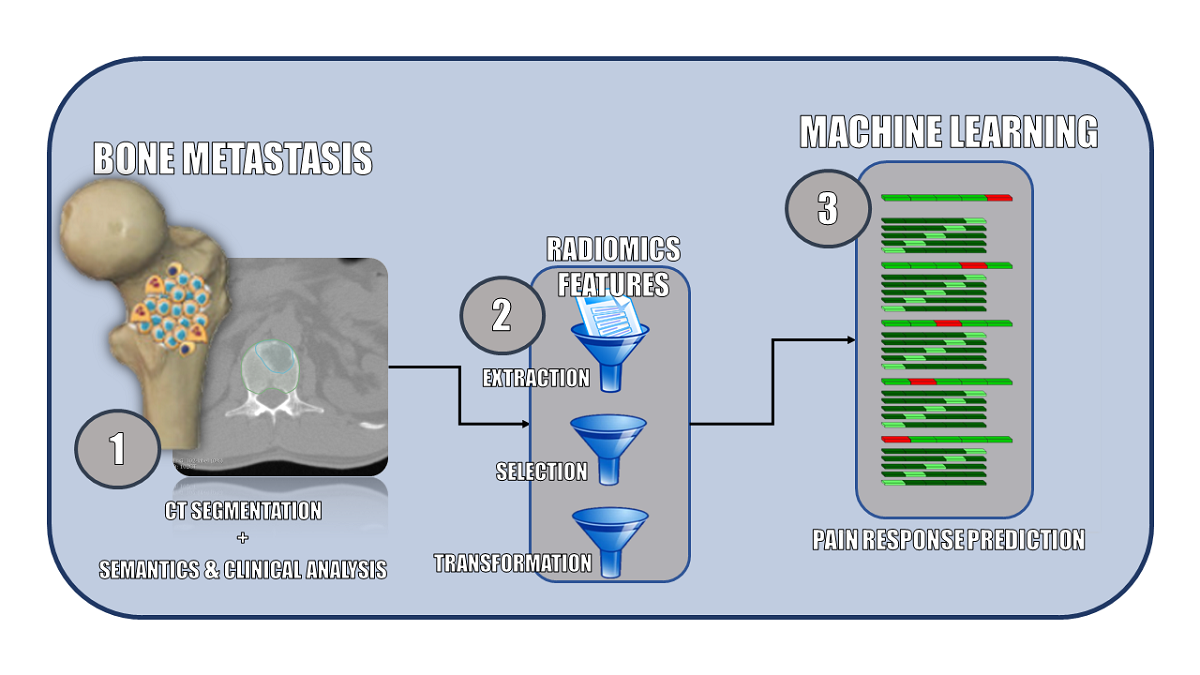
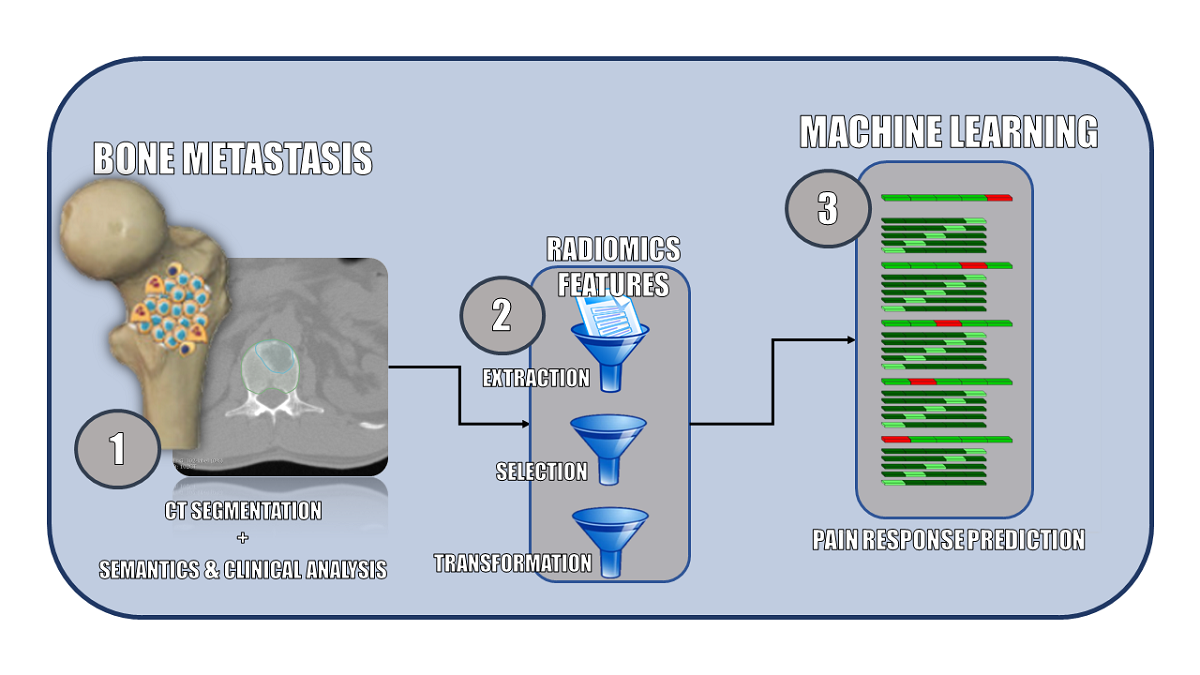
Background: Painful spinal bone metastases (PSBMs) patients regularly receive palliative radiation therapy (RT) with response rates in about 2 of 3 patients. In this exploratory study, we evaluated the value of machine learning (ML) models based on radiomic, semantic and clinical features to predict complete pain response. Methods: Gross tumour volumes (GTV) and clinical target volumes (CTV) of 261 PSBMs were segmented on planning computed tomography (CT) scans. Radiomic, semantic and clinical features were collected for all patients. Random forest (RFC) and support vector machine (SVM) classifiers were compared using repeated nested cross-validation.Results: The best radiomic classifier was trained on CTV with an area under the receiver-operator curve (AUROC) of 0.62 ± 0.01 (RFC; 95% confidence interval). The semantic model achieved a comparable AUROC of 0.63 ± 0.01 (RFC), significantly below the clinical model (SVM, AUROC: 0.80 ± 0.01); and slightly lower than the spinal instability neoplastic score (SINS; LR, AUROC: 0.65 ± 0.01). A combined model did not improve performance (AUROC: 0,74 ± 0,01).Conclusions: We could demonstrate that radiomic and semantic analyses of planning CTs allowed for limited prediction of therapy response to palliative RT. ML predictions based on established clinical parameters achieved the best results.