1. Introduction
In contemporary gynecology, a holistic approach that also includes aspects of sexual health is increasingly recommended for many clinical issues. Preventive measures such as maintaining a healthy lifestyle, physical activity, and appropriate diet play a significant role, with particular emphasis placed on dietotherapy—for example, in the context of the interdisciplinary nature of genital discomfort.
Vulvar discomfort, manifested by itching or burning sensations in the intimate area, reduces the quality of life of girls and women regardless of age [
1]. In sexually active women, it is associated with dyspareunia and decreased libido, becoming a partnership problem that often requires sexological couples therapy [
2]. In postmenopausal and elderly patients, due to the risk of vulvar cancer, it is not only a gynecological or geriatric issue but also an important dermatological and oncological concern [
3].
The problem of genital discomfort may have multiple causes—from dermatoses, fungal and bacterial infections, and allergies, to hormonal disorders—and it affects patients of all ages, becoming a significant issue also in developmental-age gynecology (also referred to as pediatric and adolescent gynecology) [
2,
4,
5].
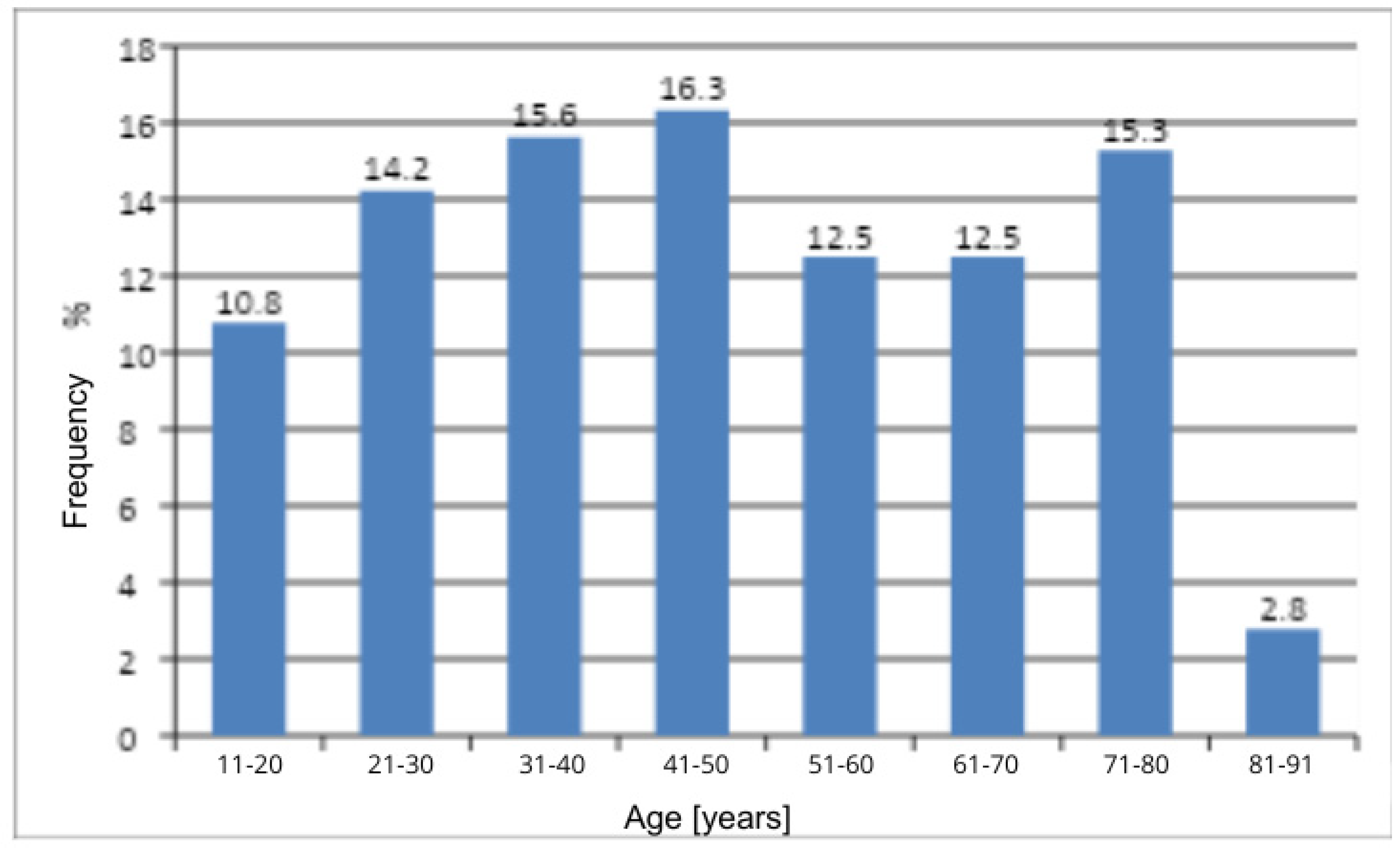
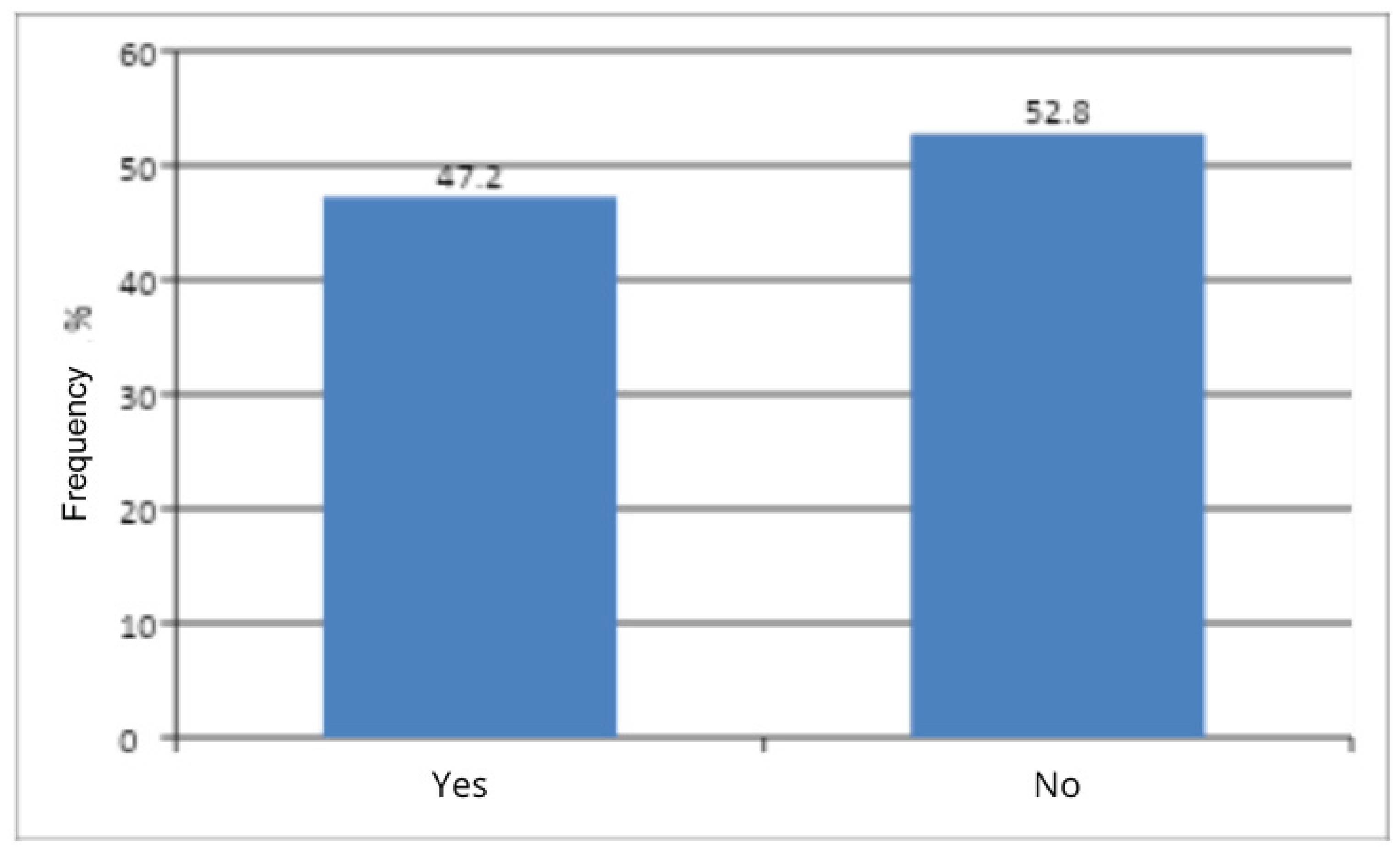
The pilot study included 288 gynecological patients aged 11 to 91 years who presented to outpatient clinics with symptoms of vulvar itching and genital discomfort. All patients reported discomfort. It should be emphasized that this study did not analyze the subgroup of girls attending pediatric gynecology clinics, in whom such discomfort was an additional but not the primary problem; this group was analyzed separately in another study.
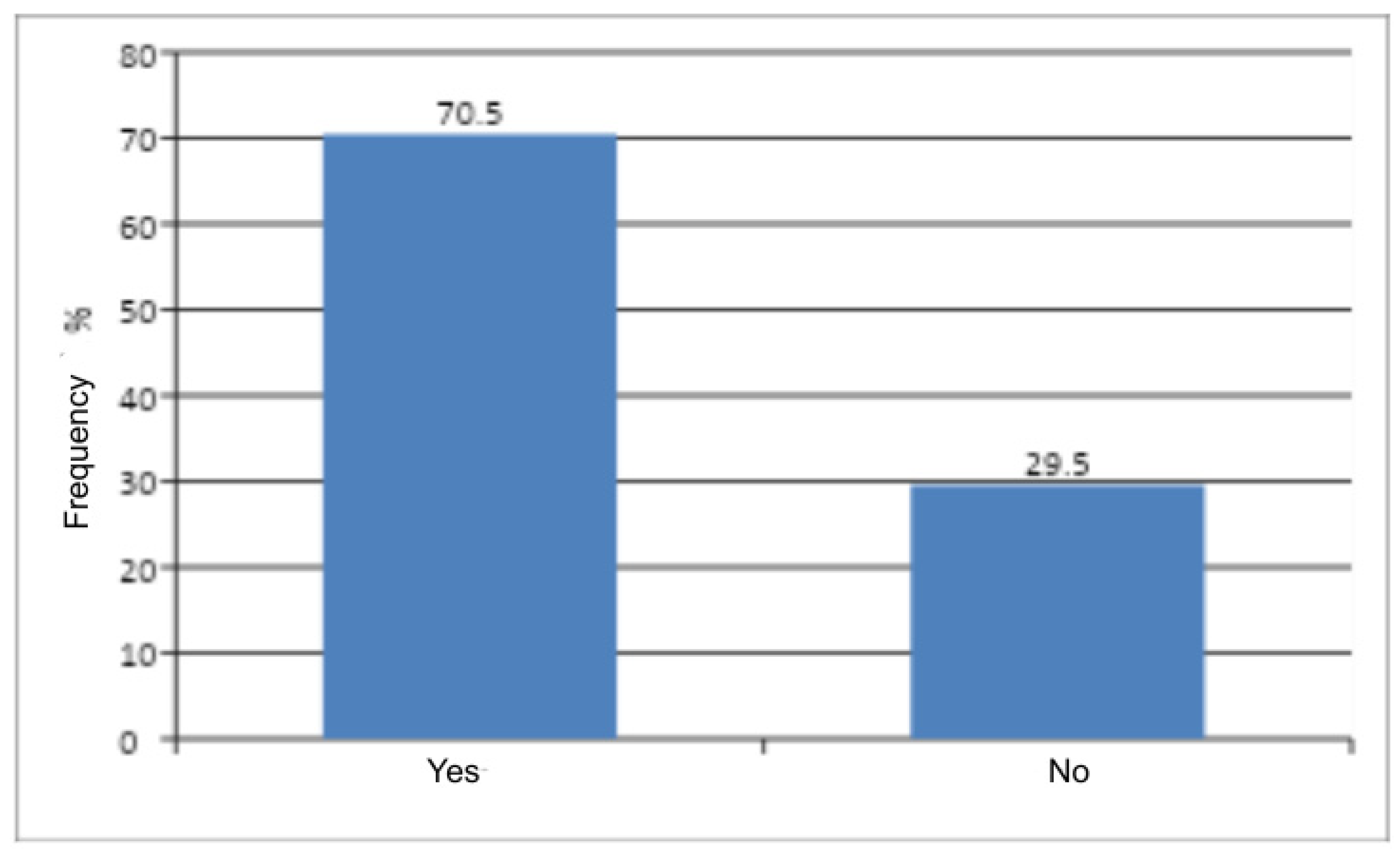
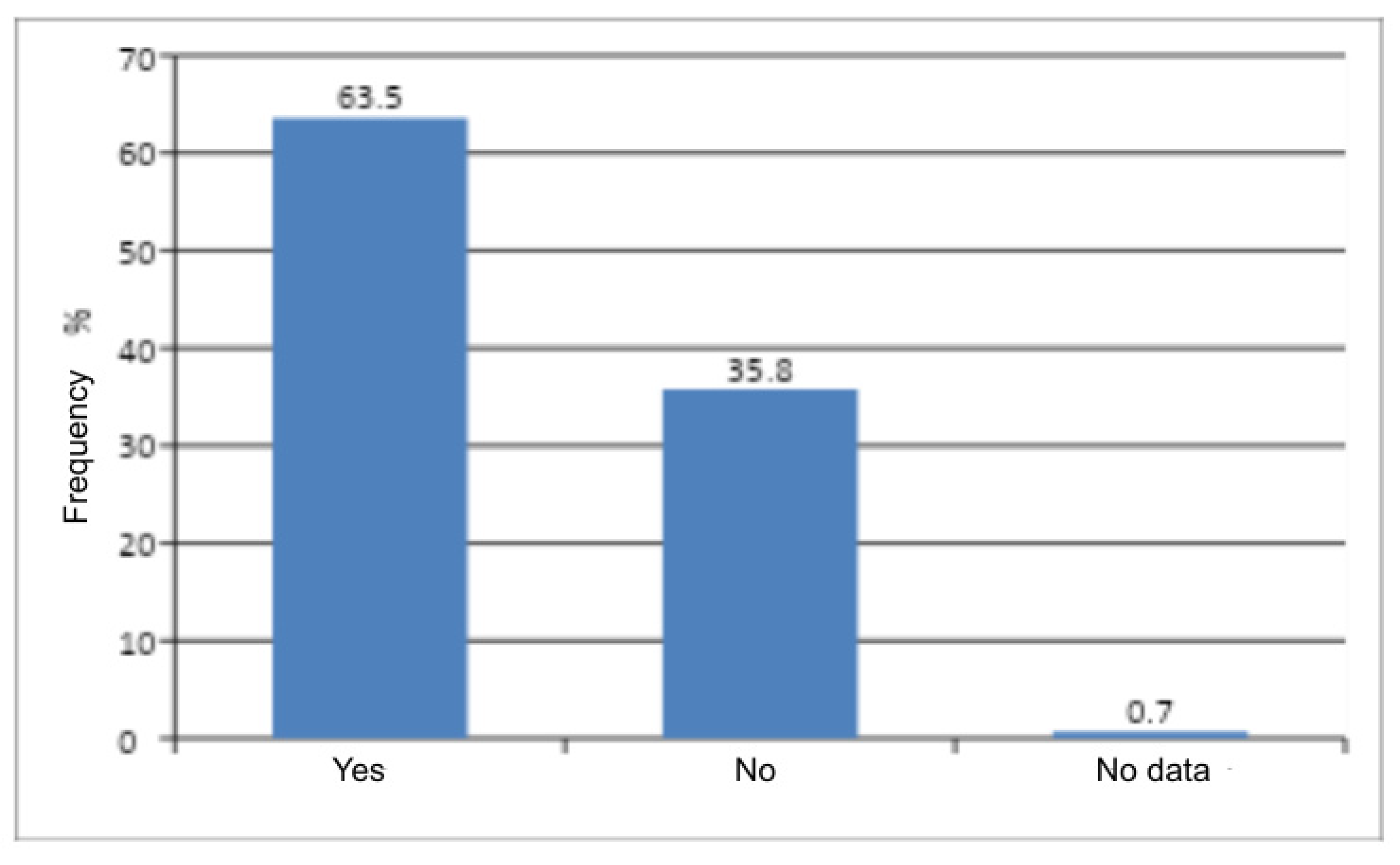
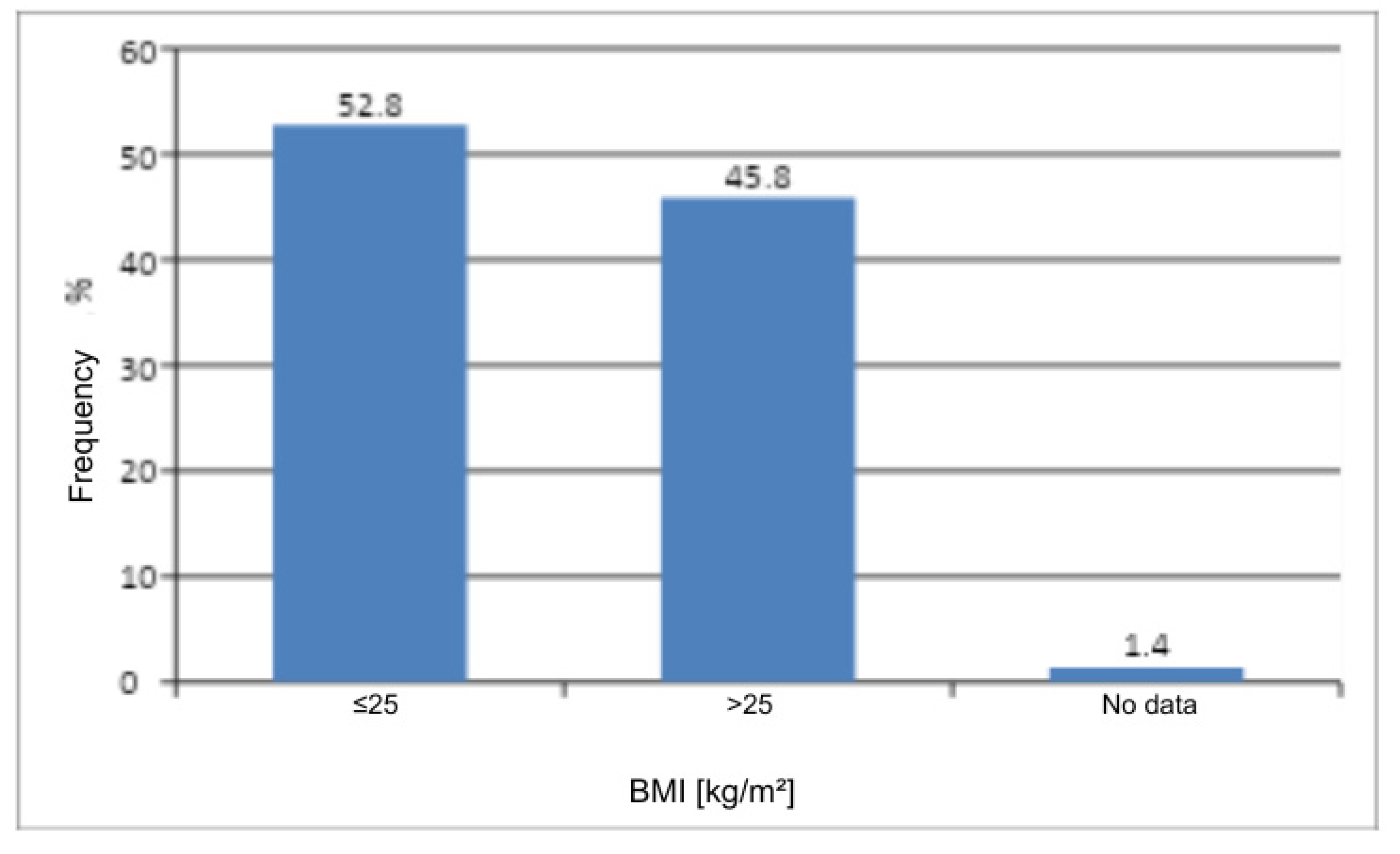
In the pilot analysis, typical correlations between discomfort and variables such as age group, comorbidities, pregnancy status, BMI (underweight/normal/overweight/obese), or menopausal status (<48 years / ≥48 years) were not examined. Instead, an attempt was made to determine whether any specific subcategory predominated among the studied gynecological patients. The patients underwent further diagnostic evaluation, including sexological and dermatological consultations. However, the results of these further diagnostic assessments are not the subject of this pilot report. It is worth emphasizing, nevertheless, the interdisciplinary nature of this issue.
Given the widespread nature of the problem of genital discomfort (vulvar itching), the aim of this study was to determine whether, and to what extent, selected factors from the medical history—such as age, obstetric history, and body mass index (BMI)—influence the frequency of this condition as a reason for visiting a gynecologist.
4. Discussion
Genital discomfort, manifested by burning and vaginal irritation, is a condition that can significantly reduce the quality of life of girls and women. This problem affects patients of all ages and may have various etiologies—ranging from dermatoses, fungal and bacterial infections, and allergies to hormonal disorders. Although itching is usually transient and mild, in some cases it may indicate more complex and serious health problems, often associated with metabolic disturbances [
1]. In this context, attention should also be drawn to the importance of probiotics, prebiotics, symbiotics, and dietotherapy, which play a role in maintaining genital health [
6].
Genital discomfort and vulvar diseases represent conditions for which patients commonly seek consultation with gynecologists and dermatologists. The symptoms of vulvar disorders frequently require combined gynecological and dermatological management. A significant group in this regard consists of dermatoses that may involve not only the genital area—the vulva may be just one of several affected sites [
7,
8,
9].
In sexually active women, genital discomfort is often associated with dyspareunia and reduced libido, becoming a relationship problem that may require sexological couples therapy [
2]. In postmenopausal and elderly women, due to the risk of vulvar cancer, this condition represents not only a gynecological and geriatric issue but also a dermatological and oncological concern [
3].
Genital discomfort, with its diverse causes—dermatoses, infections (fungal or bacterial), allergies, and hormonal disturbances—affects women across all age groups and constitutes an important problem also in developmental-age gynecology [
5].
The pilot study included 288 gynecological patients aged 11 to 91 years who presented to outpatient clinics with symptoms of vulvar itching and genital discomfort. All patients reported the presence of discomfort. It should be emphasized that the study did not include a group of girls attending pediatric gynecology clinics, in whom such discomfort was an additional but not the primary reason for consultation; this subgroup was analyzed separately in another study.
In this pilot analysis, typical correlations between genital discomfort and variables such as age (age groups), comorbidities (yes/no), pregnancy history (yes/no), body mass index (underweight/normal/overweight/obese), or menopausal status (<48 years / ≥48 years) were not examined. Instead, the analysis focused on identifying whether any specific subcategory predominated among the gynecological patients studied. The participants underwent further diagnostic evaluation, including sexological and dermatological consultations; however, the results of those additional assessments are beyond the scope of this pilot report. It is worth underscoring once again the interdisciplinary character of this issue.
The discomfort experienced by the patients was characterized primarily by intense itching in the intimate area. This symptom could involve both the vaginal interior and the external parts of the vulva, such as the labia, clitoris, and vestibule of the vagina. The itching sensation could make sitting uncomfortable, cause distraction, provoke scratching, and—as emphasized—may even prevent sexual activity. The discomfort was often accompanied by burning, skin irritation, and changes in vaginal discharge, all of which may significantly affect a woman’s well-being and daily quality of life. A more detailed differentiation of these symptoms is planned for subsequent analyses.
It should be reiterated that genital discomfort as a gynecological complaint may result from minor irritations, but can also be a sign of more serious health conditions requiring diagnosis and treatment. It may be a manifestation of dermatoses [
5,
7,
8,
9], hypoestrogenism typical of postmenopausal and senium periods [
3], or various medical disorders, including fungal and bacterial infections [
10], allergies, endocrine diseases [
11] and vulvodynia [
12].
Although the applied therapy in the studied patients was not the subject of analysis, it is important to emphasize that in order to select an appropriate treatment, it is essential to determine which microorganism is responsible for the symptoms. This requires a detailed medical history, including information about other symptoms accompanying the itching—such as the type of discharge, presence of pain, and skin changes in the intimate area. It is also necessary to perform appropriate diagnostic tests and, when indicated, refer patients for specialist consultations, including dermatology, oncology, and other relevant disciplines [
1].
In some patients, genital discomfort and intense itching of the vagina and vulva are the only noticeable symptoms of an allergy or genital infection. However, the vast majority of women experience additional symptoms, such as:
Redness in the intimate area, including the labia, clitoral region, and vaginal introitus,
Swelling of both the minor and major labia,
Pain and tenderness in the genital area, particularly during intercourse, washing, or touch,
Vaginal discharge with unpleasant odor, abnormal consistency (e.g., curd-like or foamy), or color (white, gray, greenish),
Burning sensation during urination and increased urinary frequency,
Nighttime discomfort associated with itching and urgency,
Postcoital vaginal itching,
Atrophic changes of the vulvar and vaginal epithelium [
1,
2,
8,
10,
13,
14,
15,
16].
Genital discomfort and the accompanying itching may have numerous causes, which can be broadly divided into infectious and non-infectious origins. The most important among them include:
Allergic reactions to components present in products such as sanitary pads, panty liners, or tampons—especially those containing fragrances or dyes. Allergies may also be triggered by the materials used in underwear, particularly synthetic, non-breathable fabrics. In addition, laundry detergents, including strongly perfumed washing powders and fabric softeners, may provoke allergic irritation [
5,
10].
Fungal infection (candidiasis, yeast infection) of the vagina: it is estimated that up to 75% of women experience vaginal and vulvar candidiasis at least once in their lifetime, and approximately 40–50% of cases are recurrent. The infection is most often caused by Candida albicans, responsible for 80–92% of cases. Symptoms include white, curd-like discharge, irritation of the vaginal and vulvar mucosa, swelling, pain, and intense itching, particularly during sexual intercourse and urination. Predisposing factors include pregnancy, diabetes, obesity, antibiotic or corticosteroid therapy, immunosuppression, hormonal disturbances, poor hygiene, and the use of intrauterine devices (IUDs) [
1,
6,
10,
14].
Trichomoniasis, an infection caused by Trichomonas vaginalis, manifests as profuse, frothy, greenish vaginal discharge with a foul, musty odor, pain during urination, burning, dyspareunia (pain during intercourse), and swelling of the vagina and vulva. In severe cases, the swelling may be so pronounced that it impedes sexual intercourse or gynecological examination. Trichomoniasis is primarily sexually transmitted [
1,
10,
14].
Bacterial infection – bacterial vaginosis: in such cases, itching is usually mild, but there is a characteristic fishy odor of the vaginal discharge. The condition results from an imbalance in the vaginal microbiota and excessive proliferation of anaerobic bacteria, such as
Prevotella spp., Gardnerella vaginalis, and
Mycoplasma hominis [
1,
10,
14].
Risk factors for genital discomfort and inflammatory conditions include the use of intrauterine devices (IUDs), smoking, diabetes, and poor hygiene, especially during menstruation, as well as a high number of sexual partners, which will be analyzed in subsequent stages of the study [
10,
14]
Another important risk factor, as analyzed, is obstetric history, with multiparity playing a notable role.
Viral infections caused by herpes simplex virus type 2 (HSV-2)—less commonly HSV-1—lead to genital herpes. Early symptoms include pain, burning, and itching, followed by redness, vesicles, and ulcerations. The disease is often accompanied by painful urination, vaginal discharge, joint and muscle pain, and fever. Symptoms may persist for several weeks, and the infection tends to recur. Genital herpes is particularly dangerous during pregnancy, as it can lead to preterm delivery and neonatal infection [
14].
Hormonal changes, occurring particularly during the perimenopausal and senium periods, have been shown to play a significant role. A low level of estrogens may lead to atrophy of the vaginal and vulvar mucosa. As a result, the epithelium becomes thinner, less hydrated, and more prone to irritation, leading to dryness, burning, and itching. Contact spotting and dyspareunia may also occur. A reduced estrogen level increases vaginal pH, thereby raising the risk of infection. Treatment includes estrogen supplementation, the use of moisturizing preparations, and attention to proper hygiene and lifestyle, including smoking cessation [
3].
Other, less common causes of vaginal itching (not analyzed in this study) include: mechanical irritation, e.g., during sexual intercourse or the use of erotic devices; excessive hygiene practices, leading to dryness of the intimate area, including vaginal douching; sexually transmitted diseases (STDs) such as chlamydia, genital herpes, HPV (condylomata acuminata), gonorrhea, and others [
14], which can cause characteristic symptoms including skin lesions, abnormal discharge, and persistent itching; hemorrhoids, whose itching and irritation may extend to the vaginal area; dermatoses such as lichen sclerosus [
17], psoriasis, or atopic dermatitis, which can manifest with itching of the intimate regions; diabetes mellitus [
18], which increases susceptibility to fungal infections due to altered microflora and elevated glucose levels promoting yeast growth; chronic stress and emotional tension, which may affect the skin and mucous membranes, leading to itching; and vulvar cancer, which may present with severe itching, nodules, or ulcerations in the vulvar region.
It should be emphasized that in all these contexts, the cooperation between gynecologists and dermatologists is of particular importance.
Failure to undertake diagnosis and treatment of conditions associated with genital discomfort may lead to serious and irreversible consequences, which tend to worsen the longer the problem persists. It is essential to emphasize the need for histopathological verification of vulvar skin lesions, especially in postmenopausal and elderly patients, as this stage of life carries an increased risk not only of dystrophic changes but also of vulvar cancer [
3].
Another non-oncological concern is that inflammatory processes, particularly those of bacterial origin, may spread to the urethra, cervix, and fallopian tubes, leading to adhesion formation and, consequently, infertility [
19]. Untreated genital infections may also result in the development of pelvic abscesses, which often require surgical intervention, since conservative antibiotic therapy is usually insufficient in such cases.
During a gynecological consultation, a detailed medical history is crucial, with attention paid to the circumstances under which symptoms occur, their intensity, duration, and any additional manifestations related to sexual activity. A thorough examination of the vulva and vagina using a speculum is necessary, with a focus on redness, mucocutaneous changes, and the character of vaginal discharge. It is also important to perform a transvaginal ultrasound (TVUS) and collect a vaginal swab for cytology, as well as refer the patient for blood or urine tests and, when indicated, specialist consultations, particularly dermatologicts [
1].
The treatment of genital discomfort depends on its underlying cause. If symptoms appear after the introduction of new hygienic or washing products, their use should be immediately discontinued; in many cases, symptoms will resolve spontaneously. If they persist, oral antihistamines may be indicated [
5].
In cases of candidiasis, topical antifungal creams or vaginal suppositories are used, and in more severe cases, oral antifungal therapy may be required for a longer duration. Bacterial infections are treated with metronidazole, administered both orally and topically. Trichomoniasis is treated with antiprotozoal agents, such as nifuratel [
1].
In the case of genital herpes, no treatment can completely eliminate the virus; however, during exacerbations, antiviral medications such as acyclovir are used to inhibit viral replication [
1,
14].
Itching resulting from vulvar dystrophy, caused by a decrease in estrogen levels during the perimenopausal and senium periods, can be alleviated with creams, tablets, or vaginal rings containing estriol. If the itching is due to insufficient lubrication leading to microtraumas and abrasions, the use of moisturizing and mucosal-regenerating preparations is recommended—these most often contain hyaluronic acid or its salts and are available in the form of vaginal suppositories, creams, or gels [
3].
In other cases of irritation and itching, such as those caused by lichen sclerosus, topical steroid therapy may be necessary.
In terms of prevention, it is important to follow basic hygiene principles: intimate areas should be washed at least twice daily with neutral cleansing agents, and sanitary pads or panty liners should be changed regularly. It is also advisable to increase the consumption of dairy products, which are a natural source of probiotics that support the colonization of beneficial bacteria [
6].
During treatment of genital infections, alcohol consumption should be avoided, and sexual abstinence is recommended; in some cases, simultaneous treatment of the partner may be necessary.
Symptoms such as discomfort, itching of the vulva and vagina tend to recur, which highlights the importance of preventive measures, including:
Using gentle, hypoallergenic intimate hygiene products that do not cause irritation, while avoiding excessive hygiene practices (especially vaginal douching), which may disturb the natural microbiota;
Avoiding perfumed cosmetics, toilet paper, and sanitary products, as well as potential allergens such as new laundry detergents;
Using pads instead of tampons, particularly during the last days of menstruation;
Washing the perineal area with warm water, always from the vaginal vestibule toward the anus;
Wiping from front to back after bowel movements;
Avoiding prolonged moisture in the genital area, such as sitting in a wet swimsuit;
Wearing loose, breathable cotton underwear [
10];
Using condoms during sexual intercourse [
14];
Taking probiotics to support the restoration of the vaginal microbiota [
6];
Applying gentle vaginal moisturizers, such as vaginal suppositories [
1].
Author Contributions
Conceptualization, G.J.B., A.P. and M.P; methodology, K.P.G.; validation, A.P, M.P., Y.Y; formal analysis, G.J.P, W.K.; investigation, M.M, M.P.K, J.M.; resources, W.K.; data curation, A.P., M.P.; writing—original draft preparation, G.J.B, K.P.R, M.M, M.P,K, J.M.; writing—review and editing, A.P.; supervision, G.J.B, W.K.; project administration, G.J.B.; funding acquisition, G.J.P, W.K. All authors have read and agreed to the published version of the manuscript.