1. Introduction
The modern healthcare system has witnessed a remarkable change evident through the transformation of service delivery mechanisms with reference to patient-centred, value-based and coordinated approaches [
1]. It is expected as a result of this evolution, the next decade will see tremendous shifts in the approach and delivery of the healthcare system fostered by an immense rise in healthcare costs, growth in consumerism and digital transformation. Most importantly, a critical contribution to the changing dynamics of the healthcare system has been made by Electronic Medical Records (EMR). EMR has fostered disruptive innovation in the American healthcare system with the technology expected to improve the functioning of healthcare organizations by 6% each year [
2]. It has led to increased performance efficiency of healthcare systems achieved through automation of activities and processes such as appointment scheduling, processing payments and insurance claims and sharing information with staff which can help to reduce administrative burden and increase the efficiency of care delivery. Moreover, EMR has significantly improved the quality of care evident through the provision of tools for population health management and data analytics, enabling healthcare providers to identify recent trends and revolutions [
3]. Given these aspects, the aim of this review is to provide an in-depth account of the importance of EMR in terms of its role in the transformation of the healthcare system with a critical overview of the changes that can help to streamline and enhance its implementation efficiency in the American healthcare system in an effective manner.
2. Innovation and Its Relation to Optimal Healthcare Provision
Innovation development in healthcare has paved the path towards improvement in system efficiency, quality of patient care, collaboration and communication mechanisms, and cost-effective healthcare services, increasing the overall efficiency of the healthcare system in a significant manner [
4].
2.1. Recent Trends—A Perspective of EMR
It is evident through the current dynamics that there has been a trend towards the widespread adoption of EMRs in the healthcare system. According to the ONC, as of 2021, over 90% of hospitals and 50% of clinical physicians have adopted and implemented some form of EMR system in their healthcare practice [
5]. This trend has been driven by various factors such as government incentives, not-for-profit organisations and the potential for improved care delivery and cost savings. In addition, due to the rise in consumerism in healthcare in terms of enhanced use of technology by individuals to manage their own health with the use of wearable devices, mobile health applications and other tools that allows them to track their health metrics and communicate with their healthcare providers, EMRs can play a profound role by providing a platform for communication and by allowing individuals to access their own medical recorded through their smart device while also being able to communicate with staff through the mobile application [
4]. This shows that EMR have a dominant positive role in the transformation of healthcare by increasing the affordability and accessibility of healthcare services while also leading towards improved efficiency and quality of patient care in an effective manner.
2.2. Effective Usage Practices and Requirements
EMR has fostered interoperability and collaboration in healthcare departments by enabling different systems to exchange and use patient data. This trend has been accelerated dominantly by the pandemic, leading to increased use of telemedicine, referring specifically to the use of electronic communication to provide healthcare services remotely [
6]. The significance of telemedicine is evident from the fact that it allows patients to access healthcare services from their homes or other locations remotely, proving to be extremely useful, especially for patients in rural or underserved areas. It can revolutionize healthcare as patients will be able to access healthcare services on a global scale with reference to transcending the geographical barriers of visa requirements and economic barriers of costly healthcare services. Moreover, an increasing prevalence towards the use of artificial intelligence (AI) and machine learning in healthcare has contributed effectively towards the rigorous and informed analysis of large amounts of data as well as to identify patterns or trends that may be useful for improving care delivery or identifying potential issues. For instance, AI algorithms can serve effectually towards an increase in efficacy of prediction related to the likelihood of a patient developing a particular condition based on their medical history and other factors [
7]. Hence, providing a platform that can provide competitive benefits to both patients and healthcare professionals in terms of improved provision and access to healthcare services.
2.3. Healthcare Dynamics—A Regulatory Perspective
Political involvement in healthcare can take many forms including the development of policies and regulations, the allocation of funding, and the shaping of healthcare delivery models. Governments at all levels play a crucial role in shaping the healthcare system and can have both positive and negative impacts on the healthcare innovation [
8]. The government policies and practices towards the healthcare system of the US has usually exhibited a positive role in relation to constructive approach towards healthcare innovation. For instance, the Affordable Care Act 2010 is a comprehensive healthcare reform law that was enacted in the United States in 2010. It had a number of benefits for individuals, families, and the healthcare system as a whole with reference to enhanced access to healthcare services, improvement in quality of care, the decline in healthcare costs and improvement in patient outcomes [
9]. Most importantly, the government of the US also played a significant role in the implementation and promotion of the EMR system as it not only made it mandatory for hospitals to convert to the digital format or EMR in particular but also invested 27 million dollars for the purpose as a part of Health Information Technology for Economic and Clinical Health (HITECH) Act [
10]. This illustrates that government has a dominant role in influencing the healthcare system of a country towards a significant direction, which in the case of the US has been influenced by innovation development and constructive factors, ultimately leading to the implementation of EMR in nearly 95% of hospitals of the country.
2.4. Challenges to Health Innovation
Despite the innumerable competitive benefits provided by EMR, the implementation and usability effectiveness of the system are significantly detracted because of the lack of unification [
11]. This is especially true for the American healthcare system where although EMR has played a profound role in terms of an informed approach towards the procedure, diagnosis and management of symptoms, yet the lack of unification of EMR systems nationally is a dominant challenge that needs to be addressed and tackled to utilize the benefits of EMR to the maximum extent. This is mainly due to the use of proprietary formats and strict privacy and compliance protocols followed by different EMR systems, which hence makes it difficult to share and exchange information between different healthcare organizations [
12]. In light of this aspect, there is a crucial need to standardize data formats and develop effective interoperability standards as this will increase healthcare efficiency remarkably reflected through the outcomes of improved data quality, enhanced healthcare accessibility, and elevated healthcare quality.
3. Framework for EMR Priority Assessment
Priority assessment is one of the fundamental areas of patient care as it helps healthcare professionals to access and analyse information leading to the development of a strategic plan for effective patient stability and quality of care.
3.1. Principles and Priorities of the Healthcare System
EMR has brought an immense revolution in the American healthcare system as it is considered as the key driver of creativity and innovation that contributes towards exceptional healthcare quality and patient care. Given the fundamental importance of EMR, as a part of the American Recovery and Reinvestment Act (2014), all the public and private healthcare institutions, professionals and practitioners were required to implement and illustrate the informed use of EMR [
13]. This will be accomplished through the “meaningful use” of digital innovation and medical records, reflected through the following parameters.
Improve the quality and safety of healthcare services by reducing the likelihood of health disparities.
Foster collaboration by engaging the patients and family in an efficient manner with the help of technological tools to ensure that all members of the healthcare system have equal and informed access to information and care services, thereby leading to improved patient care.
Improve care planning and coordination with the aim to improve the health stability and status of the general public.
Maintain efficient and effective data security and privacy throughout the system.
Since then, the adoption of EMR systems has been a priority for the majority of healthcare organizations in the US as they offer numerous benefits over traditional paper-based record-keeping systems. For instance, EMR systems can facilitate healthcare providers improve the quality and efficiency of care by making it easier to access and share patient information, reduce the risk of errors and discrepancies, and support better decision-making. Most importantly, the US government has strongly incentivized the adoption of EMR systems through various initiatives such as the Meaningful Use program, which provides financial incentives to healthcare providers who demonstrate that they are using EMR systems in meaningful ways to improve the quality of care [
14]. In concise terms, through enhanced government investment and innovation development mainly in the form of real-time data collection and analysis has enabled healthcare providers to gather insights and information that can help improve patient outcomes and reduce healthcare costs in a sustained manner.
3.2. Challenges to EMR Standardization and Advanced Implementation
Despite the innumerable benefits fostered by EMR in the American healthcare system is the lack of standardization of EMR. This is mainly due to inconsistency in terms of types and data collection techniques of EMR systems, each with its own features, capabilities and interfaces [
12]. This thus makes it difficult for healthcare providers to select and implement the right EMR system for their needs as well as creates interoperability issues when different EMR systems are used within the same healthcare organization or network. In addition, standardization of EMR often requires significant investments in hardware, software, and training, which can be a barrier for some healthcare providers, particularly smaller organizations or those serving low-income populations. Most important is the barrier to data privacy and security when using EMR systems as the large volumes of sensitive patient information stored in these systems can be vulnerable to cyber-attacks or unauthorized access [
14]. Given this, it can be inferred that the standardization of EMR systems in the American healthcare system is a complex and ongoing process that requires the collaboration and coordination of many different stakeholders, including healthcare providers, EMR vendors, regulatory bodies, and patient advocacy groups, each contributing significantly towards the effective implementation of sound and secure standardized EMR system.
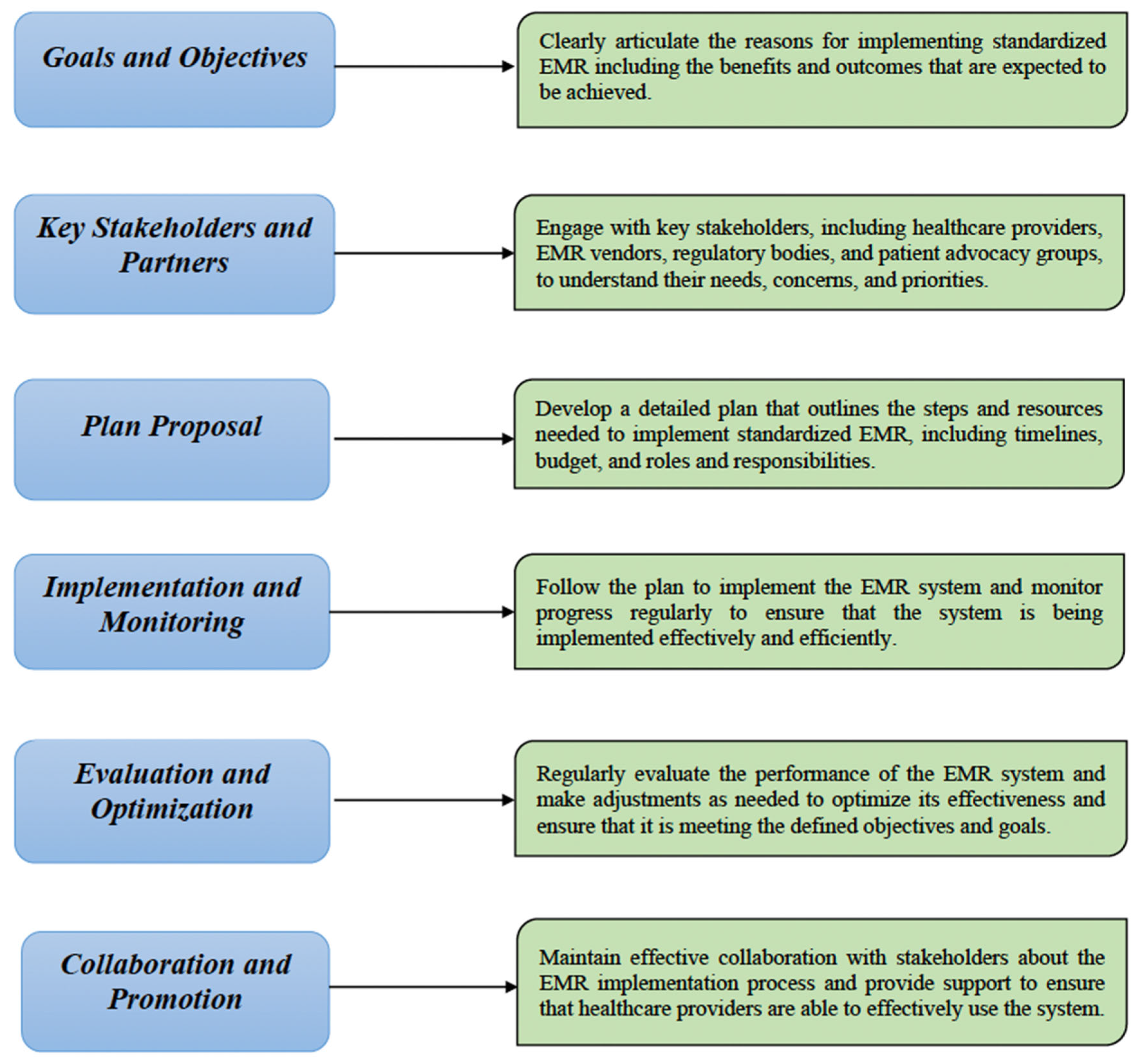
3.3. Pathways to Advanced EMR Implementation- Prospects and Constraints
The key objective of implementing advanced EMR in the US is to provide a structured and comprehensive approach to implementing standardized EMR, with the goal of improving the quality and efficiency of healthcare. With a standardized EMR system in place, healthcare providers would be able to easily enter, access and share patient information electronically rather than having to rely on paper records or manual data entry [
15]. This could them to allocate time to prioritise healthcare activities and processes for healthcare providers to focus on providing care to patients while also being able to reduce the risk of medical negligence and errors, which can have serious consequences for patient safety. For this purpose, the following implementation pathway is suggested (
Figure 1).
The advanced version of EMR with reference to the above strategic proposal will be termed a
Unified EMR System that will generate competitive opportunities and success prospects with reference to enhanced interoperability in US healthcare departments, improving the quality and efficiency of care by making it easier for healthcare providers to access and share patient information as well as reducing the risk of errors and discrepancies, thereby supporting informed and better decision-making [
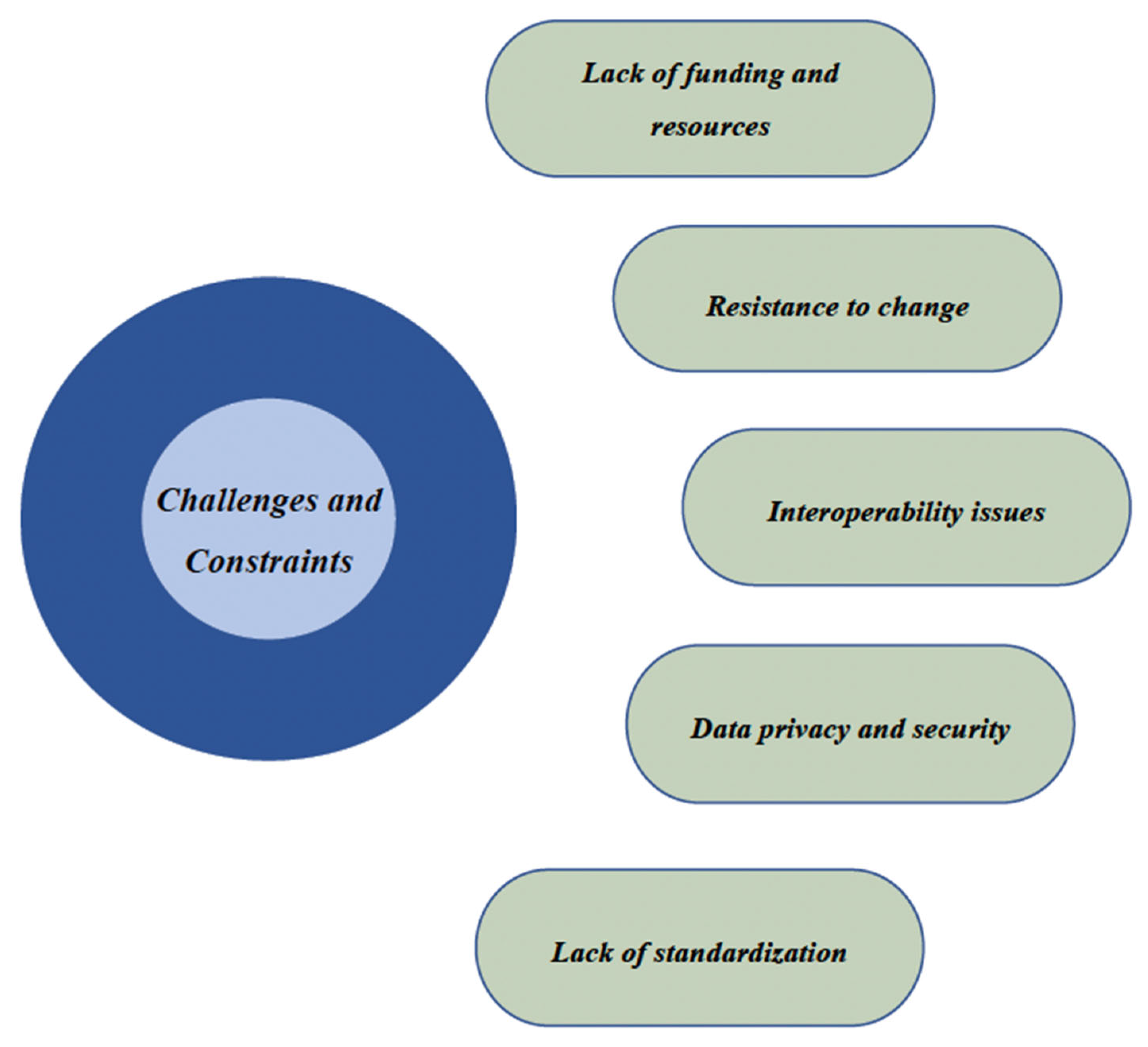
16]. However, it is important to consider the challenges and constraints that can detract from the effectiveness of implementation and hence, the associated positive outcomes (
Figure 2).
Discussed above are the dominant challenges and constraints that present challenges that could hinder the implementation of standardized electronic medical records in the US. It is because the implementation of EMR systems can be costly and might require significant investments in hardware, software and training, hence being a strong barrier for some healthcare organizations, particularly smaller ones or those serving low-income populations [
11]. Most importantly, interoperability issues related to EMR systems using different standards and protocols can make it difficult for healthcare organizations to exchange data and support seamless care delivery healthcare providers, and the resistant to adopting new EMR systems, particularly with reference to the preference for manual record system or unfamiliarity with EMR systems, can significantly detract the execution and effectiveness of EMR systems.
4. Healthcare Outcomes—Advanced EMR Perspective
It is crucial for healthcare providers to strategize the effective implementation of advanced EMR as a lack of clear and concise planning can lead to the selection of a system that might not meet the needs of the relevant healthcare organization and its patients, hence resulting in a dominant decrease in user satisfaction, increased healthcare costs and reduced efficiency [
16]. In addition, it is equally important to formulate and execute effective monitoring and evaluation with reference to the ability to identify and overcome potential improvements, the absence of which will prevent the healthcare organizations from utilising of EMR system to its full potential, hence leading to lack of optimization in terms of decreased efficiency and effectiveness of healthcare processes and strategies [
17]. Given this aspect, a comprehensive account of positive and negative outcomes associated with the implementation of a unified EMR system in the American Healthcare System can be developed.
4.1. Positive Outcomes
The positive outcomes associated with the implementation of advanced electronic medical records systems are listed below.
Improved Patient Care- Unified EMR systems can provide healthcare providers with access to a wide range of patient information and data, enabling them to make more informed decisions and foster quality care in an efficient manner.
Enhanced Collaboration and Coordination- Unified EMR systems that use standardized approaches and protocols can facilitate the exchange of patient data between different healthcare organizations in an efficient and seamless manner, hence facilitating better and quality care coordination.
Increased efficiency- Unified EMR systems can help streamline healthcare processes as well as reduce the risk of errors and duplications, decreasing the incidence of medical negligence and improving the overall efficiency and effectiveness of healthcare delivery.
Reduced Healthcare Costs- Unified EMR systems can help reduce healthcare costs by automating routine tasks, reducing the need for manual record-keeping, and enabling real-time data collection and analysis that can contribute towards the prioritization of healthcare activities and diversion of investment towards essential healthcare areas, hence contributing towards reduced healthcare costs.
Improved Patient Satisfaction- Implementation of a unified EMR system will significantly eliminate the need to carry out the repetitive patient assessment in relation to tests and other examinations, hence contributing towards enhanced patient safety and satisfaction in an efficient manner. It is because this aspect will help foster patients to become increasingly contended with their care when they have access to their own medical records and can track their health progress over time.
4.2. Negative Outcomes
The negative outcomes associated with the implementation of advanced electronic medical records systems are listed below.
High upfront costs: Implementing advanced EMR systems can be costly specifically with reference to the learning and development needs that are necessary to equip and train the healthcare team with the accurate and efficient usability of standardized EMR.
Data privacy and security concerns- Ensuring the security and privacy of patient data can be a significant challenge. It is because EMR systems store large volumes of sensitive patient information, which can be vulnerable to cyberattacks or unauthorized access, thereby requiring the healthcare system to devise and implement methods for careful and informed access to information stored in EMR.
Technical issues- Unified EMR systems will involve complex networks, technologies and processes and hence will require ongoing maintenance and support over defined intervals, which can create additional challenges for healthcare organizations in terms of finances and the effectiveness of the functioning mechanism.
5. Suggested Interventions to Effective EMR Implementation
In order to counter the aforementioned challenges, constraints and negative outcomes that can significantly detract from the effective implementation and performance of unified EMR systems in the American healthcare system, a systematic framework consisting of three main elements with reference to planning, execution and monitoring perspectives is illustrated in a comprehensive manner.
5.1. Standards of Design and Development
To develop effective standards of design and development of unified EMR, the healthcare system should initially identify and engage with key stakeholders including medical staff, IT staff and administrative experts with the aim to gather input and ensure that the new system meets the needs of preferences of modern healthcare dynamics as well as access and address any concerns that are detracting the execution of unified EMR [
17]. This will be followed by the development of a clear and concise set of standards for the design and development of the EMR system with reference to specifications for data storage, security, and interoperability with other systems. For this purpose, these standards will be based on industry best practices and align with relevant regulatory requirements such as the Health Insurance Portability and Accountability Act (HIPAA) [
18]. Most importantly, the system will be developed on the foundation of a user-friendly interface that will thus facilitate an effective and seamless transition to a unified EMR system, ensuring smooth implementation and ultimately, enhanced care interventions and outcomes.
5.2. Guidelines on Access to Data and Information
When developing guidelines for access to data and information in a unified electronic medical record system in the United States, it is crucially important to provide access only to the defined persons specifically medical staff and administrative members. It is also important to consider and ensure that the security and privacy of patient data are in accordance with appropriate safeguards to prevent unauthorized access to sensitive information [
12]. This can be effectively facilitated through the establishment of a stringent and systematic process for requesting and granting access to data and information within the EMR system containing procedures for revoking access when necessary. Hence, fostering effective functioning of the EMR system along with improved patient safety and satisfaction.
5.3. Monitoring and Evaluation Post EMR Deployment
To monitor and evaluate the performance of a standardized EMR system after deployment in the US healthcare system, it is crucial to focus on the impact of the system on patient care. While traditional metrics such as usage rates and user satisfaction are important, they do not necessarily provide a complete picture of the value of the EMR system. By collecting data on the impact of the EMR system on patient outcomes, organizations can get a more comprehensive view of the value of the system. This might include gathering data on the frequency and severity of medical errors, patient satisfaction with care and the time required to complete various tasks [
18]. Hence, by regularly reviewing this data, organizations can identify areas where the EMR system is making a positive impact on patient care and make any necessary adjustments to ensure that the system continues to support high-quality care.
6. Conclusion
This review provides an in-depth analysis and evaluation of positive and negative outcomes related to the implementation of standardized EMR in the US. With a standardized EMR system, healthcare departments and medical staff can easily access and update patient records, reducing healthcare costs along with the time and effort required to manage patient information. This can lead to improved patient care, increased collaboration and reduced medical errors achieved through enhanced interoperability of healthcare systems, making it easier for healthcare organizations to exchange information with one another and hence, the patients to receive care from multiple providers. In a nutshell, standardized EMR will significantly contribute towards a reduction in barriers to quality care and improvement in quality and coordination of care for patients.
References
- Jones, P., The Arts Therapies : A Revolution in Healthcare (version Second edition). Second ed. Abingdon Oxon: Routledge, 2020.
- Uslu, A. and J. Stausberg, Value of the Electronic Medical Record for Hospital Care: Update From the Literature. J Med Internet Res, 2021. 23(12): p. e26323.
- Cucciniello, M., I. Lapsley, and G. Nasi, Managing health care in the digital world: A comparative analysis. Health Services Management Research, 2016. 29(4): p. 132-142.
- Moullin, J.C., et al., A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Syst, 2015. 13: p. 16.
- Adler-Milstein, J., et al., Electronic Health Record Adoption In US Hospitals: Progress Continues, But Challenges Persist. Health Aff (Millwood), 2015. 34(12): p. 2174-80.
- Dahlweid, M., et al., Clinical Knowledge Platform (CKP): A Collaborative Ecosystem to Share Interoperable Clinical Forms, Viewers, and Order Sets with Various EMRs. Stud Health Technol Inform, 2022. 298: p. 117-121.
- Miller, D.D. and E.W. Brown, Artificial Intelligence in Medical Practice: The Question to the Answer? Am J Med, 2018. 131(2): p. 129-133.
- Filipe, A., A. Renedo, and C. Marston, The co-production of what? Knowledge, values, and social relations in health care. PLoS Biol, 2017. 15(5): p. e2001403.
- Tilhou, A.S., et al., The Affordable Care Act Medicaid Expansion Positively Impacted Community Health Centers and Their Patients. J Gen Intern Med, 2020. 35(4): p. 1292-1295.
- Luna, R. A Framework for Evaluation of Risk Management Models for HIPAA Compliance for Electronic Personal Health Information used by Small and Medium Businesses using Cloud Technologies. 2018.
- Day-Duro, E., G. Lubitsh, and G. Smith, Understanding and investing in healthcare innovation and collaboration. J Health Organ Manag, 2020. ahead-of-print(ahead-of-print).
- Beam, A.L., A.K. Manrai, and M. Ghassemi, Challenges to the Reproducibility of Machine Learning Models in Health Care. JAMA, 2020. 323(4): p. 305-306.
- Watson, M.D., et al., Surgery Residents Spend Nearly 8 Months of Their 5-Year Training on the Electronic Health Record (EHR). J Surg Educ, 2020. 77(6): p. e237-e244.
- Biltoft, J. and L. Finneman, Clinical and financial effects of smart pump-electronic medical record interoperability at a hospital in a regional health system. Am J Health Syst Pharm, 2018. 75(14): p. 1064-1068.
- Alahmar, A., M.E. Crupi, and R. Benlamri, Ontological framework for standardizing and digitizing clinical pathways in healthcare information systems. Comput Methods Programs Biomed, 2020. 196: p. 105559.
- Lancaster, E. and E. Wick, Standardized Care Pathways as a Means to Improve Patient Safety. Surg Clin North Am, 2021. 101(1): p. 49-56.
- Janett, R.S. and P.P. Yeracaris, Electronic Medical Records in the American Health System: challenges and lessons learned. Cien Saude Colet, 2020. 25(4): p. 1293-1304.
- Edemekong, P.F., P. Annamaraju, and M.J. Haydel, Health Insurance Portability and Accountability Act, in StatPearls. 2022: Treasure Island (FL).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).