Submitted:
02 February 2023
Posted:
03 February 2023
Read the latest preprint version here
Abstract
Keywords:
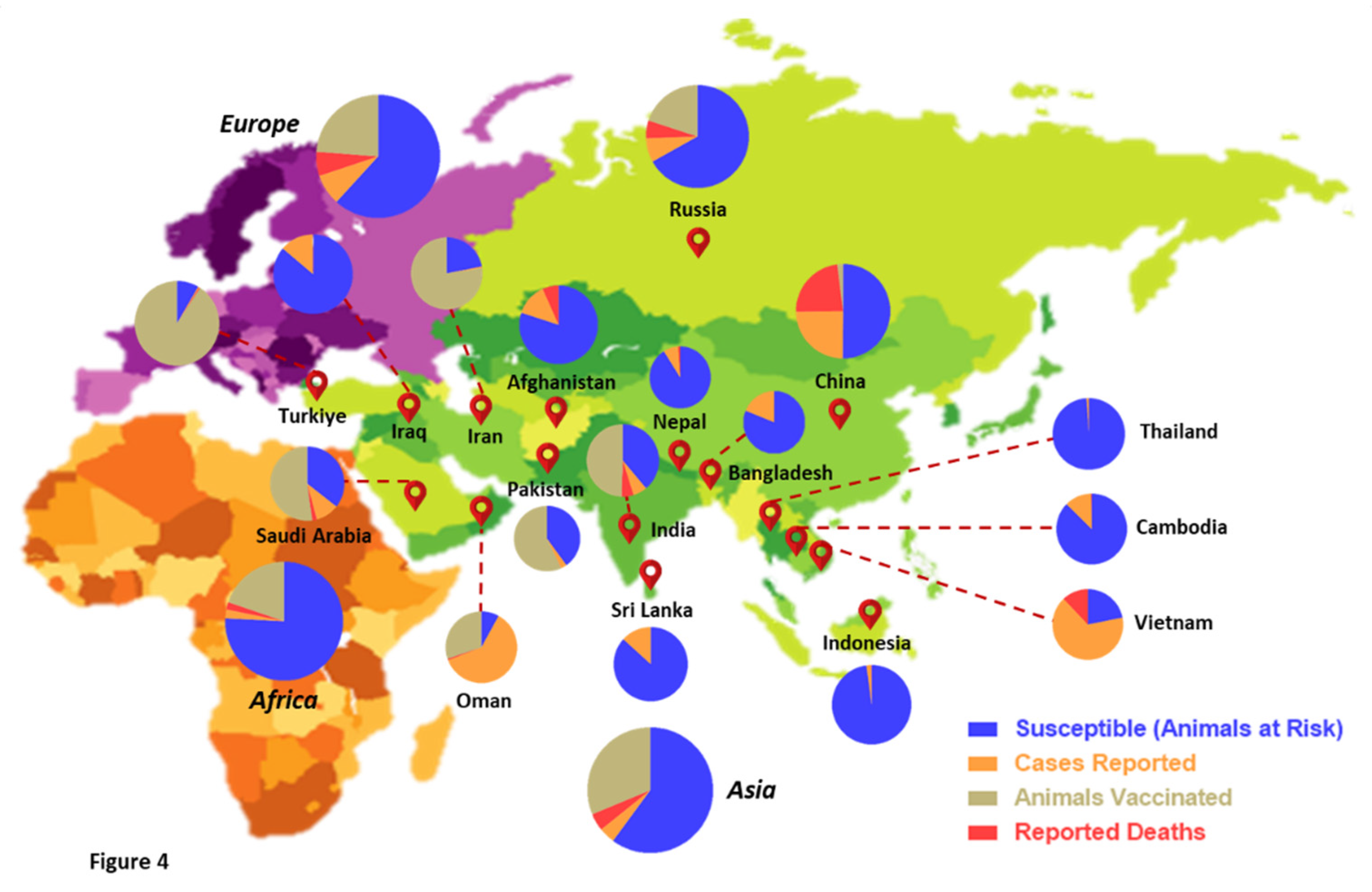
1. Introduction
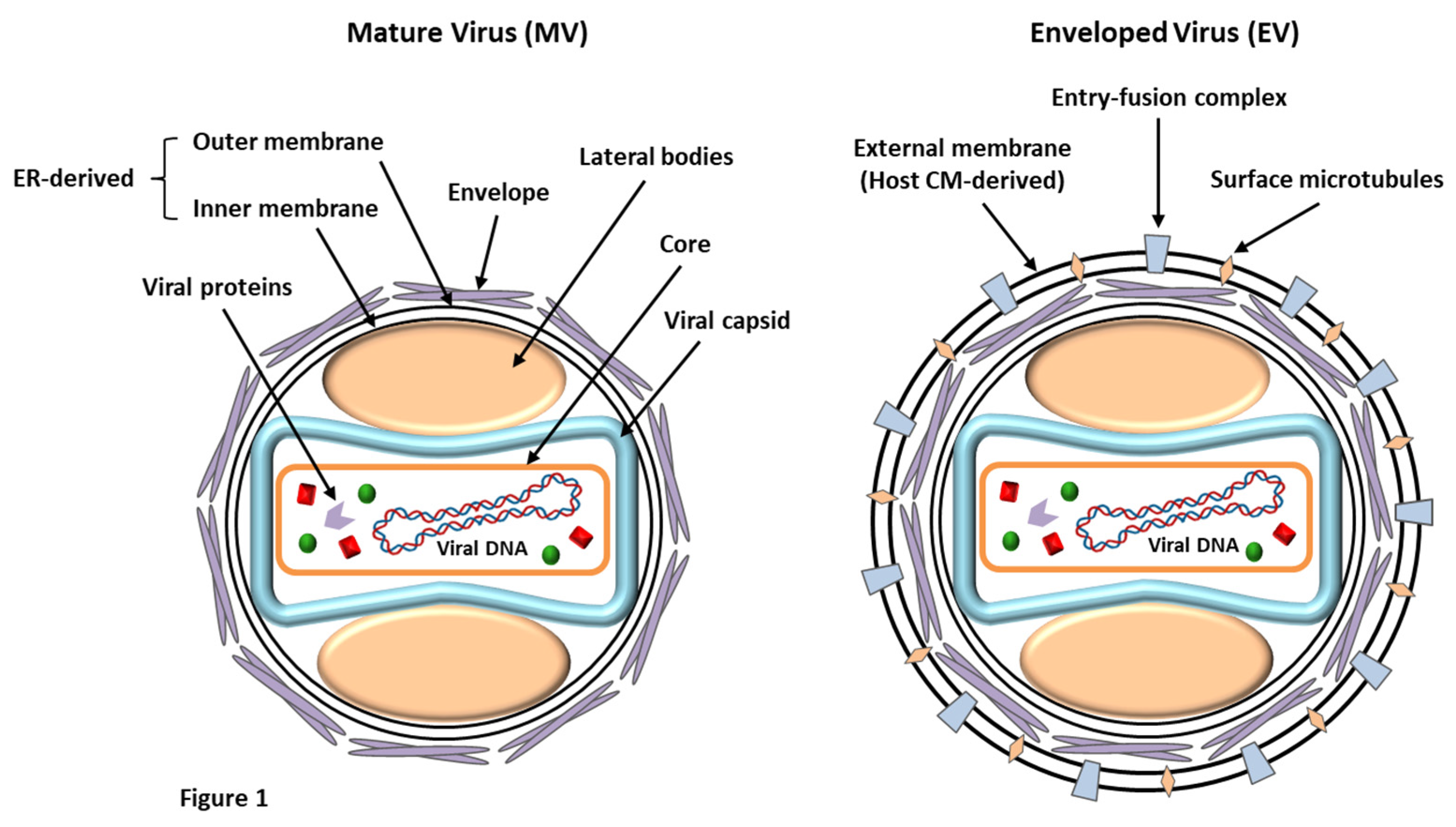
2. Etiology of LSDV: a brief overview of virus structure
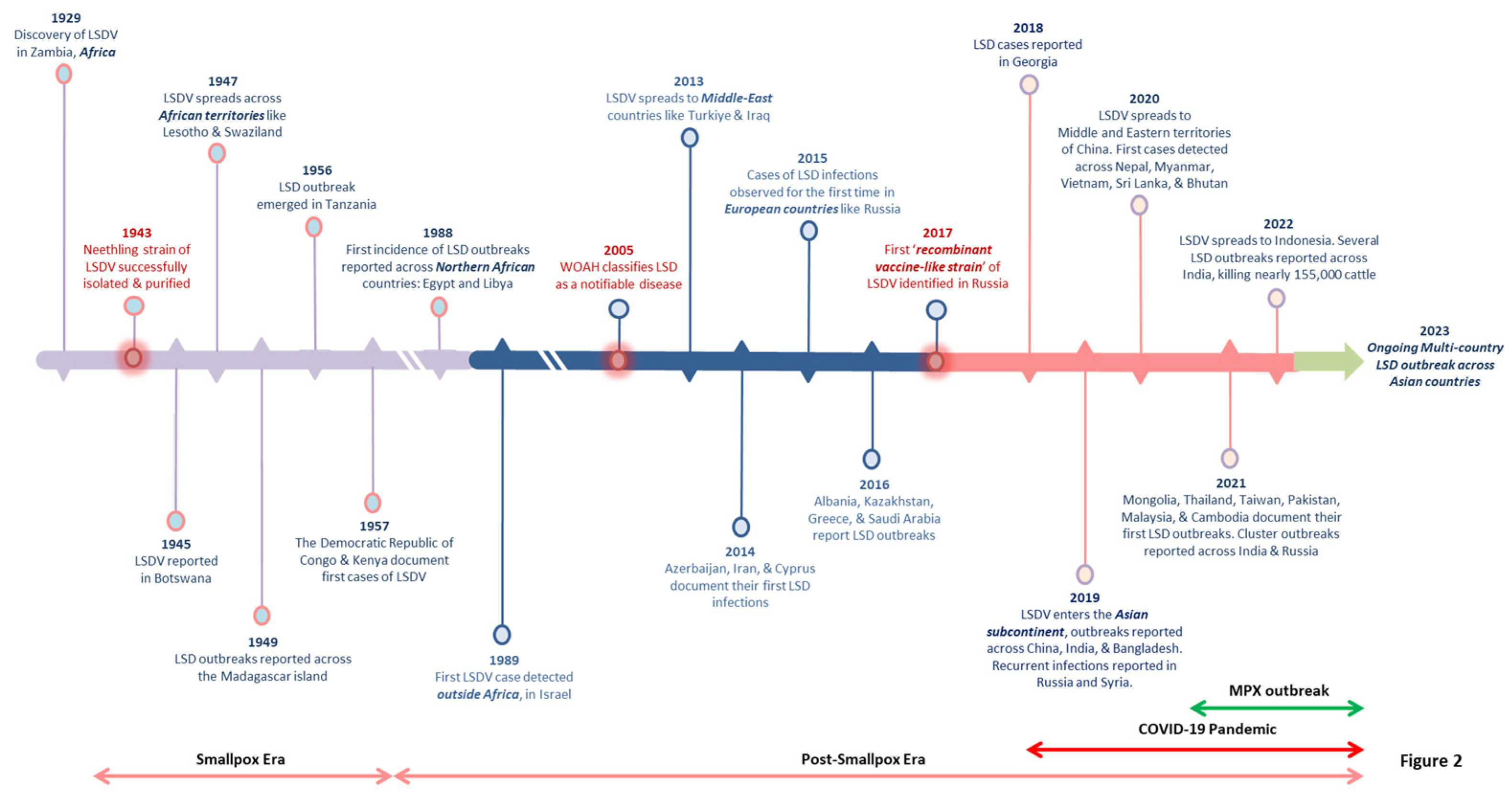
3. Epidemiological trends and the expanding geographical footprint of LSD: unraveling the viral transition
4. Transmission, reservoirs, and hosts of LSDV: a panoramic yet distal view
5. Pathogenesis and clinical representations of LSDV: from signs to symptoms
6. Diagnosis, preventive measures, and treatment of LSD
7. Current scenario & economic repercussions of LSD outbreaks
8. Causes of LSDV resurgence: from ground reality to speculations, and beyond
Conclusion
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Mourya, D.; Yadav, P.; Ullas, P.T.; et al. Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian Journal of Medical Research 2019, 149, 447–467. [Google Scholar] [PubMed]
- Chadha, J.; Khullar, L.; Gulati, P.; et al. Insights into the monkeypox virus: Making of another pandemic within the pandemic? Environmental Microbiology 2022, 24, 4547–4560. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, E.S.M.; Venter, E.H.; Shisler, J.L.; et al. Review: Capripoxvirus Diseases: Current Status and Opportunities for Control. Transboundary and Emerging Diseases 2017, 64, 729–745. [Google Scholar] [CrossRef] [PubMed]
- Khan, Y.R.; Ali, A.; Hussain, K.; et al. A review: Surveillance of lumpy skin disease (LSD) a growing problem in Asia. Microbial Pathogenesis 2021, 158, 105050. [Google Scholar] [CrossRef] [PubMed]
- Diallo, A.; Viljoen, G.J. Genus Capripoxvirus. In: Mercer, A.A., Schmidt, A., Weber, O. (eds) Poxviruses. Birkhäuser Advances in Infectious Diseases. Birkhäuser Basel 2007; 167-181.
- Gupta, T.; Patial, V.; Bali, D.; et al. A review: Lumpy skin disease and its emergence in India. Veterinary Research Communications 2020, 44, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, E.S.M.; Stoltsz, W.H.; Troskie, M.; et al. Potential Role for Ixodid (Hard) Tick Vectors in the Transmission of Lumpy Skin Disease Virus in Cattle. Transboundary and Emerging Diseases 2011, 58, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Yao, K.; Wang, S.; et al. Understanding the research advances on lumpy skin disease: A comprehensive literature review of experimental evidence. Frontiers in Microbiology 2022, 13, 1065894. [Google Scholar] [CrossRef] [PubMed]
- Namazi, F.; Khodakaram-Tafti, A. Lumpy skin disease, an emerging transboundary viral disease: A review. Veterinary Medicine and Science 2021, 7, 888–896. [Google Scholar] [CrossRef]
- Selim, A.; Manaa, E.; Khater, H. Molecular characterization and phylogenetic analysis of lumpy skin disease in Egypt. Comparative Immunology, Microbiology and Infectious Diseases 2021, 79, 101699. [Google Scholar] [CrossRef] [PubMed]
- Ayelet, G.; Haftu, R.; Jemberie, S.; et al. Lumpy skin disease in cattle in central Ethiopia: outbreak investigation and isolation and molecular detection of the virus. Revue Scientifique et Technique de l'OIE 2014, 33, 877–887. [Google Scholar] [CrossRef]
- Anwar, A.; Na-Lampang, K.; Preyavichyapugdee, N.; et al. Lumpy Skin Disease Outbreaks in Africa, Europe, and Asia (2005–2022): Multiple Change Point Analysis and Time Series Forecast. Viruses 2022, 14, 2203. [Google Scholar] [CrossRef] [PubMed]
- Scientific Opinion on lumpy skin disease: EFSA Panel on Animal Health and Welfare (AHAW). EFSA Journal 2015, 13, 3986.
- Bhanuprakash, V.; Hosamani, M.; Singh, R.K. Prospects of control and eradication of capripox from the Indian subcontinent: A perspective. Antiviral Research 2011, 91, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; et al. The Genomes of Sheeppox and Goatpox Viruses. Journal of Virology 2002, 76, 6054–6061. [Google Scholar] [CrossRef] [PubMed]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; et al. Genome of Lumpy Skin Disease Virus. Journal of Virology 2001, 75, 7122–7130. [Google Scholar] [CrossRef] [PubMed]
- Azeem, S.; Sharma, B.; Shabir, S.; et al. Lumpy skin disease is expanding its geographic range: A challenge for Asian livestock management and food security. The Veterinary Journal 2022, 279, 105785. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.A.; Esmat, M.; Attia, H.; et al. Clinical and pathological studies on lumpy skin disease in Egypt. Vet Rec 1990, 127, 549–550. [Google Scholar] [PubMed]
- Yeruham, I.; Nir, O.; Braverman, Y.; et al. Spread of lumpy skin disease in Israeli dairy herds. Veterinary Record 1995, 137, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Lojkić, I.; Šimić, I.; Krešić, N. Complete Genome Sequence of a Lumpy Skin Disease Virus Strain Isolated from the Skin of a Vaccinated Animal. Genome Announcements 2018, 6, e00482-18. [Google Scholar] [CrossRef] [PubMed]
- Byadovskaya, O.; Prutnikov, P.; Shalina, K.; et al. The changing epidemiology of lumpy skin disease in Russia since the first introduction from 2015 to 2020. Transboundary and Emerging Diseases 2022, 69, e2551–e2562. [Google Scholar] [CrossRef] [PubMed]
- Das, M.; Chowdhury, M.; Akter, S.; et al. An updated review on lumpy skin disease: a perspective of Southeast Asian countries. Journal of Advanced Biotechnology and Experimental Therapeutics 2021, 4, 322–333. [Google Scholar] [CrossRef]
- Lu, G.; Xie, J.; Luo, J.; et al. Lumpy skin disease outbreaks in China, since 3 August 2019. Transboundary and Emerging Diseases 2020, 68, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Sudhakar, S.B.; Mishra, N.; Kalaiyarasu, S.; et al. Lumpy skin disease (LSD) outbreaks in cattle in Odisha state, India in August 2019: Epidemiological features and molecular studies. Transboundary and Emerging Diseases 2020, 67, 2408–2422. [Google Scholar] [CrossRef] [PubMed]
- Koirala, P.; Meki, I.K.; Maharjan, M.; et al. Molecular Characterization of the 2020 Outbreak of Lumpy Skin Disease in Nepal. Microorganisms 2022, 10, 539. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Tripathi, B.N. A serious skin virus epidemic sweeping through the Indian subcontinent is a threat to the livelihood of farmers. Virulence 2022, 13, 1943–1944. [Google Scholar] [CrossRef] [PubMed]
- Sprygin, A.; Pestova, Y.; Wallace, D.B.; et al. Transmission of lumpy skin disease virus: A short review. Virus Research 2019, 269, 197637. [Google Scholar] [CrossRef] [PubMed]
- Rouby, S.; Aboulsoud, E. Evidence of intrauterine transmission of lumpy skin disease virus. The Veterinary Journal 2016, 209, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Annandale, C.H.; Holm, D.E.; Ebersohn, K.; et al. Seminal Transmission of Lumpy Skin Disease Virus in Heifers. Transboundary and Emerging Diseases 2014, 61, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Melcher, U.; Sprygin, A.; Babin, Y.; et al. Analysis and insights into recombination signals in lumpy skin disease virus recovered in the field. Plos One 2018, 13, e0207480. [Google Scholar]
- Chihota, C.M.; Rennie, L.F.; Kitching, R.P.; et al. Attempted mechanical transmission of lumpy skin disease virus by biting insects. Medical and Veterinary Entomology 2003, 17, 294–300. [Google Scholar] [CrossRef]
- El-Ansary, R.E.; El-Dabae, W.H.; Bream, A.S.; et al. Isolation and molecular characterization of lumpy skin disease virus from hard ticks, Rhipicephalus (Boophilus) annulatus in Egypt. BMC Veterinary Research 2022, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sprygin, A.; Pestova, Y.; Prutnikov, P.; et al. Detection of vaccine-like lumpy skin disease virus in cattle and Musca domestica L. flies in an outbreak of lumpy skin disease in Russia in 2017. Transboundary and Emerging Diseases 2018, 65, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Neamat-Allah, A.N.F.; Mahmoud, E.A. Assessing the possible causes of hemolytic anemia associated with lumpy skin disease naturally infected buffaloes. Comparative Clinical Pathology 2019, 28, 747–753. [Google Scholar] [CrossRef]
- Jainudeen, M.R. Buffalo husbandry. Asia. Encyclopedia of Dairy Sciences 2002; 186-193.
- Elhaig, M.M.; Selim, A.; Mahmoud, M. Lumpy skin disease in cattle: Frequency of occurrence in a dairy farm and a preliminary assessment of its possible impact on Egyptian buffaloes. Onderstepoort Journal of Veterinary Research 2017, 84, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.D.; Tran, L.H.; Nguyen, H.D.; et al. Characterization of Lumpy skin disease virus isolated from a giraffe in Vietnam. Transboundary and Emerging Diseases 2022, 69, e3268–e3272. [Google Scholar] [CrossRef] [PubMed]
- Fagbo, S.; Coetzer, J.A.W.; Venter, E.H. Seroprevalence of Rift Valley fever and lumpy skin disease in African buffalo Syncerus caffer in the Kruger National Park and Hluhluwe-iMfolozi Park, South Africa. Journal of the South African Veterinary Association 2014, 85, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Babiuk, S.; Bowden, T.R.; Parkyn, G.; et al. Quantification of Lumpy Skin Disease Virus Following Experimental Infection in Cattle. Transboundary and Emerging Diseases 2008, 55, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, E.S.M.; Venter, E.H.; Coetzer, J.A.W. The detection of lumpy skin disease virus in samples of experimentally infected cattle using different diagnostic techniques. Onderstepoort J Vet Res 2005, 72, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Kahana-Sutin, E.; Klement, E.; Lensky, I.; et al. High relative abundance of the stable fly Stomoxys calcitrans is associated with lumpy skin disease outbreaks in Israeli dairy farms. Medical and Veterinary Entomology 2017, 31, 150–160. [Google Scholar] [CrossRef]
- Badhy, S.C.; Chowdhury, M.G.A.; Settypalli, T.B.K.; et al. Molecular characterization of lumpy skin disease virus (LSDV) emerged in Bangladesh reveals unique genetic features compared to contemporary field strains. BMC Veterinary Research 2021, 17, 61. [Google Scholar] [CrossRef] [PubMed]
- Khalafalla, A. Lumpy Skin Disease: An Economically Significant Emerging Disease. In: Cattle Diseases - Molecular and Biochemical Approach 2022; 1-14.
- Beard, P.M. Lumpy skin disease: a direct threat to Europe. Veterinary Record 2016, 178, 557–558. [Google Scholar] [CrossRef] [PubMed]
- Şevik, M.; Doğan, M. Epidemiological and Molecular Studies on Lumpy Skin Disease Outbreaks in Turkey during 2014-2015. Transboundary and Emerging Diseases 2017, 64, 1268–1279. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.S.; Alvarez, J.; Bicout, D.J.; et al. Assessment of the control measures for category A diseases of Animal Health Law: Lumpy Skin Disease. EFSA Journal 2022, 20, e07069. [Google Scholar] [PubMed]
- Ali, A.A.; Neamat-Allah, A.N.F.; Sheire, H.A.; et al. Prevalence, intensity, and impacts of non-cutaneous lesions of lumpy skin disease among some infected cattle flocks in Nile Delta governorates, Egypt. Comparative Clinical Pathology 2021, 30, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Kamr, A.; Hassan, H.; Toribio, R. Oxidative stress, biochemical, and histopathological changes associated with acute lumpy skin disease in cattle. Veterinary World 2022; 1916-1923.
- Abutarbush, S.M.; Ababneh, M.M.; Al Zoubi, I.G.; et al. Lumpy Skin Disease in Jordan: Disease Emergence, Clinical Signs, Complications and Preliminary-associated Economic Losses. Transboundary and Emerging Diseases 2015, 62, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Gaber, A.; Rouby, S.; Elsaied, A.; et al. Assessment of heterologous lumpy skin disease vaccine-induced immunity in pregnant cattle vaccinated at different times of gestation period and their influence on maternally derived antibodies. Veterinary Immunology and Immunopathology 2022, 244, 110380. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Liu, Q.; Jin, N.; et al. A duplex PCR assay for simultaneous detection and differentiation of Capripoxvirus and Orf virus. Molecular and Cellular Probes 2007, 21, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Lamien, C.E.; Lelenta, M.; Goger, W.; et al. Real time PCR method for simultaneous detection, quantitation and differentiation of capripoxviruses. Journal of Virological Methods 2011, 171, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Menasherow, S.; Rubinstein-Giuni, M.; Kovtunenko, A.; et al. Development of an assay to differentiate between virulent and vaccine strains of lumpy skin disease virus (LSDV). Journal of Virological Methods 2014, 199, 95–101. [Google Scholar] [CrossRef]
- Molla, W.; de Jong, M.C.M.; Frankena, K. Temporal and spatial distribution of lumpy skin disease outbreaks in Ethiopia in the period 2000 to 2015. BMC Veterinary Research 2017, 13, 310. [Google Scholar] [CrossRef] [PubMed]
- Aleksandr, K.; Olga, B.; David, W.B.; et al. Non-vector-borne transmission of lumpy skin disease virus. Scientific Reports 2020, 10, 7436. [Google Scholar] [CrossRef]
- Bedeković, T.; Šimić, I.; Krešić, N.; et al. Detection of lumpy skin disease virus in skin lesions, blood, nasal swabs and milk following preventive vaccination. Transboundary and Emerging Diseases 2018, 65, 491–496. [Google Scholar] [CrossRef]
- Tuppurainen, E.; Dietze, K.; Wolff, J.; et al. Review: Vaccines and Vaccination against Lumpy Skin Disease. Vaccines 2021, 9, 1136. [Google Scholar] [CrossRef] [PubMed]
- Kitching, R.P. Vaccines for lumpy skin disease, sheep pox and goat pox. Dev Biol (Basel) 2003, 114, 161–167. [Google Scholar]
- Haegeman, A.; De Leeuw, I.; Mostin, L.; et al. Comparative Evaluation of Lumpy Skin Disease Virus-Based Live Attenuated Vaccines. Vaccines 2021, 9, 473. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, J.; Boumart, Z.; Daouam, S.; et al. Development and Evaluation of an Inactivated Lumpy Skin Disease Vaccine for Cattle. Veterinary Microbiology 2020, 245, 108689. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.; Tuppurainen, E.; Adedeji, A.; et al. Characterization of a Nigerian Lumpy Skin Disease Virus Isolate after Experimental Infection of Cattle. Pathogens 2021, 11, 16. [Google Scholar] [CrossRef] [PubMed]
- Es-sadeqy, Y.; Bamouh, Z.; Ennahli, A.; et al. Development of an inactivated combined vaccine for protection of cattle against lumpy skin disease and bluetongue viruses. Veterinary Microbiology 2021, 256, 109046. [Google Scholar] [CrossRef]
- Kara, P.D.; Mather, A.S.; Pretorius, A.; et al. Characterisation of putative immunomodulatory gene knockouts of lumpy skin disease virus in cattle towards an improved vaccine. Vaccine 2018, 36, 4708–4715. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Oura, C.A.L. Review: Lumpy Skin Disease: An Emerging Threat to Europe, the Middle East and Asia. Transboundary and Emerging Diseases 2012, 59, 40–48. [Google Scholar] [CrossRef] [PubMed]
- LUMPY SKIN DISEASE A field manual for veterinarians. In Food and Agriculture Organization of the United Nations (FAO). Available online: https://www.fao.org/3/i7330e/i7330e.pdf (accessed on 31 January 2023).
- Bhatt, L.; Bhoyar, R.C.; Jolly, B.; et al. The genome sequence of the Lumpy Skin Disease virus from the outbreak in India suggests a distinct lineage of the virus. bioRxiv 2022. [Google Scholar] [CrossRef] [PubMed]
- Pineda, P.S.; Flores, E.B.; Herrera, J.R.V.; et al. Opportunities and Challenges for Improving the Productivity of Swamp Buffaloes in Southeastern Asia. Frontiers in Genetics 2021, 12, 629861. [Google Scholar] [CrossRef] [PubMed]
- Xavier-Roche, A.R.; TagoPacheco, D.; Kamata, A. Introduction and spread of lumpy skin disease in South, East and Southeast Asia - Qualitative risk assessment and management. FAO animal production and health 2020; 1-50.
- Kiplagat, S.K.; Kitala, P.M.; Onono, J.O.; et al. Risk Factors for Outbreaks of Lumpy Skin Disease and the Economic Impact in Cattle Farms of Nakuru County, Kenya. Frontiers in Veterinary Science 2020, 7, 259. [Google Scholar] [CrossRef] [PubMed]
- Casal, J.; Allepuz, A.; Miteva, A.; et al. Economic cost of lumpy skin disease outbreaks in three Balkan countries: Albania, Bulgaria and the Former Yugoslav Republic of Macedonia (2016-2017). Transboundary and Emerging Diseases 2018, 65, 1680–1688. [Google Scholar] [CrossRef]
- The Hindu (Businessline) Slight impact Lumpy skin disease had marginal impact on India’s milk output this year:, U.S.D.A. Available online: https://www.thehindubusinessline.com/economy/agri-business/lumpy-skin-disease-outbreak-marginally-impacted-indias-milk-output-this-year-usda/article66065825.ece (accessed on 31 January 2023).
- Campbell-Lendrum, D.; Manga, L.; Bagayoko, M.; et al. Climate change and vector-borne diseases: what are the implications for public health research and policy? Philosophical Transactions of the Royal Society B: Biological Sciences 2015, 370, 20130552. [Google Scholar] [CrossRef]
- Tuladhar, R.; Singh, A.; Banjara, M.R.; et al. Effect of meteorological factors on the seasonal prevalence of dengue vectors in upland hilly and lowland Terai regions of Nepal. Parasites & Vectors 2019, 12, 42. [Google Scholar]
- Alkhamis, M.A.; VanderWaal, K. Spatial and Temporal Epidemiology of Lumpy Skin Disease in the Middle East, 2012–2015. Frontiers in Veterinary Science 2016, 3, 19. [Google Scholar] [CrossRef] [PubMed]
- Agianniotaki, E.I.; Mathijs, E.; Vandenbussche, F. Complete Genome Sequence of the Lumpy Skin Disease Virus Isolated from the First Reported Case in Greece in 2015. Genome Announcements 2017, 5, e00550-17. [Google Scholar] [CrossRef] [PubMed]
- Gelaye, E.; Belay, A.; Ayelet, G.; et al. Capripox disease in Ethiopia: Genetic differences between field isolates and vaccine strain, and implications for vaccination failure. Antiviral Research 2015, 119, 28–35. [Google Scholar] [CrossRef]
- Kononov, A.; Prutnikov, P.; Shumilova, I.; et al. Determination of lumpy skin disease virus in bovine meat and offal products following experimental infection. Transboundary and Emerging Diseases 2019, 66, 1332–1340. [Google Scholar] [CrossRef]
- Uddin, J.M.; Sprygin, A.; Pestova, Y.; et al. Evidence of recombination of vaccine strains of lumpy skin disease virus with field strains, causing disease. Plos One 2020, 15, e0232584. [Google Scholar]
- Kononova, S.; Kononov, A.; Shumilova, I.; et al. A lumpy skin disease virus which underwent a recombination event demonstrates more aggressive growth in primary cells and cattle than the classical field isolate. Transboundary and Emerging Diseases 2020, 68, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Zeballos, E.; Chelius, C. The effects of grazing on daily caloric intake and dietary quality. International Journal of Behavioral Nutrition and Physical Activity 2021, 18, 163. [Google Scholar] [CrossRef] [PubMed]
- Kegley, E.B.; Ball, J.J.; Beck, P.A.; et al. Impact of mineral and vitamin status on beef cattle immune function and health. Journal of Animal Science 2016, 94, 5401–5413. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, M.; Klement, E. The Effect of Vaccination with Live Attenuated Neethling Lumpy Skin Disease Vaccine on Milk Production and Mortality—An Analysis of 77 Dairy Farms in Israel. Vaccines 2020, 8, 324. [Google Scholar] [CrossRef] [PubMed]
- Nohynek, H.; Wilder-Smith, A. Does the World Still Need New Covid-19 Vaccines? New England Journal of Medicine 2022, 386, 2140–2142. [Google Scholar] [CrossRef] [PubMed]
- Young, M.; Crook, H.; Scott, J.; et al. Covid-19: virology, variants, and vaccines. BMJ Medicine 2022, 1, e000040. [Google Scholar] [CrossRef] [PubMed]
- Chadha, J.; Khullar LMittal, N. Facing the wrath of enigmatic mutations: a review on the emergence of severe acute respiratory syndrome coronavirus 2 variants amid coronavirus disease-19 pandemic. Environmental Microbiology 2021, 24, 2615–2629. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.A.; Chen, X.; Kunasekaran, M.; et al. Global epidemiology of vaccine-derived poliovirus 2016–2021: A descriptive analysis and retrospective case-control study. eClinicalMedicine 2022, 50, 101508. [Google Scholar] [CrossRef] [PubMed]
- Rush, E.R.; Dale, E.; Aguirre, A.A. Illegal Wildlife Trade and Emerging Infectious Diseases: Pervasive Impacts to Species, Ecosystems and Human Health. Animals 2021, 11, 1821. [Google Scholar] [CrossRef] [PubMed]
- Boniface, D.; Tapia-Rico, G. Oncology During the COVID-19 Pandemic: a Lockdown Perspective. Current Oncology Reports 2022, 24, 1219–1235. [Google Scholar] [CrossRef] [PubMed]


| S. No. | Commercial name | Viral strain | Target animal | Viral titer (per dose) | Vaccine efficacy | Reference |
|---|---|---|---|---|---|---|
| 1. | Lumpyvax™ (Intervet (Pty) South Africa/MSD Animal Health) |
LSD SIS Neethling type strain | Cattle | 104.0 TCID50 | ~ 80 % | http://www.msd-animal-health.co.za |
| 2. | Bovivax-LSD™ | LSD Neethling strain | Cattle | 103.5 TCID50 | 100 % | http://www.mci-santeanimale.com/en/ |
| 3. | Lumpy Skin Disease Vaccine for Cattle ( Onderstepoort Biological Products (OBP) South Africa) |
LSD Neethling strain | Cattle | Not known | ~ 70 % | http://www.obpvaccines.co.za |
| 4. | LumpyShield-N™ | LSD Neethling strain | Cattle | 104.0 TCID50 | Not available | http://www.jovaccenter.com |
| 5. | MEVAC LSD | LSD Neethling strain | Cattle | 103.5 TCID50 | ~ 41 % | https://www.me-vac.com/about |
| 6. | Lumpy Skin Disease Vaccine ( National Veterinary Institute (NVI) Ethiopia) |
LSD Neethling strain | Cattle | 103.0TCID50 | 100% |
https://www.nvi.com.et |
| 7. | Lumpivax™ [Kenya Veterinary Vaccines Production Institute (KEVEVAPI)] |
Live attenuated LSDV | Cattle | Not known | 100 % | http://www.kevevapi.org/ |
| 8. | Penpox-M™ Live SPPV |
Bakirköy SPPV strain | Cattle | 102.5 TCID50 | Not available | https://vetkontrol.tarimorman.gov.tr/pendik/Sayfalar/EN/AnaSayfa.aspx |
| 9. | Poxvac™ | Bakirköy SPPV strain | Sheep, Cattle |
102.5 TCID50 | Not available | http://www.vetal.com.tr |
| 10. | Lumpyvac™ | LSD Neethling strain | Cattle | 103.5 TCID50 | Not available | http://www.vetal.com.tr |
| 11. | Poxdoll™ |
Bakirköy SPPV strain | Cattle Sheep Goat |
102.5 TCID50 | Not available | http://www.dollvet.com.tr |
| 12. | LSD-NDOLLTM | LSD Neethling strain | Cattle | 103.5 TCID50 | Not available | http://www.dollvet.com.tr |
| 13. | Sheep Pox Cultural Dry™ |
Arriah SPPV Strain |
Sheep Cattle |
Not known | Not available | http://www.arriah.ru |
| 14. | Herbivac-LS | LSD Neethling strain | Cattle | Not known | 100 % |
https://deltamune.co.za/ |
| 15. | Kenyavac | KSGP 0240 | Sheep, goat, cattle | Not known | 100 % | https://jovaccenter.com |
| 16. | Jovivac | Yugoslavian SPPV RM-65 strain | Sheep, cattle | 103.9 TCID50 | Not available | https://jovaccenter.com |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





