1. Introduction
Uterus didelphys bicollis is part of the congenital uterine anomalies caused by a failure in the fusion of the paramesonephric ducts, also called Müllerian ducts [
1].
Congenital malformations of the female reproductive tract are estimated to occur in 0.1% to 3% of live births. In the case of Müllerian malformations, the prevalence is thought to depend on the population studied: between 5.5% and 6.7% of diagnoses in the general population, 8% of patients with infertility, and 24% of patients with a history of abortion and infertility [
2]. Didelphys uterus accounts for approximately 5% of uterine anomalies [
1].
The objective of this report is to present the case of a patient with uterus didelphys bicollis with uterine myomatosis from the imaging service of Gynecological Pediatric Hospital No. 7, with a finding in this service.
2. Case Presentation
This is a 34-year-old female patient, referred to the imaging service to investigate a didelphys uterus vs. a bicornuate uterus. Without a significant personal history, she reports G0, menarche at 13 years, rhythm 7-8x30, start of active sexual life at 21 years, number of sexual partners: 3. The patient was under follow-up by the gynecology service due to the diagnosis of abnormal uterine bleeding (AUB). A Mirena IUD was inserted with complications upon insertion due to a non-patent duct, so she was referred to the imaging service.
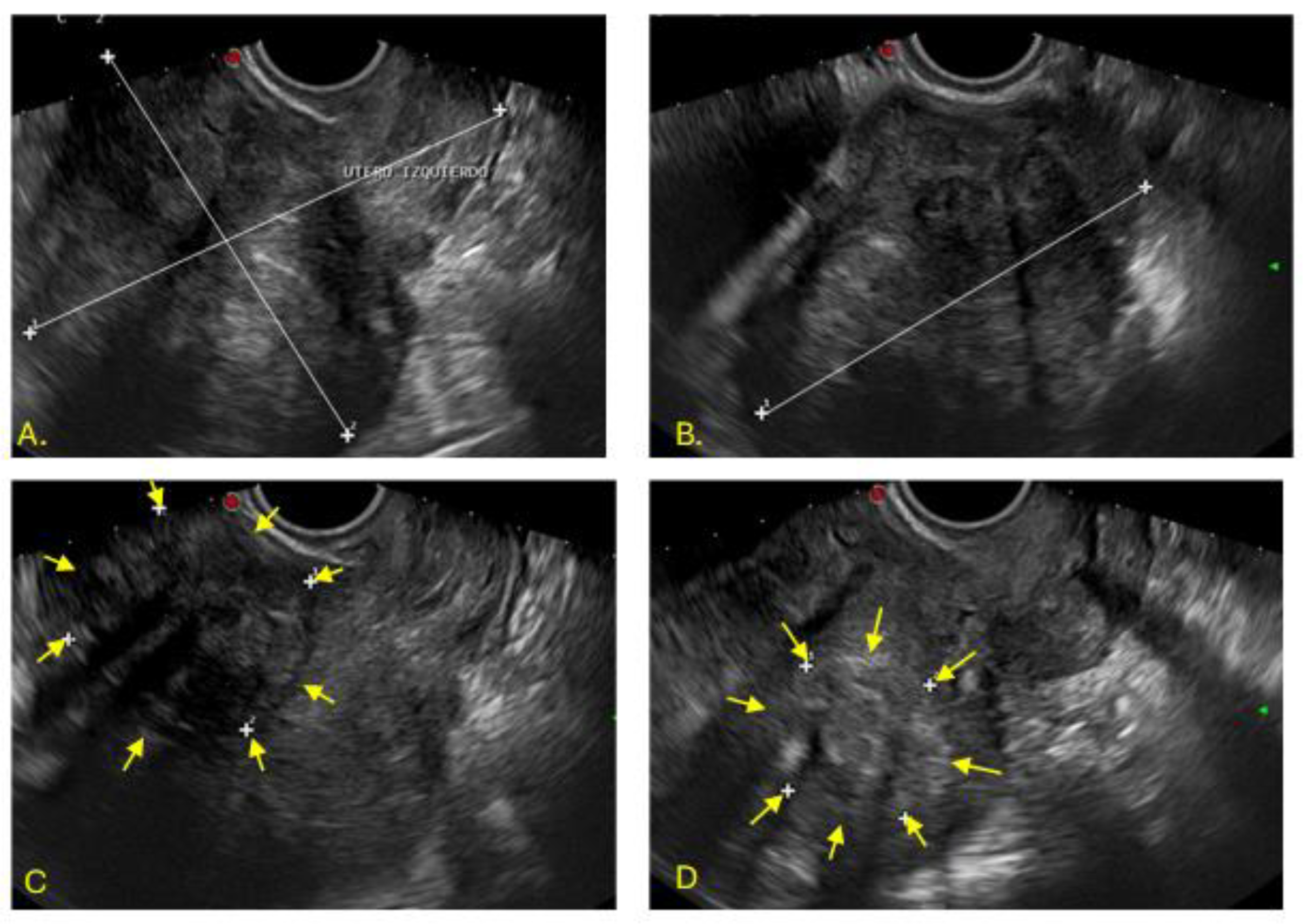
An endovaginal ultrasound was performed in the imaging department, identifying two uteri. The left uterus, with lobulated borders, measured 105x90x90mm and showed a heterogeneous myometrium, with two solid nodular images: one intramural, 50x48mm, and the other posterior, 36x43mm, corresponding to FIGO 2 and 3 fibroids (
Figure 1).
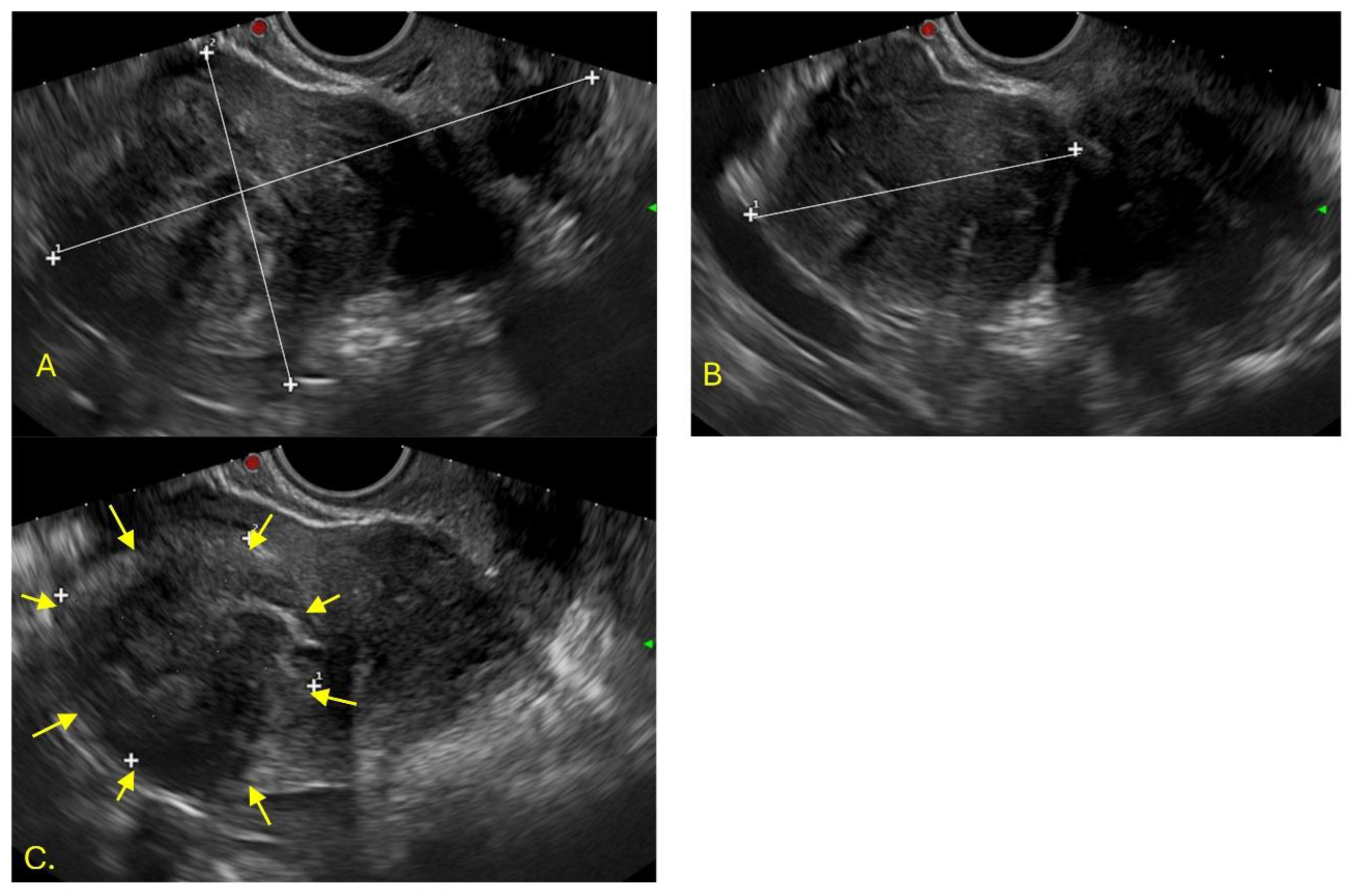
The right uterus measured 112x67x65mm, with heterogeneous myometrium and a solid submucosal nodular image of 52x49mm (FIGO 1), which caused endometrial dilation (
Figure 2)
To complete the diagnosis, a hysterosalpingogram was ordered. Before the procedure, a gynecological examination with a vaginal speculum was performed, revealing a well-structured septum completely separating the two vaginal cavities. The follow-up x-ray revealed an IUD in the right endometrial cavity (
Figure 3).
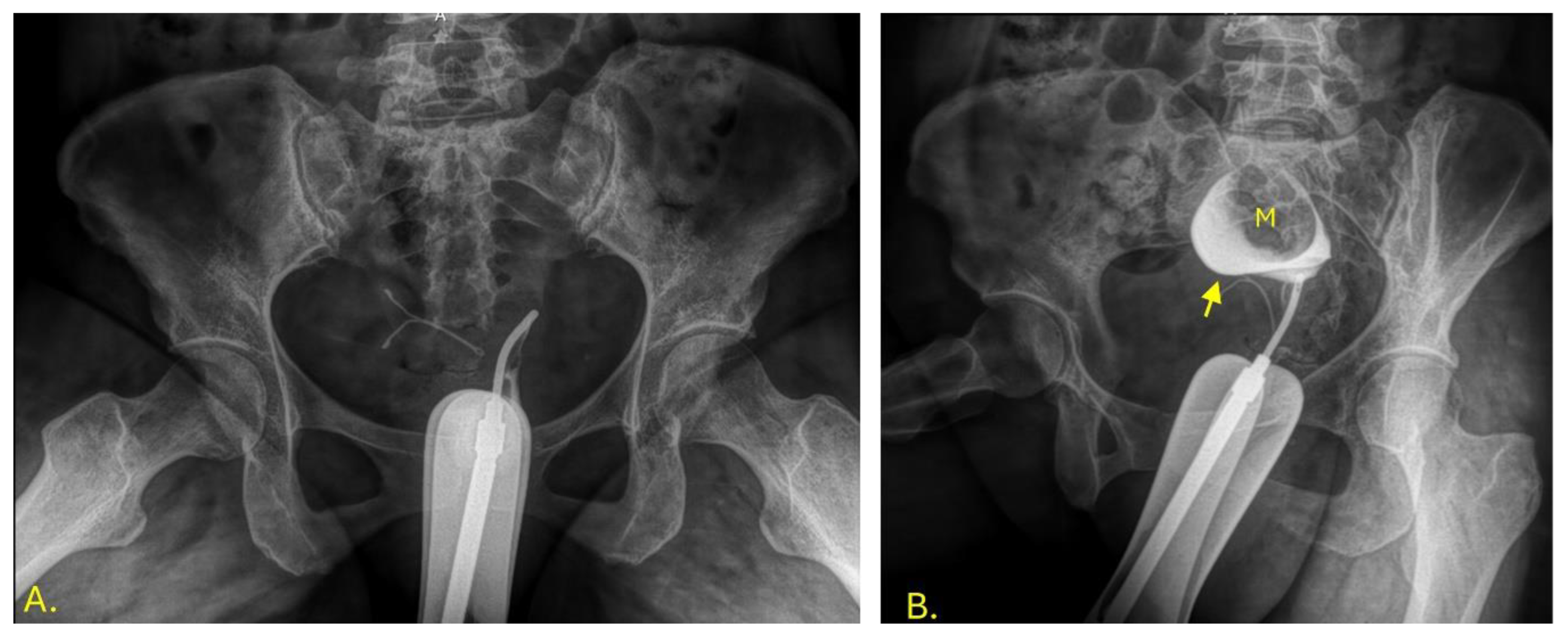
During the hysterosalpingography, a uterus was observed in the left vaginal cavity in anteroversion lateralized to the left, with adequate passage of the contrast medium towards the peritoneum through the uterine tube. The edges of the uterus in the evaluable area are defined as uterus didelphys bicollis (
Figure 4).
Figure 4.
Left hysterosalpingography. Image A: Jarcho cannula in the left uterus. Image B: Contrast medium is instilled, revealing the endometrial cavity (indicated by an arrow) with an image inside that suggests the presence of a submucous fibroid (M).In the right vaginal cavity, the IUD was seen in the vaginal fundus, and contrast passed into the peritoneum through the right uterine tube without complications, with an anteroverted uterus lateralized to the right (
Figure 5).
Figure 4.
Left hysterosalpingography. Image A: Jarcho cannula in the left uterus. Image B: Contrast medium is instilled, revealing the endometrial cavity (indicated by an arrow) with an image inside that suggests the presence of a submucous fibroid (M).In the right vaginal cavity, the IUD was seen in the vaginal fundus, and contrast passed into the peritoneum through the right uterine tube without complications, with an anteroverted uterus lateralized to the right (
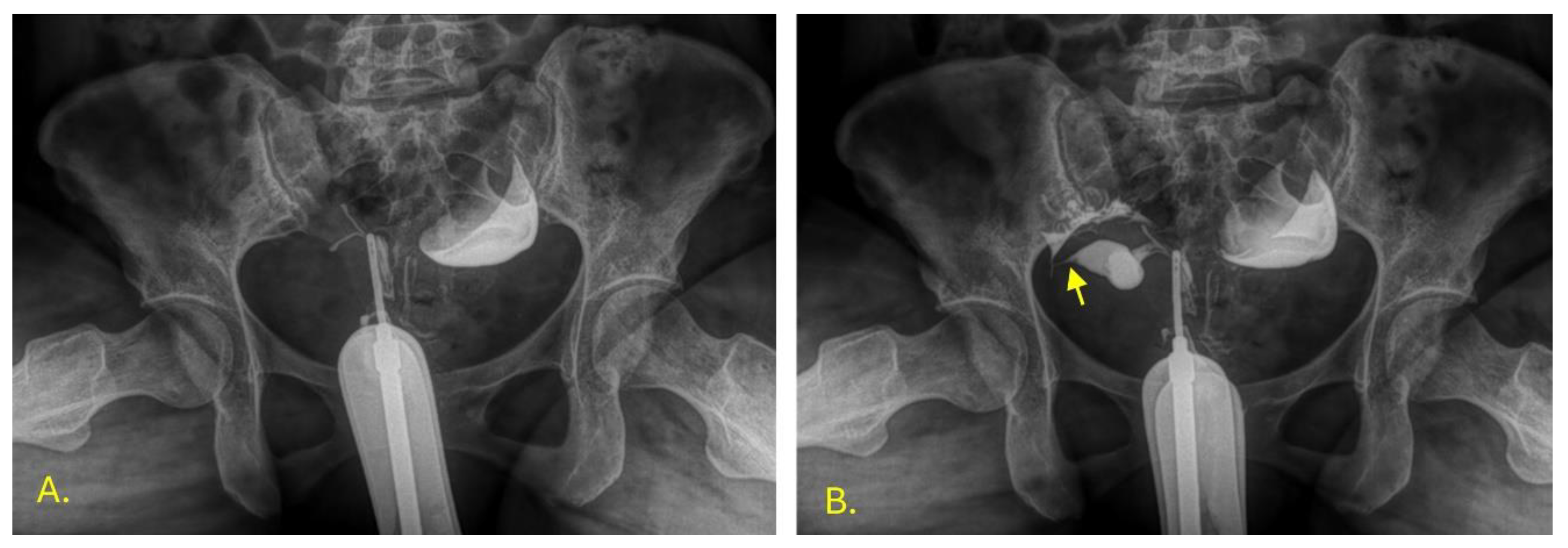
Figure 5).
Figure 5.
Right hysterosalpingography. Image A: Jarcho cannula in the right uterus. Image B: Contrast medium is instilled, revealing the endometrial cavity and part of the right fallopian tube (indicated by an arrow).
Figure 5.
Right hysterosalpingography. Image A: Jarcho cannula in the right uterus. Image B: Contrast medium is instilled, revealing the endometrial cavity and part of the right fallopian tube (indicated by an arrow).
Imaging revealed uterine didelphys bicollis and uterine myomatosis. The patient continues to be monitored by the gynecology department.
3. Discussion
The Müllerian ducts are vital structures during the development of the female reproductive system; however, they are present in both sexes. During embryonic development, the Müllerian ducts go through three phases: initiation, invagination, and elongation. In men, these ducts degenerate due to anti-Müllerian hormone; in women, in its absence, they fuse in their medial and distal portions, giving rise to the uterus and the upper portion of the vagina. Subsequently, complete resorption of the medial septum results in a single uterine cavity [
3]. When this fusion and resorption process fails, the uterus didelphys bicollis arises.
Uterus didelphys bicollis refers to the presence of two separate, non-communicating uterine horns, each with its own cervix and fallopian tube [
4]. There is usually only one vagina, although in some cases it may be accompanied by a longitudinal septum [
2]. According to the American Fertility Society (AFS) classification, “Classification of Müllerian duct malformations,” the didelphys uterus belongs to class III [
5].
Among the main complications associated with didelphys uterus are spontaneous abortions in up to 21% of cases, premature births in 24%, intrauterine growth retardation and perinatal mortality in 11%, and cesarean sections in up to 84% [
6]. However, our patient had no obstetric or reproductive history, and the finding was incidental during imaging studies requested for AUB and complications from IUD insertion.
The clinical presentation is usually nonspecific; most patients are asymptomatic, but some present with dyspareunia. During a gynecological examination, a longitudinal vaginal septum can be seen [
6].
Ultrasound, hysterosalpingography, magnetic resonance imaging, hysteroscopy, and diagnostic laparoscopy are tools that guide the diagnosis of uterine malformations, and the findings can guide medical management [
7,
8].
The coexistence of uterus didelphys with uterine myomatosis is extremely rare. Most available reports conclude a diagnosis incidentally after surgical interventions such as cesarean section or hysterectomy [
9,
10,
11,
12]. In contrast, in this case report, uterus didelphys was identified noninvasively through imaging studies [
9,
10,
11,
12,
13]. This fact highlights the importance of imaging as an early diagnostic tool that can guide clinical decisions without the need for surgical procedures.
4. Conclusions
Uterus didelphys bicollis is a type of Müllerian duct malformation. Despite being a relatively rare finding, it represents a significant cause of infertility and miscarriage, as well as adverse reproductive outcomes. However, compared to pregnancies associated with other uterine anomalies, the prognosis for pregnancies in patients with uterus didelphys is more favorable.
Its association with uterine myomatosis can increase diagnostic and therapeutic complexity, since fibroids themselves cause abnormal uterine bleeding and infertility, and when combined with a congenital uterine malformation, the impact on fertility and obstetric outcomes can be even greater [
13].
Imaging studies, particularly ultrasound and hysterosalpingography, are essential for a timely noninvasive diagnosis. Multidisciplinary follow-up can improve reproductive prognosis and reduce complications.
Author Contributions
Conceptualization, R. B. C.; methodology, R. B. C. and M. V. J. B.; validation, R. B. C. and M. V. J . B.; formal analysis, M. V. J. B.; investigation, Y. C. J.; writing—original draft preparation, Y. C. J..; writing—review and editing, M. V. J. B., M. M. C. H. and M. E. G. C.; supervision, R. B. C. and O. R. P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Wilson D, Bordoni B. Embryology, Mullerian Ducts (Paramesonephric Ducts) [Updated 2023 Mar 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557727/.
- Zamboni M, Pomés C, Celle CA, Rivera CA. Malformaciones müllerianas: actualización y revisión a propósito de casos clínicos. Rev Chil Obstet Ginecol. 2023;88(4):237-47. [CrossRef]
- 3. Etskovitz, Haley; Nandivada, Prathima; Hsi Dickie, Belinda. Mullerian and vaginal anomalies. Current Opinion in Pediatrics 36(6):p 710-719, December 2024. [CrossRef]
- Dixit, R., Duggireddy, CS y Pradhan, GS. Anomalías müllerianas: revisión de la imagenología y la clasificación. Insights Imaging 16 , 40 (2025). [CrossRef]
- Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. Mullerian duct anomalies: from diagnosis to intervention. Br J Radiol. 2009 Dec;82(984):1034-42. Epub 2009 May 11. PMID: 19433480; PMCID: PMC3473390. [CrossRef]
- López-Olmos J, Vizuete del Río J. Útero didelfo, bicollis y tabique vaginal longitudinal, causa de aborto habitual. Clín Investig Ginecol Obstet. 2014;41(3):134-7. [CrossRef]
- Eggermont J, Hummelshoj L, Fauser BCJM. Twenty-five years after the first case: uterine didelphys, fibroids, and reproductive outcomes. Fertil Steril. 2007;87(2):345-349.
- de Mattos Pinto e Passos I, Lopes Britto R. Diagnosis and treatment of müllerian malformations. Taiwan J Obstet Gynecol. 2020;59(2):183-8. Available from: https://www.sciencedirect.com/science/article/pii/S1028455920300036. [CrossRef]
- Ali MK, Abdelbadee AY, Shazly SA, Abbas MA. Uterus didelphys with multiple fibroids: a case report. Proc Obstet Gynecol. 2013;3(2):3 [4 p.]. Available from: https://pubs.lib.uiowa.edu/pog/article/id/3842/. [CrossRef]
- Mashala JN, Wekesa D, Chemwey R, Pulei A, Kihara A. An incidental case of uterus didelphys and fibroids: right sided myomectomy and left hemi-hysterectomy. Anat J Afr. 2020;9(2):1762-4. [CrossRef]
- Longoria K, Bennett D, Rizk B. Obstetric outcome of a primagravida with a uterine didelphys, a 20 cm fibroid, and a vaginal septum. Proc Obstet Gynecol. [Internet]. (fecha no indicada);3(2) [citado 2025 sep 22]. Disponible en: https://journals.ekb.eg/article_19526_1b8d80ab74d02b4598142ea79f131bdd.pdf. [CrossRef]
- Mullen MM, Kuroki LM, Hunt SR, Ratkowski KL, Mutch DG. A Transperineal Approach to Hysterectomy of a Retained Didelphic Uterine Horn. Obstet Gynecol. 2017 Sep;130(3):561-564. PMID: 28796686. [CrossRef]
- Defran AJ, Forestier C, Morgan E, Thomas M. Uterine Leiomyoma in the Context of Uterine Didelphys: A Case Report. Cureus. 2023 Sep 6;15(9):e44791. PMID: 37809224; PMCID: PMC10558276. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).