Submitted:
01 January 2026
Posted:
04 January 2026
You are already at the latest version
Abstract
Keywords:
1. Introduction
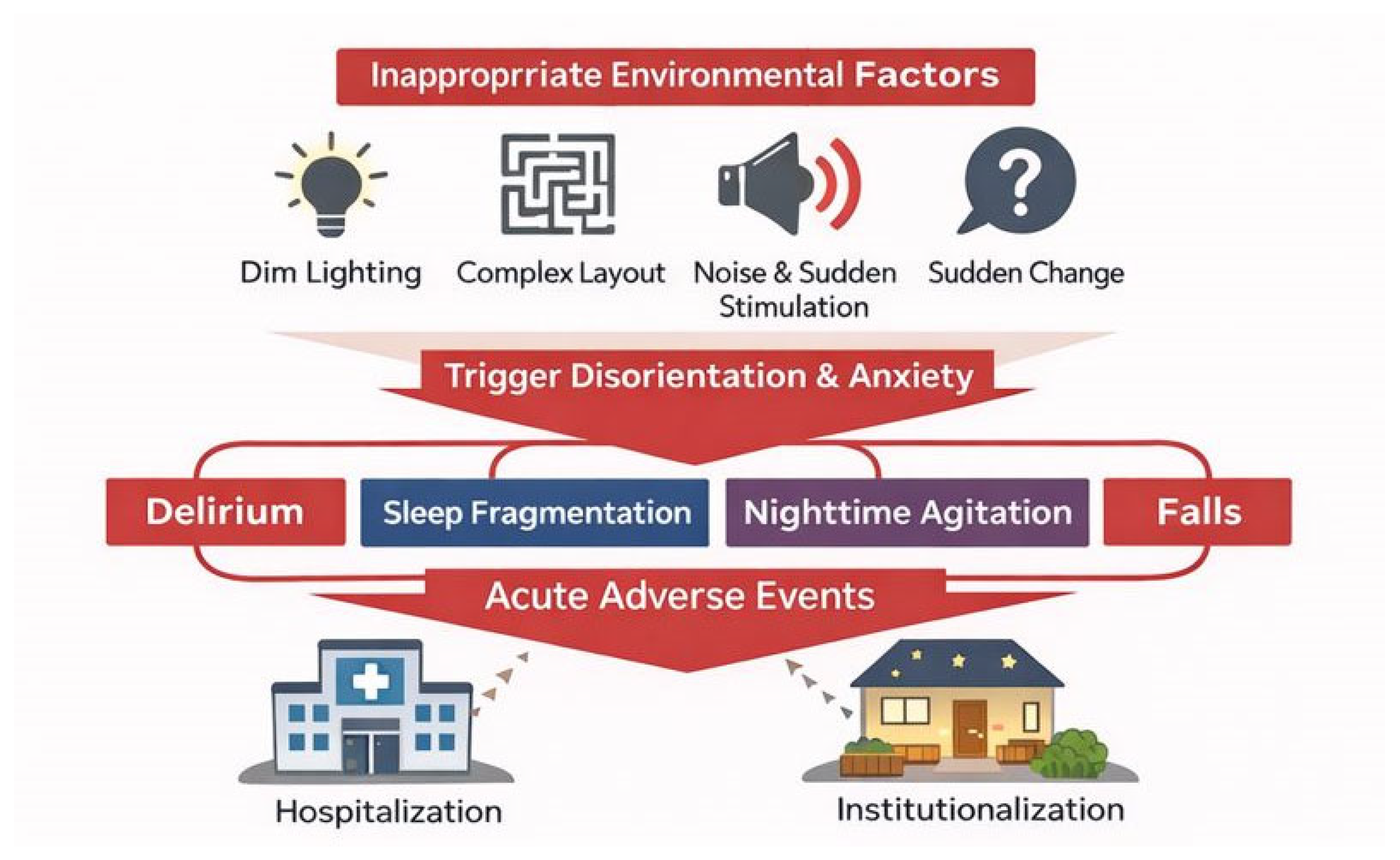
1.1. Redefining the "Environment" in Dementia Care
1.2. Limitations of Conventional Environmental Design Approaches
- Major renovations or dedicated equipment are feasible.
- Caregivers are consistently able to optimize environmental conditions.
- The person with dementia can understand and adapt to changes in the environment.
2. Constraints on Environmental Interventions in Dementia Care
2.1. Cognitive Constraints: Impaired Processing of Temporal and Spatial Cues
2.2. Emotional and Behavioral Constraints: Overstimulation and Reactive BPSD
2.3. Implementation Constraints: Person-Dependent Environmental Management
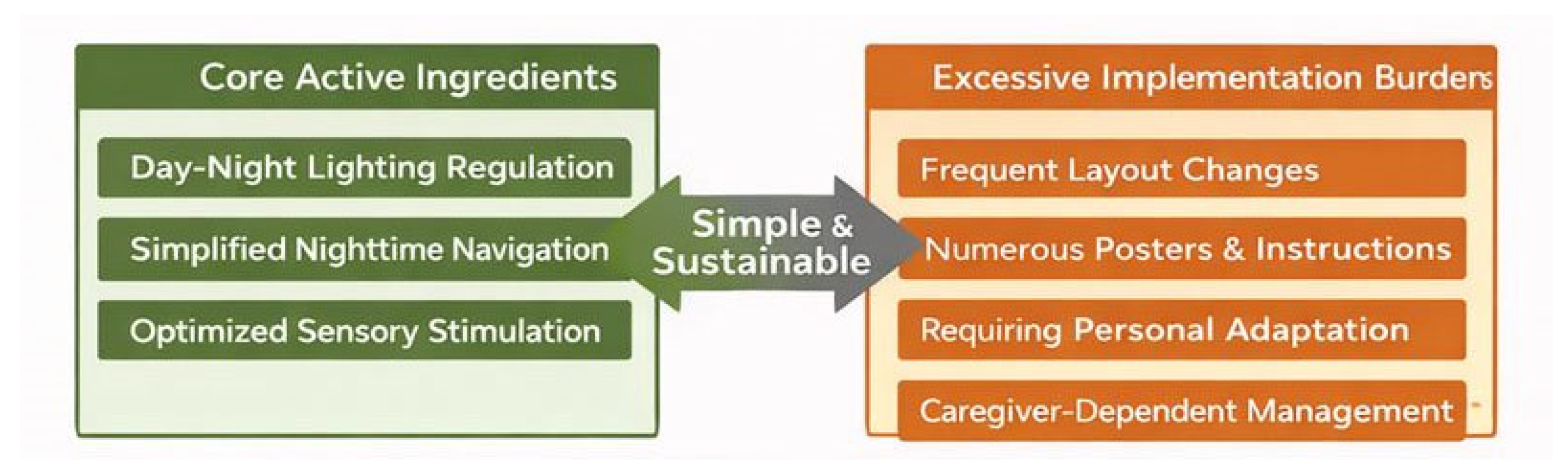
3. Differentiating Core Active Ingredients from Excessive Implementation Burdens
3.1. Core Active Ingredients in Environmental Interventions
- Lighting that clarifies temporal cues for day and night
- Simplification of nighttime pathways and assurance of visibility
- Optimization of sensory stimulation
3.2. Implementation Burdens to Be Eliminated
- Frequent rearrangement of furniture or layout
- Excessive signage and information displays
- Requiring the person with dementia to understand and adapt to environmental changes
- Management dependent on caregiver attention and vigilance
4. Dementia-Adapted Minimal Environmental Intervention Model
4.1. Minimal Component ①: Bright Days, Dark Nights
- Daytime: Maximize natural light and maintain sufficient indoor brightness.
- Nighttime: Use minimal lighting only to ensure footpath visibility.
4.2. Minimal Component ②: Fixed Nighttime Pathways
- Establish a consistent route from bed to toilet.
- Avoid rearranging furniture.
4.3. Minimal Component ③: Reduced Sensory Load
- Avoid keeping the television on continuously or at high volume.
- Minimize nighttime verbal interactions and sudden physical contact.
5. Implementation Protocol (Summary)
- Frequency: Continuous (applied at all times)
- Responsible party: The environment itself (do not place responsibility on the person with dementia)
- Inspection: Simple weekly checks
6. Implications for Research, Practice, and Policy
7. Conclusion
Appendix
- Care workers engaged in facility-based or home-based dementia care
- Family caregivers supporting individuals with dementia
- Medical and welfare professionals seeking to integrate environmental adjustments into daily care without excessive burden
- Individuals with mild to moderate dementia
- Individuals prone to instability in orientation to time, place, or situation
- Individuals exhibiting nighttime agitation, falls, delirium, or hypersensitivity to sensory stimuli
- Persistent severe agitation or aggression, where environmental adjustments alone are insufficient to ensure safety
- Medically unstable conditions such as acute delirium, infection, or severe pain
- Situations where acute-phase medical symptoms requiring clinical judgment take priority
- Do not require the individual to understand, learn, or adapt to the environment
- Avoid interventions that rely on explanations, memory, or judgment
- Avoid sudden stimuli or environmental changes
- If anxiety, confusion, or fear reactions are observed, reduce or stop the intervention immediately
- Keep lighting, pathways, and layout as fixed and consistent as possible
- Do not create environments that change from day to day
- Do not rely on the individual’s attention, judgment, or effort
- Aim to create a state in which “safety is ensured even if the person does nothing”
- Environmental adjustments: Applied continuously
- Inspection and confirmation: Simple checks conducted approximately once per week
- The individual's familiar living environment
- Does not assume major renovations or the use of special equipment
- Makes use of existing resources such as furniture, lighting, and acoustic conditions
- Prevent day-night reversal, nighttime agitation, and delirium
- Support the stabilization of circadian rhythms
- During the daytime, ensure the environment is as bright as possible, using natural and indoor light
- During the nighttime, avoid excessive lighting and use only minimal foot-level lighting as needed
- Do not suddenly switch on ceiling lights at night
- Avoid frequent changes to the color or position of lighting
- Prevent falls, disorientation, and anxiety reactions during the night:
- Fix the route from bed to toilet
- Remove obstacles from walkways
- Install minimal lighting that allows clear visibility of the floor
- Frequent rearrangement of furniture layout
- Temporarily placing objects along the walking path
- Prevent the onset of BPSD, delirium, and anxiety reactions
- Avoid leaving the TV or radio on continuously or at high volume
- Reduce sudden verbal interactions or physical contact during the night
- Minimize unpredictable sounds and light stimuli
- It is not necessary to enforce total silence
- The problems arise from stimuli that are:
- Explaining the reasons for environmental changes and expecting the individual to understand
- Using signs, labels, or notices as cognitive compensation
- Safety measures that depend on the individual's attention or judgment
- Frequent redecorating or rearranging of furniture
- Light intensity (may be reduced if needed)
- Level of sensory stimulation (sound, light, human traffic)
- Degree of pathway simplification
- Clear increase in anxiety, fear, or confusion
- Worsening of nighttime agitation or delirium
- Cases where fall risk increases as a result of the intervention
- The intervention carries extremely low physical invasiveness
- The greatest risk is overzealous environmental modifications driven by good intentions
- Do not aim for a perfect environment
- The mere fact that the environment remains stable is, in itself, the most effective intervention
- The relationship between lighting environment, circadian rhythm, sleep, and delirium
- The relationship between environmental factors, falls, and BPSD
- The positioning of environmental adjustments as a form of non-pharmacological intervention
- Supplementary material to describe the content of interventions
- Documentation of implementation methods and fidelity
- Clarification of the definition of non-pharmacological interventions
- A simple manual for care workers
- Handout materials for family caregivers
- Shared reference for aligning care policies and environmental strategies

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




