1. Introduction
Total knee arthroplasty (TKA) is one of the most commonly performed and resource-intensive orthopedic procedures, with steadily rising utilization in the United States and worldwide [
1,
2,
3]. As surgical volume continues to grow, optimizing perioperative quality, minimizing preventable complications, and reducing unnecessary readmissions have become central priorities for hospitals and health systems [
4,
5]. Among the organizational factors believed to influence outcomes, the “weekend effect” the theory that patients admitted or treated on weekends experience inferior outcomes due to reduced staffing and ancillary service availability has received considerable attention across multiple medical and surgical fields [
6,
7].
Evidence of weekend-associated risk has been reported in stroke, cardiac emergencies, and trauma populations [
8,
9,
10], but findings in elective orthopedic surgery are limited and inconsistent. Several existing arthroplasty studies have combined urgent and elective cases, pooled different joint procedures, or relied on pre-COVID-19 datasets that do not reflect contemporary enhanced recovery protocols [
11]. Moreover, nearly all prior studies have examined day of admission, not day of surgery, which creates a major classification bias: many patients admitted on a weekend undergo surgery on the following weekday, meaning their operative care does
not occur under weekend staffing conditions.
Under modern elective arthroplasty pathways, admission and surgery occur on the same calendar day, making this restriction highly accurate and clinically meaningful. Thus, in this analysis, a weekend admission truly represents a weekend surgery, eliminating the exposure misclassification that affects prior research.
Despite the importance of TKA as a high-volume, protocol-driven procedure, no contemporary nationwide study has evaluated whether weekend surgery influences postoperative complications, in-hospital outcomes, or 90-day readmissions in a homogeneous cohort of elective, primary, hospital-day-0 TKA patients in the post-COVID era [
12].
Research Questions
Does weekend admission, compared with weekday admission, adversely affect in-hospital outcomes, postoperative complications, or 90-day readmissions among adults undergoing elective primary total knee arthroplasty?
2. Methods
2.1. Study Design and Data Source
We conducted a retrospective cohort study using the Healthcare Cost and Utilization Project (HCUP) Nationwide Readmissions Database (NRD) for the years 2020-2022. The NRD is an encounter-level, all-payer claims database that captures approximately 60% of all U.S. inpatient hospitalizations and enables patient tracking within each calendar year through encrypted linkage identifiers.
2.2. Cohort Identification
Patients We identified adult patients (≥18 years) who underwent elective primary total knee arthroplasty (TKA) using ICD-10-PCS procedure codes listed in the primary procedure field (PR1). To obtain a clean and homogeneous elective cohort reflecting modern perioperative pathways, we applied the following criteria:
Inclusion
Exclusion
Nonelective or trauma admissions
Revision or bilateral TKA
Fracture, infection, or neoplasm at the time of admission
COVID-19 diagnosis (U07.1)
Patients <18 years old
Discharges after September (insufficient 90-day follow-up)
A total of 437,121 elective day-0 primary TKA admissions met criteria.
2.3. Exposure Definition: Weekend vs. Weekday Admission
The main exposure was day of admission:
Weekday: Monday-Friday
Weekend: Saturday-Sunday
This definition aligns with prior “weekend effect” studies and reflects typical U.S. hospital staffing structures.
2.4. Variables and Covariates
We extracted demographic, clinical, and hospital characteristics including: Age, Sex, Primary expected payer, Urban-rural patient location (NCHS categories), Comorbidities: hypertension, dyslipidemia, type 2 diabetes, chronic kidney disease, chronic lung disease, congestive heart failure, liver disease, chronic anemia, obesity, osteoporosis, obstructive sleep apnea, Robotic-assisted surgery (ICD-10-PCS 8E0Y0CZ, 8E0YXCZ).
2.5. Justification for Unadjusted Analysis
Weekend and weekday cohorts demonstrated near-identical distributions across all demographic variables, comorbidities, and hospital characteristics. Given this intrinsic balance, additional propensity-score matching or multivariable adjustment was not required, as these methods would not meaningfully reduce confounding or change effect estimates. Therefore, analyses were conducted on the raw, unadjusted cohort.
2.6. Outcomes
Measured outcomes included length of stay (LOS), total hospital charges, and postoperative complications—specifically deep vein thrombosis (DVT), pulmonary embolism (PE), acute kidney injury (AKI), sepsis, pneumonia, urinary tract infection (UTI), respiratory failure, intraoperative fracture, surgical site infection, blood loss anemia, postoperative pain (G89.18), and blood transfusion. Ninety-day outcomes included all-cause readmission, days to readmission, readmission LOS and readmission requiring a procedure.
2.7. Statistical Analysis
Continuous variables were compared using independent-samples t-tests. Categorical variables were compared using chi-square tests or Fisher’s exact test when expected cell counts were <5.Significance threshold was p < 0.05, two-sided. Analyses were performed using IBM SPSS Statistics.
2.8. Ethics Approval and Data Use Compliance
This study used fully de-identified data from the HCUP NRD. Per HCUP and federal policy, research using NRD data does not constitute human subjects research and does not require institutional review board (IRB) approval or informed consent. All analyses complied with the HCUP Data Use Agreement, and no attempt was made to identify individuals or institutions.
3. Results
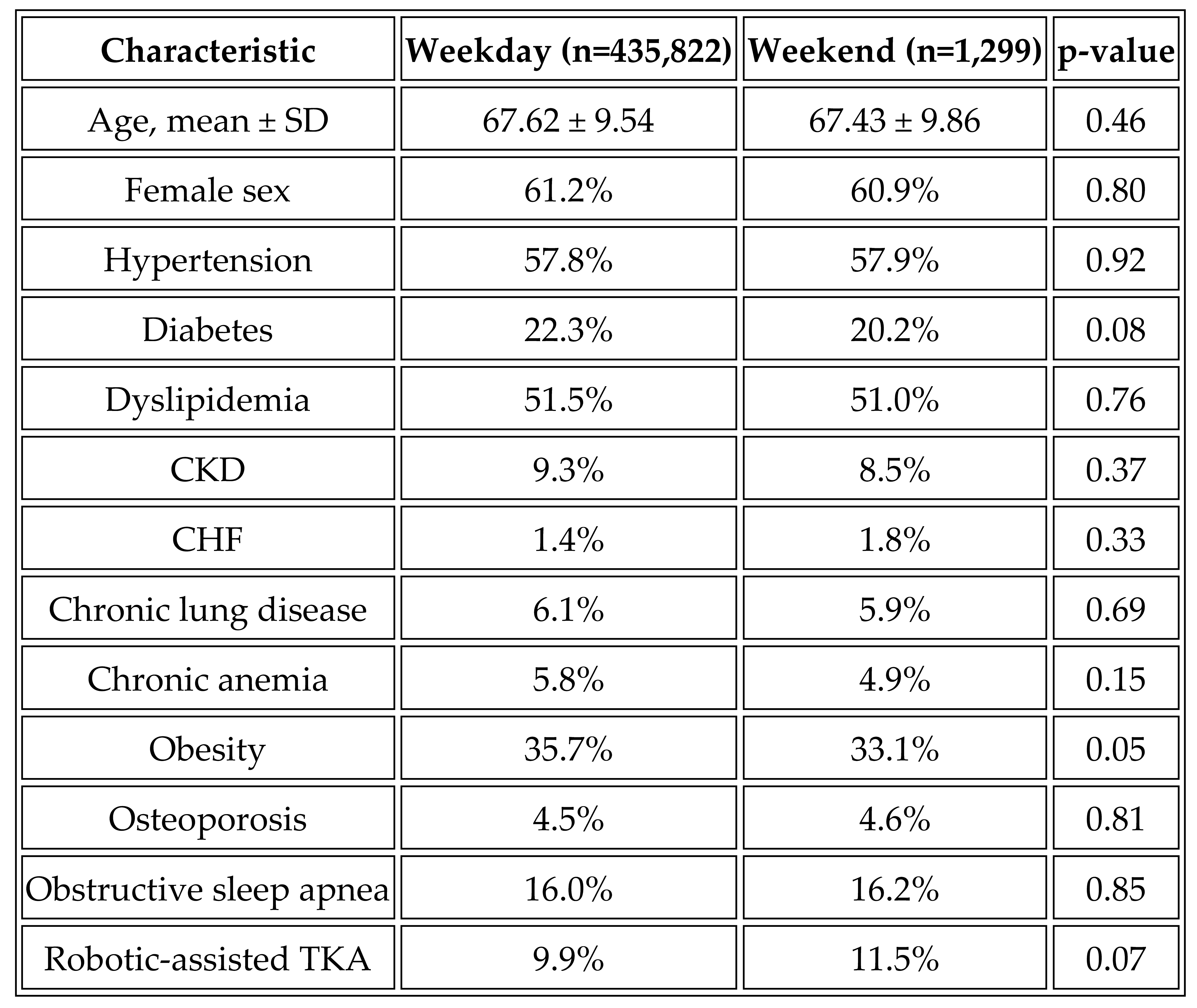
A total of 437,121 elective day-0 primary TKA admissions met inclusion criteria. Of these, 435,822 (99.7%) occurred on weekdays and 1,299 (0.3%) occurred on weekends. Baseline demographic, clinical, and hospital characteristics were highly similar between groups (
Table 1). Age and sex distribution were nearly identical, and no clinically meaningful differences were observed across primary payer type, urban-rural location, or any major comorbidity category. Robotic-assisted TKA was used at similar rates in both cohorts.
3.1. In-Hospital Outcomes
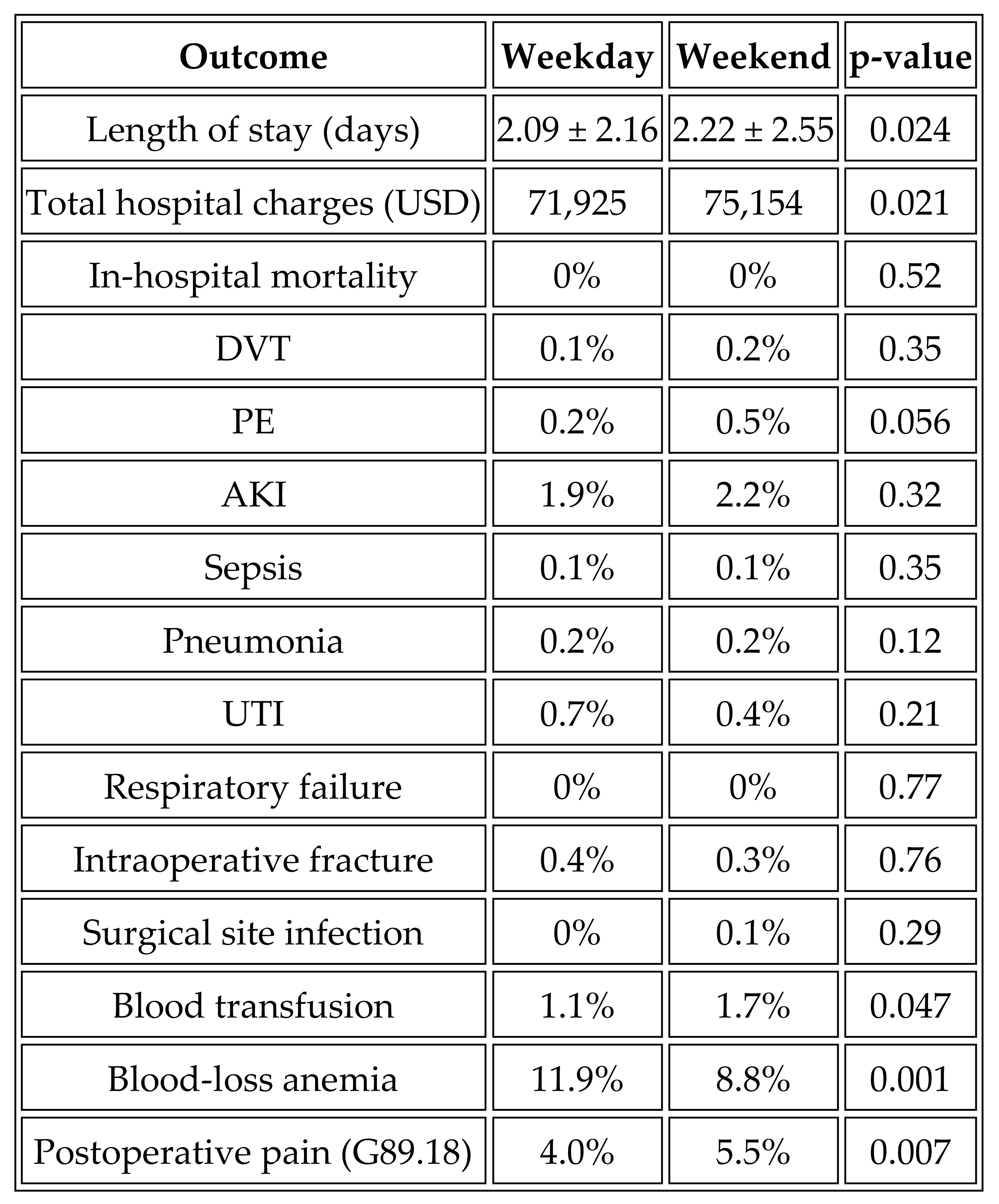
In-hospital outcomes were comparable between weekday and weekend admissions (
Table 2). Length of stay was similar (2.09 vs. 2.22 days), with a small absolute difference that did not represent a clinically meaningful effect. Total hospital charges were also comparable. In-hospital mortality was extremely rare in both groups, with no difference observed.
Postoperative complications including deep vein thrombosis, pulmonary embolism, acute kidney injury, sepsis, pneumonia, urinary tract infection, respiratory failure, intraoperative fracture, and surgical site infection occurred at low rates in both groups, with no significant or clinically meaningful differences. Although statistically significant p-values were noted for blood transfusion, blood-loss anemia, and postoperative pain, their absolute differences were small and not consistent with a weekend effect.
3.2. Ninety-Day Outcomes
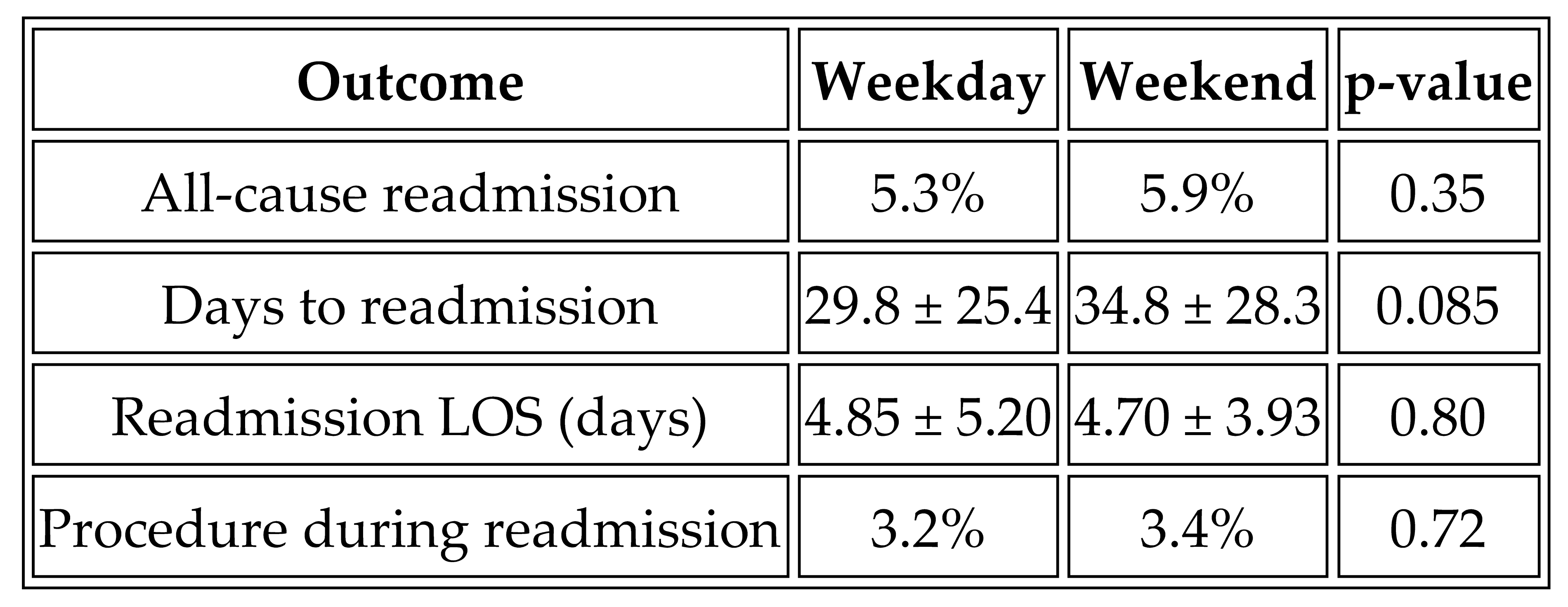
Ninety-day outcomes were also similar between groups (
Table 3). All-cause readmission occurred in 5.9% of weekend versus 5.3% of weekday admissions. Time to readmission and length of stay during readmission did not differ significantly. The proportion of readmissions requiring a procedure was nearly identical in both groups.
Across all evaluated inpatient and 90-day outcomes, no clinically meaningful weekend effect was identified in elective primary TKA.
4. Discussion
4.1. Key Observations
In this large, contemporary national cohort of more than 437,000 elective TKA procedures, weekend admission and surgery were not associated with worse in-hospital outcomes, postoperative complications, or 90-day readmissions. These findings suggest that, under modern perioperative pathways, elective TKA can be performed safely on weekends without evidence of a weekend effect.
4.2. Comparison with Prior Literature
Previous studies evaluating weekend outcomes in surgical populations have reported mixed findings. Some investigations observed higher mortality or complication rates for weekend admissions in emergency and high-acuity conditions, including stroke, myocardial infarction, and trauma [
12,
13]. In orthopedics, earlier studies often combined elective and urgent procedures, covered multiple joints, or predated enhanced recovery and standardized care pathways [
14,
15]. Many also relied on day of admission rather than day of surgery, introducing potential misclassification, because elective arthroplasty patients admitted on weekends frequently undergo surgery on weekdays [
16].
Our study overcomes this limitation by restricting the cohort to hospital-day-0 elective TKA, ensuring that weekend admissions represent weekend surgery. Within this refined definition, we found no evidence that weekend operative care compromises safety, complication risk, or readmission outcomes. These results align with more recent single-center and registry studies reporting comparable perioperative performance between weekend and weekday elective orthopedic procedures [
17,
18].
4.3. Interpretation and Clinical Implications
The absence of a weekend effect in elective primary TKA likely reflects several contemporary factors: standardized operative workflows, enhanced recovery protocols, multimodal analgesia, improved perioperative nursing coverage, and structured postoperative monitoring. Elective TKA is a highly protocolized operation, and deviations in staffing patterns during weekends may have limited practical impact on care delivery.
For hospitals seeking to expand surgical capacity or optimize scheduling flexibility, these results support the feasibility and safety of performing elective TKA on weekends. However, the extremely low proportion of weekend cases in this dataset suggests that weekend elective surgery remains uncommon nationally and may reflect institutional policies rather than patient selection.
4.4. Strengths and Limitations
Strengths of this study include its large national sample, restriction to elective day-0 surgery to avoid exposure misclassification, and evaluation of contemporary post-COVID-19 datasets that reflect current perioperative practice. The NRD structure also enabled robust assessment of 90-day readmissions.
Limitations include reliance on administrative coding, which may miss subtle clinical details or misclassify complications. The weekend cohort was small relative to the weekday cohort. Unmeasured confounders such as surgeon experience, staffing patterns, or intraoperative efficiency could not be captured. The NRD does not provide implant details, functional outcomes, or outpatient complications. Finally, the observational design precludes establishing causality.
5. Conclusions
In this contemporary nationwide cohort of more than 437,000 TKA procedures, weekend admission and surgery were not associated with higher rates of postoperative complications, in-hospital morbidity, or 90-day readmission. Outcomes were highly comparable between weekend and weekday cases across all clinically relevant measures. These findings indicate that, within modern standardized perioperative pathways, elective TKA can be performed safely on weekends without evidence of a weekend effect. Further work should explore whether these results apply to other elective orthopedic procedures and to institutions with varying staffing structures.
Author Contributions
Conceptualization, YB and DM; Writing—original draft DM; Statistical analysis, DM; Writing—review & editing DM; Supervision, mentoring, and project administration YS YB. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted under exempt status granted by the institutional review board, and the requirement for informed consent was waived due to the de-identified nature of the NIS dataset.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nham, F.H.; Patel, I.; Zalikha, L. Epidemiology of primary and revision total knee arthroplasty: Analysis of demographics, comorbidities and outcomes from the national inpatient sample. Arthroplasty 2023, 5, 18. [Google Scholar] [CrossRef]
- Shichman, I.; Roof, M.; Askew, N.; Nherera, L.; Rozell, J.C.; Seyler, T.; Schwarzkopf, R. Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040–2060. JBJS Open Access 2023, 8, e22.00112. [Google Scholar] [CrossRef]
- Mantel, J.; Ruppenkamp, J.W.; Cantu, M. Total knee arthroplasty in the outpatient vs inpatient settings: Impact of site of care on early postoperative economic and clinical outcomes. J Orthop Surg Res 2023, 18, 273. [Google Scholar] [CrossRef]
- MacMahon, A.; Rao, S.S.; Chaudhry, Y.P.; Hasan, S.A.; Epstein, J.A.; Hegde, V.; Valaik, D.J.; Oni, J.K.; Sterling, R.S.; Khanuja, H.S. Preoperative Patient Optimization in Total Joint Arthroplasty—The Paradigm Shift from Preoperative Clearance: A Narrative Review. HSS J. 2022, 18, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Hospital Readmissions After Total Joint Arthroplasty: An Updated Analysis and Implications for Value-Based Care, published in Journal of Arthroplasty, 2023;38(3):431-436 has DOI 10.1016/j.arth.2022.09.
- Mathews JA, Vindlacheruvu M, Khanduja V. Is there a weekend effect in hip fracture patients presenting to a United Kingdom teaching hospital? World J Orthop. 2016 Oct 18;7(10):678-686. [CrossRef]
- Al-Naseem AO, Mehkri Y, Chakravarti S, Johnson E, Kelly-Hedrick M, Kuo C, Erickson M, Than KD, Rocos B, Bhowmick D, Shaffrey CI, Foster N, Baaj A, Dahdaleh N, Goodwin CR, Williamson TL, Lu Y, Abd-El-Barr MM. Comparison of intraoperative and postoperative outcomes between open, wiltse, and percutaneous approach to traumatic thoracolumbar spine fractures without neurological injury: A systematic review and meta-analysis. N Am Spine Soc J. 2024 Aug 14;20:100547. [CrossRef]
- Saposnik, G.; Baibergenova, A.; Bayer, N.; Hachinski, V. Weekends: A Dangerous Time for Having a Stroke? Stroke 2007, 38, 1211–1215. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Al-Dokheal, M.; Aldaham, S.; Rushton, C.; Butler, R.; Kinnaird, T.; Zaman, A.; Zaman, M.J.; Timmis, A.; Mamas, M.A. Weekend Effect in Acute Coronary Syndrome: A Meta-Analysis of Observational Studies. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 432–442. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-C.; Liu, C.-Y.; Tzeng, I.-S.; Hsieh, T.-H.; Chang, C.-Y.; Hou, Y.-T.; Chen, Y.-L.; Chien, D.-S.; Yiang, G.-T.; Wu, M.-Y. The Impact of Holiday Season and Weekend Effect on Traumatic Injury Mortality: Evidence from a 10-Year Analysis. Tzu Chi Med. J. 2023, 35, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.; Nightingale, J.; Sehat, K. Is there a ‘weekend effect’ in elective lower limb arthroplasty? Ann. R. Coll. Surg. Engl. 2021, 103, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Momtaz, D.; Khalafallah, Y.; McLennan, A.; Ghali, A.; Ghobrial, P.; González, R.; Seifi, A.; Saleh, K. Weekend versus Weekday Procedures for Total Knee Arthroplasty. J. Knee Surg. 2025, 38, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Aylin, P.; Alexandrescu, R.; Jen, M.H.; Mayer, E.K.; Bottle, A. Day of week of procedure and 30-day mortality for elective surgery: Retrospective analysis of hospital episode statistics. BMJ 2013, 346, f2424. [Google Scholar]
- Aylin, P.; Alexandrescu, R.; Jen, M.H.; Mayer, E.K.; Bottle, A. Day of week of procedure and 30-day mortality for elective surgery: Retrospective analysis of hospital episode statistics. BMJ 2013, 346, f2424. [Google Scholar] [CrossRef]
- Kim, S.B.; Lee, J.W.; Kim, A. Weekend effect on 30-day mortality for ischemic and hemorrhagic stroke: A nationwide cohort study. PLoS ONE 2023, 18, e0283491. [Google Scholar] [CrossRef]
- Sorita, A.; Ahmed, A.; Starr, S.R. Off-hour presentation and outcomes in patients with acute myocardial infarction: Systematic review and meta-analysis. BMJ 2014, 348, f7393. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.; Nightingale, J.; Sehat, K. Is there a ‘weekend effect’ in elective lower limb arthroplasty? Ann. R. Coll. Surg. Engl. 2021, 103, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Momtaz, D.; Khalafallah, Y.; McLennan, A.; Ghali, A.; Ghobrial, P.; González, R.; Seifi, A.; Saleh, K. Weekend versus Weekday Procedures for Total Knee Arthroplasty. J. Knee Surg. 2025, 38, 477–484. [Google Scholar] [CrossRef] [PubMed]
Table 1.
Baseline Characteristics of Weekday vs. Weekend Admissions.
Table 1.
Baseline Characteristics of Weekday vs. Weekend Admissions.
Table 2.
In-Hospital Outcomes.
Table 2.
In-Hospital Outcomes.
Table 3.
Ninety-Day Outcomes.
Table 3.
Ninety-Day Outcomes.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).