Submitted:
10 March 2023
Posted:
16 March 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Study design
Participants recruitment and eligibility criteria
Demographic and health data
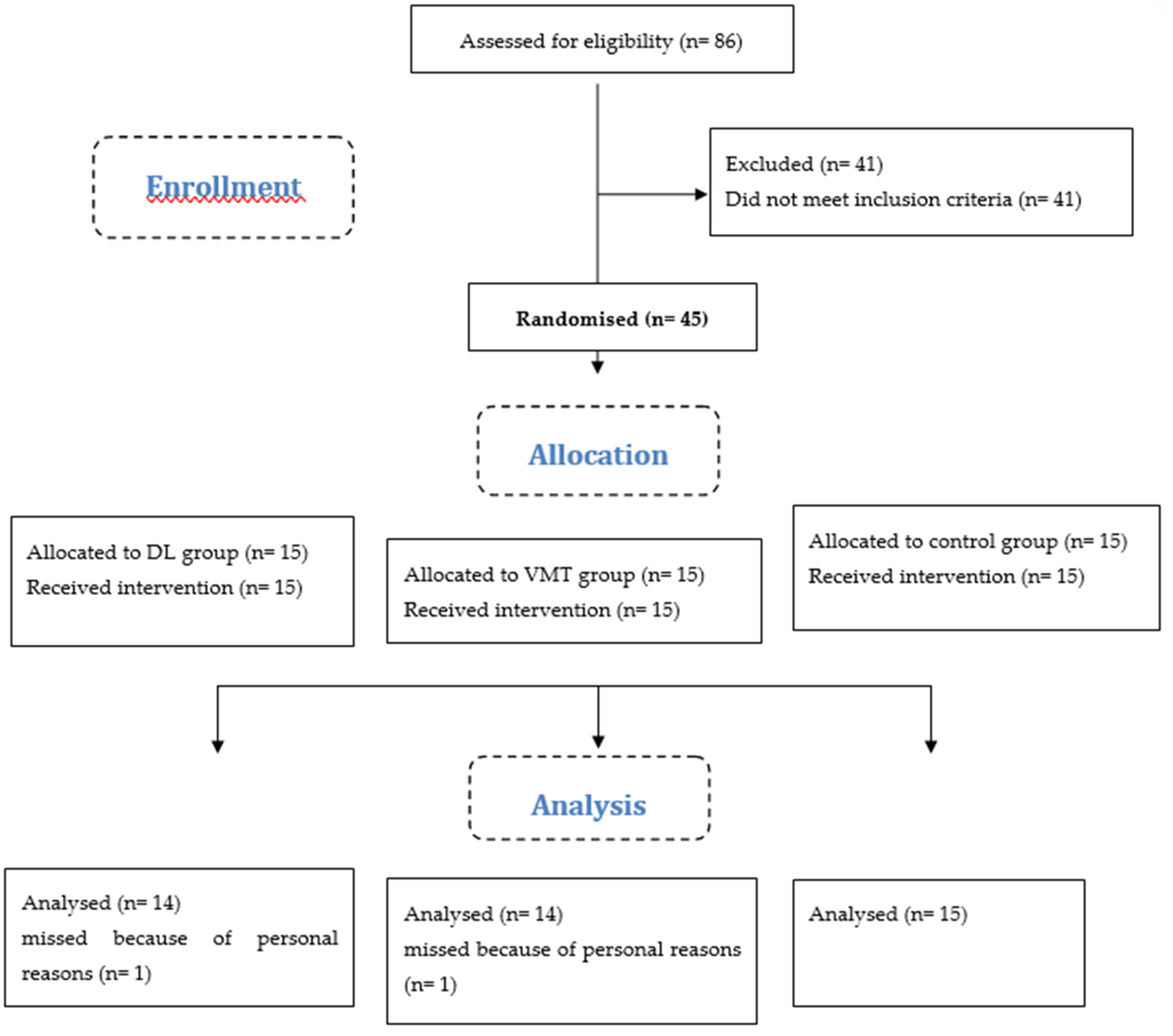
Randomization, allocation, and implementation
Sample size calculation
Procedures
Primary outcome measure
Functional performance (triple hop test)
Secondary outcome measures
Dynamic balance (Star Excursion Balance Test)
Biomechanics during single-leg drop-landing task
Data collection
Kinesiophobia (TSK)
Interventions
Differential learning (DL)
Visual-motor training (VMT)
Control
Statistical analysis
Results
Functional performance (triple hop test)
Dynamic balance (SEBT)
Biomechanics (hip and knee flexion, ankle dorsiflexion, knee valgus, and VGRF)
Kinesiophobia (TSK)
Discussion
Prospect
Conclusion
Author Contributions
Funding
Institutional review board statement
Informed Consent statement
Data availability statement
Acknowledgements
Conflicts of interest
References
- Gokeler A, Dingenen B, Hewett TE. Rehabilitation and return to sport testing after anterior cruciate ligament reconstruction: where are we in 2022? Arthrosc Sport Med Rehabil. 2022;4(1):e77–82. [CrossRef]
- Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–76. [CrossRef]
- Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53(18):1162–7. [CrossRef] [PubMed]
- Thomee P, Währborg P, Börjesson M, Thomee R, Eriksson BI, Karlsson J. Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports. 2007;17(3):238–45. [CrossRef]
- Gokeler A, Schmalz T, Knopf E, Freiwald J, Blumentritt S. The relationship between isokinetic quadriceps strength and laxity on gait analysis parameters in anterior cruciate ligament reconstructed knees. Knee Surgery, Sport Traumatol Arthrosc. 2003;11:372–8. [CrossRef] [PubMed]
- Paterno M V, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258–62. [CrossRef]
- Gokeler A, Hof AL, Arnold MP, Dijkstra PU, Postema K, Otten E. Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports. 2010;20(1):e12–9. [CrossRef]
- Salgarello M, Visconti G, Barone-Adesi L. Interlocking circumareolar suture with undyed polyamide thread: a personal experience. Aesthetic Plast Surg. 2013;37:1061–2. [CrossRef]
- Dingenen B, Janssens L, Luyckx T, Claes S, Bellemans J, Staes FF. Postural stability during the transition from double-leg stance to single-leg stance in anterior cruciate ligament injured subjects. Clin Biomech. 2015;30(3):283–9. [CrossRef]
- Simoneau GG, Wilk KE. The challenge of return to sports for patients post-ACL reconstruction. JOSPT, Inc. JOSPT, 1033 North Fairfax Street, Suite 304, Alexandria, VA …; 2012.
- Øiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–10. [CrossRef]
- Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40(2):215–22. [CrossRef] [PubMed]
- Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of motor learning to support neuroplasticity after ACL injury: implications for optimizing performance and reducing risk of second ACL Injury. Sport Med. 2019;49(6):853–65. [CrossRef] [PubMed]
- Stergiou N, Harbourne RT, Cavanaugh JT. Optimal movement variability: a new theoretical perspective for neurologic physical therapy. J Neurol Phys Ther. 2006;30(3):120–9. [CrossRef]
- Schöllhorn WI, Beckmann H, Michelbrink M, Sechelmann M, Trockel M, Davids K. Does noise provide a basis for the unification of motor learning theories? Int J Sport Psychol. 2006;37(2/3):186.
- Kal E. Prosé e R, Winters M, Van Der Kamp J. Does implicit motor learning lead to greater automatization of motor skills compared to explicit motor learning? a systematic review. PLoS One. 2018;13(9):e0203591. [CrossRef]
- Ghanati HA, Letafatkar A, Shojaedin S, Hadadnezhad M, Schöllhorn WI. Comparing the Effects of Differential Learning, Self-Controlled Feedback, and External Focus of Attention Training on Biomechanical Risk Factors of Anterior Cruciate Ligament (ACL) in Athletes: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19(16):10052. [CrossRef]
- Schöllhorn WI. Individualität-ein vernachlässigter Parameter. Leistungssport; 1999.
- Liao C-M, Masters RSW. Analogy learning: A means to implicit motor learning. J Sports Sci. 2001;19(5):307–19. [CrossRef] [PubMed]
- Maxwell JP, Masters RSW, Kerr E, Weedon E. The implicit benefit of learning without errors. Q J Exp Psychol Sect A. 2001;54(4):1049–68.
- Schöllhorn,WI, Horst F. Effects of complex movements on the brain as a result of increased decision-making. J Complex Heal Sci. 2019;2(2):40–5. [CrossRef]
- Schöllhorn WI, Mayer-Kress G, Newell KM, Michelbrink M. Time scales of adaptive behavior and motor learning in the presence of stochastic perturbations. Hum Mov Sci. 2009;28(3):319–33. [CrossRef]
- Henz D, Schöllhorn WI. Differential training facilitates early consolidation in motor learning. Front Behav Neurosci. 2016;10:199. [CrossRef]
- Henz D, John A, Merz C, Schöllhorn WI. Post-task effects on EEG brain activity differ for various differential learning and contextual interference protocols. Front Hum Neurosci. 2018;19. [CrossRef]
- Schöllhorn WI, Rizzi N, Slapšinskaitė-Dackevičienė A, Leite N. Always Pay Attention to Which Model of Motor Learning You Are Using. Int J Environ Res Public Health. 2022;19(2):711. [CrossRef] [PubMed]
- Schöllhorn WI, Bauer HU. Identifying individual movement styles in high performance sports by means of self-organizing Kohonen maps. In: ISBS-conference proceedings archive. 1998.
- Apidogo JB, Burdack J, Schöllhorn WI. Learning Multiple Movements in Parallel—Accurately and in Random Order, or Each with Added Noise? Int J Environ Res Public Health. 2022;19(17):10960. [CrossRef]
- Nitsch JR, Hackfort D. Streß in Schule und Hochschule-eine handlungspsychologische Funktionsanalyse. Streß Theor Untersuchungen, Maßnahmen Bern. 1981;263–311.
- Hackfort D. Commentary on “Towards a Grand Unified Theory of sports performance.” Hum Mov Sci. 2017;56:166–8. [CrossRef] [PubMed]
- Cube F von. Kybernetische Grundlagen des Lernens und Lehrens. 1965;
- Schöllhorn WI, Beckmann H, Davids K. Exploiting system fluctuations. Differential training in physical prevention and rehabilitation programs for health and exercise. Medicina (B Aires). 2010;46(6):365. [CrossRef] [PubMed]
- Repšaitė V, Vainoras A, Berškienė K, Baltaduonienė D, Daunoravičienė A, Sendžikaitė E. The effect of differential training-based occupational therapy on hand and arm function in patients after stroke: Results of the pilot study. Results of the pilot study. Neurol Neurochir Pol. 2015;49(3):150–5. [CrossRef] [PubMed]
- Rosset-Llobet J, Fàbregas-Molas S. Rehabilitation and plasticity of task-specific focal hand dystonia. Treat Dystonia; Dressler, D, Altenmüller, E, Krauss, JK, Eds. 2018;256–60.
- Kurz J, Gosenheimer A, Schumann-Schmid B, Steinmetz F, Schöllhorn WI. Differenzielles Gangtraining in der stationären Rehabilitation bei Knie-oder Hüft-TEP. B&G Bewegungstherapie und Gesundheitssport. 2016;32(06):221–5. [CrossRef]
- Quaney BM, He J, Timberlake G, Dodd K, Carr C. Visuomotor training improves stroke-related ipsilesional upper extremity impairments. Neurorehabil Neural Repair. 2010;24(1):52–61. [CrossRef]
- Eng K, Siekierka E, Pyk P, Chevrier E, Hauser Y, Cameirao M, et al. Interactive visuo-motor therapy system for stroke rehabilitation. Med Biol Eng Comput. 2007;45:901–7. [CrossRef]
- Bigsby K, Mangine RE, Clark JF, Rauch JT, Bixenmann B, Susaret AW, et al. Effects of postural control manipulation on visuomotor training performance: comparative data in healthy athletes. Int J Sports Phys Ther. 2014;9(4):436. [PubMed]
- Grooms D, Appelbaum G, Onate J. Neuroplasticity following anterior cruciate ligament injury: a framework for visual-motor training approaches in rehabilitation. J Orthop Sport Phys Ther. 2015;45(5):381–93. [CrossRef]
- Wohl TR, Criss CR, Grooms DR. Visual perturbation to enhance return to sport rehabilitation after anterior cruciate ligament injury: a clinical commentary. Int J Sports Phys Ther. 2021;16(2):552. [CrossRef] [PubMed]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9(8).
- Shrestha B, Dunn L. The declaration of Helsinki on medical research involving human subjects: a review of seventh revision. J Nepal Health Res Counc. 2019;17(4):548–52. [CrossRef]
- Sturgill LP, Snyder-Mackler L, Manal TJ, Axe MJ. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sport Phys Ther. 2009;39(12):845–9. [CrossRef]
- Meierbachtol A, Yungtum W, Paur E, Bottoms J, Chmielewski TL. Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction. J Orthop Sport Phys Ther. 2018;48(11):864–72. [CrossRef] [PubMed]
- Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury–Prevention Program in Elite-Youth Soccer Athletes. J Athl Train [Internet]. 2015;50(6):589–95. [CrossRef]
- Cohen J. Statistical power analysis for the behavioral sciences. Routledge; 2013.
- Sheikhi B, Letafatkar A, Thomas AC, Ford KR. Altered trunk and lower extremity movement coordination after neuromuscular training with and without external focus instruction: a randomized controlled trial. BMC Sports Sci Med Rehabil. 2021;13(1):1–9. [CrossRef]
- Dingenen B, Truijen J, Bellemans J, Gokeler A. Test–retest reliability and discriminative ability of forward, medial and rotational single-leg hop tests. Knee. 2019;26(5):978–87. [CrossRef]
- Munro AG, Herrington LC. Between-session reliability of the star excursion balance test. Phys Ther Sport. 2010;11(4):128–32. [CrossRef] [PubMed]
- Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. [CrossRef]
- Nagelli C V, Di Stasi S, Wordeman SC, Chen A, Tatarski R, Hoffman J, et al. Knee biomechanical deficits during a single-leg landing task are addressed with neuromuscular training in anterior cruciate ligament–reconstructed athletes. Clin J Sport Med. 2021;31(6):e347–53. [CrossRef] [PubMed]
- Harriman SL, Patel J. When are clinical trials registered? An analysis of prospective versus retrospective registration. Trials. 2016;17(1):1–8. [CrossRef]
- Wilkins L, Appelbaum LG. An early review of stroboscopic visual training: insights, challenges and accomplishments to guide future studies. Int Rev Sport Exerc Psychol. 2020;13(1):65–80. [CrossRef]
- Welling W, Benjaminse A, Gokeler A, Otten B. Enhanced retention of drop vertical jump landing technique: a randomized controlled trial. Hum Mov Sci. 2016;45:84–95. [CrossRef]
- Stensrud S, Myklebust G, Kristianslund E, Bahr R, Krosshaug T. Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. Br J Sports Med. 2011;45(7):589–95. [CrossRef]
- Oftadeh S, Bahram A, Yaali R, Ghadiri F, Schöllhorn WI. External Focus or Differential Learning: Is There an Additive Effect on Learning a Futsal Goal Kick? Int J Environ Res Public Health. 2021;19(1):317. [CrossRef]
- Silverman S. Communication and motor skill learning: What we learn from research in the gymnasium. Quest. 1994;46(3):345–55. [CrossRef]
- Fuchs PX, Fusco A, Bell JW, von Duvillard SP, Cortis C, Wagner H. Effect of differential training on female volleyball spike-jump technique and performance. Int J Sports Physiol Perform. 2020;15(7):1019–25. [CrossRef]
- Newell KM. Schema theory (1975): Retrospectives and prospectives. Res Q Exerc Sport. 2003;74(4):383–8. [CrossRef] [PubMed]
- Dhawale AK, Smith MA, Ölveczky BP. The role of variability in motor learning. Annu Rev Neurosci. 2017;40:479–98. [CrossRef]
- Kotsifaki A, Korakakis V, Whiteley R, Van Rossom S, Jonkers I. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2020;54(3):139–53. [CrossRef] [PubMed]
- Tran AA, Gatewood C, Harris AHS, Thompson JA, Dragoo JL. The effect of foot landing position on biomechanical risk factors associated with anterior cruciate ligament injury. J Exp Orthop. 2016;3(1):1–7. [CrossRef]
- Ghanati HA, Letafatkar A, Abbasi A. Effect of Motor Learning Strategies Exercises on Peak Hip Abduction Moment, Peak Knee Valgus Angle and Performance in Active Participants. J Clin Physiother Res. 2018;3(1):21–8. [CrossRef]
- Kotsifaki A, Whiteley R, Van Rossom S, Korakakis V, Bahr R, Sideris V, et al. Single leg hop for distance symmetry masks lower limb biomechanics: time to discuss hop distance as decision criterion for return to sport after ACL reconstruction? Br J Sports Med. 2022;56(5):249–56. [CrossRef]
- Dobija L, Reynaud V, Pereira B, Van Hille W, Descamps S, Bonnin A, et al. Measurement properties of the Star Excursion Balance Test in patients with ACL deficiency. Phys Ther Sport. 2019;36:7–13. [CrossRef] [PubMed]
- Michelbrink M, Schöllhorn WI. Changes in noise structure by learning a balancing tasks. J Biomech. 2006;(39):S483. [CrossRef]
- Michelbrink M, Schöllhorn WI. 22.23 Differencial learning and random walk analysis inhuman balance. Gait Posture. 2005;(21):S148–9. [CrossRef]
- Wind J, Horst F, Rizzi N, John A, Schöllhorn WI. Electrical brain activity and its functional connectivity in the physical execution of modern jazz dance. Front Psychol. 2020;11:586076. [CrossRef]
- John AT, Barthel A, Wind J, Rizzi N, Schöllhorn WI. Acute Effects of Various Movement Noise in Differential Learning of Rope Skipping on Brain and Heart Recovery Analyzed by Means of Multiscale Fuzzy Measure Entropy. Front Behav Neurosci. 2022;16:20. [CrossRef] [PubMed]
- Grooms DR, Chaudhari A, Page SJ, Nichols-Larsen DS, Onate JA. Visual-motor control of drop landing after anterior cruciate ligament reconstruction. J Athl Train. 2018;53(5):486–96. [CrossRef] [PubMed]
- Appelbaum LG, Schroeder JE, Cain MS, Mitroff SR. Improved visual cognition through stroboscopic training. Front Psychol. 2011;2:276. [CrossRef] [PubMed]
- Appelbaum LG, Cain MS, Schroeder JE, Darling EF, Mitroff SR. Stroboscopic visual training improves information encoding in short-term memory. Attention, Perception, Psychophys. 2012;74:1681–91. [CrossRef] [PubMed]
- Dale RB, Gollapalli RP, Price T, Megahee K, Duncan M, Tolstick N, et al. The effect of visual perturbation upon femoral acceleration during the single and bilateral squat. Phys Ther Sport. 2017;27:24–8. [CrossRef] [PubMed]
- Mitroff SR, Friesen P, Bennett D, Yoo H, Reichow AW. Enhancing ice hockey skills through stroboscopic visual training: a pilot study. Athl Train Sport Heal Care. 2013;5(6):261–4. [CrossRef]
- Wilkins L, Gray R. Effects of stroboscopic visual training on visual attention, motion perception, and catching performance. Percept Mot Skills. 2015;121(1):57–79. [CrossRef]
- Hülsdünker T, Rentz C, Ruhnow D, Käsbauer H, Strüder HK, Mierau A. The effect of 4-week stroboscopic training on visual function and sport-specific visuomotor performance in top-level badminton players. Int J Sports Physiol Perform. 2019;14(3):343–50. [CrossRef]
- Scherzer CB, Brewer BW, Cornelius AE, Van Raalte JL, Petitpas AJ, Sklar JH, et al. Psychological skills and adherence to rehabilitation after reconstruction of the anterior cruciate ligament. J Sport Rehabil. 2001;10(3):165–72. [CrossRef]
- Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–8. [CrossRef]
- Culliton SE, Bryant DM, Overend TJ, MacDonald SJ, Chesworth BM. The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty. 2012;27(3):490–2. [CrossRef] [PubMed]
- Waljee J, McGlinn EP, Sears ED, Chung KC. Patient expectations and patient-reported outcomes in surgery: a systematic review. Surgery. 2014;155(5):799–808. [CrossRef] [PubMed]
- Pizzari T, McBurney H, Taylor NF, Feller JA. Adherence to anterior cruciate ligament rehabilitation: a qualitative analysis. J Sport Rehabil. 2002;11(2):90–102. [CrossRef]
- Chaput M, Ness BM, Lucas K, Zimney KJ. A Multi-Systems Approach to Human Movement after ACL Reconstruction: The Nervous System. Int J Sports Phys Ther. 2022;17(1):47–59. [CrossRef]
- Herman DC, Barth JT. Drop-jump landing varies with baseline neurocognition: implications for anterior cruciate ligament injury risk and prevention. Am J Sports Med. 2016;44(9):2347–53. [CrossRef]
- Monfort SM, Pradarelli JJ, Grooms DR, Hutchison KA, Onate JA, Chaudhari AMW. Visual-Spatial Memory Deficits Are Related to Increased Knee Valgus Angle During a Sport-Specific Sidestep Cut. Am J Sports Med. 2019;47(6):1488–95. [CrossRef] [PubMed]
- Swanik CB, Covassin T, Stearne DJ, Schatz P. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med. 2007;35(6):943–8. [CrossRef] [PubMed]
- Avedesian JM, Forbes W, Covassin T, Dufek JS. Influence of cognitive performance on musculoskeletal injury risk: A systematic review. Am J Sports Med. 2022;50(2):554–62. [CrossRef]
- Halperin I, Chapman DW, Martin DT, Abbiss C, Wulf G. Coaching cues in amateur boxing: an analysis of ringside feedback provided between rounds of competition. Psychol Sport Exerc. 2016;25:44–50. [CrossRef]
- Porter JM, Nolan RP, Ostrowski EJ, Wulf G. Directing attention externally enhances agility performance: A qualitative and quantitative analysis of the efficacy of using verbal instructions to focus attention. Front Psychol. 2010;1:216. [CrossRef]
- Durham K, Van Vliet PM, Badger F, Sackley C. Use of information feedback and attentional focus of feedback in treating the person with a hemiplegic arm. Physiother Res Int. 2009;14(2):77–90. [CrossRef]
- Hunt C, Paez A, Folmar E. The impact of attentional focus on the treatment of musculoskeletal and movement disorders. Int J Sports Phys Ther. 2017;12(6):901. [CrossRef]
- Wulf G, Lauterbach B, Toole T. The learning advantages of an external focus of attention in golf. Res Q Exerc Sport. 1999;70(2):120–6. [CrossRef] [PubMed]
- Baddeley AD, Thomson N, Buchanan M. Word length and the structure of short-term memory. J Verbal Learning Verbal Behav. 1975;14(6):575–89. [CrossRef]
- Baddeley AD, Hitch GJ, Allen RJ. From short-term store to multicomponent working memory: The role of the modal model. Mem Cognit. 2019;47:575–88. [CrossRef]
- Schollhorn WI, Hegen P, Davids K. The nonlinear nature of learning-A differential learning approach. Open Sports Sci J. 2012;5(1).
- Ghaderi M, Letafatkar A, Thomas AC, Keyhani S. Effects of a neuromuscular training program using external focus attention cues in male athletes with anterior cruciate ligament reconstruction: a randomized clinical trial. BMC Sports Sci Med Rehabil. 2021;13(1):1–11. [CrossRef] [PubMed]
- Masters RSW, Poolton JM, Maxwell JP, Raab M. Implicit motor learning and complex decision making in time-constrained environments. J Mot Behav. 2008;40(1):71–9. [CrossRef] [PubMed]
- McNevin NH, Wulf G, Carlson C. Effects of attentional focus, self-control, and dyad training on motor learning: implications for physical rehabilitation. Phys Ther. 2000;80(4):373–85. [CrossRef] [PubMed]
- Kelso JAS. Dynamic patterns: The self-organization of brain and behavior. MIT press; 1995.
- Schöllhorn WI. Practical consequences of systems dynamic approach to technique and strength training. Acta Acad Olympique Est. 2000;8:25–37.
- Schöllhorn WI. Practical consequences of biomechanically determined individuality and fluctuations on motor learning. In: Conference proceedings of the international society of biomechanics Calgary: University press. 1999.
- Singer W. Development and plasticity of cortical processing architectures. Science (80- ). 1995;270(5237):758–64. [CrossRef]
- Schöllhorn W. Systemdynamische Betrachtung komplexer Bewegungsmuster im Lernprozeß: prozeßorientierte Strukturierung der Entwicklung eines Bewegungsablaufs mit Hilfe biomechanischer Beschreibungsgrößen. Lang; 1998.
- Smith LB, Thelen EE. A dynamic systems approach to development: Applications. In: This book grew out of a workshop," Dynamic Systems in Development," held for the Society for Research in Child Development in Kansas City, KS, Apr 1989. The MIT Press; 1993.
- Wade MG, Whiting HTA. Motor development in children: Aspects of coordination and control. Nijhoff; 1986.
- Horst F, Janssen D, Beckmann H, Schöllhorn WI. Can individual movement characteristics across different throwing disciplines be identified in high-performance decathletes? Front Psychol. 2020;11:2262. [CrossRef]
- Aragonés D, Eekhoff A, Horst F, Schöllhorn WI. Fatigue-related changes in technique emerge at different timescales during repetitive training. J Sports Sci. 2018;36(11):1296–304. [CrossRef] [PubMed]
- Burdack J, Horst F, Aragonés D, Eekhoff A, Schöllhorn WI. Fatigue-related and timescale-dependent changes in individual movement patterns identified using support vector machine. Front Psychol. 2020;11:551548. [CrossRef] [PubMed]
- Horst F, Eekhoff A, Newell KM, Schöllhorn WI. Intra-individual gait patterns across different time-scales as revealed by means of a supervised learning model using kernel-based discriminant regression. PLoS One. 2017;12(6):e0179738. [CrossRef] [PubMed]
- Horst F, Mildner M, Schöllhorn WI. One-year persistence of individual gait patterns identified in a follow-up study–A call for individualised diagnose and therapy. Gait Posture. 2017;58:476–80. [CrossRef] [PubMed]
- Horst F, Kramer F, Schäfer B, Eekhoff A, Hegen P, Nigg BM, et al. Daily changes of individual gait patterns identified by means of support vector machines. Gait Posture. 2016;49:309–14. [CrossRef] [PubMed]
- Newell KM, McDonald P V. Searching for solutions to the coordination function: Learning as exploratory behavior. 1992;
- Pacheco MM, Lafe CW, Newell KM. Search strategies in the perceptual-motor workspace and the acquisition of coordination, control, and skill. Front Psychol. 2019;10:1874. [CrossRef] [PubMed]
- Koffka K. Perception: an introduction to the Gestalt-Theorie. Psychol Bull. 1922;19(10):531. [CrossRef]
- Newell KM. Constraints on the development of coordination. Mot Dev Child Asp Coord Control. 1986;
- Mosston M. Inclusion and exclusion in education—II. Innov Curric Des Phys Educ. 1969.
- Behzadnia B, Mohammadzadeh H, Ahmadi M. Autonomy-supportive behaviors promote autonomous motivation, knowledge structures, motor skills learning and performance in physical education. Curr Psychol. 2019;38:1692–705. [CrossRef]
- Fisher R. Statistical methods and scientific induction. J R Stat Soc Ser B. 1955;17(1):69–78. [CrossRef]
- Neyman J, Pearson ES. IX. On the problem of the most efficient tests of statistical hypotheses. Philos Trans R Soc London Ser A, Contain Pap a Math or Phys Character. 1933;231(694–706):289–337. [CrossRef]
- Stegmüller W. Personelle und statistische Wahrscheinlichkeit [Personal and statistical probability] Probleme und Resultate der Wissenschaftstheorie und analytischen Philosophie [Problems and results of philosophy of science and analytical philosophy]. Berlin, Heidelberg, New York: Springer; 1973.
- Nuzzo R. Statistical errors: P values, the’gold standard’of statistical validity, are not as reliable as many scientists assume. Nature. 2014;506(7487):150–3. [CrossRef] [PubMed]
- Gigerenzer G. Mindless statistics. J Socio Econ. 2004;33(5):587–606. [CrossRef]
- Weiss WM, Uguento AM, Mahmooth Z, Murray LK, Hall BJ, Nadison M, et al. Mental health interventions and priorities for research for adult survivors of torture and systematic violence: a review of the literature. Torture J. 2016;26(1):27. [CrossRef]
| Groups | CLT (n=15) | VMT (n=15) | Control (n=15) | p-value* |
|---|---|---|---|---|
| Age (years) | 28.86 (4.68) | 29.13 (3.79) | 27.93 (2.96) | 0.67 |
| Mass (kg) | 78.46 (6.01) | 77.01 (4.84) | 79.05 (4.91) | 0.56 |
| Height (cm) | 175.26 (4.75) | 174.06 (4.60) | 174.33 (3.97) | 0.71 |
| Body mass index (kg/m^2) | 22.41 (1.99) | 22.12 (1.44) | 22.69 (1.52) | 0.64 |
| Time since surgery (months) | 8.5 ±1.1 | 8.8 ±1.2 | 7.8 ±1.5 | 0.39 |
| Internal Variants: | External Variants: |
| Cognition/Coordination-oriented Before jumping:
Fatigue:
|
With primary stimulations of sensory system (apperception): Visual:
|
| Exercise | Visual Cues | |
| Tap-test | Tap the cones Acoustic Cue |
The Tap-test requires the athlete to run 10 m to tap a cone, cut to the right or left for 5 m to tap another cone, cut to the opposite direction for 10 m to tap the third cone, return to the center by cutting 5 m to tap the first cone and then run 10 m back to the start position – thereby running in a “T” formation). A modification that increases the difficulty of this task and simulates the cognitive demands of sport is to have the clinician call out “Left” or “Right” to indicate which direction the athlete should cut prior to reaching the first cone, thereby creating an unanticipated cutting task which has been previously associated with increased injury-risk biomechanics compared to anticipated trials. |
| Agility Ladder Drills | The confines of the ladder | Agility ladder drills require athletes to match specific foot-placement patterns within an agility ladder context. |
| Single-leg Deadlifts | Place an object by the cone(s) | Single-leg deadlifts may be modified by requiring athletes to gently place a small object on the ground next to a cone target. To increase the difficulty, multiple cones can be placed at different angles within the athlete’s field of view, set at distances equal to his or her max volitional reaching distance while standing on one leg. For example, if the clinician chooses to use three targets, then he or she may call out “Left,” “Center,” or “Right” to vary the task order and difficulty. |
| Single-leg Stance (on foam) | Hold the bar horizontally | Single-leg stance on a foam surface may be modified by having the participant hold a light-weight bar with an outstretched arm and focus on keeping it steadily horizontal |
| Vertical Jumps | Hit the overhead target | The VERTEC is a therapeutic tool that assesses maximum vertical jump height by requiring athletes to jump and hit an overhead target. While using the VERTEC to have athletes hit the mark equal to 80% of their maximal jump height, clinicians may call out “Left” or “Right” during the initial flight phase of the jump to signal to the athlete to unilaterally land on his or her left or right leg. The use of spontaneous cuing creates an unanticipated landing task, which has been previously associated with increased injury-risk biomechanics compared to anticipated landing. |
| Squat Jumps | Land facing the cones | Jump squats may be modified by placing four cones around the participant at 0, 90, 180 and 270-degree positions (Figure 1F). After numbering each cone one through four, the clinician may then rapidly call out cues to the athlete to specify which cone they should face after each jump squat. To increase the difficulty of this cognitive challenge, the clinician can introduce more cones or increase the rapidity of cuing. |
| Exercise | Error Count |
| T-test | Miss a cone Cut to the wrong direction |
| Agility Ladder Drills | Hit the ladder Incorrect foot placement |
| Single-leg Deadlifts | Opposite foot touches ground Either hand touches ground Object placed in wrong location |
| Single-leg Stance (on foam) | Opposite foot touches ground Either hand touches ground |
| Vertical Jumps | Miss the target Land on wrong foot |
| Squat Jumps | Land facing wrong orientation |
| Variable | Group | Pre-test Mean ± SD |
post-test Mean ± SD |
ES (CI95%) † |
P value | ||
|---|---|---|---|---|---|---|---|
| Main effect of time | Main effect of group | Group × time interaction | |||||
| Triple hop test (cm) | DL | 457.3±51.2 | 531.3±74.4 ‡ § | 1.15 ! (0.06 to 2.25) |
F=16.226 p <0.001* |
F=2.609 p <0.085 |
F=3.861 p <0.029* |
| VMT | 456.4±54 | 517.6±78.9 ‡ | 0.90 ! (-0.15 to 1.96) |
||||
| Control | 455.6±51 | 457.4±51.1 | 0.03 (-0.97 to 1.04) |
||||
| Variables (cm) |
group | Pre-test Mean ± SD |
8-weeks Mean ± SD |
ES (CI95%) † |
P value | ||
|---|---|---|---|---|---|---|---|
| Main effect of time | Main effect of group | Group × time interaction | |||||
| Anterior | DL | 80.6 ± 3.9 | 89.5 ±1.9 ‡ § | 2.90 ! (1.45 to 4.35) |
F=170.914 p <0.001* |
F=13.324 p <0.001* |
F=25.849 p <0.001* |
| VMT | 80.4 ± 3.2 | 88.8±1.4 ‡ § | 3.40 ! (1.81 to 4.98) |
||||
| Control | 80.1±3 | 81.5±3.2 | 0.45 (-0.57 to 1.47) |
||||
| Anteromedial | DL | 81.8±5 | 90.1±3.4 ‡ § | 1.94 ! (0.71 to 3.16) |
F=48.253 p <0.001* |
F=6.221 p <0.004* |
F=9.617 p <0.001* |
| VMT | 82.2±4.8 | 89.8±3.2 ‡ § | 1.86 ! (0.65 to 3.07) |
||||
| Control | 82.5±4.5 | 83.4±3.9 | 0.21 (-0.80 to 1.22) |
||||
| Medial | DL | 81.8±5 | 90.1±3.4 ‡ | 1.94 ! (0.71 to 3.16) |
F=74.274 p <0.001* |
F=3.514 p <0.039* |
F=13.337 p <0.001* |
| VMT | 82.2±4.8 | 89.8±3.2 ‡ | 1.86 ! (0.65 to 3.07) |
||||
| Control | 82.5±4.5 | 83.4±3.9 | 0.21 (-0.80 to 1.22) |
||||
| Posteromedial | DL | 78.7±3.1 | 89 ±4.4 ‡ § | 2.70 ! (1.30 to 4.10) |
F=162.347 p <0.001* |
F=12.205 p <0.001* |
F=31.295 p <0.001* |
| VMT | 78.7±3.1 | 87.8±3.2 ‡ § | 2.88 ! (1.44 to 4.33) |
||||
| Control | 78.7±3.1 | 79.6±2.9 | 0.30 (-0.26 to 1.83) |
||||
| Posterior | DL | 82.2±3.3 | 90.1±3.3 ‡ § | 2.39 ! (1.06 to 3.72) |
F=84.773 p <0.001* |
F=5.316 p <0.009* |
F=16.797 p <0.013* |
| VMT | 81.9±3.8 | 89.8±3.3 ‡ § | 2.22 ! (0.93 to 3.50) |
||||
| Control | 82.6±3.7 | 83.2±3.8 | 0.16 (-0.85 to 1.17) |
||||
| Posterolateral | DL | 76.4± 3.2 | 87±4 ‡ § | 2.92 ! (1.47 to 4.38) |
F=147.187 p <0.001* |
F=10.384 p <0.001* |
F=26.928 p <0.001* |
| VMT | 76.6±3.3 | 85.9±4 ‡ § | 2.53 ! (1.17 to 3.89) |
||||
| Control | 76.9±3.3 | 78±1.8 | 0.41 (-0.60 to 1.43) |
||||
| Lateral | DL | 74.8±4.6 | 87.6±4.6 ‡ § | 2.78 ! (1.36 to 4.20) |
F=123.620 p <0.001* |
F=9.974 p <0.001* |
F=23.937 p <0.001* |
| VMT | 74.3±4.4 | 85.2±3.7 ‡ § | 2.68 ! (1.28 to 4.07) |
||||
| Control | 75±4 | 76.1±4.6 | 0.25 (-0.76 to 1.27) |
||||
| Anterolateral | DL | 77±4 | 88.6±4 ‡ § | 2.9 ! (1.45 to 4.35) |
F=98.265 p <0.001* |
F=10.488 p <0.001* |
F=22.583 p <0.013* |
| VMT | 78±3.9 | 87.5±4.1 ‡ § | 2.37 ! (1.05 to 3.69) |
||||
| Control | 77.6±4.3 | 78±4.7 | 0.08 (-0.92 to 1.10) |
||||
| Variables | Group | Pre-test Mean ± SD |
8-weeks Mean ± SD |
ES (CI95%) † |
P value | ||
|---|---|---|---|---|---|---|---|
| Main effect of time | Main effect of group | Group × time interaction | |||||
| Hip flexion (degree) | DL | 55.9±5.5 | 62±6.1 ‡ § | 1.05 ! (-0.29 to 2.13) |
F=31.011 p <0.001* |
F=2.979 p <0.062 |
F=8.386 p <0.001* |
| VMT | 50.5±7.7 | 56.6±7.8 ‡ § | 0.78 (-0.26 to 1.83) |
||||
| Control | 51.9±11 | 51.8±11 | -0.00 (-1.02 to 1) |
||||
| KF (degree) | DL | 28.1±7.1 | 39.2±4.5 ‡ § | 1.86 ! (0.65 to 3.08) |
F=55.063 p <0.001* |
F=20.632 p <0.001* |
F=18.190 p <0.001* |
| VMT | 27.8±5.9 | 41.7±3.07 ‡ § | 2.95 ! (1.49 to 4.42) |
||||
| Control | 26.6±4.8 | 25.9±6 | -0.12 (-1.21 to 0.81) |
||||
| AD (degree) | DL | 18.2±1.8 | 23±3.6 ‡ | 1.68 ! (-0.50 to 2.86) |
F=53.829 p <0.001* |
F=4.095 p <0.024* |
F=8.469 p <0.001* |
| VMT | 19.7±1.2 | 25.7±4.3 ‡ | 1.90 ! (0.68 to 3.12) |
||||
| Control | 21.9±2.2 | 22.1±2.2 | 0.09 (-0.61 to 1.43) |
||||
| KV (degree) | DL | -4.9±0.2 | -3.6±0.2 ‡ § | 6.5 ! (3.96 to 9.03) |
F=119.261 p <0.001* |
F=53.577 p <0.001* |
F=39.136 p <0.001* |
| VMT | -5.3±0.4 | -3.8±0.3 ‡ § | 4.24 ! (2.41to 6.06) |
||||
| Control | -5.1±0.4 | -5.2±0.4 | -0.12 (-1.26 to 0.76) |
||||
| VGRF (N) | DL | 3.3±0.2 | 2.8±0.1 ‡ § | -3.16 ! (-4.68 to -1.64) |
F=51.717 p <0.001* |
F=8.211 p <0.001* |
F=4.870 p <0.013* |
| VMT | 3±0.4 | 2.7±0.1 ‡ § | -1.02 ! (-2.10 to 0.04) |
||||
| Control | 3.4±0.4 | 3.3±0.5 | -0.22 (-1.52 to 0.52) |
||||
| Variable | Group | Pre-test Mean ± SD |
8-weeks Mean ± SD |
ES (CI95%) † |
P value | ||
|---|---|---|---|---|---|---|---|
| Main effect of time | Main effect of group | Group × time interaction | |||||
| TSK test | DL | 37.6 ±7.3 | 22.6 ±4.8 ‡ § | -2.42 ! (-3.76 to -1.09) |
F=50.047 p <0.001* |
F=3.438 p <0.029* |
F=6.154 p <0.001* |
| VMT | 38 ±6.7 | 23.3 ±4.1 ‡ § | -2.64 ! (-4.03 to -1.26) |
||||
| Control | 37.4 ±6.5 | 36.2 ±6.0 | -0.19 (-1.20 to 0.82) |
||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





