Submitted:
25 November 2025
Posted:
26 November 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Data Source and Management
2.3. Study Outcomes
2.4. Ethical Approval
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
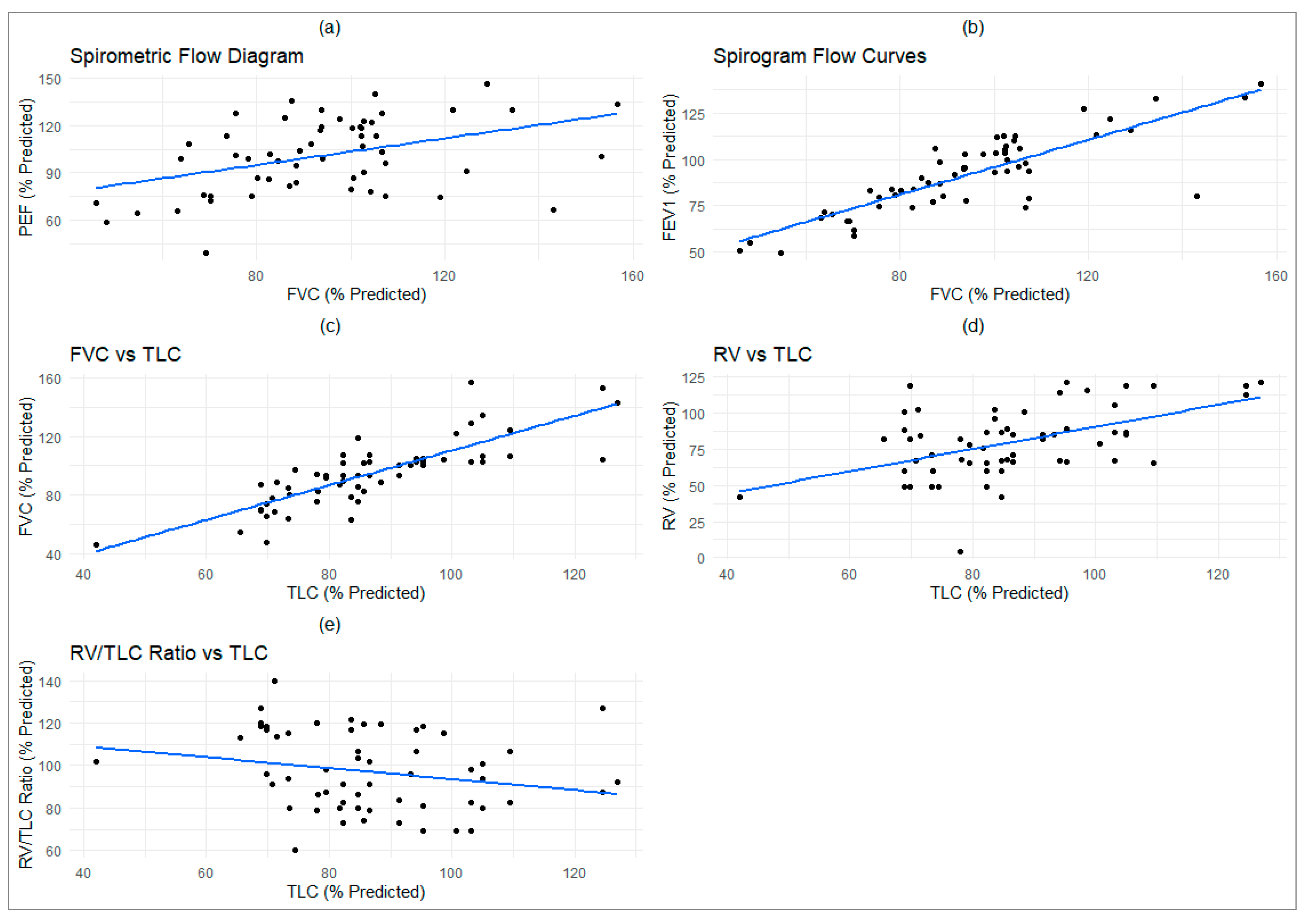
3.2. Pulmonary Function Test
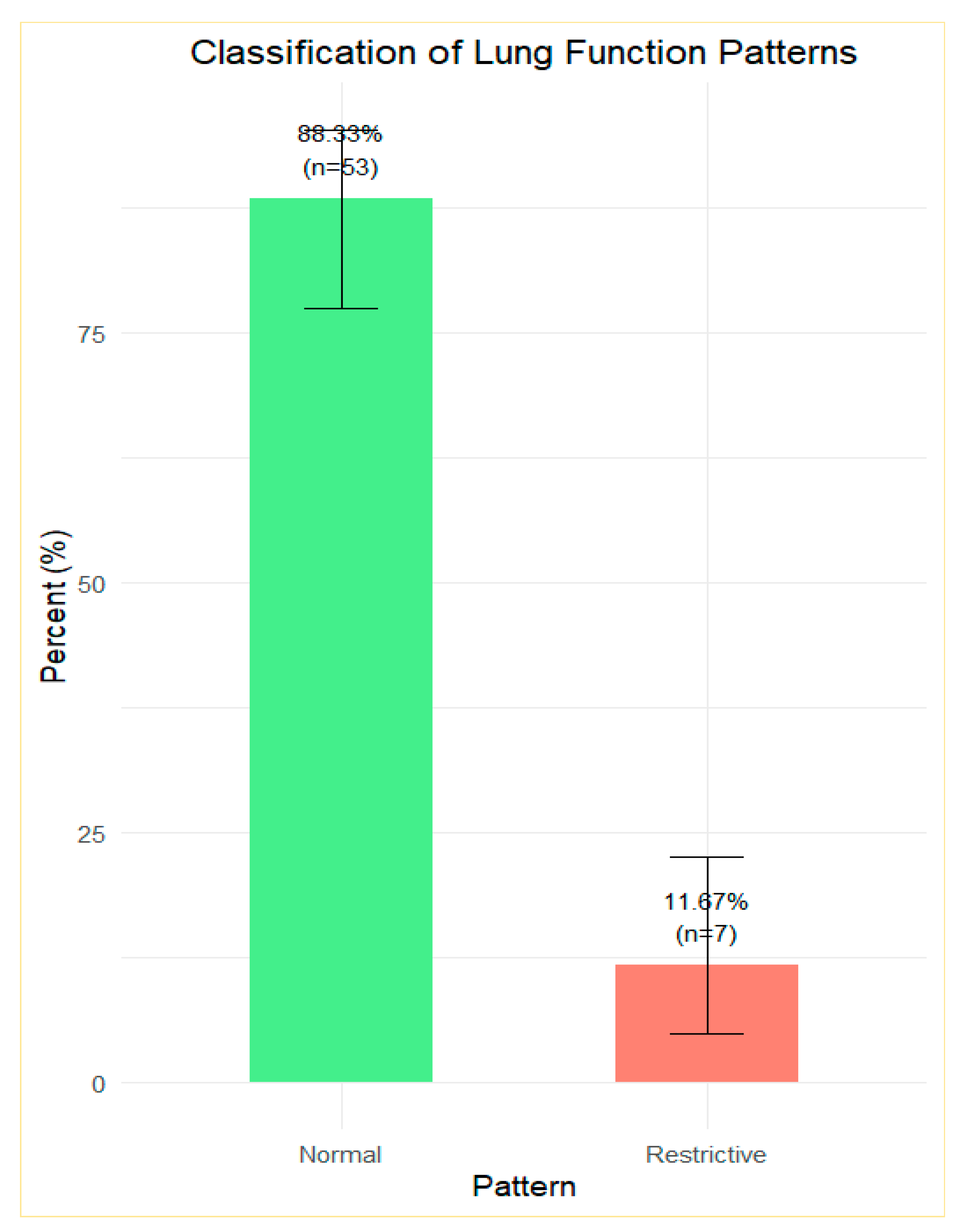
3.3. Lung Function Patterns
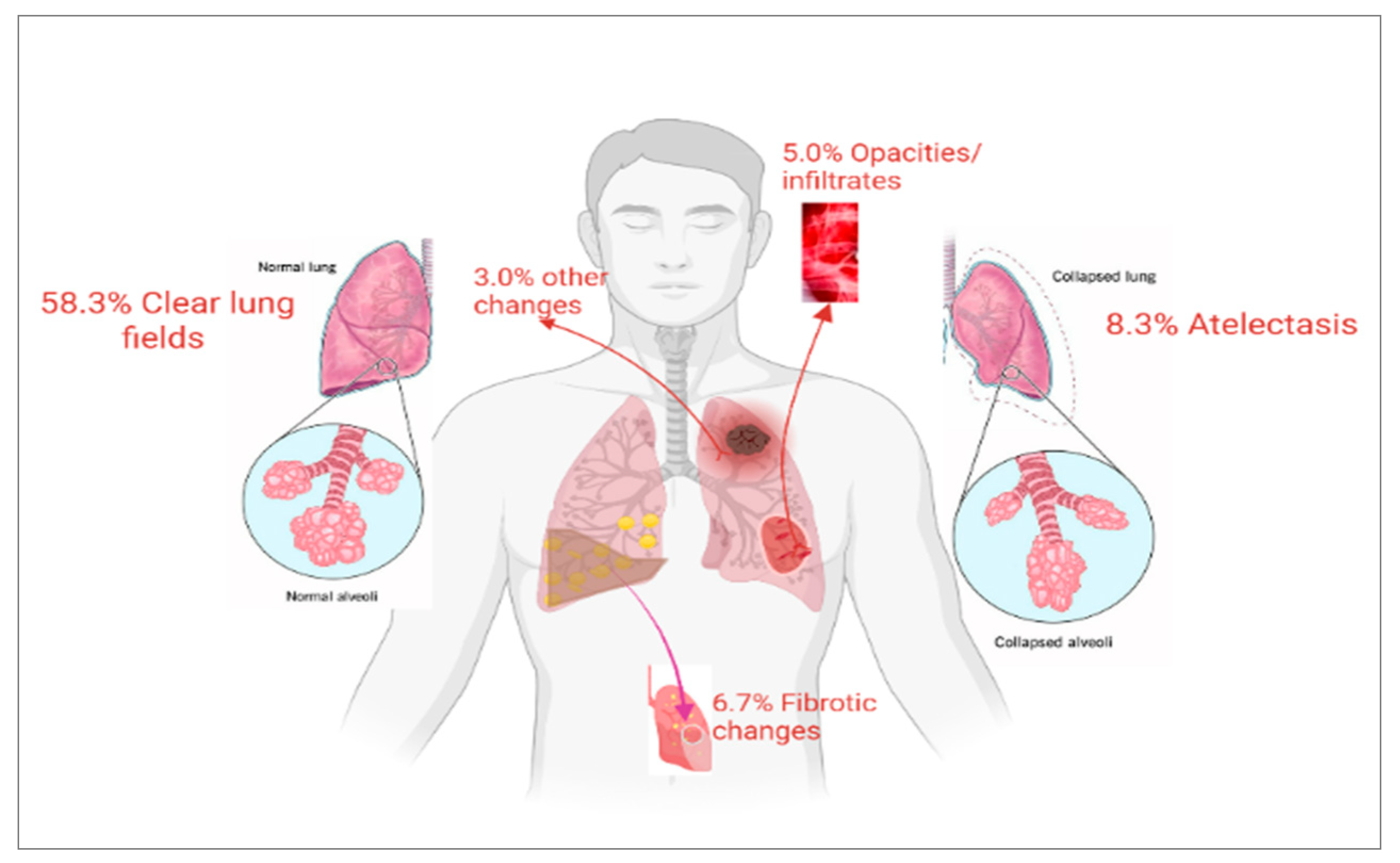
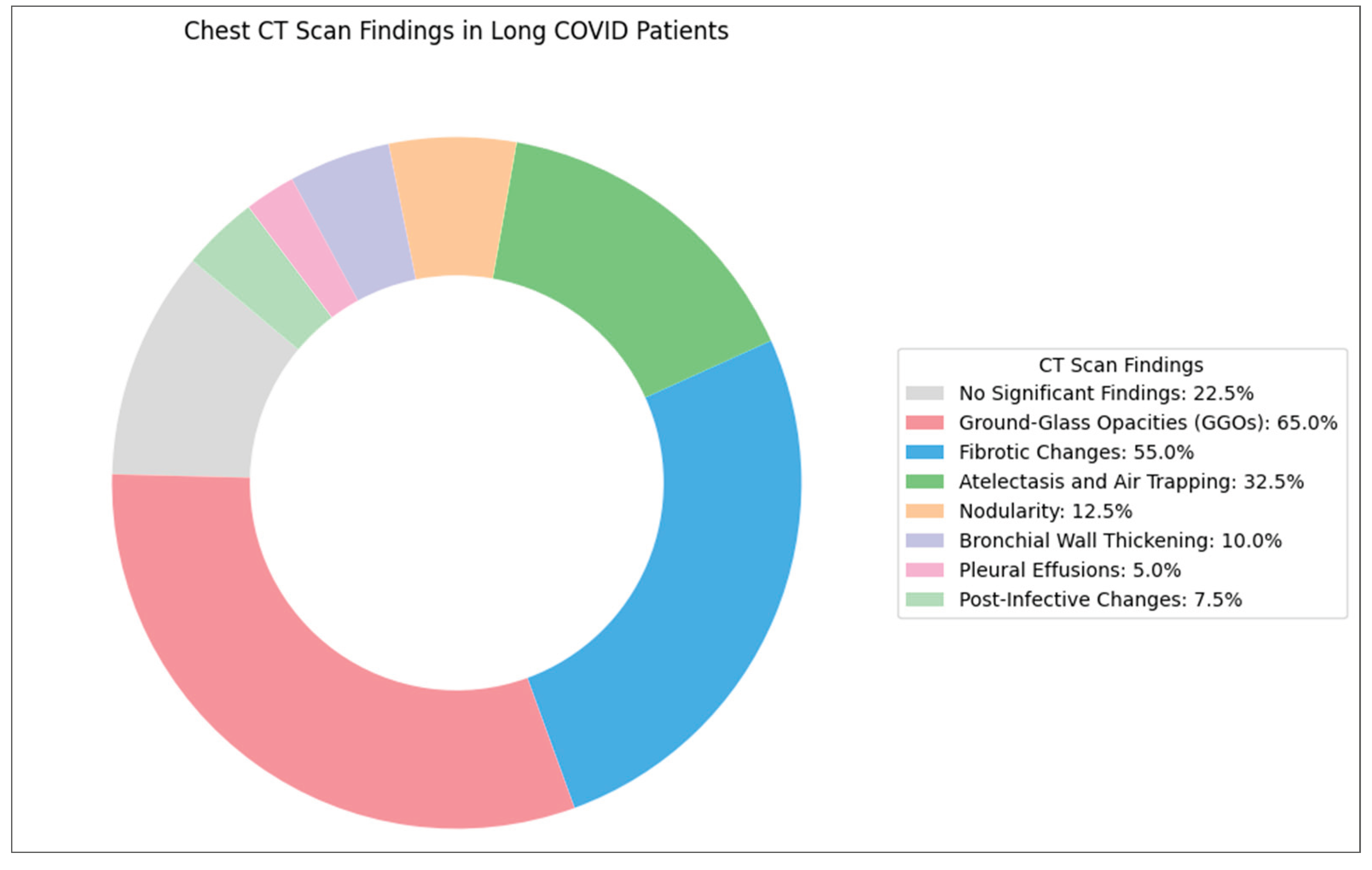
3.4. Radiographic and Tomographic Findings
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 6MWT | Six-Minute Walk Test |
| ARDS | Acute Respiratory Distress Syndrome |
| BMI | Body Mass Index |
| COVID-19 | Coronavirus Disease 2019 |
| CXR | Chest X-Ray |
| CT | Computed Tomography |
| DLCO | Diffusing Capacity of the Lungs for Carbon Monoxide |
| FVC | Forced Vital Capacity |
| FEV₁ | Forced Expiratory Volume in One Second |
| FRC | Functional Residual Capacity |
| GOLD | Global Initiative for Chronic Obstructive Lung Disease |
| HRCT | High-Resolution Computed Tomography |
| ICU | Intensive Care Unit |
| ILD | Interstitial Lung Disease |
| LC | Long COVID |
| LTOT | Long-Term Oxygen Therapy |
| MRI | Magnetic Resonance Imaging |
| mMRC | Modified Medical Research Council Dyspnea Scale |
| PFT | Pulmonary Function Test |
| RV | Residual Volume |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| TLC | Total Lung Capacity |
| V/Q | Ventilation/Perfusion |
| VATS | Video-Assisted Thoracoscopic Surgery |
| WHO | World Health Organisation |
| Xe-MRI | Xenon-129 Magnetic Resonance Imaging |
References
- Yong, S. Long COVID or Post-COVID-19 Syndrome: Putative Pathophysiology, Risk Factors, and Treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Giuliano, M.; Tiple, D.; Agostoni, P.; et al. Italian Good Practice Recommendations on Management of Persons with Long-COVID. Front. Public Health 2023, 11, 1122141. [Google Scholar] [CrossRef]
- Torres, G. Exercise Is the Most Important Medicine for COVID-19. Curr. Sports Med. Rep. 2023, 22, 284–289. [Google Scholar] [CrossRef]
- Dahal, A.; Pohl, G.; Laxmi, R.; et al. Long COVID-19 Effects (Chronic COVID-19 Syndrome) in Nepalese Cohort Recovered from SARS-CoV-2 Infection. J. Curr. Med. Res. Opin. 2023, 6, 1884–1893. [Google Scholar] [CrossRef]
- Sideratou, C. Persisting Shadows: Unravelling the Impact of Long COVID-19 on Respiratory, Cardiovascular, and Nervous Systems. Infect. Dis. Rep. 2023, 15, 806–830. [Google Scholar] [CrossRef]
- Somalwar, S. Long COVID and Perimenopause. J. S. Asian Feder. Obstet. Gynaecol. 2024, 16, 174–176. [Google Scholar] [CrossRef]
- Michalski, J.E.; Kurche, J.S.; Schwartz, D.A.; et al. From ARDS to Pulmonary Fibrosis: The Next Phase of the COVID-19 Pandemic? Transl. Res. 2022, 241, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Peng, F.; Zhou, Y.; et al. Pulmonary Fibrosis: A Short- or Long-Term Sequela of Severe COVID-19? Chin. Med. J. Pulm. Crit. Care Med. 2023, 1, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, L.A.; Costa, I.B.S.; Rizk, S.I.; et al. Intensive Care Management of Patients with COVID-19: A Practical Approach. Ann. Intensive Care 2021, 11, 36. [Google Scholar] [CrossRef] [PubMed]
- Myall, K.; Mukherjee, B.; West, A.; et al. How COVID-19 Interacts with Interstitial Lung Disease. Breathe (Sheff.) 2022, 18, 210158. [Google Scholar] [CrossRef]
- Mart, M.F.; Ware, L.B. The Long-Lasting Effects of the Acute Respiratory Distress Syndrome. Expert Rev. Respir. Med. 2020, 14, 577–586. [Google Scholar] [CrossRef]
- Huijts, T.; Witvliet, M.; Balaj, M.; et al. Assessing the Long-Term Health Impact of COVID-19: The Importance of Using Self-Reported Health Measures. Scand. J. Public Health 2023, 51, 645–647. [Google Scholar] [CrossRef]
- Karmakar, S.; Rungta, R.; Singh, K.; et al. Post-COVID-19 Pulmonary Fibrosis: Report of Two Cases. EMJ Respir. 2021. [CrossRef]
- Sweis, J. From Acute Infection to Prolonged Health Consequences: Understanding Health Disparities and Economic Implications in Long COVID Worldwide. Int. J. Environ. Res. Public Health 2024, 21, 325. [Google Scholar] [CrossRef] [PubMed]
- Wheibe, E. The Multisystem Effects of Long COVID Syndrome and Potential Benefits of Massage Therapy in Long COVID Care. Int. J. Ther. Massage Bodywork Res. Educ. Pract. 2024, 17, 19–42. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.; Liu, S. Proposed Subtypes of Post-COVID-19 Syndrome (or Long-COVID) and Their Respective Potential Therapies. Rev. Med. Virol. 2021, 32. [Google Scholar] [CrossRef]
- Zhao, Y.; Shang, Y.; Song, W.; et al. Follow-Up Study of the Pulmonary Function and Related Physiological Characteristics of COVID-19 Survivors Three Months After Recovery. EClinicalMedicine 2020, 25, 100463. [Google Scholar] [CrossRef]
- Biswas, S. Pulmonary Features of Long COVID-19: Where Are We Now? J. Clin. Oncol. Rep. 2023, 2, 1–5. [Google Scholar] [CrossRef]
- Montani, D.; Savale, L.; Noël, N.; et al. Post-Acute COVID-19 Syndrome. Eur. Respir. Rev. 2022, 31, 210185. [Google Scholar] [CrossRef]
- Gerayeli, F.; Park, H.Y.; Milne, S.; et al. Single-Cell Sequencing Reveals Cellular Landscape Alterations in the Airway Mucosa of Patients with Pulmonary Long COVID. Eur. Respir. J. 2024, 64, 2301947. [Google Scholar] [CrossRef]
- Ponce, M.C.; Sankari, A.; Sharma, S. Pulmonary Function Tests. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Funke-Chambour, M.; Bridevaux, P.-O.; Clarenbach, C.F.; et al. Swiss Recommendations for the Follow-Up and Treatment of Pulmonary Long COVID. Respiration 2021, 100, 826–841. [Google Scholar] [CrossRef]
- Suppini, N.; Fira-Mladinescu, O.; Traila, D.; et al. Longitudinal Analysis of Pulmonary Function Impairment One Year Post-COVID-19: A Single-Center Study. J. Pers. Med. 2023, 13, 1190. [Google Scholar] [CrossRef] [PubMed]
- Aritonang, M.E.; Pandia, P.; Pradana, A.; et al. Factors Associated with Small Airway Obstruction in COVID-19 Survivors: A Cross-Sectional Study Among Health-Care Providers. Narra J. 2023, 3, e437. [Google Scholar] [CrossRef] [PubMed]
- Teles, G.B.D.S.; Fonseca, E.K.U.N.; Capobianco, J.; et al. Correlation Between Chest Computed Tomography Findings and Pulmonary Function Test Results in the Post-Recovery Phase of COVID-19. Einstein (São Paulo) 2023, 21, eAO0288. [Google Scholar] [CrossRef]
- Alrajhi, N.N. Post-COVID-19 Pulmonary Fibrosis: An Ongoing Concern. Ann. Thorac. Med. 2023, 18, 173–181. [Google Scholar] [CrossRef] [PubMed]
- [Entry removed — "Vxccc" appears to be an invalid placeholder].
- Thomas, M.; Price, O.J.; Hull, J.H. Pulmonary Function and COVID-19. Curr. Opin. Physiol. 2021, 21, 29–35. [Google Scholar] [CrossRef]
- Laveneziana, P.; Straus, C.; Meiners, S. How and to What Extent Immunological Responses to SARS-CoV-2 Shape Pulmonary Function in COVID-19 Patients. Front. Physiol. 2021, 12, 628288. [Google Scholar] [CrossRef]
- Vontetsianos, A.; Chynkiamis, N.; Anagnostopoulou, C.; et al. Small Airways Dysfunction and Lung Hyperinflation in Long COVID-19 Patients as Potential Mechanisms of Persistent Dyspnoea. Adv. Respir. Med. 2024, 92, 329–337. [Google Scholar] [CrossRef]
- Cimmino, G.; D'Elia, S.; Morello, M.; et al. Cardio-Pulmonary Features of Long COVID: From Molecular and Histopathological Characteristics to Clinical Implications. Int. J. Mol. Sci. 2025, 26, 7668. [Google Scholar] [CrossRef]
- Balkissoon, R. Journal Club: The Intersection of Racial/Ethnic Disparities in Coronavirus Disease 2019 and COPD. Chronic Obstr. Pulm. Dis. 2021, 8, 292–302. [Google Scholar] [CrossRef]
- Poerio, A.; Carlicchi, E.; Lotrecchiano, L.; et al. Evolution of COVID-19 Pulmonary Fibrosis-Like Residual Changes over Time: Longitudinal Chest CT up to 9 Months After Disease Onset. SN Compr. Clin. Med. 2022, 4, 57. [Google Scholar] [CrossRef]
- Liu, W.; Feng, Q.; Yuan, X.; et al. Diagnostic Value of Lung Function Tests in Long COVID: Analysis of Positive Bronchial Provocation Test Outcomes. Front. Med. 2025, 11, 1512658. [Google Scholar] [CrossRef]
- Bretas, D.C.; Leite, A.S.; Mancuzo, E.V.; et al. Lung Function Six Months After Severe COVID-19: Does Time, in Fact, Heal All Wounds? Braz. J. Infect. Dis. 2022, 26, 102352. [Google Scholar] [CrossRef]
- Salvi, S.S.; Ghorpade, D.; Dhoori, S.; et al. Role of Antifibrotic Drugs in the Management of Post-COVID-19 Interstitial Lung Disease: A Review of Literature and Expert Working Group Report. Lung India 2022, 39, 177–186. [Google Scholar] [CrossRef]
- Durak, G.; Akin, K.; Cetin, O.; et al. Radiologic and Clinical Correlates of Long-Term Post-COVID-19 Pulmonary Sequelae. J. Clin. Med. 2025, 14, 4874. [Google Scholar] [CrossRef] [PubMed]
- Treasa, S. Post-COVID Pulmonary Fibrosis: Pathophysiological Mechanisms, Diagnostic Tools, and Emerging Therapies. J. Pulmonol. Respir. Res. 2025, 9, 009–013. [Google Scholar] [CrossRef]
- Suppini, N.; Fira-Mladinescu, O.; Traila, D.; et al. Longitudinal Analysis of Pulmonary Function Impairment One Year Post-COVID-19: A Single-Centre Study. J. Pers. Med. 2023, 13, 1190. [Google Scholar] [CrossRef] [PubMed]
- Patton, M.; Benson, D.; Robison, S.; et al. Characteristics and Determinants of Pulmonary Long COVID. JCI Insight 2024, 9. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.; Kanne, J.; Ashizawa, K.; et al. Best Practice: International Multisociety Consensus Statement for Post-COVID-19 Residual Abnormalities on Chest CT Scans. Radiology 2025, 316. [Google Scholar] [CrossRef]
| Variables | N= 60 |
|---|---|
| Age(years)1 | 60(13) |
| Gender2 | |
| Female | 34 (57%) |
| Male | 26 (43%) |
| BMI (kg/m2)1 | 32.4 (6.3) |
| Ethnicity2 | |
| White | 24 (40%) |
| Black | 12 (20%) |
| Asian | 16 (27%) |
| Any other ethnic | 8 (13%) |
| Smoking status2 | |
| Non-smoker | 40 (67%) |
| Ex-smoker | 18 (30%) |
| Smoker | 2 (3.3%) |
| Patient on medications2 | 21(35%) |
| PFT | |
| Spirometry1 | |
| FEV1 | 92 (21) |
| FVC | 94 (23) |
| VC | 92 (22) |
| FEV/VC | 102 (14) |
| PEF | 100 (23) |
| MMEF75/25 | 93 (44) |
| Lung volume1 | |
| TLC | 86 (18) |
| ERV | 95 (52) |
| RV | 83 (25) |
| RV/TLC | 98 (19) |
| Diffusion capacity1 | |
| TLCO SB | 83 (92) |
| VA Single Breath | 77 (17) |
|
1 Mean (SD); 2 n (%) |
|
| Parameter | Percentage of Patients | p-value* |
|---|---|---|
| FEV1 | 30.00 | 0.00 |
| FVC | 25.00 | 0.00 |
| FEV/VC | 3.33 | 0.00 |
| TLC | 35.00 | 0.00 |
| TLCO | 75.00 | 0.00 |
| VC | 25.00 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





