Introduction
During illness and old age, the systemic changes originating from loss of albumin (HSA) binding cause cumulative cellular changes (1-6). These changes are reflected in the ability of the liver to maintain levels needed for systemic delivery of almost all nutrients including gaseous exchange (2,3).
There are two main mechanisms of adjusting cellular health when illness occurs: either remove the irritation or adjust the medium the cells are bathed in to maintain best survival. In cases of COVID-19, influenza and bacterial diseases, conventional wisdom is to remove the offending virus or bacteria. This is usually done by a vaccine, which uses the body’s own immune system to create antibodies to promote dissipation or antibiotics which destroy the bacteria in situ. The second method is to stabilise cells and the immune system by altering the medium in which they sit. This method must take into consideration a number of factors because the systemic system controlling individual organs and cellular structures is diverse and during illness normal vascular control is usually impeded. We suggest one method of increasing the immunity of the body is to improve nutrient supply and oncotic pressure to the cells which can be done by infusion of HSA to the liver and increasing whole body fluids (WBF) to a level at which the cardiovascular/lymphatic system is efficient.
In anaesthesiology and surgery maintaining correct whole-body fluids is essential for the efficiency of heart and lungs both in terms of pressure and nutrients (8). Correct cellular nutrients increase recovery from surgery (9). All systemic pharmaceuticals depend both on the levels of WBF but also on the binding constraints of HSA in determining the constitution of the blood, interstitial fluids, lymph, and other body fluids. A successful protocol to maintain HSA at set levels will alleviate diurnal and systemic variation permitting finite control of glucose and ketone level by allowing the precise maintenance of pancreatic and adrenal hormones all of which compete for transport by binding to HSA. The maintenance of these hormonal levels controlling plasma nutrients is the result of an algorithm predicted by their release properties and the timing constraints on delivery. The hormones have been largely identified.
As liver HSA production levels change all other components of the blood change correspondingly with equilibrium determined by timing of distribution through the interstitial fluid and lymph. All other proteins and cellular distribution of blood components are maintained secondary to HSA including nutrients, red and white blood cell count, the levels of hormones and waste. HSA through its control of colloidal pressure and whole-body fluids also is the underlying maintenance of blood pressure and of maintaining efficiency of the heart.
We have already published evidence that:
HSA levels are age HSALNP and have a direct relationship to mortality due to COVID-19 and other illnesses (1, 2).
A decrease in HSA binding causes Albumin binding diseases (ABD), whereby insufficient binding for nutrient affects oncotic pressure and cellular nutrients. ABD are defined symptoms caused by lack of correct binding to has, resulting in illness caused by resulting nutrient deficiency and adverse pressure changes. We define systemic sepsis as being ABD as well as most metabolic diseases and many cardiac symptoms (2). ABD may be also responsible for altitude sickness. (3,4)
We have demonstrated how ABD causes endothelial collapse and have defined the cause of systemic sepsis as its effects (3). The endothelial glycocalyx plays an important role in vascular homeostasis, regulating vascular permeability and cell adhesion, has antithrombotic and anti-inflammatory functions and is bound within the glycocalyx, thus contributing to stability of the layer. In addition, albumin transports sphingosine-1-phosphate which has protective endothelial effects (5).
We demonstrated that the human serum albumin lymphatic nutrient pump (HSALNP) distributes nutrients selectively to organs, simultaneously maintaining oncotic pressure (6).
We showed how present regimens for saline and colloids do not consider physiological reality (4) and showed how infusion of to the periphery can produce cellular damage.
We demonstrated that the correct procedure for fluid therapy is by direct infusion to the liver and that the most convenient route is by the hepatic portal vein by ultrasound guided core needle.
We have shown that HSA liver levels through maintenance of whole-body fluids (WBF) is an elemental control for blood pressure, cellular pressure, and nutrients in all tissues.
This we propose raising HSA will correct the deficiencies that cause vulnerabilities in ABD.
Gaseous supply to cells is through the through the heart lungs capillary network and diffusion to the cells. This can be thought of as the fast primary circulation timing with the red blood cells (RBCs) returning every few minutes. Over 50% of HSA forms a secondary circulation that has a half-life of many hours formed from the leakage of HSA through the interstitial spaces into the lymph. This secondary circuit is fed from the primary circuit which is maintained by HSA liver production. In turn metabolites such as glucose and ketones are controlled in the primary circuit by circulating hormones mainly from the adrenal glands (cortisol, aldosterone, adrenaline, and noradrenaline), pancreas (Insulin and glucagon). It is organ dependent and provides nutrients to cells.
The ability to raise or decrease WBF has many clinical consequences in almost all areas of medicine. In ABD an increase in albumin levels will gradually stabilise HSA diurnal rhythm by settling variations in the cardiovascular capillary circulation and stabilising cardiovascular output. Once at a higher level any ABD will be reversed as the chain of nutrients supplied by the liver and the complex equilibrium of nutrients in the plasma re-establish. In the longer term the 7-hour half-life of the HSALNP, which supplies the interstitial spaces and deep cells with nutrients and maintains correct colloidal pressure, will resume providing interstitial spaces and cells correctly.
The HSALNP separates the cardiovascular system into different circulations according to the half-life of substances transported. Thus, conventionally gaseous respiration provides exchange in minutes to the cells from the lungs. The speed and distribution of all other components in the blood is controlled by the binding levels of albumin; 60% of which passes into the interstitial spaces and lymph taking many hours. It is this second longer nutrient circulation which has been overlooked, the timing of which may be weeks. Levels of all other components of the blood respond to changes in HSA.
In a healthy body, HSA production in the liver is regulated is by pressure in the hepatocytes of the liver. Increased levels of HSA produce an increase in ketone bodies from the liver a preferential metabolite for the lungs, heart, and brain. Glucagon plays a limited role in ketogenesis during fasting or in response to SGLT2 Inhibition (7). The lungs are the primary site of plasma and lymph flow from the liver after passing through the heart. The delivery of ketones to the lungs is immediate, excess may produce ketoacidosis (13), while a deficit causes inefficiency in cellular function. A chain of events maintains the normal supply of ketones from the lungs and depends upon albumin levels. Both ketones and glucose levels are also controlled by levels of insulin and glucagon secreted from the pancreas directly into the hepatic portal vein. The pancreas samples plasma for glucose levels from cardiac output and is reactive to glucose levels within a few minutes in the capillary circulation but many hours in the interstitial lymph circulation.
Raising albumin safely depends upon the timing of distributed nutrients through the interstitial cells and the constitution of the resulting lymph. Although the timing to infuse HSA to the cardiovascular capillary circulation takes a few minutes the resulting flow through the interstitial-lymph circuit takes many hours. Many nutrients such as glucose are only partly bound to HSA and their timing through the interstitial/lymph does not follow HSA. This mean that glucose variations follow discrete timings as lymph returns to the venous system slowly. Glucose levels are maintained mainly by insulin and glucagon excretion by the pancreas as well as epinephrine in times of stress. Insulin (levels HSALNP upon HSA to which it is bound) is maintained by concentrations in the hepatic portal (HPV) vein as it passes to the liver. Levels of glucose are therefore HSALNP upon only the insulin levels in the HPV and not the rest of the circulatory system. This is reflected in the rapidity of glucose homeostasis. Therefore, in illness where the lymph flow is irregular, insulin measurements should ideally be taken from the HPV or arterial blood where a more direct relationship exists. In the liver insulin promotes glycogenosis leading to a reduction of blood sugar. This feedback loop that regulates glucose is dependent upon only the cardiovascular/capillary circulation, as the pancreas is primarily sampling glucose through this loop with changes in lymph occurring over the longer term depending upon lymph flow. The interdependency of insulin, glucose metabolism and levels of insulin can also be seen in the age variations in diabetes 2 in terms of both obesity and the age profile. In diabetes, hepatic production of serum albumin decreases, and it has been long established that insulin positively controls albumin gene expression (10). Serious illness in COVID-19 occurs during the secondary phase when IgG3 cells are at their highest (11). In addition, glycosylation of HSA decreases available HSA binding.
A chain of nutrition therefore exists between the liver – lungs - heart and the rest of the body organs, such that release of proteins and nutrients of the liver are exchanged in the lungs before entering the capillary circulation of the periphery. The lungs and heart are both ketone metabolisers and therefore have a different dependency to HSA binding than does the periphery. Maintaining this chain is critical for the correct health of the heart and lungs especially during stress or illness. As blood flows from one organ to the next in series, binding by albumin and corresponding nutrient binders of nutrients change to reflect the correct medium for cell growth and cardiovascular efficiency. It is very important that this chain of binding and concentrations of metabolites is maintained so that individual organs operate within their correct nutrient medium and pressures.
Ketones, (released concurrently with HSA production) are preferentially metabolised by the lungs heart and brain during prolonged exercise or when glucose levels drop during illness (13). Increased synthesis and use of ketone bodies as ancillary fuel during periods of deficient food supply and low insulin levels causes oxidative stress in the mitochondria, which initiates a protective response allowing cells to cope with decreased energy availability (13).
In a normal healthy sedentary body, ketone levels are balanced to the release of HSA. Exercise produces a relative drop in pressure in the liver producing both nutrient bound HSA and ketone bodies. In a healthy individual any excess acetone from ketone metabolism is largely excreted by the lungs thus avoiding keto acidosis. In a respiratory compromised individual for example, where the lungs are infected by COVID-19, any increase in HSA and ketones will result in ketoacidosis and cellular death. An inverse relationship exists between HSA levels and ketosis for type 2 diabetes (14). As the release of ketones is HSALNP on natural release of HSA, any infused HSA will therefore lead to a drop in ketones as plasma volume increases. In acute respiratory distress syndrome (ARDS) this may have a beneficial effect of increasing antioxidants and decreasing the risk of ketoacidosis. If HSA is administered rapidly both ketones and glucose may require adaptation, either by hormonal influence or direct infusion. The ketone-body metabolism is maintained by the anabolic hormone insulin and the primarily catabolic hormones, glucagon, cortisol, catecholamines and growth hormone (15). The level of ketones should be assessed, ideally in the hepatic artery, arterial blood, and venous blood, to monitor their usage and production.
Albumin and magnesium concentrations are linearly related at high and low albumin concentrations. (16). Both magnesium and calcium are bound to HSA with calcium up to 80% bound. The relationship between this competitive binding is well known with the magnesium and calcium metabolism closely related to the intestinal absorption and the renal excretion, the two ions being interdependent (17). Plasma calcium concentration is maintained within a narrow range by the coordinated action of parathyroid hormone (PTH), 1,25(OH)2D3, calcitonin, and ionized calcium (iCa2+) (18). HSA is an intermediary transporting both calcium and magnesium which compete for binding and dissolution in surrounding fluid. Transport of both calcium and magnesium are dependent on HSA levels for binding and appropriate oncotic pressures to adequately supply cells. Modified calcium and magnesium ratios are implicated in COVID-19 vulnerabilities (19, 20).
Correct pressure regulation of cardiac function is dependent upon the levels of body fluids and distribution. Levels of pressure in the cells supplying nutrients are ultimately maintained by repetitive heartbeats. For a healthy heart to be maintained sufficient blood must be returned to the heart with every filling of the atria so that the ventricles can operate within their limits as defined by the Frank-Starling effect. It is the liver and HSA production that defines WBF, blood volume and content providing both a stable WBF and cardiovascular output within the limits of each individual physiology, by sampling pressure at its lowest in the HPV.
Serum albumin concentration is an important predictor of both baseline haemoglobin (Hgb) and Erythropoietin (Epo) sensitivity. (21). Erythropoietin (Epo) is released on sustained hypoxia leading to changes in Hgb following 6 weeks of acclimatisation. Increasing WBF and blood volume will have an immediate effect of increasing blood flow which may alleviate some sensitivity to HSA infusion.
Acute-phase reactants such as high-sensitive C-reactive protein (CRP), lactate dehydrogenase (LDH), ferritin, procalcitonin, interleukin (IL)-6, tumour necrosis factor-alpha, and IL-1 are elevated in all most all cases of sepsis and early elevation is associated with high mortality.
Discussion
To successfully raise HSA depends upon different pathologies of individuals and the technology to cannulate and evaluate nutrients and hormones.
Core needle biopsy under ultrasound is now a regular procedure and has been used for the liver (22) and this technique can be used for safe cannulation of the HPV.
Lungs and COVID-19.
The lungs are almost always the first point of infection in COVID-19. Any damage to the lungs affects the primary circuit of the HSALNP affecting all metabolites in the blood. Metabolites controlled by the liver such as glucose and ketones are metabolised selectively according to the activity of the lungs. In damaged tissue ketosis is a danger. Reduced respiration will reduce the level of acetone removal and promote ketoacidosis. In cases with damage the lungs, infusion of HSA to the liver should be to a well-ventilated supine subject with at least ketone/glucose levels monitored and adjusted. Levels of adrenaline should be at least stable.
ABD
In ABD where lung inflammation is not problematic direct infusion to the HPV should adequately raise WBF and reduce vulnerabilities and sepsis. As HSA rises all other components of the blood rise accordingly. Timing is still critical, and care should be taken as the effluent from the lymph mixes with that of the plasma.
Acclimatisation to altitude.
Upon climbing from sea level to altitude blood pressure reduces stimulating the release of HSA, simultaneously less oxygen produces hypoxia. HSA release increases WBF including the blood volume increasing hypoxic symptoms. In a healthy body HSA release stimulates all other blood components with RBC stabilising after 6 weeks. During this acclimatisation period the body responds to the hypoxic systemic environment by increased flow to the periphery and through the lymph.
In our protocol we suggest monitoring glucose, ketones and corresponding hormones, insulin, glucagon with the aim of maintaining a balance where necessary. Both pancreatic and adrenal hormones are important in maintaining primary ketone/glucose balance during stress and must be maintained at or near optimal as HSA rises. HSA should be infused into the liver where it is formed naturally and where binding to metabolites originates.
Ketones and glucose are the secondary variants in the cardiovascular circuit after HSA, variations in levels of both are determined by the pancreatic and adrenal hormones with the timing of other nutrients in response.
The liver is highly complex moderating the content of diverse ligands in the blood. It is adaptable to huge variation in its production of HSA and metabolites. There is no evidence to suggest that healthy liver cannot produce, and recharge metabolites linked to infused HSA.
Almost all systemic pharmaceuticals form ligands with albumin or other related protein binders like prealbumin. Changes in WBF will change their concentration determined by the flow and distribution of HSA, this modifies their action.
Increase in WBF caused by HSA infusion leads to changes in systemic hormones leading to concomitant changes in both Glucose and Ketone metabolism. Ketones are metabolised in the fast cardiovascular-capillary circuit. Important during exercise when the lungs and heart metabolise ketones under stress and on release of epinephrine. Any infusion of HSA to the liver assumes the best possible oxygenation of the blood.
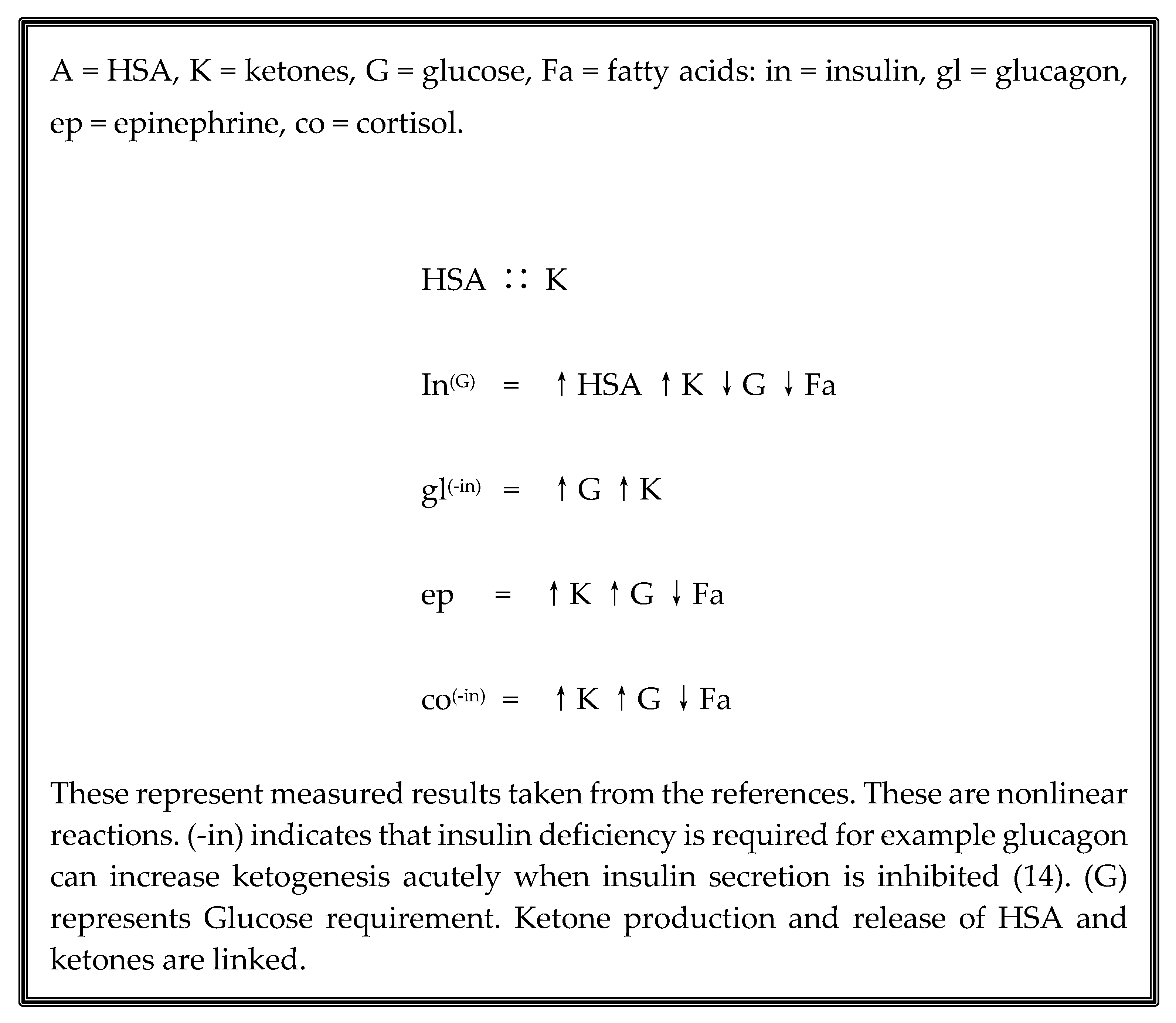
An insulin increase is followed by a decrease in Glucose, and increasing levels of HSA, ketones, and fatty acids. Glucagon act to increase glucose when insulin id deficient, ketone levels also increase. Epinephrine raises ketones, glucose, and fatty acids. Cortisol like Glucagon raises ketones, glucose and decreases fatty acids when insulin is deficient. Note that Glucagon is being controlled from the pancreas, and cortisol is controlled from a separate blood supply to the adrenal gland, sampling blood from two diverse sites.
Deconstructing the actions of these hormones in respect to their sampling of the plasma demonstrates that HSA levels are also maintained from the glucose/ketone balance by the secretion of insulin
Figure 1. HSA is primarily controlled by pressure in the hepatic portal vein (HPV) and this further attribute may have practical value for increasing HSA during illness. It may be possible to increase HSA naturally by fine timing levels of these hormones accurately and maintaining ketone and glucose levels. Theoretically, it is possible to change the actions and nutrient content by manipulating these hormones and their targets. For example, correct insulin infusion coupled with additional glucose will produce HSA if HSA levels are low with minimal change in glucose and ketone levels. Perhaps insufficient to raise HSA binding levels alone, this provides a technique for stabilisation of levels with addition of HSA infused to the HPV during infusion.
Infusion of HSA reduces effective concentrations of these hormones and interferes with their respective binding to HSA until equilibrium is restored. Equilibrium should occur with ketones and glucose rapidly in a healthy individual, however our knowledge of how the hormones gives an opportunity to raise HSA rapidly and safely. It is this equilibrium and the balance between ketones glucose and the rest of the nutrients that maintains body health.
Conclusion
In a normal healthy sedentary individual raising HSA levels may be achieved by infusion of HSA into the liver whilst importantly maintaining insulin and glucose levels. The establishment of correct timing for infusion will depend largely upon diurnal and other varying factors from cellular discharge into the lymph. The two main concerns are the Ketones and Glucose, both of which are controlled in the fast cardiovascular capillary circuit needing monitoring in minute intervals. Individuals are different and often present with different symptoms. It is important to recognise that any infusion of HSA should also monitor the control of at least ketones and glucose, both of which have relatively short half-life in the body, with adjustments to ensure correct balance of nutrients.
There is ample evidence that a healthy body should respond to increase of WBF by replacing all nutrients and blood cells according to their timing. HSA infusion will have limited adverse effect with acclimatisation ending with whole RBC count which attains full production after 6 weeks.
Evidence indicates that clinical maintenance of WBF by HSA infusion to the liver, will stabilise HSA variability and diurnal changes, permitting the finite control of metabolites including glucose and ketones balance. In addition, further advantages can be gained from the targeting of pharmaceuticals linked to albumin. HSA is the only factor maintaining long-term blood pressures from environmental changes in posture and physiology. Increasing HSA binding should decrease mortality by removing the limiting factors in ABD.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Johnson AS and Winlow W. “The HSA Lymphatic Nutrient Pump (HSALNP) and its Critical and Central Importance to Health”. EC Pharmacology and Toxicology 10.12 (2022):32-34.
- Johnson AS, & Winlow W. (2021). COVID-19 vulnerabilities are intensified by declining human serum albumin levels. Experimental Physiology. 2021;1–9. [CrossRef]
- Levitt DG, Levitt MD. Human serum albumin homeostasis: a new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int J Gen Med. 2016 Jul 15;9:229-55. [CrossRef]
- Johnson AS, Fatemi R and Winlow W (2020) SARS-CoV-2 Bound Human Serum Albumin and Systemic Septic Shock. Front. Cardiovasc. Med. 7:153. [CrossRef]
- Johnson AS, Polese G, Johnson M and Winlow W. Appropriate Human Serum Albumin Fluid Therapy and the Alleviation ofCOVID-19 Vulnerabilities: An Explanation of the HSA Lymphatic Nutrient Pump. COVID 2022, 2, 1379–1395. [CrossRef]
- Aldecoa, C., Llau, J.V., Nuvials, X. et al. Role of albumin in the preservation of endothelial glycocalyx integrity and the microcirculation: a review. Ann. Intensive Care 10, 85 (2020). [CrossRef]
- Capozzi ME, Coch RW, Koech J, Astapova II, Wait JB, Encisco SE, Douros JD, El K, Finan B, Sloop KW, Herman MA, D'Alessio DA, Campbell JE. The Limited Role of Glucagon for Ketogenesis During Fasting or in Response to SGLT2 Inhibition. Diabetes. 2020 May;69(5):882-892. [CrossRef]
- Casey JD, Brown RM, Semler MW. Resuscitation fluids. Curr Opin Crit Care. 2018 Dec;24(6):512-518. [CrossRef]
- Laffel, L. (1999), Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab. Res. Rev., 15: 412-426. [CrossRef]
- Seccombe A, Sapey E. What is the evidence base for fluid resuscitation in acute medicine? . Clin Med (Lond). 2018 Jun;18(3):225-230. https://doi.org/10.7861/clinmedicine.18-3-225. Chen Q, Lu M, Monks BR, Birnbaum MJ. Insulin Is Required to Maintain Albumin Expression by Inhibiting Forkhead Box O1 Protein. J Biol Chem. 2016 Jan 29;291(5):2371-8. [CrossRef]
- Iles, R.K 2023. The COVID-19 antibody responses, isotypes and glycosylation: Why SARS-CoV-2 Spike protein complex binding of IgG3 is potentiated in some and immuno-pathologies manifest. medRxiv 2023.01.13.23284524. [CrossRef]
- Mey JT, Hari A, Axelrod CL, Fealy CE, Erickson ML, Kirwan JP, Dweik RA, Heresi GA. Lipids and ketones dominate metabolism at the expense of glucose control in pulmonary arterial hypertension: a hyperglycaemic clamp and metabolomics study. Eur Respir J. 2020 Apr 9;55(4):1901700. [CrossRef]
- Kolb, H., Kempf, K., Röhling, M. et al. Ketone bodies: from enemy to friend and guardian angel. BMC Med 19, 313 (2021). [CrossRef]
- Po-Chung Cheng, Shang-Ren Hsu, Yun-Chung Cheng, "Association between Serum Albumin Concentration and Ketosis Risk in Hospitalized Individuals with Type 2 Diabetes Mellitus", Journal of Diabetes Research, vol. 2016, Article ID 1269706, 5 pages, 2016. [CrossRef]
- Alberti KG, Johnston DG, Gill A, Barnes AJ, Orskov H. Hormonal regulation of ketone-body metabolism in man. Biochem Soc Symp. 1978, 43, 163–182, PMID: 749914.
- Kroll MH, Elin RJ. Relationships between magnesium and protein concentrations in serum. Clin Chem. 1985 Feb;31(2):244-6. PMID: 3967355.
- Paunier, L. Effect of magnesium on phosphorus and calcium metabolism. Monatsschr Kinderheilkd. 1992 Sep;140(9 Suppl 1):S17-20. PMID: 1331782.
- Jeon, U.S. Kidney and calcium homeostasis. Electrolyte Blood Press. 2008 Dec;6(2):68-76. [CrossRef]
- Guerrero-Romero F, Mercado M, Rodriguez-Moran M, Ramírez-Renteria C, Martínez-Aguilar G, Marrero-Rodríguez D, Ferreira-Hermosillo A, Simental-Mendía LE, Remba-Shapiro I, Gamboa-Gómez CI, Albarrán-Sánchez A, Sanchez-García ML. Magnesium-to-Calcium Ratio and Mortality from COVID-19. Nutrients. 2022 Apr 19;14(9):1686. [CrossRef]
- Coman, A.E.; Ceasovschih, A.; Petroaie, A.D.; Popa, E.; Lionte, C.; Bologa, C.; Haliga, R.E.; Cosmescu, A.; Slănină, A.M.; Bacușcă, A.I.; Șorodoc, V.; Șorodoc, L. The Significance of Low Magnesium Levels in COVID-19 Patients. Medicina 2023, 59, 279. [Google Scholar] [CrossRef] [PubMed]
- Agarwal R, Davis JL, Smith L. Serum albumin is strongly associated with erythropoietin sensitivity in hemodialysis patients. Clin J Am Soc Nephrol. 2008 Jan;3(1):98-104. [CrossRef]
- Johnson KD, Laoveeravat P, Yee EU, Perisetti A, Thandassery RB, Tharian B. Endoscopic ultrasound guided liver biopsy: Recent evidence. World J Gastrointest Endosc. 2020 Mar 16;12(3):83-97. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).