot deformity. Therefore, operating the first metatarsal bone is vital in correcting Cavovarus foot deformity. The proximal dorsal wedge osteotomy of the first metatarsal is usually performed in conjunction with plantar fascia release, but Singh and Briggs et al. [
18] reported good results even in the absence of plantar fascia release. The proximal metatarsal epiphysis of the first metatarsal must be protected from injury during the dorsal wedge osteotomy of the proximal first metatarsal in children with high arches, especially in younger children. For children with more severe deformities, the metatarsal wedge osteotomy of the medial cuneus can be added to be closer to the apex of the deformity to achieve a better orthopedic effect. Ward et al. [
19] reported 25 children with high arch varus foot caused by CMT who were treated with a dorsal wedge osteotomy of the first metatarsal, transfer of the peroneus longus to the peroneus brevis, Release of the plantar fascia, transfer of the extensor hallucis longus to the neck of the first metatarsal, and transfer of the anterior tibial tendon to the lateral cuneus in individual cases. The mean follow-up was 26 years, although arthritis was found in 11 patients. However, none of the patients underwent joint fusion surgery. It indicates that the combination of the first metatarsal osteotomy and soft tissue surgery is of great importance for the orthosis of the Cavovarus foot. It not only changes the imbalance of muscle strength but also corrects the malformation of the bone and fully corrects the malformation of the Cavovarus foot, which is conducive to preventing the recurrence of the Cavovarus deformity and maintaining the surgical effect.
4.2.3. Middle foot osteotomy and fusion
Several osteotomy methods for the middle foot have been reported, and different osteotomy methods are selected according to the different characteristics of each patient. Generally, the apex of the Cavovarus foot deformity may be at the navicular cuneiform joint or the medial cuneus and can be corrected by the first metatarsal dorsal wedge osteotomy combined with the first cuneus metatarsal wedge osteotomy. Mubarak et al. [
20] used the first sequence osteotomy to treat stiff high arches with an average age of 11 years. That is, the first step was to perform a closed dorsal wedge osteotomy of 20-30° at the proximal end of the metatarsal head and remove the bone fragments; the second step was to perform an open metatarsal osteotomy of 20-30° at the medial cuneus and put the bone fragments obtained in the first step into the cuneus space. The final follow-up time was 46 months, no serious complications occurred, and both imaging and clinical symptoms were improved.
However, Mosca et al. [
21] advocated using the I-III cuneiform metatarsal wedge osteotomy rather than the first metatarsal osteotomy because the wedge osteotomy was closer to the apex of the deformity. Wicart et al. [
22] used the same surgical method as Mosca to treat 26 children with neurogenic hyper arches foot deformity, followed up for 6.9 years, and achieved good results. He also believes that the I-III cuneiform osteotomy is closer to the apex of the deformity and, due to the presence of the intermetatarsal ligament, may better correct the adductor deformity of the forefoot.
Other methods of a mid-foot osteotomy include Jahss osteotomy, Cole osteotomy, Steindler osteotomy, Japas "V" osteotomy, and fornix osteotomy. In 1968, Japas reported for the first time the use of Japas "V" osteotomy for the posterior treatment of Cavovarus [
29]. It was reported that Japas "V" osteotomy treated 18 adolescents with Cavovarus deformity. After 5.4 years of follow-up, the excellent and good rate reached 77%.[
22]Zhou et al. [
23] reported 17 cases of adolescents and young adults (12-36 years old) who underwent cole midfoot osteotomy, including navicular wedge fusion and dice bone closed wedge osteotomy, combined with percutaneous plantar fascial release treatment. In some of our patients, anchors were used to selectively transfer the posterior tibial tendon through the interosseous membrane to the dorsalis pedis; In the case of horseshoe muscle contracture, the Achilles tendon "Z" lengthening is performed. After the flexor tendon was severed with claw toe deformity, the toe was fixed in the extended state with Kirschner wire. In fixed deformity, distal interphalangeal arthroplasty was performed. After 28 months of follow-up, the curative effect was satisfactory. Mubarak et al. [
24] introduced a salvage operation, which included the excision of the scaphoid bone of the foot and a closed wedge osteotomy of the dorsal cuboid bone in the middle foot. The effect was good within 5 years of follow-up. Through retrospective analysis of recurrent cases, some scholars believe that the key to the postoperative efficacy of middle foot osteotomy surgery lies in determining the malformed apex of the foot deformity, and the osteotomy operation is performed at the malformed apex [
27,
30,
34,
35,
36,
37,
38].
When the therapeutic effect cannot be achieved through the osteotomy, three-joint fusion surgery must be considered, which has become the consensus of most scholars [
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38]. As a last resort for treating Cavovarus, three-joint fusion surgery requires careful evaluation of the patient and a complete understanding of the disease characteristics ofCavovarus and is performed after the child's bone is mature. Barg et al. [
38] reported that 11 patients, with an average age of 62 years and an average follow-up of 36 months, underwent triple joint fusion. The deformity of the Cavovarus was corrected in all patients, and the pain was significantly relieved with satisfactory efficacy. Coleman's test evaluated the presence of a rigid varus deformity in the hind foot of a Cavovarus deformity, requiring calcaneal osteotomy to reduce or correct the varus. Currently, there are many surgical methods for calcaneal osteotomy, but according to current studies, scholars are more inclined to choose Dwyer osteotomy or calcaneal slide osteotomy [
35]. Calcaneal osteotomy is generally used as a supplementary surgical method after orthosis of anterior and middle foot osteotomy, and according to current reports, the curative effect is satisfactory [
22,
35,
36].
In summary, the present Cavovarus foot deformity is relatively complicated, and preoperative physical examination and imaging examination are significant for evaluating Cavovarus foot deformity. However, the selection of surgical methods is controversial, and no one surgical method can be used as a standard surgical treatment. Extensive and long-term studies are needed to confirm the effectiveness of these procedures.
Author Contributions
Writing—original draft preparation, Conceptualization, Writing - review & editing, Data curation and Software, D.T.A.V. Methodology and Data curation ,Investigation and Formal analysis, and
Visualization,Supervision, Project administration.
Informed Consent Statement
The authors declare that the research was conducted without any financial or commercial support, so there cannot be a potential conflict of interest.
Data Availability Statement
The data that support this study’s findings are available in this article.
Acknowledgments
This work would not have been possible without the support colleagues
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Wicart, P. Cavus foot from neonates to adolescents. Orthop Traumatol Surg Res 2012; 98(7):813–28. [CrossRef]
- Ghanem I, Zeller R, Seringe R. The foot in hereditary motor and sensory neuropathies in children. Rev Chir Orthop Reparatrice Appar Mot 1996; 82 (2):152–60.
- Laura M, Singh D, Ramdharry G, et al. Prevalence and orthopedic management of foot and ankle deformities in Charcot-Marie-Tooth disease. Muscle Nerve 2018; 57(2):255–9. [CrossRef]
- Neumann, JA; Nickisch, F; Neurologic Disorders and Cavovarus Deformity.[J].Foot Ankle Clin.2019,24(2):195-203. [CrossRef]
- Hamel J. Corrective procedures and indications for cavovarus foot deformities in children and adolescents. Oper Orthop Traumatol 2017; 29(6):473–82. [CrossRef]
- Perera AG, Guha A. Clinical and radiographic evaluation of the cavus foot: surgical implications. In: Kadakia A, editor. Innovations in the cavus foot deformity, an issue of foot and ankle clinics. 1st edition. Philadelphia: Elsevier; 2013. p. 619–88.
- Pin T, Dyke P, Chan M. The effectiveness of passive stretching in children with cerebral palsy. Dev Med Child Neurol 2006; 48(10):855–62. [CrossRef]
- Maas J, Dallmeijer A, Huijing P, et al. A randomized controlled trial studying efficacy and tolerance of a knee-ankle-foot orthosis used to prevent equinus in children with spastic cerebral palsy. Clin Rehabil 2014; 28(10):1025–38. [CrossRef]
- d’Astorg H, Rampal V, Seringe R, et al. Is non-operative management of childhood neurologic cavovarus foot effective? Orthop Traumatol Surg Res 2016; 102(8):1087–91. [CrossRef]
- Burns J, Scheinberg A, Ryan MM, et al. Randomized trial of botulinum toxin to prevent pes cavus progression in pediatric Charcot-Marie-Tooth disease type 1A. Muscle Nerve 2010; 42(2):262–7. [CrossRef]
- Tiffreau V, Allart E, Dangleterre C, et al. Botulinum toxin treatment of pes cavovarus in a child suffering from autosomal recessive axonal Charcot-Marie-Tooth neuropathy (AR-CMT2). Eur J Phys Rehabil Med 2015; 51(3):345–9.
- Kwon YU, Kim HW, Hwang JH, et al. Changes in dynamic pedobarography after extensive plantarmedial release for paralytic pes cavovarus. Yonsei Med J 2014; 55(3):766–72. [CrossRef]
- Sanpera I Jr, Frontera-Juan G, Sanpera-Iglesias J, et al. Innovative treatment for pes cavovarus: a pilot study of 13 children. Acta Orthop 2018; 89(6):668–73. [CrossRef]
- Hsu J, Hoffer M. Posterior tibial tendon transfer anteriorly through the interosseous membrane: a modification of the technique. Clin Orthop Relat Res. 1978:131; 202-204.
- Dreher T, Wolf SI, Heitzmann D, et al. Tibialis posterior tendon transfer corrects the foot drop component of cavovarus foot deformity in Charcot-Marie-Tooth disease. J Bone Joint Surg Am 2014; 96(6):456–62. [CrossRef]
- Breusch SJ, Wenz W, Doderlein L. Function after correction of a clawed great toe by a modified Robert Jones transfer. J Bone Joint Surg Br 2000; 82(2):250–4. [CrossRef]
- Erickson S, Hosseinzadeh P, Iwinski HJ, et al. Dynamic pedobarography and radiographic evaluation of surgically treated cavovarus foot deformity in children with Charcot-Marie-Tooth disease. J Pediatr Orthop 2015; 24 (4): 336–40. [CrossRef]
- Singh AK, Briggs PJ. Metatarsal extension osteotomy without plantar aponeurosis release in cavus feet. The effect on claw toe deformity a radiograp-hic assessment. Foot Ankle Surg 2012; 18(3):210–2. [CrossRef]
- Ward CM, Dolan LA, Bennett DL, et al. Long-term results of reconstruction for treatment of a flexible cavovarus foot in Charcot-Marie-Tooth disease. J Bone Joint Surg Am 2008; 90(12):2631–42. [CrossRef]
- Mubarak SJ, Van Valin SE. Osteotomies of the foot for cavus deformities in children. J Pediatr Orthop 2009; 29(3):294–9. [CrossRef]
- Harrasser N, Lenze F. Cavovarus foot.[J]. Orthopade.2021,50(1):75-85. [CrossRef]
- Wicart P, Seringe R. Plantar opening-wedge osteotomy of cuneiform bones combined with selective plantar release and Dwyer osteotomy for pes cavovarus in children. J Pediatr Orthop 2006; 26(1):100–8. [CrossRef]
- Zhou Y, Zhou B, Liu J, et al. A prospective study of midfoot osteotomy combined with adjacent joint sparing internal fixation in treatment of rigid pes cavus deformity. J Orthop Surg Res 2014; 9:44. [CrossRef]
- Mubarak SJ, Van Valin SE. Osteotomies of the foot for cavus deformities in children. J Pediatr Orthop 2009; 29(3):294–9. [CrossRef]
- Krhenbühl N, Weinberg MW. Anatomy and Biomechanics of Cavovarus Deformity.J Foot Ankle Clin.2019,24(2):173-181. [CrossRef]
- Neumann A, Nickisch F.Neurologic Disorders and Cavovarus Deformity. [J].Foot Ankle Clin.2019,24(2):195-203. [CrossRef]
- Wallroth A, Dreher T. Components of the joint-sparing, combined bony and soft tissue correction of the cavovarus foot.J Oper Orthop Traumatol. 2018,30(4):286-292. [CrossRef]
- Abbasian A, Pomeroy G. The idiopathic cavus foot-not so subtle after all. Foot Ankle Clin 2013; 18(4):629–42. [CrossRef]
- Japas LM. Surgical treatment of pes cavus by tarsal V-osteotomy. Preliminary report. J Bone Joint Surg Am 1968; 50(5):927–44.
- Chen Y, Wu Y, An H.Soft tissue release combined with joint-sparing osteotomy for treatment of cavovarus foot deformity in older children: Analysis of 21 cases.J World J Clin Cases.2019,7(20):3208-3216. [CrossRef]
- Lin T, Gibbons P, Mudge AJ.Surgical outcomes of cavovarus foot deformity in children with Charcot-Marie-Tooth disease. J Neuromuscul Disord; 201 9,29(6):427-436. [CrossRef]
- Kaplan M, Aiyer A, Cerrato A, et al.Operative Treatment of the Cavovarus Foot.J Foot Ankle Int.2018,39(11):1370-1382. [CrossRef]
- O’Malley M, DeSandis B, Allen A, et al. Operative treatment of fifth metatarsal Jones fractures (zones II and III) in the NBA. Foot Ankle Int 2016; 37(5):488–500. [CrossRef]
- Raikin, SM; Parekh, SG; Avoiding Failure and Complications in Cavovarus Foot Deformity Reconstruction.J Instr Course Lect.2018,67(1):269-274.
- Marks RM. Midfoot and forefoot issues cavovarus foot: assessment and treatment issues. Foot Ankle Clin 2008; 13(2):229–41. [CrossRef]
- Myerson S, Myerson L.Cavus Foot: Deciding Between Osteotomy and Arthrodesis.J Foot Ankle Clin.2019,24(2):347-360. [CrossRef]
- Kaplan M, Aiyer A, Cerrato A.Operative Treatment of the Cavovarus Foot.J Foot Ankle Int. 2018,39(11):1370-1382. [CrossRef]
- Barg A, Ruiz R, Hintermann, B. Triple arthrodesis for correction of cavovarus deformity.J Oper Orthop Traumatol.2017; 29(6):461-472. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).