Submitted:
24 December 2025
Posted:
25 December 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Subjects
Appliances Design, Expansion Protocol
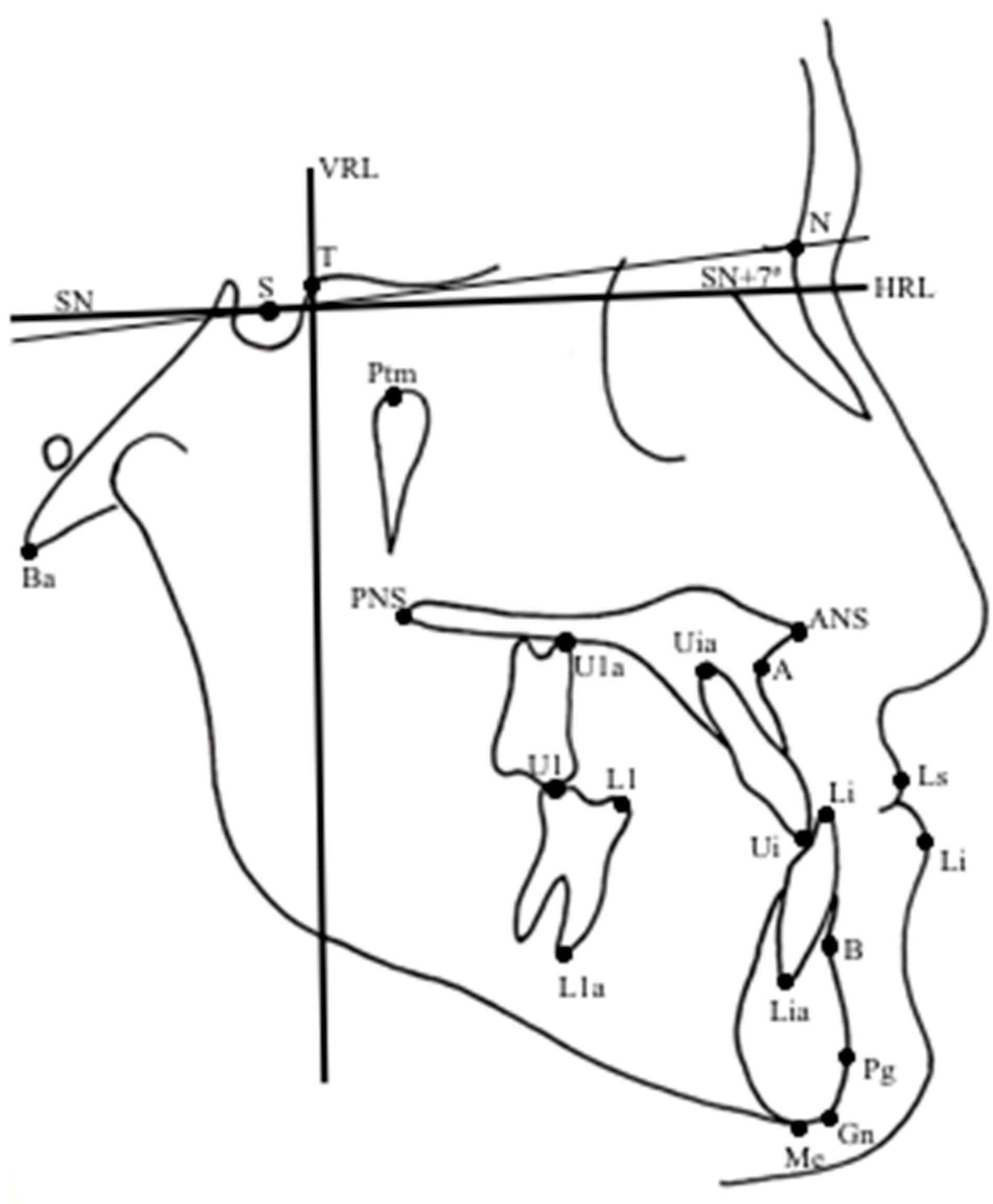
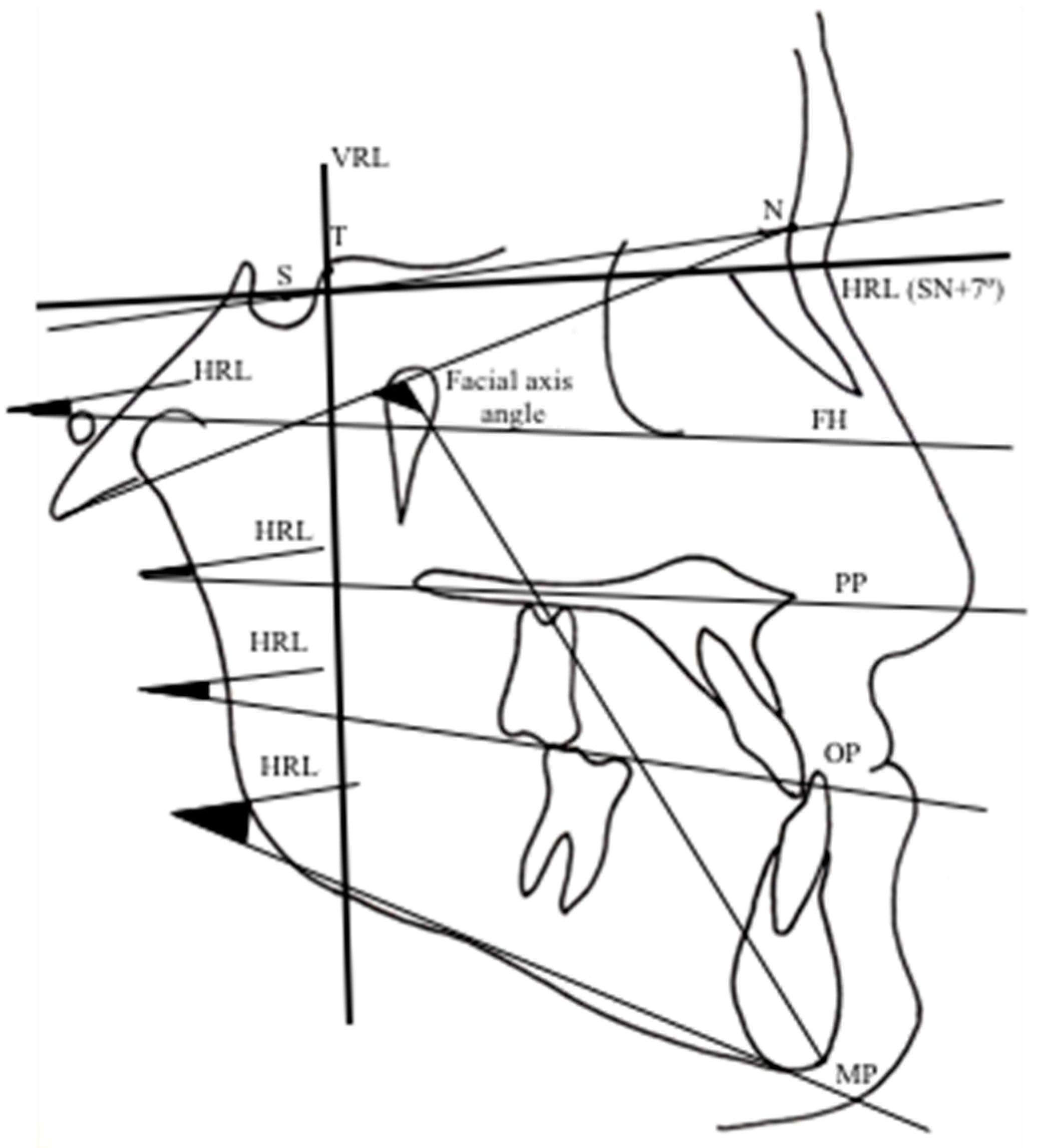
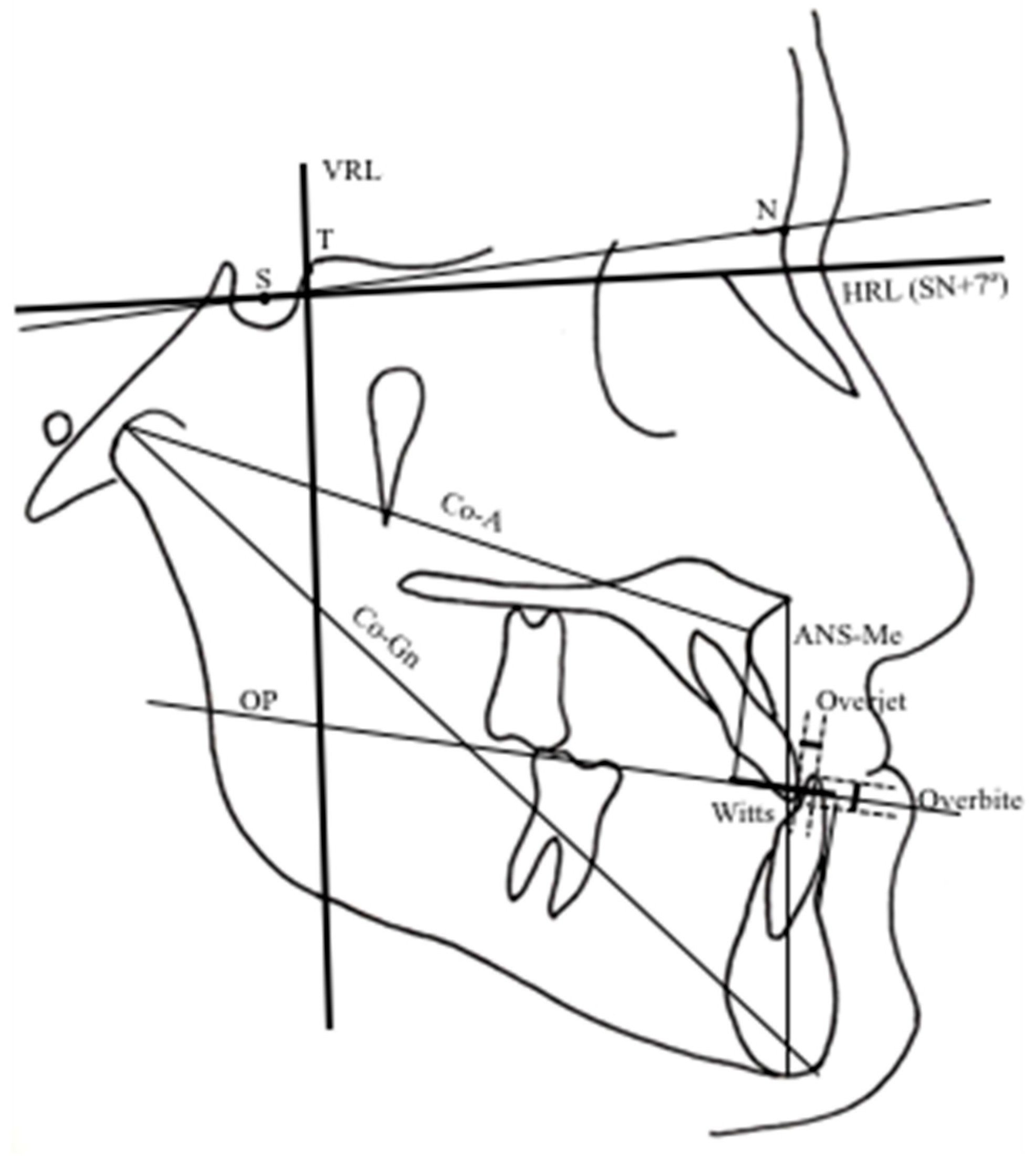
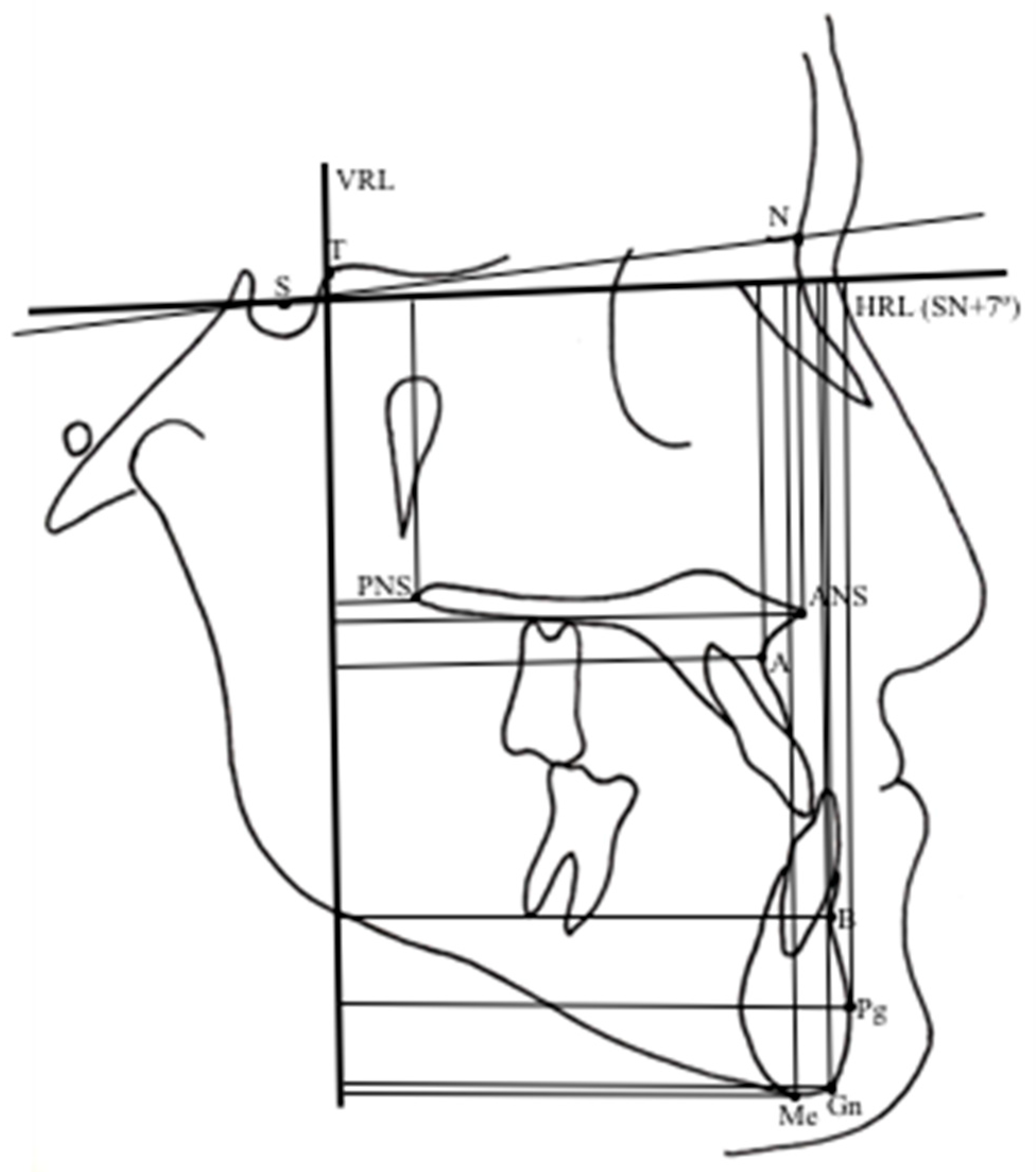
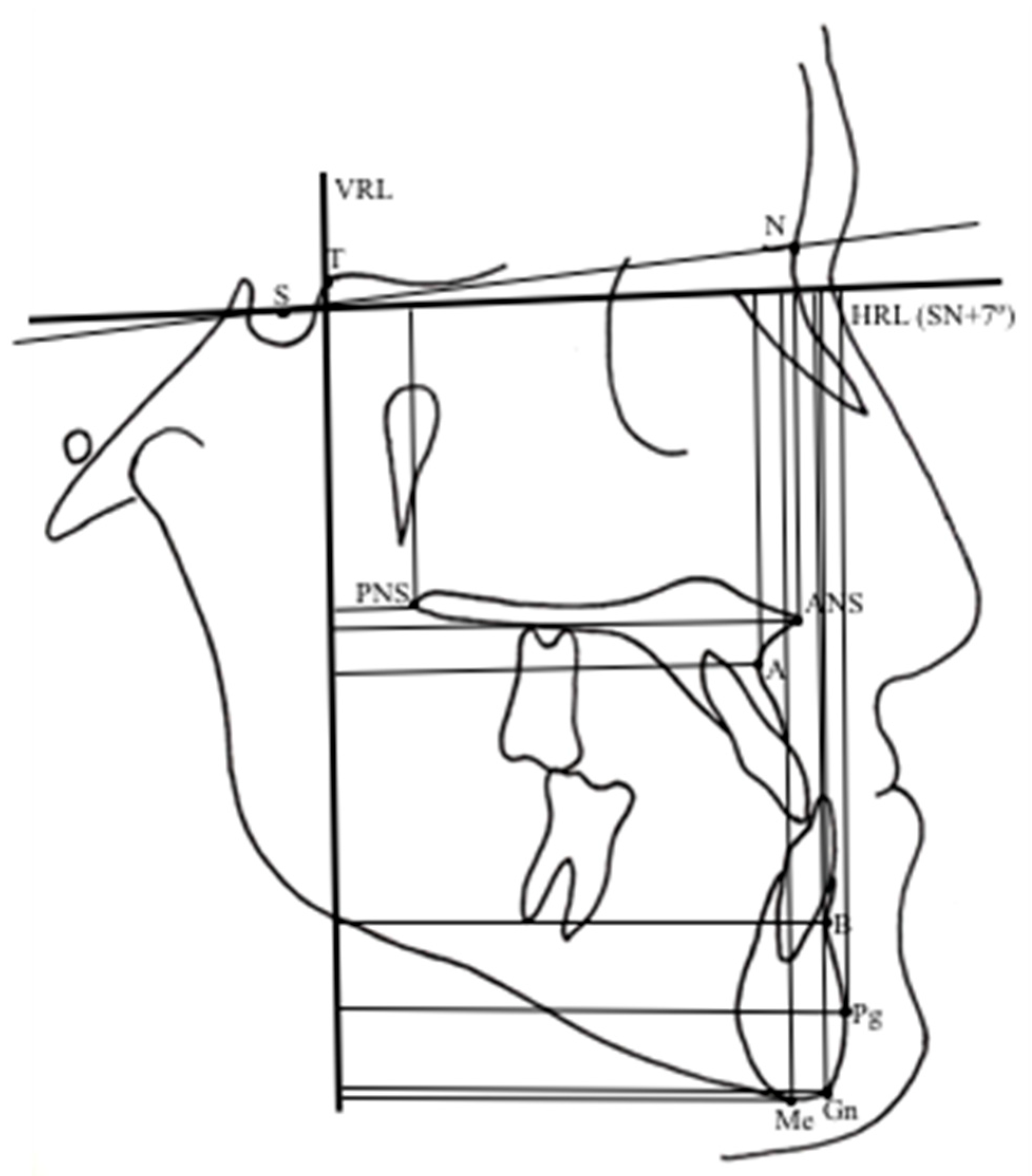
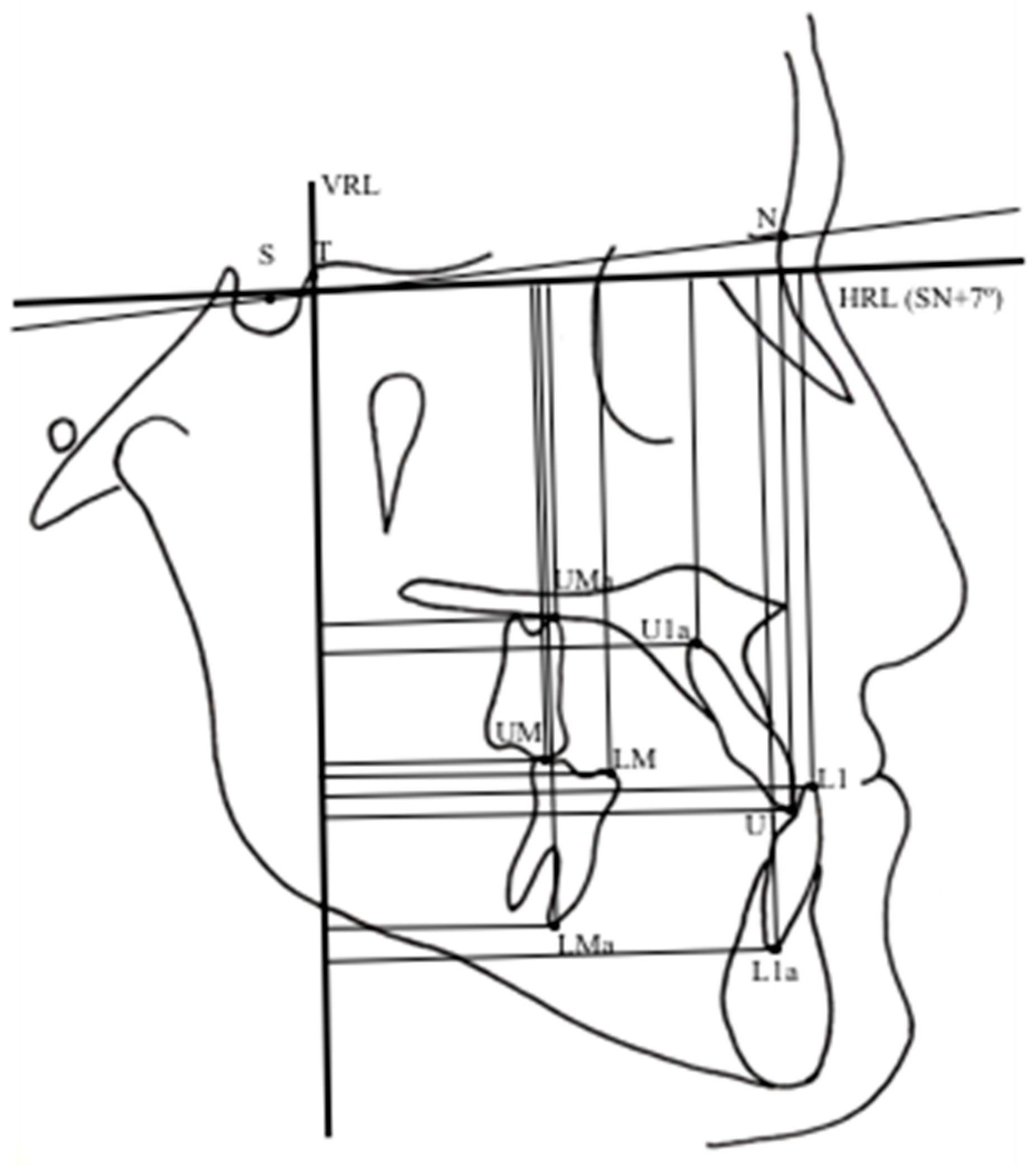
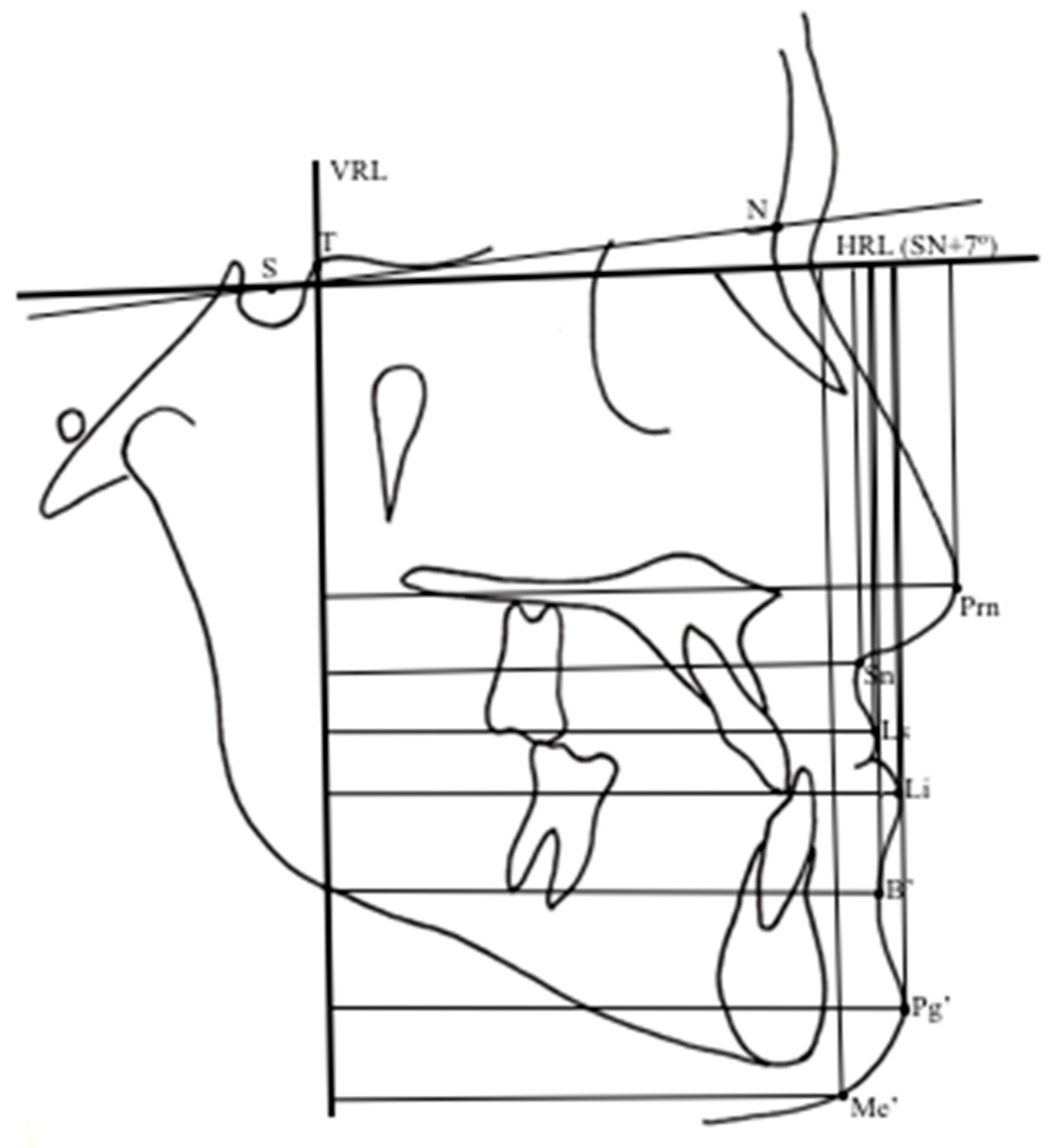
Cephalometric Analysis

Periodontal Evaluation
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Evidence based on outcomes of this study revealed that Alt-RAMEC/2-hinged expander combinations provide more favorable immediate maxillary skeletal advancement (2.56 mm) in growing period.
- Class III malocclusion characterized by maxillary retrusion was improved by combination of both the maxillary counterclockwise rotation and the mandibular clockwise rotation.
- Although plaque formation was controlled, an inflammatory tendency was found in the soft tissue periodontal status during Alt-RAMEC.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| RME | Rapid Maxillary Expansion (RME) |
| Alt-RAMEC | Alternate Rapid Maxillary Expansion and Construction |
| FM | Face Mask |
| CT | Computerized Tomography |
| CBCT | Cone Beam Computerized Tomography |
| HRL | Horizontal Reference Line |
| VRL | Perpendicular Line |
| CVM | Cervical Vertebrae Maturation |
| PI | Plaque Index |
| GI | Gingival Index |
| PPD | Periodontal Pocket Depth |
| BI | Bleeding Index |
| KGT | Keratinized Gingival Tissue |
References
- Haas, AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961, 31, 73–90. [Google Scholar]
- Biederman, W; Chem, B. Rapid correction of Class III malocclusion by midpalatal expansion. Am J Orthod. 1973, 63, 47–55. [Google Scholar] [CrossRef]
- Krag, G; Duterloo, HS; Ten Bosch, JJ. The initial effect of the orthopedic forces: a study of alterations in the craniofacial complex of a macerated human skull. Am J Orthod. 1982, 81, 57–64. [Google Scholar] [CrossRef]
- Nanda, R. Protraction of maxilla in Rhesus monkeys by controlled extraoral forces. Am J Orthod. 1978, 74, 121–141. [Google Scholar] [CrossRef]
- Williams, MD; Sarver, DM; Sadowsky, PL; Bradley, E. Combined rapid maxillary expansion and protraction facemask in the treatment of Class III malocclusions in growing children: A prospective long-term study. Semin Orthod. 1997, 3, 265–274. [Google Scholar] [CrossRef]
- Alcan, T; Keles, A; Erverdi, N. The effects of a modified protraction headgear on maxilla. Am J Orthod Dentofacial Orthop. 2000, 117, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, GA; Mason, B; Moon, HB; Turley, PK. The effects of maxillary protraction therapy with or without rapid palatal expansion: A prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005, 128, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Liou, EJW; Tsai, WC. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of Alternate Rapid Maxillary Expansions and Constrictions. Cleft Palate Craniofac J. 2005, 42, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Masucci, C; Franchi, L; Giuntini, V; Defraia, E. Short-term effects of a modified Alt-RAMEC protocol for early treatment of Class III malocclusion: a controlled study. Orthod Craniofac Res. 2014, 17, 259–269. [Google Scholar] [CrossRef]
- Canturk, BH; Celikoglu, M. Comparison of the effects of face mask treatment started simultaneously and after the completion of the alternate rapid maxillary expansion and constriction procedure. Angle Orthod. 2015, 85, 284–291. [Google Scholar] [CrossRef]
- Kaya, D; Kocadereli, İ; Kan, B; Tasar, F. Effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions: A pilot study. Angle Orthod. 2011, 81, 639–646. [Google Scholar] [CrossRef]
- Isci, D; Turk, T; Elekdag-Turk, S. Activation–deactivation rapid palatal expansion and reverse headgear in Class III cases. Eur J Orthod. 2010, 32, 706–715. [Google Scholar] [CrossRef]
- Sitaropoulou, V; Yılmaz, HN; Yılmaz, B; Küçükkeles, N. Three-dimensional evaluation of treatment results of the Alt-RAMEC and facemask protocol in growing patients. J Orofac Orthop. 2020, 81, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Gökalp, H. Quantitative Evaluation of Consecutively Rapid Maxillary Expansions and Constrictions Effects on Circum-Maxillary Sutures in Boys by SPECT Bone Scintigraphy. EC Dental Science. 2020, 19, 48–59. [Google Scholar]
- Garib, DG; Henriques, JFC; Janson, G; de Freitas, MR; Fernandes, AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006, 129, 749–758. [Google Scholar] [CrossRef]
- Gandedkar, NH; Liou, EJW. The immediate effect of alternate rapid maxillary expansions and constrictions on the alveolus: a retrospective cone beam computed tomography study. Prog Orthod. 2018, 19, 40. [Google Scholar] [CrossRef]
- Broadbent, BH. A new x-ray technique and its application to orthodontia. Angle Orthod. 1931, 1, 45–66. [Google Scholar]
- Silness, J; Löe, H. Periodontal disease in pregnancy. 3. Response to local treatment. Acta Odontol Scand. 1966, 24, 747–759. [Google Scholar] [CrossRef] [PubMed]
- Liu, C; Song, R; Song, Y. Sutural expansion osteogenesis for management of the bony-tissue defect in cleft palate repair: experimental studies in dogs. Plast Reconstr Surg. 2000, 105, 2012–2025. [Google Scholar] [CrossRef]
- Wang, YC; Chang, PMS; Liou, EJW. Opening of circumaxillary sutures by alternate rapid maxillary expansions and constrictions. Angle Orthod. 2009, 79, 230–234. [Google Scholar] [CrossRef]
- Huang, CT; Wang, YC; Huang, CS; Liou, EJW. Maxillary displacement after rapid maxillary expansions: An animal study. J Taiwan Assoc Orthod. 2008, 20, 19–23. [Google Scholar]
- Greenbaum, KR; Zachrisson, BU. The effect of palatal expansion therapy on the periodontal supporting tissues. Am J Orthod. 1982, 81, 12–21. [Google Scholar] [CrossRef] [PubMed]

| n= 15 | Alt-RAMEC Group | Control Group | |||||
|---|---|---|---|---|---|---|---|
| Age (Year) | CVM* Stages | n= 7 | Age (Year) | CVM* Stages | |||
| Mean±SD | CVM II | CVM III | Mean±SD | CVM II | CVM III | ||
| Females 6 | 12.6±1.42 | 3 | 3 | Females 1 | 12.5±1.54 | 0 | 7 |
| Males 9 | 13.1±1,92 | 5 | 4 | Males 6 | 12.6±1.45 | 13 | 7 |
| Screw opening- First week | Screw closing- Second week | |||||
| Morning | Evening | Morning | Evening | |||
| 1st | 2 turns | 2 turns | 8th day | 2 turns | 2 turns | |
| 2nd day | 9th day | |||||
| 3rd day | 10th day | |||||
| 4th day | 11th day | |||||
| 5th day | 12th day | |||||
| 6th day | 13th day | |||||
| 7th day | 14th day | |||||
| Screw opening- Third week | Screw closing- Fourth week | |||||
| Morning | Evening | Morning | Evening | |||
| 15 th day | 2 turns | 2 turns | 22 th day | 2 turns | 2 turns | |
| 16 th day | 23 th day | |||||
| 17th day | 24 th day | |||||
| 18 th day | 25 th day | |||||
| 19 th day | 26th day | |||||
| 20 th day | 27 th day | |||||
| 21 th day | 28 th day | |||||
| Screw opening- Fifth week | Screw closing- Sixth week | |||||
| Morning | Evening | Morning | Evening | |||
| 29th day | 2 turns | 2 turns | 36 th day | 2 turns | 2 turns | |
| 30 th day | 37 th day | |||||
| 31 th day | 38 th day | |||||
| 32 th day | 39 th day | |||||
| 33 th day | 40 th day | |||||
| 34 th day | 41 th day | |||||
| 35 th day | 42 th day | |||||
| Screw opening- Seventh week | Screw closing- Eigth week | |||||
| Morning | Evening | Morning | Evening | |||
| 43 th day | 2 turns | 2 turns | 50 th day | 2 turns | 2 turns | |
| 44 th day | 51 th day | |||||
| 45 th day | 52 th day | |||||
| 46 th day | 53 th day | |||||
| 47 th day | 54 th day | |||||
| 48 th day | 55 th day | |||||
| 49 th day | 56 th day | |||||
| Screw opening- Nineth week | ||||||
| Morning | Evening | |||||
| 2 turns | 2 turns | |||||
| 57th | ||||||
| 58 th | ||||||
| 59 th | ||||||
| 60 th | ||||||
| 61 th | ||||||
| 62 th | ||||||
| 63 th | ||||||
| Measurements | Alt-RAMEC (T0) | Control (T0) | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | P | |
| Nperp-A, mm | -1.00 | 1.91 | -2.14 | 4.10 | Ns |
| Co-A, mm | 85.67 | 7.29 | 88.71 | 6.60 | Ns |
| B-VR, mm | 63.33 | 7.76 | 61.14 | 11.81 | Ns |
| Pog-Nperp, mm | 5.59 | 6.63 | 4.43 | 3.82 | Ns |
| Wits appraisal, mm | -0.67 | 3.09 | 0.57 | 1.40 | Ns |
| FH/MP, ° | 22.46 | 3.38 | 25.14 | 5.58 | Ns |
| NBa/Ptm-Gn, ° | 90.9 | 3.20 | 91.57 | 4.08 | Ns |
| Overjet, mm | -0.43 | 1.51 | 0.14 | 0.38 | ** |
| Overbite, mm | 2.93 | 1.44 | 0.14 | 0.38 | ** |
| Measurements | Alt-RAMEC (T0) | Alt-RAMEC (T1) |
Control (T0) |
Control (T1) |
Mann Whitney U Test P |
||||||
| Maxillary Skeletal | Mean | SD | Mean | SD | P | Mean | SD | Mean | SD | P | |
| Nperp-A, mm | -1.00 | 1.91 | -0.17 | 2.18 | * | -2.14 | 4.10 | -2.57 | 4.39 | Ns | ** |
| A-VRL , mm | 59.37 | 4.01 | 61.93 | 3.98 | ** | 62.71 | 6.32 | 61.14 | 8.12 | Ns | ** |
| A-HRL, mm | 45.57 | 5.60 | 46.70 | 5.93 | Ns | 49.86 | 3.18 | 50.79 | 4.18 | Ns | Ns |
| ANS-VRL, mm | 63.80 | 3.70 | 66.20 | 8.29 | ** | 69.00 | 5.86 | 67.57 | 8.54 | Ns | ** |
| ANS-HRL, mm | 40.97 | 5.45 | 42.97 | 5.38 | Ns | 43.71 | 4.19 | 47.71 | 3.82 | Ns | Ns |
| PNS-VRL, mm | 17.13 | 4.10 | 17.40 | 3.40 | Ns | 16.36 | 4.84 | 17.00 | 5.16 | Ns | Ns |
| PNS-HRL, mm | 40.23 | 4.07 | 41.80 | 4.32 | * | 40.93 | 7.66 | 41.93 | 7.37 | Ns | * |
| Co-A, mm | 85.67 | 7.29 | 88.70 | 5.37 | * | 88.71 | 6.60 | 90.21 | 4.98 | Ns | * |
| Maxillary Dental | |||||||||||
| Ui-Nperp, mm | 20.90 | 2.93 | 22.90 | 3.32 | * | 14.14 | 4.74 | 15.29 | 5.02 | Ns | Ns |
| Ui-APg, mm | 5.97 | 1.93 | 6.17 | 2.24 | Ns | 4.71 | 2.06 | 3.71 | 3.15 | Ns | Ns |
| Ui-VRL, mm | 63.00 | 5.89 | 64.30 | 4.69 | Ns | 65.79 | 6.87 | 66.71 | 10.81 | Ns | Ns |
| Ui-HRL, mm | 67.60 | 7.61 | 68.70 | 6.82 | Ns | 71.43 | 6.65 | 73.79 | 6.04 | Ns | Ns |
| Uia- VRL, mm | 54.70 | 4.12 | 54.90 | 3.27 | Ns | 59.00 | 10.83 | 58.93 | 9.10 | Ns | Ns |
| Uia- HRL, mm | 51.20 | 13.62 | 52.70 | 12.84 | Ns | 50.57 | 8.54 | 52.36 | 7.87 | Ns | Ns |
| U1- VRL, mm | 37.03 | 4.96 | 37.60 | 3.22 | Ns | 35.57 | 5.38 | 36.64 | 7.45 | Ns | Ns |
| U1- HRL, mm | 58.33 | 10.93 | 59.60 | 8.49 | Ns | 60.57 | 11.84 | 63.43 | 9.95 | Ns | * |
| U1a-VRL, mm | 36.10 | 3.31 | 37.20 | 3.25 | Ns | 35.86 | 5.34 | 37.79 | 6.15 | Ns | Ns |
| U1a-HRL, mm | 50.00 | 13.46 | 51.83 | 13.76 | Ns | 43.43 | 7.23 | 46.57 | 5.50 | * | Ns |
| Mandibular Skeletal | |||||||||||
| Nperp-Pg, mm | 5.59 | 6.63 | 2.57 | 5.95 | * | 4.43 | 3.82 | 8.00 | 4.86 | Ns | Ns |
| B-VRL, mm | 63.33 | 7.76 | 61.37 | 5.77 | Ns | 61.14 | 11.81 | 59.36 | 11.1 | Ns | Ns |
| B-HRL, mm | 83.63 | 9.32 | 86.27 | 7.60 | Ns | 86.07 | 11.03 | 87.86 | 6.39 | Ns | Ns |
| Pg-VRL, mm | 63.03 | 7.32 | 61.43 | 7.48 | Ns | 61.07 | 12.1 | 61.43 | 11.98 | Ns | Ns |
| Pg-HRL, mm | 98.33 | 10.85 | 100.60 | 9.27 | Ns | 99.00 | 17.11 | 102.300 | 7.81 | Ns | Ns |
| Go-VRL, mm | 7.30 | 4.31 | 7.37 | 6.21 | Ns | 4.71 | 4.39 | 5.57 | 4.86 | Ns | Ns |
| Go-HRL, mm | 73.33 | 5.79 | 74.07 | 5.91 | Ns | 99.00 | 17.11 | 102.00 | 7.81 | Ns | Ns |
| Co-VRL, mm | 9.53 | 3.38 | 9.40 | 3.38 | Ns | 11.86 | 4.38 | 15.43 | 6.95 | * | Ns |
| Co-HRL, mm | 21.80 | 2.98 | 22.33 | 2.89 | Ns | 81.86 | 11.55 | 78.57 | 4.43 | Ns | Ns |
| Co-Gn, mm | 125.22 | 9.94 | 126.03 | 10.01 | Ns | 116.57 | 8.79 | 114.64 | 6.71 | Ns | Ns |
| Mandibular Dental | |||||||||||
| Li-APg, mm | 5.47 | 2.30 | 4.87 | 2.20 | * | 3.00 | 1.41 | 3.57 | 1.90 | Ns | Ns |
| Li-VRL, mm | 64.93 | 4.76 | 65.400 | 5.11 | Ns | 63.93 | 10.58 | 65.36 | 11.21 | Ns | Ns |
| Li-HRL, mm | 66.33 | 6.97 | 68.20 | 6.30 | Ns | 71.57 | 7.11 | 73.00 | 6.24 | Ns | Ns |
| Lia-VRL, mm | 55.73 | 7.59 | 56.73 | 7.03 | Ns | 46.00 | 17.35 | 53.00 | 13.89 | Ns | Ns |
| Lia-HRL, mm | 86.73 | 7.38 | 88.67 | 6.76 | Ns | 92.00 | 8.08 | 93.57 | 8.16 | Ns | Ns |
| L1-VRL, mm | 39.80 | 7.36 | 40.93 | 4.03 | Ns | 43.36 | 13.48 | 37.29 | 7.50 | Ns | Ns |
| L1-HRL, mm | 68.73 | 10.83 | 68.20 | 8.95 | Ns | 68.57 | 7.30 | 69.86 | 4.88 | Ns | Ns |
| L1a-VRL, mm | 35.47 | 12.92 | 33.40 | 4.88 | Ns | 31.71 | 8.40 | 32.43 | 11.31 | Ns | Ns |
| L1a-HRL, mm | 83.20 | 8.80 | 85.20 | 7.66 | Ns | 86.00 | 7.75 | 87.43 | 5.13 | Ns | Ns |
| Interdental | |||||||||||
| Overjet, mm | -2.57 | 0.86 | -0.43 | 1.51 | ** | 0.14 | 0.38 | 0.29 | 0.76 | Ns | ** |
| Overbite, mm | 2.93 | 1.44 | 1.63 | 1.06 | * | 0.14 | 0.38 | 1.36 | 1.18 | Ns | * |
| Maxillo-Mandibular | |||||||||||
| Wits, mm | -3.13 | 2.88 | -0.67 | 3.09 | * | 0.29 | 0.76 | 0.57 | 1.40 | Ns | * |
| Vertical | |||||||||||
| PP/HRL, ° | 3.80 | 2.46 | 3.87 | 1.96 | Ns | 8.14 | 6.20 | 7.71 | 3.59 | Ns | Ns |
| OP/HRL, ° | 9.53 | 3.38 | 10.60 | 4.7 | Ns | 22.71 | 9.45 | 24.14 | 7.36 | * | Ns |
| MP/HRL, ° | 23.87 | 6.2 | 25.20 | 5.53 | Ns | 22.71 | 9.45 | 24.14 | 7.36 | Ns | Ns |
| FH/MP, ° | 21.80 | 2.98 | 24.70 | 3.26 | ** | 25.14 | 5.58 | 25.57 | 5.38 | Ns | Ns |
| NBa/Ptm-Gn, ° | 88.33 | 3.56 | 87.00 | 3.51 | * | 91.57 | 4.08 | 90.57 | 4.79 | Ns | * |
| ANS-Me, mm | 65.28 | 6.07 | 68.12 | 5.28 | ** | 68.14 | 4.30 | 68.43 | 2.82 | Ns | ** |
| Soft tissue Profile | |||||||||||
| Prn-VRL, mm | 89.07 | 5.51 | 90.80 | 5.97 | * | 95.00 | 3.32 | 96.57 | 6.24 | Ns | * |
| Prn-HRL, mm | 35.73 | 7.46 | 35.47 | 5.79 | Ns | 45.86 | 4.46 | 46.57 | 4.46 | Ns | Ns |
| Sn-VRL, mm | 74.73 | 4.46 | 76.33 | 4.48 | Ns | 81.43 | 5.06 | 80.43 | 6.58 | Ns | * |
| Sn-HRL, mm | 46.93 | 7.04 | 46.80 | 6.18 | Ns | 54.00 | 1 2.85 | 56.43 | 13.67 | * | Ns |
| Ls-E line, mm | -6.93 | 2.89 | -5.60 | 2.75 | * | -3.50 | 3.14 | -3.93 | 5.47 | Ns | * |
| Ls-VRL, mm | 76.87 | 5.13 | 78.50 | 5.10 | Ns | 78.79 | 6.95 | 76.64 | 10.17 | Ns | * |
| Ls-HRL, mm | 57.73 | 6.70 | 59.07 | 6.27 | Ns | 64.14 | 9.53 | 63.29 | 5.91 | Ns | Ns |
| Li-E, mm | -0.33 | 3.81 | -1.13 | 3.18 | Ns | -0.57 | 4.65 | 0.71 | 3.9 | Ns | Ns |
| Li-VRL, mm | 77.40 | 5.90 | 77.00 | 8.49 | Ns | 75.71 | 12.808 | 80.00 | 9.95 | * | Ns |
| Li-HRL, mm | 73.73 | 7.46 | 75.47 | 7.04 | Ns | 78.29 | 9.89 | 84.00 | 7.57 | * | Ns |
| B’-VRL, mm | 73.47 | 11.78 | 73.67 | 7.02 | Ns | 73.86 | 10.96 | 77.43 | 8.87 | * | Ns |
| B’-HRL, mm | 83.13 | 8.16 | 85.93 | 7.69 | Ns | 84.71 | 12.85 | 86.57 | 13.15 | Ns | Ns |
| Pg’-VRL, mm | 75.07 | 11.07 | 72.53 | 8.58 | Ns | 66.43 | 16.62 | 67.29 | 11.61 | Ns | Ns |
| Pg’-HRL, mm | 96.53 | 8.27 | 98.07 | 8.19 | Ns | 102.43 | 5.68 | 101.71 | 9.39 | Ns | Ns |
| Me’-VRL, mm | 55.60 | 6.87 | 54.93 | 8.49 | Ns | 49.79 | 9.49 | 52.07 | 10.21 | Ns | Ns |
| Me’-HRL, mm | 109.33 | 13.56 | 113.07 | 11.26 | Ns | 109.71 | 6.87 | 111.86 | 7.47 | Ns | Ns |
| Naso-labial angle | 102.87 | 14.34 | 103.27 | 13.04 | Ns | 113.57 | 16.37 | 114.57 | 15.16 | Ns | Ns |
| Mento-labial angle | 136.73 | 11.91 | 142.33 | 9.95 | Ns | 125.86 | 24.51 | 127.71 | 16.35 | Ns | Ns |
| Measurements | Alt-RAMEC (T0) | Alt-RAMEC (T1) |
P | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Intercanine distance, mm | 34.77 | 3.16 | 37.83 | 2.60 | ** |
| First inter first premolar distance, mm | 31.19 | 2.69 | 36.52 | 2.43 | ** |
| Intermolar distance, mm | 39.98 | 3.71 | 40.85 | 3.66 | * |
| Upper arch lenght, mm | 37.54 | 4.28 | 38.86 | 4.14 | * |
| Incisors (T0) |
Incisors (T1) |
P | Premolars (T0) |
Premolars (T1) |
P | Molars (T0) |
Molars (T1) |
P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| PI | 0.61 | 0.47 | 0.73 | 0.32 | NS | 0.71 | 0.47 | 0.83 | 0.32 | NS | 0.81 | 0.47 | 0.83 | 0.32 | NS |
| GI | 0.54 | 0.12 | 0.78 | 0.31 | * | 0.63 | 0.12 | 0.77 | 0.31 | * | 0.78 | 0.12 | 0.87 | 0.31 | * |
| PPD | 1.18 | 0.22 | 1.33 | 0.28 | * | 1.17 | 0.22 | 1.55 | 0.28 | * | 1.23 | 0.22 | 1.37 | 0.28 | * |
| BI | 1.00 | 1.01 | 1.00 | 1.00 | ** | 1.00 | 1.00 | 1.00 | 1.00 | ** | 1.00 | 1.00 | 1.00 | 1.00 | ** |
| KGT | 7.80 | 1.52 | 8.13 | 1.19 | NS | 6.07 | 1.67 | 7.13 | 1.46 | NS | 6.13 | 1.42 | 7.13 | 1.25 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.




