1. Introduction
Traditional methods investigating the function of the middle ear (e.g., otoscopy and tone audiometry) are highly subjective as they rely on visual cues and patients' reports. As these patients' reports are highly subjective and based on their memories, they are likely to be unreliable in many cases. For example, the reported or documented patient history can never rule out a condition like otitis media, which may be asymptomatic [
1].
Over the past century, objective middle ear diagnostics have evolved significantly. In the 1940s, tympanometry was developed, and it became widely used in the 1960s. Tympanometry measures the mobility of the tympanic membrane in response to changes in air pressure and, therewith, analyzes the middle ear function. In the 1970s, multi-frequency tympanometry enhanced the diagnostic option without being widely adopted in clinical applications. [
2]
All around the world, tympanometry has become a standard procedure in patients; though, it’s a non-optimal measurement. On the one hand, the accuracy in predicting middle ear effusions is poor. It can be incorrect in around 50% of the cases [
3]. On the other hand, there is a need for air pressure applied to the outer ear canal, as it measures the mobility of the tympanic membrane in response to changes in air pressure. It therefore needs a sealed ear canal, which can be uncomfortable for patients and can also be challenging for the audiometry staff to achieve, and in some cases, even impossible (e.g., perforation of the tympanic eardrum, radical cavity, gaping tube, or myringosclerosis) [
4,
5,
6,
7,
8].
Most recently, optical coherence tomography has been shown to allow a non-invasive imaging of the middle ear and provide real-time diagnostics in patients with otosclerosis or acute otitis media [
9]. The positive aspect of optical coherence tomography is its high resolution. However, the negative aspect is a limited view and the need for special training for analyzing measurement results [
10]. In addition, machine learning has been shown to improve diagnostic accuracy, especially in children, which enables the identification of middle ear effusions [
11]. These innovative technologies are performed in addition to established techniques for a more precise and reliable diagnosis of the middle ear [
12]. Besides these, many other approaches have been investigated in research; most of them remain experimental and are not, or at least not widely used in clinical practice [
13].
A potential improvement to the traditional tympanometry is the so-called wideband tympanometry. In contrast to the single frequency used in traditional tympanometry, this technique uses a stimulation signal of a wide range of frequencies and analyzes the wideband absorbance. The wide range of analyzed frequencies aims to investigate more useful insights into the middle ear function (e.g., ossicular chain pathologies, superior semicircular canal dehiscence, or otosclerosis) [
14,
15,
16].
In this article, we want to take a closer look at another new method for analyzing the middle ear function in a similar way to tympanometry. The main difference is that the Neuranix Medwave doesn’t need any pressure applied to the patient and therefore is not limited by issues like the mentioned discomfort from air pressure and the partly challenging sealing of the outer ear canal. But as it’s a new technique, there is a need for clinical investigation regarding handling, ease of interpretation, and reliability of the results.
2. Materials and Methods
This observational retrospective, mono-centric study included all patients from 2024 to 2025 who were tested using Medwave (Neuranix Srl, Gardigiano di Scorze, Italy) [
17,
18]. We used two Medwave devices with the latest software version.
To perform the measurement using the Medwave device, it is necessary to use soundproof earplugs to reduce ambient noise. Note that one benefit of this new measurement technique is that the device does not need pressure-tight earplugs, which are still crucial in standard tympanometry. Here, they help maintain consistent pressure in the ear, reducing discomfort induced by pressure changes during the test.
Before measurement, we selected individual standard earplugs for every patient. Sanibel ADI earplugs were used in various forms (i.e., cap, flanged, and flanged with additional lamellae), ranging from 3mm to 19mm.
The Medwave device (see
Figure 1a) is an active diagnostic medical device for measuring middle ear impedance without air pressure variation in the ear canal. It is an innovative device based on PLAI (Pressure Less Acoustic Immittance) technology, which assesses the functional status of the middle ear by quantifying the properties of the eardrum when exposed to a wide range of sound frequencies. The ability to perform the test without changing the pressure in the ear canal allows Medwave to be used pre-, intra-, and postoperatively to check the condition of the eardrum perforation.
The device consists of a calibrated impedance probe (see
Figure 1b), which is coupled to the ear canal via an earplug. The probe primarily consists of a tube in which two microphones and a loudspeaker are positioned at a well-defined distance. The two microphones are positioned so they can pick up the speed of the moving air molecules to measure the velocity of the sound. The loudspeaker is located at the end of the tube. By measuring the sound velocity, the Acoustic Impedance/Admittance can be easily determined (Impedance = Pressure (p) / Velocity (v)).
The probe is inserted into the external auditory canal. Care must be taken to ensure that the probe is not moved during the measurement and that it remains positioned longitudinally to the external auditory canal, in the same direction that would ideally allow observation of the eardrum. Compliance with this measurement condition is essential because probe movements or vibration could cause artifacts, and the wrong angle could generate impedance signals.
By inserting the Medwave probe into the external auditory canal, Medwave automatically initiates a calibration procedure and afterward the impedance measurement. The operating principle is based on state-of-the-art electronic components (precision microphones, MEMS micro-electro-mechanical systems) that are capable of measuring the acoustic signal in the ear canal and calculating the complex acoustic admittance (Y) based on the evaluation of the response in a range between 100 and 3000 Hz. The complex acoustic impedance (Z) is an indicator of how the applied acoustic energy is absorbed by the eardrum and the ear system in general and is a function of frequency. Admittance (Y) is defined as the inverse of impedance and is often used as an equivalent alternative. When the modulus of impedance is minimal, the admittance is at its maximum. The result of the measurement performed with Medwave® is expressed in objective numerical terms:
Ve = equivalent volume of the ear canal
fR = value of the frequency at which the maximum value (P) of the admittance curve (module) occurs
P = peak admittance value (module)
All shape parameters necessary for classification are obtained from the recorded curves.
As a comparison measurement, tympanometry was performed using the GSI 39 (gsi (Granson-Stadler), Eden Prairie, Minnesota) [
19] or the eTymp (Merz Medizintechnik GmbH, Reutlingen, Germany) [
20]. The resulting tympanometry curves were separated into the following types, shown in
Table 1 [
21,
22,
23]. In contrast to the standard procedure, we differentiated type C into two subtypes called “C-“ and “C+” to pay attention to whether the peak was shifted to the left (negative pressure) or to the right (positive pressure). As recommended by the literature, we analyzed the mobility of the eardrum using a probe tone of 226Hz as a standard value and 1000Hz for patients below one year of age due to a lower ear canal volume and resulting higher resonance frequency [
24,
25,
26].
In addition, for some patients, the otoscopy results or known normal hearing without any known health issues were included in the study’s retrospective analysis. For otoscopy, our ENT department uses HEINE BETA 200 diagnostic otoscope (HEINE Optotechnik GmbH & Co. KG, Gilching, Germany) [
27] or Zeiss Opmi Pico surgery microscope (Carl Zeiss Meditec AG, Jena, Germany) [
28].
The anonymous data export was performed using Innoforce ENTstatistics (Ruggell, Liechtenstein), analyzing all patients via the export tool. This concept was approved by our university ethics commission (project number 24-0923).
In addition to the retrospective analysis, we had a closer look at an individual case of paracentesis and, later on, a second paracentesis plus tube insertion. In this case, we received individual consent from the patient to be able to use her data in this manuscript.
The data analysis for this paper was generated using the Real Statistics Resource Pack software (Release 9.3). Copyright (2013–2025) Charles Zaiontz.
www.real-statistics.com (accessed on December 2024). Numerical values were tested for normal distribution using the Shapiro–Wilk test. The two-tailed Mann-Whitney Test for Two Independent Samples was performed to test for significant differences. Holm’s method was used to correct the results of the Mann-Whitney Test for Two Independent Samples in multiple comparisons. The Spearman’s rank test was performed to test correlations. Probability values of p < 0.05 were considered significant.
3. Results
3.1. Descriptive Analysis of the Retrospective Data
The retrospective analysis found 106 patients (102 patients bilaterally, 3 patients left-sided, and 1 right-sided) tested by the Medwave device in the time range of 2024 to 2025. This results in 208 ears tested by the Medwave device. The mean age of these patients was 33.48 +- 23.92 years with a minimum value of 0 years and a maximum value of 87 years. There were 48 male patients and 58 female patients. 26 patients had no hearing problem bilaterally, and 13 had a single-sided hearing problem. This results in 65 ears with no hearing problem. The onset of hearing loss was documented in the following categories: no hearing loss, prenatal hearing loss, hearing loss during the 0-1 year age range, during the 1-5 year age range, during the 5-20 year age range, and hearing loss after the age of 20. The 65 ears with no hearing loss were matched between documentation of etiology and the start of hearing loss. 36 ears had a start of hearing loss during the prenatal phase. No ear was categorized at the start of hearing loss between 0 and 1 years of age. 26 ears had a start of hearing loss between 1 and 5 years of age. 7 ears suffered from hearing loss between the ages of 5 to 20 years. In 48 ears, the hearing loss started after the age of 20.
In 106 ears, a type A tympanogram or no known ear problem was found (in case of result uncertainty, verified by otoscopy. For further analysis, these ears were all stated as type A. In seven ears, a type As was found. In three ears, a type Ad was found. Type B was found in 19 ears. Type C+ was found in 2 ears, while type C- was found in 13 ears. In two ears, the tympanometry could not be performed due to sealing problems. In the remaining 60 ears, no corresponding tympanometry was available for comparison with the Medwave measurement.
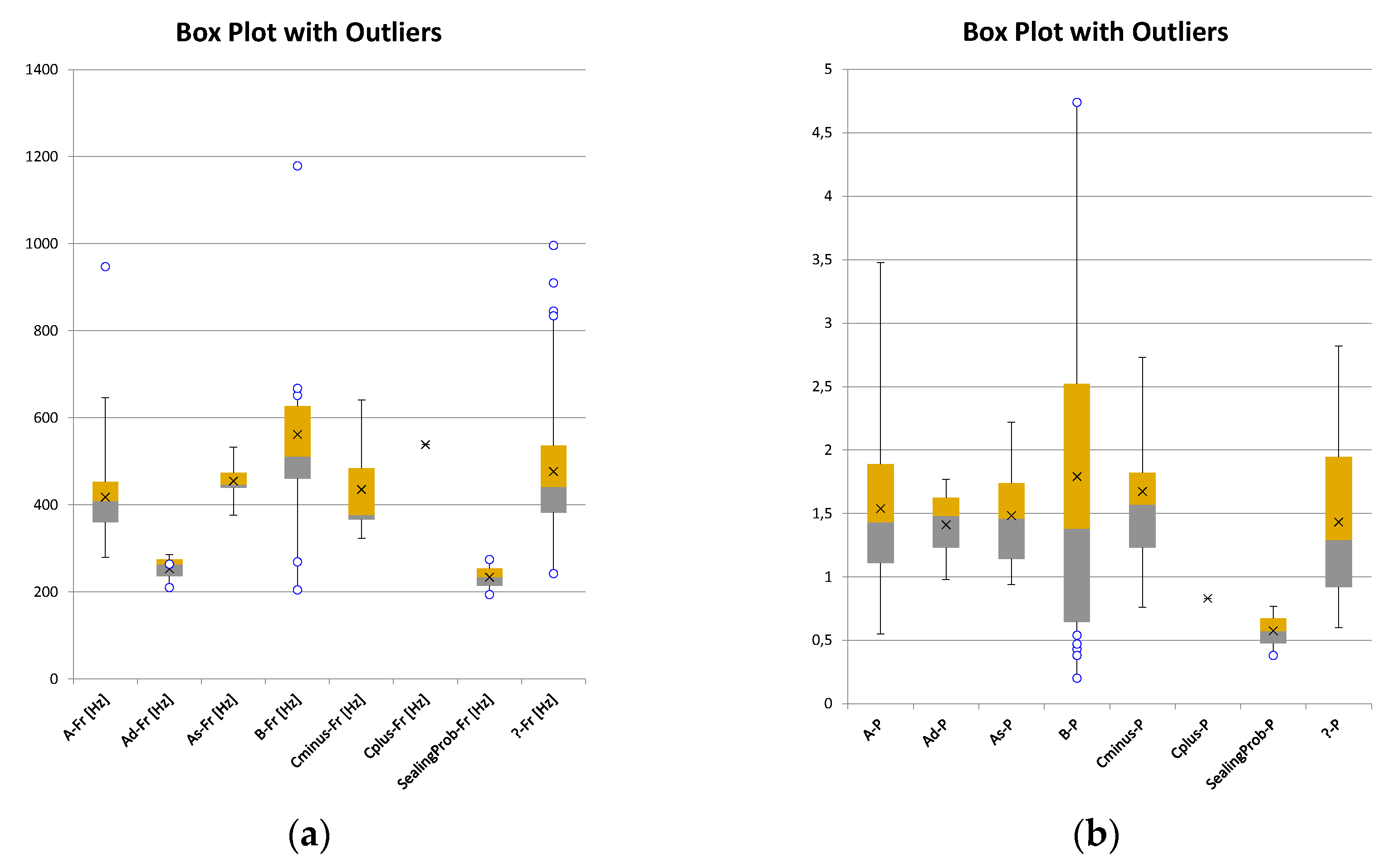
The overall mean of all Medwave measurements showed a resonance frequency fR of 445.73+-136.55 Hz and a peak admittance P of 1.52+-0.69 10^-2 mmho. In the next step, the Medwave results were separated into groups given by the tympanogram types (s. Tab. 1). For type A, we found a mean fR of 417.85+-8.37 Hz and a P of 1.54+-0.06 10^-2 mmho (n = 105). For type As, we found a mean fR of 454.50+-18.04 Hz and a P of 1.48+-0.17 10^-2 mmho (n = 7). For type Ad, we found a mean fR of 253.01+-22.41 Hz and a P of 1.41+-0.23 10^-2 mmho (n = 3). For type B, we found a mean fR of 561.96+-61.07 Hz and a P of 1.79+-0.33 10^-2 mmho (n=18). For type C+, we found a fR of 538.33 and a P of 0.83 (n = 1). For type C-, we found a fR of 435.22+-30.31 Hz and a P of 1.67+-0.19 10^-2 mmho (n=13). For the group with unknown corresponding tympanometry type, we found a mean fR of 476.55+-18.85 Hz and a P of 1.43+-0.08 10^-2 mmho (n = 59). As a boxplot with outliers for each sub-group, the fR data is shown in
Figure 2a, and the P data is shown in
Figure 2b.
3.2. Group Comparisons of the Measured Medwave Parameters
As the groups Ad, C+, and sealing problem were of a small sample size, no comparison to other groups was possible. To compare the larger groups, the Shapiro-Wilk Test was used to evaluate the distribution for normality, as only one group had more than 50 samples.
For the parameter Fr, group As showed a normal distribution, while A, B, and C- were not normally distributed. Therefore, we performed statistical tests for not normally distributed samples. Comparing group A, group As, group B, and group C-, only for group A vs B a significant difference was found regarding the parameter fR (U = 497,5; n1 = 105; n2 = 18; p = 0.001; corrected due to multiple comparisons). All other comparisons of groups showed no significant difference regarding the parameter fR (p > 0.05).
For the parameter P, group A, group As, group B, and group C- were not normally distributed (p < 0.05). Comparing group A, group As, group B, and group C-, no significant difference was found for any group regarding the parameter P (p > 0.05).
3.3. Correlation of Patients’ Age and Measured Medwave Parameters Per Group
In sub-section 3.2., we do not have a normally distributed dataset. Therefore, correlation testing was performed using Spearman’s rank test.
For the parameter fR, a correlation with the patient’s age was found for group A (ϱ (105) = -0.49; p < 0.001; see Fig. 4a) and for the group C- (ϱ (13) = -0.62; p = 0.02; see Fig. 4b). No correlation for the parameter fR with patient’s age was found for group As (ϱ (7) = -0.04; p =0.94) and group B (ϱ (18) = -0.07; p = 0.77).
For the parameter P, a correlation with the patient’s age was found for group A (ϱ (105) = 0.20; p = 0.03). No correlation for the parameter P with patients’ age was found for group As (ϱ (7) = -0.26; p = 0.57), group B (ϱ (18) = 0.35; p = 0.36), and group C- (ϱ (13) =0.11; p = 0.73).
3.4. Paracentesis and a Ventilation Tube in an Adult Subject
In a 44-year-old female patient, the initial subjective right-sided ear symptoms (pressure, pain, and glugging in the middle ear, as well as hearing loss) occurred in December 2024 and worsened till the beginning of 2025. To avoid pain in this subject, we chose Medwave’s PLAI test to analyze the current tympanic status.
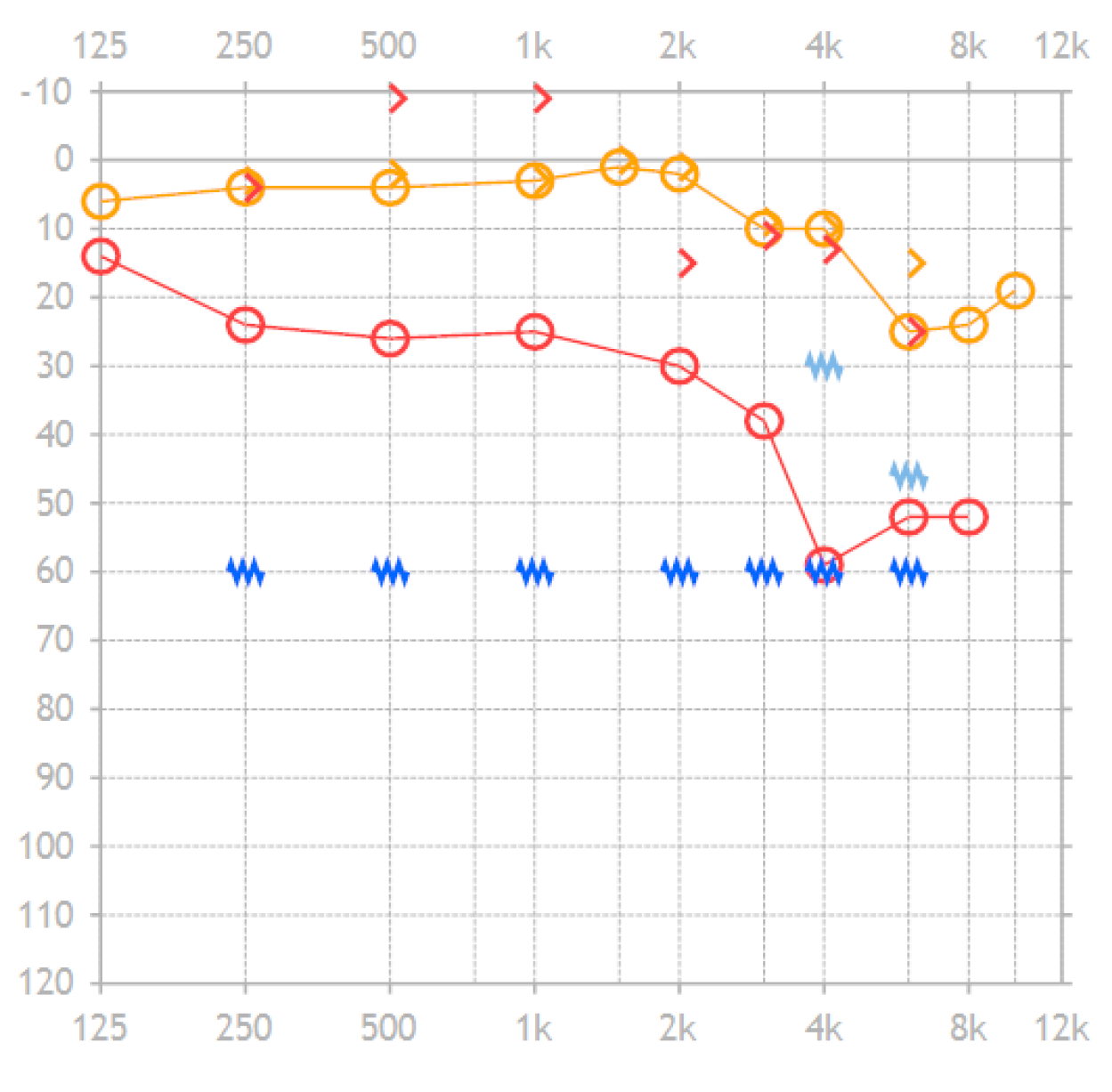
On 8th January 2025, a tympanometry showed type B on the right side and type A on the non-affected left side. Therefore, a paracentesis was performed on the right side. In addition, a tone audiogram was performed showing an air-bone gap of 27.0dB in the range of 500Hz to 2kHz and 31.8dB for the range of 500Hz to 4kHz. The pure tone audiogram worsened by 24.0 dB in the range of 500Hz to 2kHz and by 30.3dB in the range of 500Hz to 4kHz. The bone conduction showed an improvement of 1.5dB.
Figure 3.
Tone audiogram of the reported individual case’s affected right ear before suffering from the reported symptoms (orange symbols) and during the symptoms but before the two surgeries (red symbols). Circles are for air conduction, while arrows are for bone conduction. (The copyright of this figure belongs to INNOFORCE Est.).
Figure 3.
Tone audiogram of the reported individual case’s affected right ear before suffering from the reported symptoms (orange symbols) and during the symptoms but before the two surgeries (red symbols). Circles are for air conduction, while arrows are for bone conduction. (The copyright of this figure belongs to INNOFORCE Est.).
On 10th January 2025, the first surgery took place. The ear inspection showed cerumen in the outer ear canal, which was removed, and the intact eardrum showed inflammation and was less opaque. The paracentesis was performed under local anesthesia in the anterior lower quadrant. The serotympanon was suctioned. The paracentesis didn’t solve the patient’s symptoms, and the tympanometry still showed type B on the right side and type A on the non-affected left side. Another surgery was performed. Therefore, after the re-paracentesis and suction of a serotympanon, a 1.25 mm titanium ear tube was inserted.
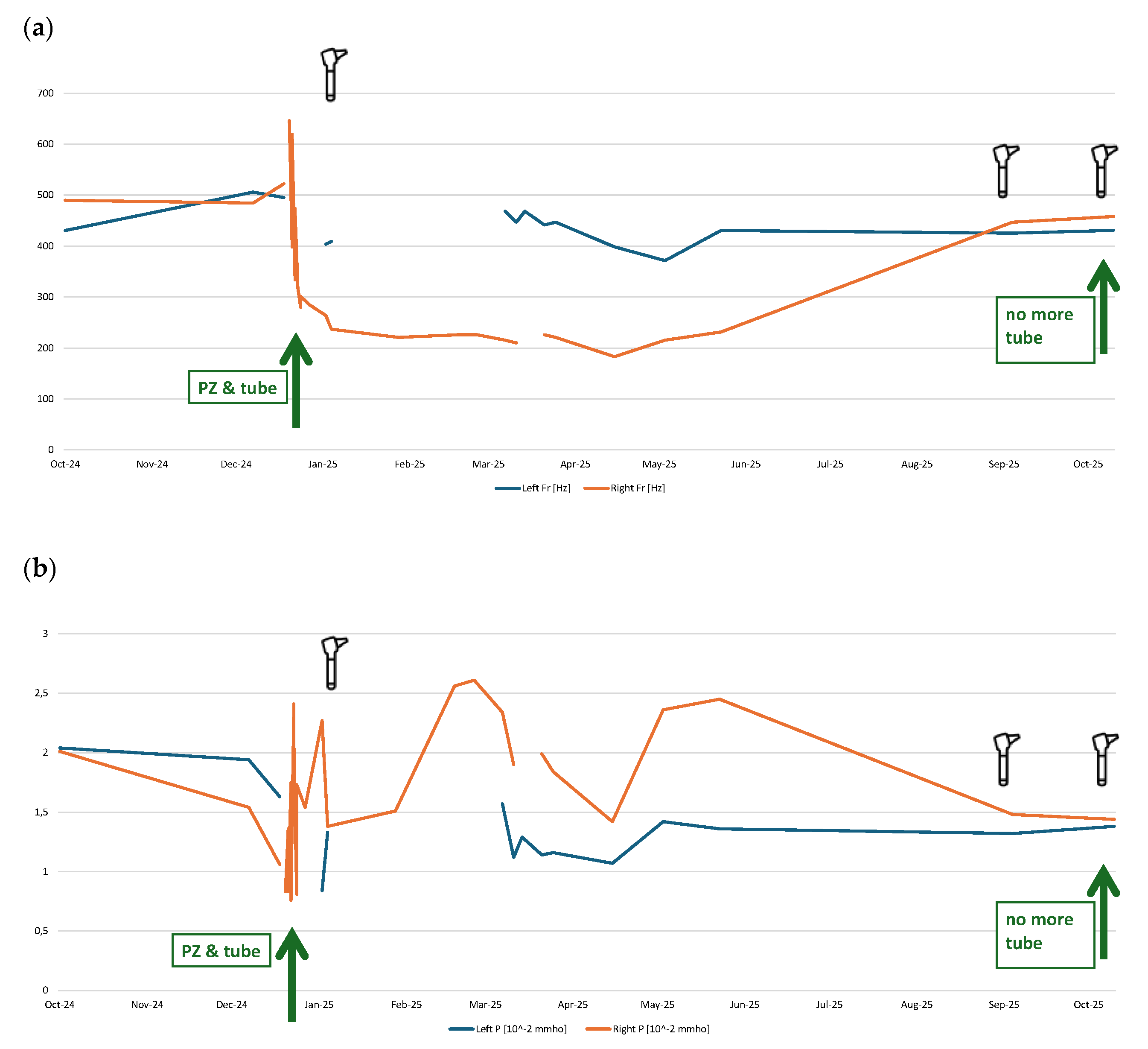
Several ‘pressureless’ measurements could be performed using the Medwave device before, on the day of, and after the surgeries. Parallelly, tympanometry was performed regularly, showing type B for the affected right side. The measured values of fR and P can be found in
Figure 4a and 4b, respectively, showing the patient's progression over time.
The resonance frequency fR (
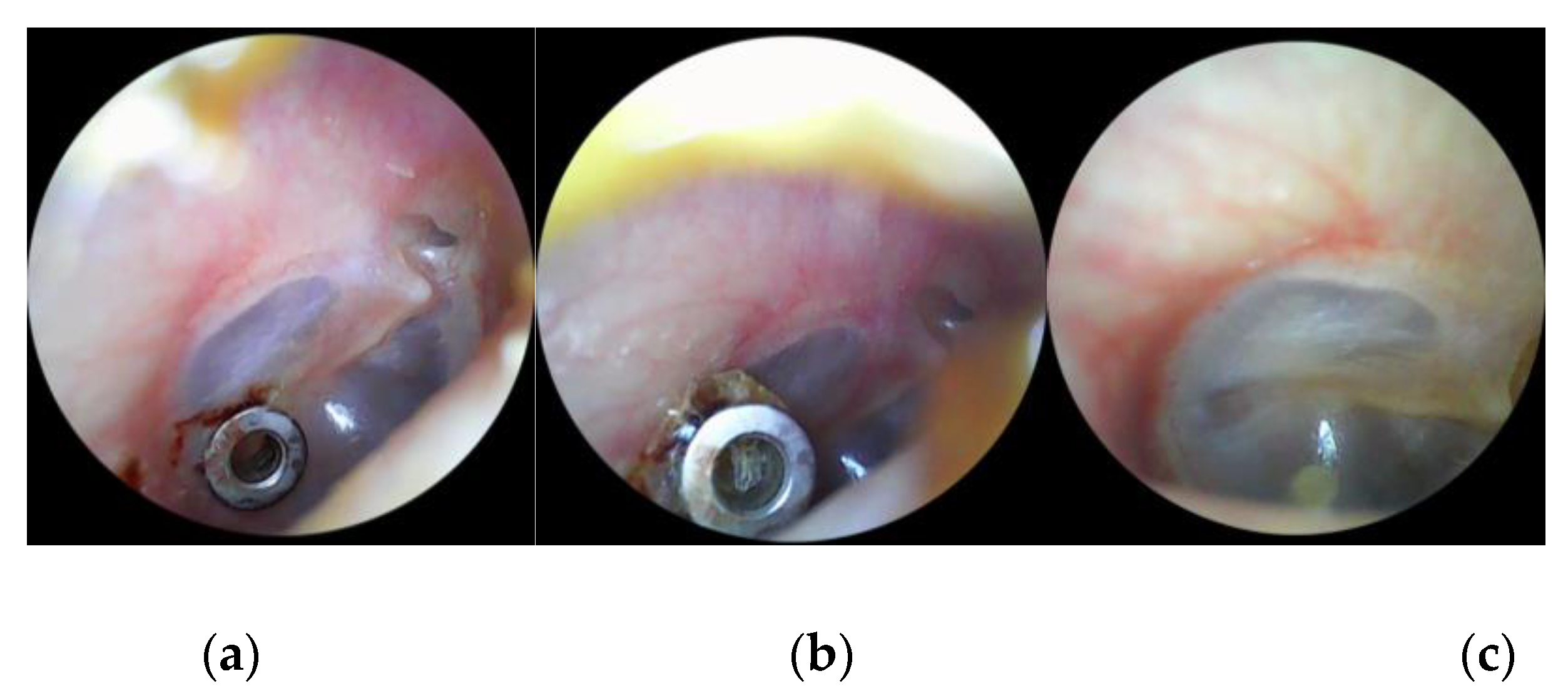
Figure 4a) of the indicates a clear difference between the right and left ear. On the right ear, it decreased significantly from approximately 500 Hz to around 250 Hz. This effect lasted for months (until May-25) and rose back to the values of the contralateral ear in Sep-25. Interestingly, the tube was not completely rejected from the tympanic eardrum at that time. The eardrum seemed closed on the images from the patient’s otoscopic camera integrated in a consumer ear cleaner (Bebird EarSight M9 S, app version 5.3.90, Heifeng Zhizao (Shenzhen) Technology Co., Ltd., Shenzhen, Guangdong, China). Finally, the tube was removed by the patient herself with a slight touch of the tube. The otoscopic images are shown in
Figure 5.
4. Discussion
The parameter fR of the Medwave-PLAI test distinguishes ears with type A vs. type B tympanometry results. All other comparisons were not statistically different between types of tympanometry results, nor for parameter fR [Hz], nor for parameter P [10^-2 mmho]. Based on this finding, a differentiation between normal and non-movable eardrum seems possible. This offers the option to use the Medwave device for detecting liquid or infection (with or without effusion) in the middle ear, or a perforation of the eardrum (with or without tube).
The correlations between the patients’ age and both the parameter fR as well as the parameter P for the group of tympanometry result type A are in alignment with the offered age-related normative values for Medwave’s PLAI test. Whether the manufacturer’s currently used age-related normative values need to be optimized cannot be evaluated by our study’s results and therefore needs to be investigated in further studies, as well as considering such grouping also for different-aged patients when using tympanometry. In general, this approach to get normal values for multiple groups of different ages is not only interesting to re-evaluate in PLAI testing but could also be of interest to investigate in tympanometry, where only children under one year of age get an (additional) tympanometry using a 1000Hz probe tone [
26].
We didn’t experience any problems using the Medwave device for measuring, nor in exporting the reports to our clinical assistance sub via flash drive as a PDF file. Especially, the testing time was very short compared to tympanometry, which eases measurements in children. In addition, as Medwave solely uses an acoustic stimulation without any pressure, like in tympanometry, it avoids possible pain in patients or could even enable a measurement where tympanometry is not possible, like in patients shortly after certain ear surgeries.
The case of the patient with paracentesis and later on paracentesis again plus insertion of a tube, highlights the sensitivity of Medwave’s test results in the parameter fR and its correlation to the visual results from otoscopy and the measurement results from clinical routine measurement (the tympanometry). The results over time highlight the possibilities Medwave may offer in such or similar cases of patients. Further studies using a prospective approach should be performed to verify this case’s results, supported by the group comparison showing significant differences between tympanometry type A vs. tympanometry type B.
A measurement using the PLAI technique is possible when tympanometry is challenging to perform or a measurement is not possible at all. This is especially helpful in children. It reduces or even avoids pain, as it doesn’t need a sealed ear canal for PLAI, where sealing is obligatory in tympanometry. In contrast to these positive aspects, departments of otolaryngology must keep in mind that PLAI is not a replacement for tympanometry. Therefore, they will face additional costs for hardware and device maintenance. Further research will show whether PLAI can replace tympanometry or if additional functionality can be added to PALI devices to make its purchase more profitable in clinical practice.
The main limitation of the study is the small groups for tympanometry types As, Ad, and C+. Further studies are needed to investigate the tympanometry types in depth using a prospective approach, as this retrospective study showed how rare these results are, especially in comparison to types A and B. This study was performed using an anonymous retrospective and monocentric approach. Due to this anonymous approach, possible data errors could not be rechecked. Due to the retrospective design, the study’s results are more susceptible to bias and confounding variables in comparison to a prospective study’s results. By its monocentric approach, the study could be biased by a few people performing the measurements and documentation in comparison to using a multicentric study design.
5. Conclusions
This study showed that using the Medwave device to perform a pressureless impedance measurement allows differentiation between tympanometry type A and tympanometry type B in clinical patients using the parameter fR (resonance frequency of the acoustic response recorded by the device’s microphone). Whether a differentiation between other tympanogram types may also be possible could not be finally found out due to the smaller groups of the tympanogram types. Type Ad and the group with sealing problems in tympanogram seem to have the highest probability for a possible differentiation to type A based on our limited data in the groups Ad and sealing problems. Age influences the parameters fR as well as P in group A. Influences of age in other groups were not found and need re-evaluation in future prospective studies. In summary, testing with the Medwave device shows promising results and was easy, quick, and more often performable in patients compared to tympanometry, being the clinical gold standard in middle ear analysis. Further measurements based on this pressureless technique, like stapedial reflex testing, may be interesting to investigate in the future.
Author Contributions
Conceptualization, M.N. and D.P.; methodology, M.N. and D.P.; validation, M.N. and D.P.; formal analysis, M.N. and D.P.; investigation, M.N. and D.P.; resources, D.P.; data curation, D.P.; writing—original draft preparation, D.P.; writing—review and editing, M.N., D.P., P.Z., and C.M.; visualization, D.P.; supervision, D.P.; project administration, D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The study was conducted anonymously and retrospectively, in accordance with the current statement of the Ethics Committee (EC) of LMU Munich, and was approved by the Ethics Committee of LMU Munich (protocol code 24-0923).
Informed Consent Statement
As the study was performed anonymously and retrospectively, according to the current statement of the Ethics Committee (EC) of LMU Munich, researchers do not require informed consent from subjects involved in the study. Written informed consent has been obtained from the individual reported patient’s case to publish this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Acknowledgments
We thank Fritz Mack (Mack Medizintechnik GmbH, Pfaffenhofen a.d.I., Germany) and Neuranix Srl (Gardigiano, VE, Italy) for lending us two Medwave devices for clinical testing at no cost.
Conflicts of Interest
D.P. received travel support from Cochlear Ltd. (Australia), INNOFORCE Est. (Liechtenstein), and MED-EL GmbH (Austria), free hardware loan from HZ Haase & Zeisberg (Germany), inomed Medizintechnik GmbH (Germany), Mack Medizintechnik GmbH (Germany), and PATH MEDICAL GmbH, research support from MED-EL GmbH (Austria), and publication discount from Georg Thieme Verlag KG, and is part of the audiological advisory board “MAUWIB” for MED-EL GmbH (Austria). M.N. received travel support from INNOFORCE Est. (Liechtenstein), and MED-EL GmbH (Austria). P.Z. some methodological consultancies for Neuranix Srl in 2023. C.M. received travel support and research support from MED-EL GmbH (Austria).
Abbreviations
The following abbreviations are used in this manuscript:
fR
MEMS
p
P
PLAI |
value of the frequency at which the maximum value (P) of the admittance curve (module) occurs
micro-electro-mechanical systems
pressure
peak admittance value (module)
Pressure Less Acoustic Immittance |
v
Ve |
Velocity
equivalent volume of the ear canal |
Y
Z |
complex acoustic admittance
complex acoustic impedance |
References
- Bluestone, C.D.; Cantekin, E.I. Design Factors in the Characterization and Identification of Otitis Media and Certain Related Conditions. Ann Otol Rhinol Laryngol Suppl 1979, 88, 13–28. [Google Scholar] [CrossRef]
- Shahnaz, N.; AlMakadma, H.; Sanford, C.A. The Rise and Fall of Aural Acoustic Immittance Assessment Tools. Seminars in Hearing 2023, 44, 005–016. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Dutta, N. Wideband Tympanometry. Annals of Otology and Neurotology 2019, 01, 126–132. [Google Scholar] [CrossRef]
- Herkal, K.; Ramasamy, K.; Saxena, S.K.; Ganesan, S.; Alexander, A. Hearing Loss in Tympanic Membrane Perforations: An Analytic Study. International Journal of Otorhinolaryngology and Head and Neck Surgery 2018, 4, 1233–1239. [Google Scholar] [CrossRef]
- Surr, R.K.; Schuchman, G.I. Measurement of the Acoustic Reflex Without a Pressure Seal. Archives of Otolaryngology 1976, 102, 160–161. [Google Scholar] [CrossRef]
- Migirov, L.; Tal, S.; Eyal, A.; Kronenberg, J. MRI, Not CT, to Rule out Recurrent Cholesteatoma and Avoid Unnecessary Second-Look Mastoidectomy. Isr Med Assoc J 2009, 11, 144–146. [Google Scholar]
- Williams, B.; Taylor, B.A.; Clifton, N.; Bance, M. Balloon Dilation of the Eustachian Tube: A Tympanometric Outcomes Analysis. Journal of Otolaryngology - Head & Neck Surgery 2016, 45, 13. [Google Scholar] [CrossRef]
- Zheng, Y.; Dong, X.; Zhao, Y.; Lu, D.; Lei, L.; Ren, J.; Wang, J.; Liu, S. Clinical Analysis of Audiology in Two Hundred Seventy-Seven Patients with Myringosclerosis. Clinical Otolaryngology 2019, 44, 465–470. [Google Scholar] [CrossRef]
- Matthews, T.J.; Adamson, R. Optical Coherence Tomography: Current and Future Clinical Applications in Otology. Current Opinion in Otolaryngology & Head and Neck Surgery 2020, 28, 296. [Google Scholar] [CrossRef]
- Wang, J.; Couvreur, F.; Farrell, J.D.; Ghedia, R.; Shoman, N.; Morris, D.P.; Adamson, R.B.A. Fusion of Middle Ear Optical Coherence Tomography and Computed Tomography in Three Ears 2024, 2024.09.23.24314125.
- Crowson, M.G.; Hartnick, C.J.; Diercks, G.R.; Gallagher, T.Q.; Fracchia, M.S.; Setlur, J.; Cohen, M.S. Machine Learning for Accurate Intraoperative Pediatric Middle Ear Effusion Diagnosis. Pediatrics 2021, 147, e2020034546. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Pandey, R.; Valdez, T.A. Label-Free Optical Technologies for Middle-Ear Diseases. Bioengineering 2024, 11, 104. [Google Scholar] [CrossRef] [PubMed]
- Marom, T.; Kraus, O.; Habashi, N.; Tamir, S.O. Emerging Technologies for the Diagnosis of Otitis Media. Otolaryngology–Head and Neck Surgery 2019, 160, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Kei, J.; Aithal, V.; Aithal, S.; Anderson, S.; Wright, D. Predicting the Characteristics of Wideband Absorbance in Ears with Middle-Ear Pathologies. The Journal of the Acoustical Society of America 2016, 140, 3263. [Google Scholar] [CrossRef]
- Biswas, A.; Dutta, N. Wideband Tympanometry. Annals of Otology and Neurotology 2018, 01, 126–132. [Google Scholar] [CrossRef]
- Anbari, M.; Zhumabaeva, S.; Beishenova, M.; Fischer, D.; Sulaimanov, S.; Just, T. Comparison of Conventional Single-Frequency Tympanometry with Pressure-Less Acoustic Immittance Measurements of Pathological and Normal Middle Ears. Online Journal of Otolaryngology and Rhinology 2024, 7, 1–11. [Google Scholar] [CrossRef]
- Zoth, P.; Fischer, D.; Anbari, M.; Just, T. ‘Druckfreie’ akustische Admittanzmessung bei Patienten mit chronischer Tubenbelüftungsstörung 2025.
- Zoth, P.; Mattente, M. 274 - Innovation in Diagnostics - Validation Results. Presented at the HEAL2024, 2024.
- Tympanometrie trifft auf Audiometrie | GSI 39TM. Available online: https://www.grason-stadler.com/de/products/tympanometers/gsi-39 (accessed on 18 June 2025).
- Tympanometer eTymp | Merz Medizintechnik. Available online: https://www.merz-medizintechnik.de/hno-diagnostik/tympanometrie/etymp/ (accessed on 18 June 2025).
- Bright, T.; Youngs, R.; Faal, Y.; Hydara, A.; Yip, J.L.Y.; Mactaggart, I.; Polack, S. Evaluating the Inclusion of Tympanometry in Population-Based Surveys of Hearing Loss. The Journal of Laryngology & Otology 2022, 136, 839–847. [Google Scholar] [CrossRef]
- Onusko, E. Tympanometry. afp 2004, 70, 1713–1720. [Google Scholar]
- Impedanzmessung - DIATEC. Available online: https://www.diatec-diagnostics.ch/knowledge-base/category/impedance-measurement (accessed on 18 June 2025).
- Son, E.J.; Park, Y.A.; Kim, J.H.; Hong, S.A.; Lim, H.Y.; Choi, J.Y.; Lee, W.-S. Classification of Trace Patterns of 226- and 1000-Hz Tympanometry in Healthy Neonates. Auris Nasus Larynx 2012, 39, 455–460. [Google Scholar] [CrossRef]
- de Resende, L.M.; dos Santos Ferreira, J.; da Silva Carvalho, S.A.; Oliveira, I.S.; Bassi, I.B. Tympanometry with 226 and 1000 Hertz Tone Probes in Infants. Brazilian Journal of Otorhinolaryngology 2012, 78, 95–102. [Google Scholar] [CrossRef]
- Gellrich, D.; Eder, K.; Echternach, M.; Gröger, M.; Huber, P. A Comparison of 226- and 1000-Hz Probe Tone Tympanometry With Myringotomy Findings in Infants. American Journal of Audiology 2024, 1–11. [Google Scholar] [CrossRef]
- HEINE BETA 200 LED F.O. Otoskop - HEINE Optotechnik. Available online: https://www.heine.com/de/produkte/allgemeinmedizin-und-hno-instrumente/otoskope/detail/33121-otoscope-heine-beta-200-led-fo (accessed on 18 June 2025).
- ZEISS OPMI pico | ZEISS Medical Technology. Available online: https://www.zeiss.com/meditec/de/produkte/operationsmikroskope/opmi-pico-s100.html (accessed on 18 June 2025).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).