Submitted:
09 October 2025
Posted:
10 October 2025
You are already at the latest version
Abstract

Keywords:
1. Introduction
2. Results
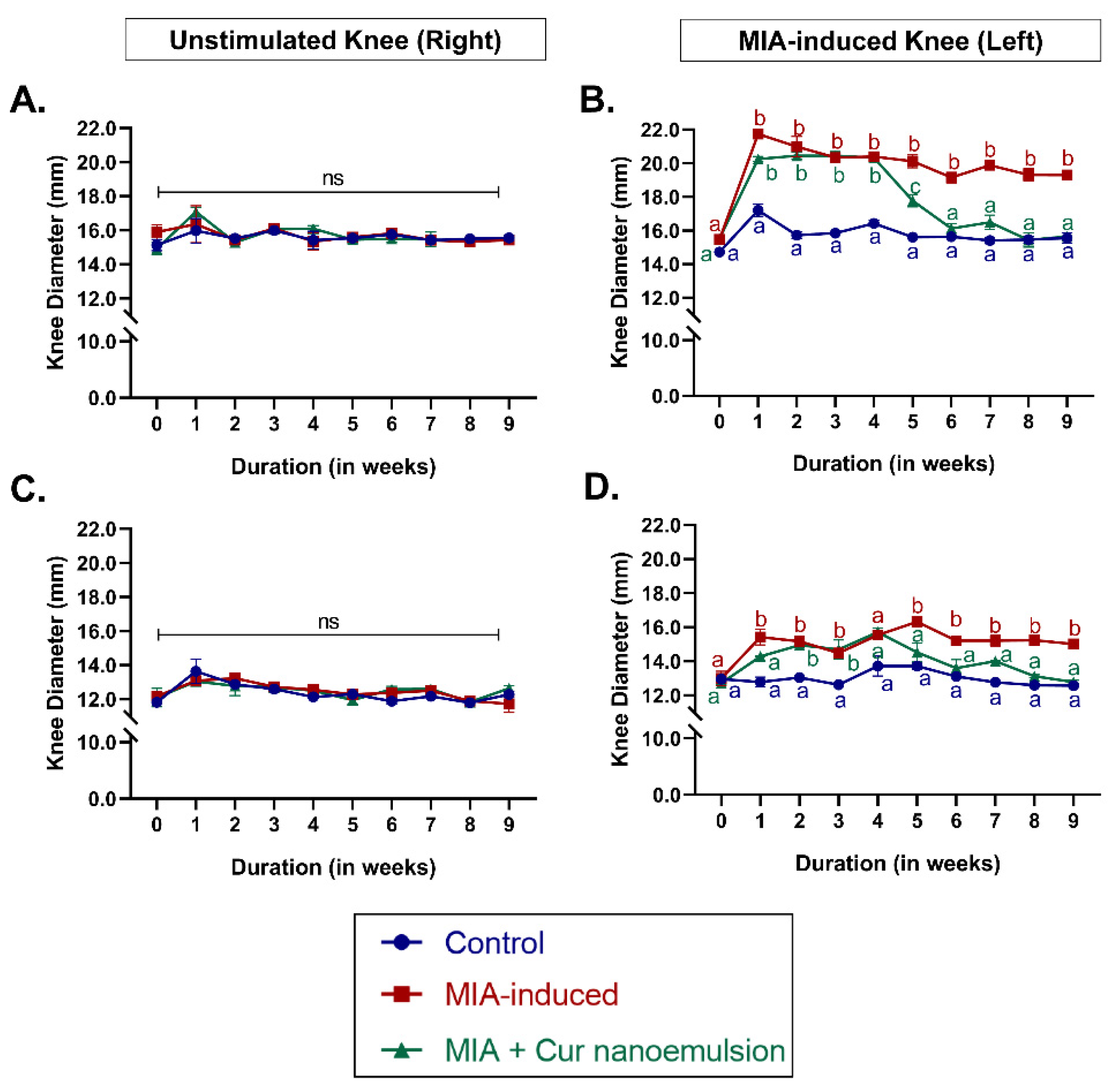
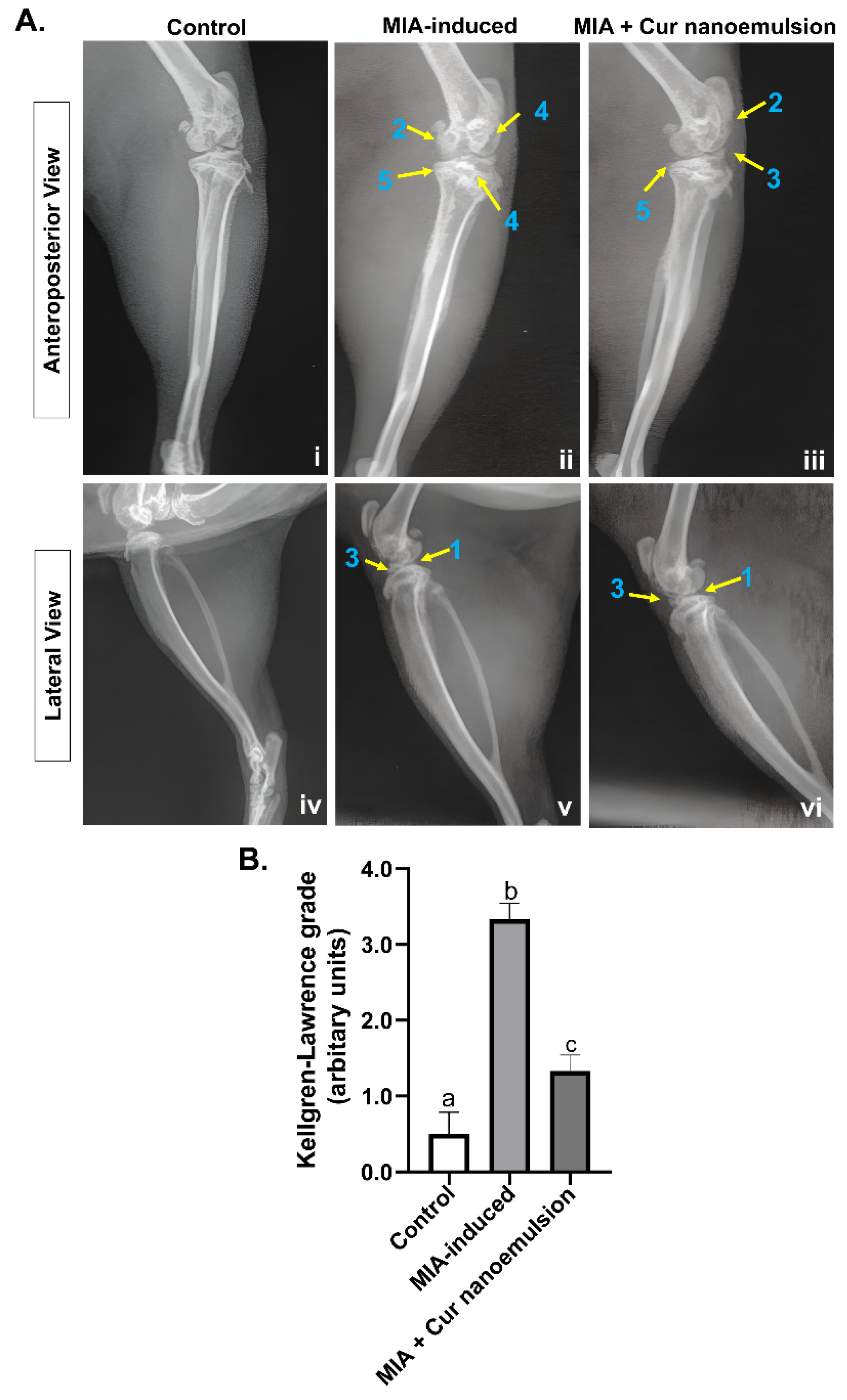
2.1. Curcumin Nanoemulsion Reduced MIA-Induced Knee Joint Edema and Articular Cavity Stenosis in Osteoarthritic Rats
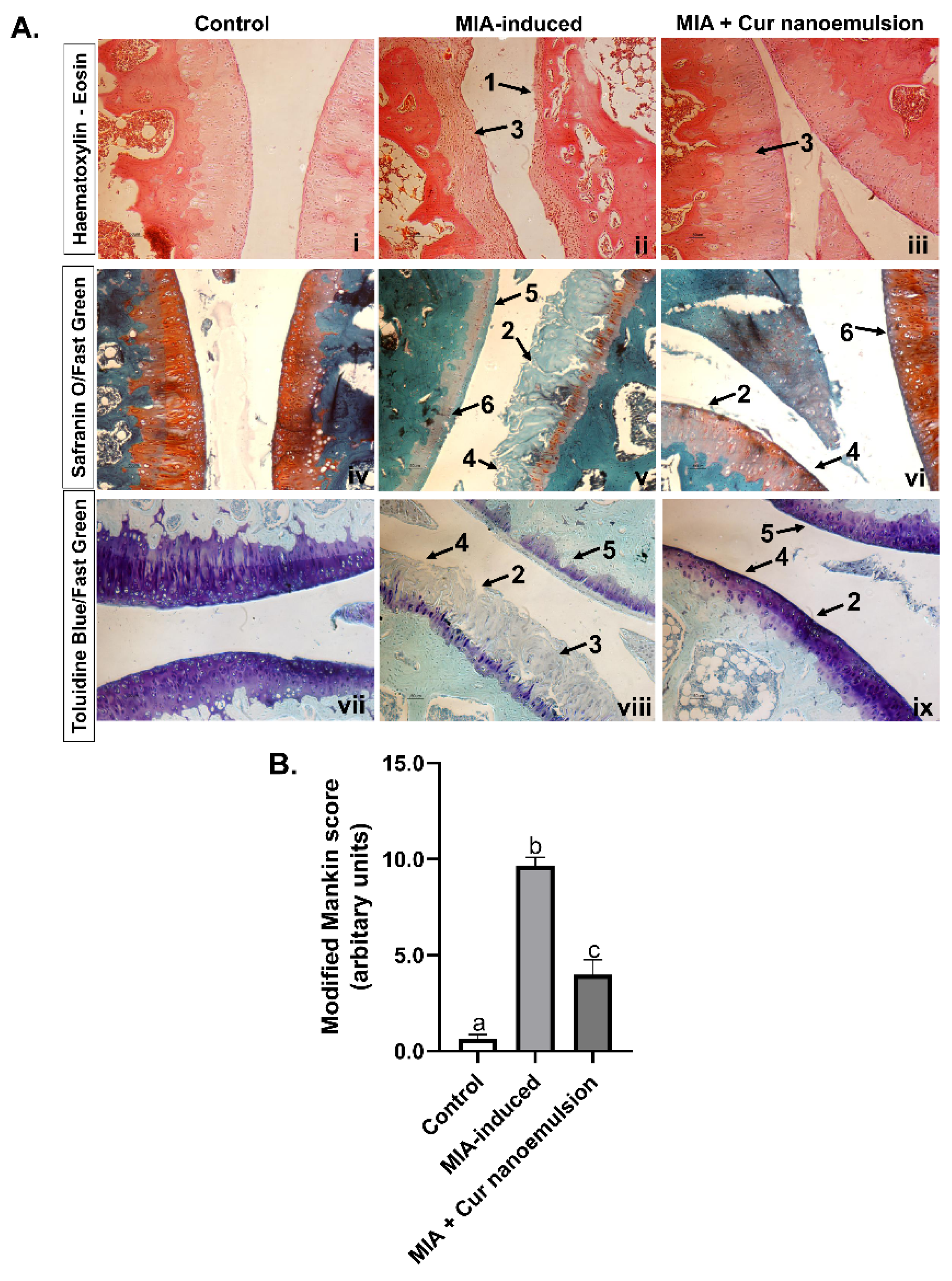
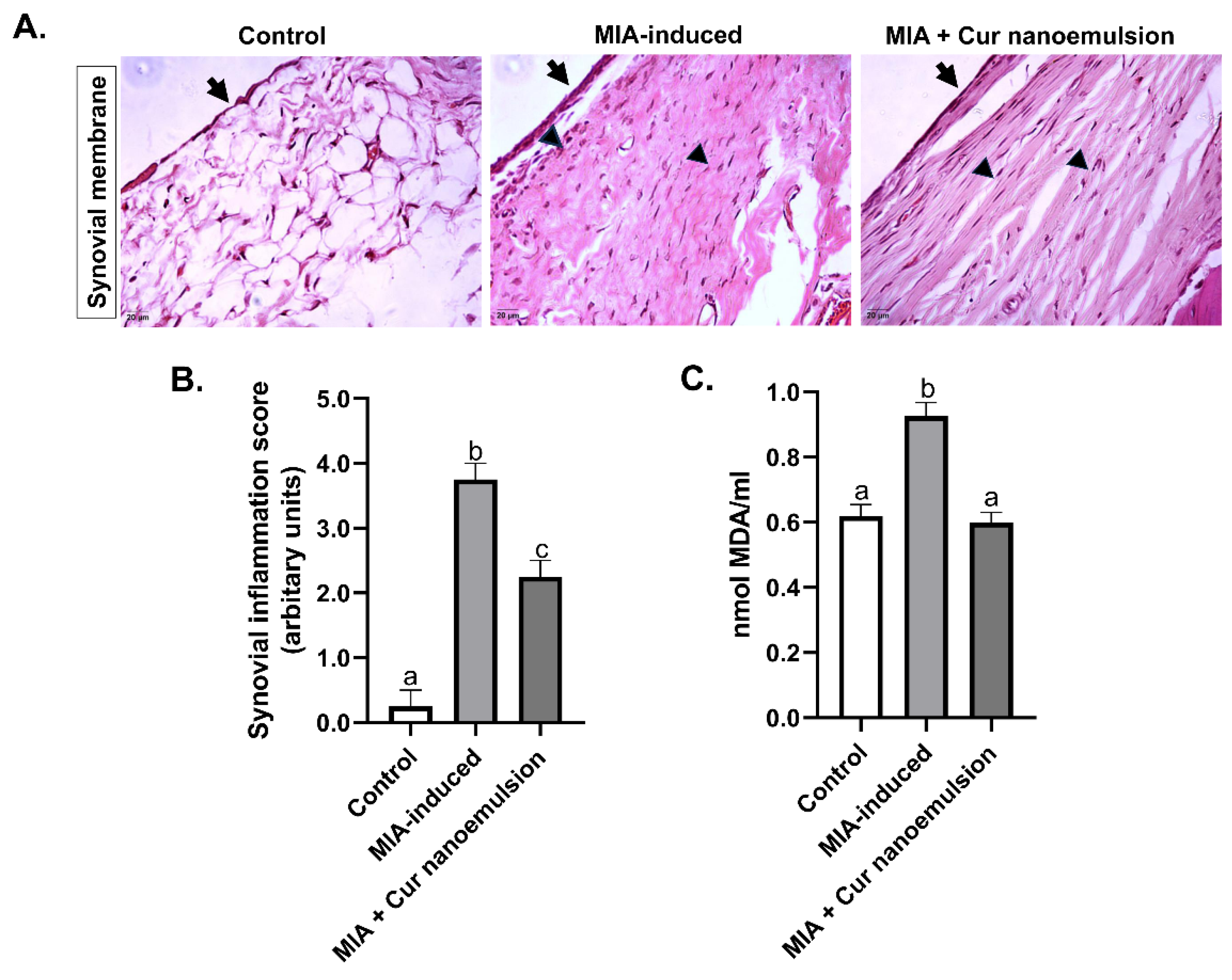
2.2. Curcumin Nanoemulsion Alleviated MIA-Induced Cartilage Fibrillation, Reduced Systemic Oxidative Stress, and Synovial Inflammation in the Knee Joint
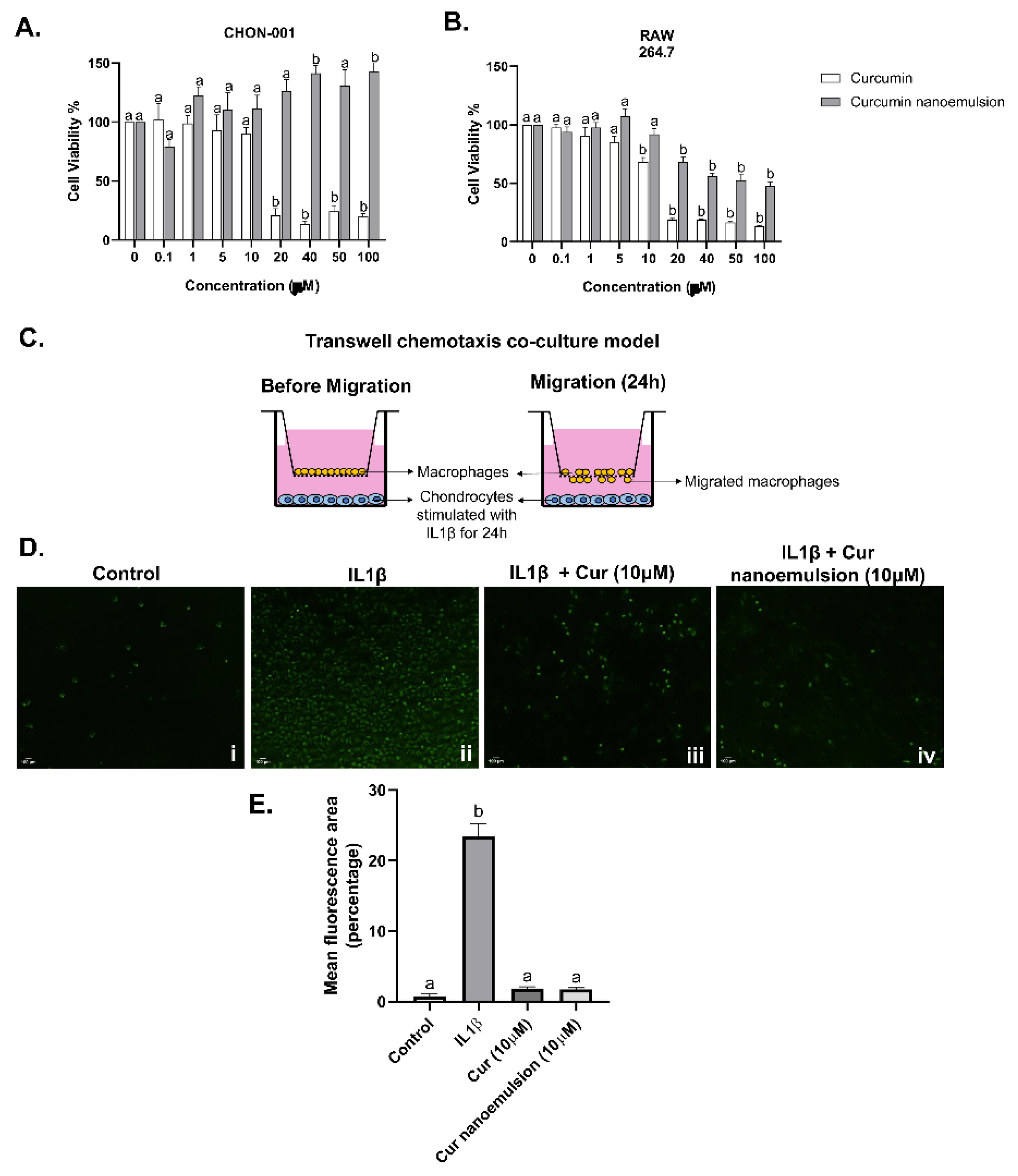
2.3. Curcumin Nanoemulsion Reduced In vitro Macrophage Migration Towards Chondrocytes in the Presence of IL1β
2.4. Modulation of Pro-Inflammatory Mediators and Matrix Regulators in Chondrocytes Exposed to Curcumin Nanoemulsion
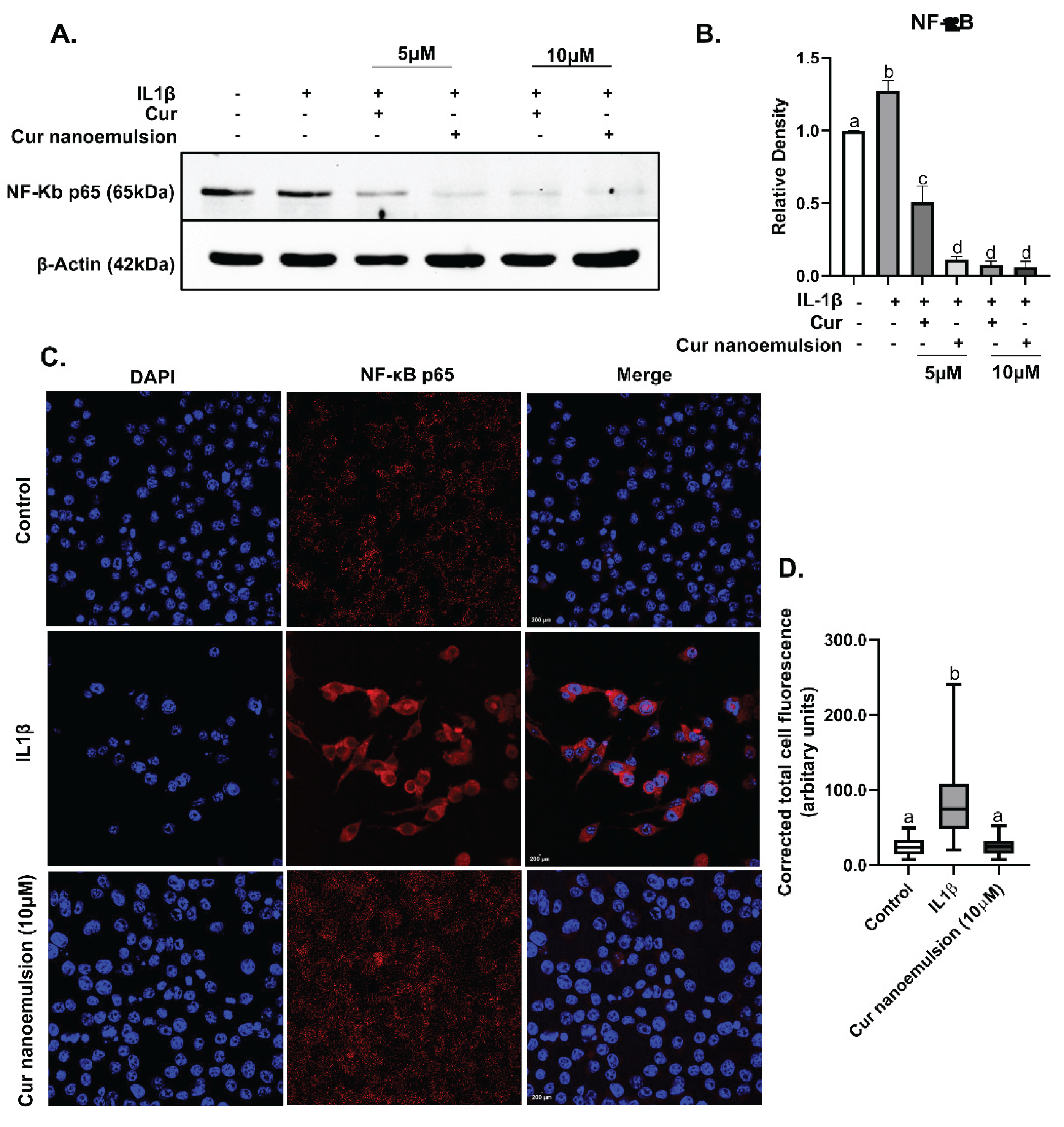
2.5. Curcumin Nanoemulsion Lowered IL1β-Induced Expression of NFκB in Macrophages (RAW264.7)
3. Discussion
4. Materials and Methods
4.1. Preparation of Nanoemulsion
4.2. Animal Experiment
4.3. X-ray Imaging and Scoring for Osteoarthritis
4.4. Knee Diameter Measurement
4.5. Collection of Blood and Knee Joints
4.6. Serum Oxidative Stress
4.7. Knee Joint Histology and Staining
4.8. Reagents and Cell Culture
4.9. Cell Viability by MTT Assay
4.10. Immunoblotting
4.11. Quantitative Real-Time PCR
4.12. Detection of NFκB Localization by Immunocytochemistry
4.13. Transwell Co-Culture Chemotaxis Assay
4.14. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gregori, D.; Giacovelli, G.; Minto, C.; Barbetta, B.; Gualtieri, F.; Azzolina, D.; Vaghi, P.; Rovati, L.C. Association of Pharmacological Treatments With Long-term Pain Control in Patients With Knee Osteoarthritis: A Systematic Review and Meta-analysis. Jama 2018, 320, 2564–2579. [Google Scholar] [CrossRef]
- Huang, H.; Lou, Z.; Zheng, S.; Wu, J.; Yao, Q.; Chen, R.; Kou, L.; Chen, D. Intra-articular drug delivery systems for osteoarthritis therapy: shifting from sustained release to enhancing penetration into cartilage. Drug delivery 2022, 29, 767–791. [Google Scholar] [CrossRef]
- Cao, Y.; Ma, Y.; Tao, Y.; Lin, W.; Wang, P. Intra-Articular Drug Delivery for Osteoarthritis Treatment. Pharmaceutics 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Naveen, S.V.; Ahmad, R.E.; Hui, W.J.; Suhaeb, A.M.; Murali, M.R.; Shanmugam, R.; Kamarul, T. Histology, glycosaminoglycan level and cartilage stiffness in monoiodoacetate-induced osteoarthritis: comparative analysis with anterior cruciate ligament transection in rat model and human osteoarthritis. International journal of medical sciences 2014, 11, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.; Nam, D.; Kim, J. Pathological Characteristics of Monosodium Iodoacetate-Induced Osteoarthritis in Rats. Tissue engineering and regenerative medicine 2023, 20, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Guzman, R.E.; Evans, M.G.; Bove, S.; Morenko, B.; Kilgore, K. Mono-iodoacetate-induced histologic changes in subchondral bone and articular cartilage of rat femorotibial joints: an animal model of osteoarthritis. Toxicologic pathology 2003, 31, 619–624. [Google Scholar] [CrossRef]
- Li, J.; Gui, T.; Yao, L.; Guo, H.; Lin, Y.L.; Lu, J.; Duffy, M.; Zgonis, M.; Mauck, R.; Dyment, N.; et al. Synovium and infrapatellar fat pad share common mesenchymal progenitors and undergo coordinated changes in osteoarthritis. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research 2024, 39, 161–176. [Google Scholar] [CrossRef]
- Lewallen, E.A.; Bonin, C.A.; Li, X.; Smith, J.; Karperien, M.; Larson, A.N.; Lewallen, D.G.; Cool, S.M.; Westendorf, J.J.; Krych, A.J.; et al. The synovial microenvironment of osteoarthritic joints alters RNA-seq expression profiles of human primary articular chondrocytes. Gene 2016, 591, 456–464. [Google Scholar] [CrossRef]
- Ostojic, M.; Zevrnja, A.; Vukojevic, K.; Soljic, V. Immunofluorescence Analysis of NF-kB and iNOS Expression in Different Cell Populations during Early and Advanced Knee Osteoarthritis. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef]
- Choi, M.C.; Jo, J.; Park, J.; Kang, H.K.; Park, Y. NF-κB Signaling Pathways in Osteoarthritic Cartilage Destruction. Cells 2019, 8. [Google Scholar] [CrossRef]
- Wu, S.; Morrison, A.; Sun, H.; De Luca, F. Nuclear factor-kappaB (NF-kappaB) p65 interacts with Stat5b in growth plate chondrocytes and mediates the effects of growth hormone on chondrogenesis and on the expression of insulin-like growth factor-1 and bone morphogenetic protein-2. The Journal of biological chemistry 2011, 286, 24726–24734. [Google Scholar] [CrossRef]
- Caron, M.M.; Emans, P.J.; Surtel, D.A.; Cremers, A.; Voncken, J.W.; Welting, T.J.; van Rhijn, L.W. Activation of NF-κB/p65 facilitates early chondrogenic differentiation during endochondral ossification. PLoS One 2012, 7, e33467. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Bhutani, N. Profiling joint tissues at single-cell resolution: advances and insights. Nature reviews. Rheumatology 2024, 20, 7–20. [Google Scholar] [CrossRef]
- Liu, Y.; Hao, R.; Lv, J.; Yuan, J.; Wang, X.; Xu, C.; Ma, D.; Duan, Z.; Zhang, B.; Dai, L.; et al. Targeted knockdown of PGAM5 in synovial macrophages efficiently alleviates osteoarthritis. Bone Res 2024, 12, 15. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.L.; Harasymowicz, N.S.; Klimak, M.A.; Collins, K.H.; Guilak, F. The role of macrophages in osteoarthritis and cartilage repair. Osteoarthritis and cartilage 2020, 28, 544–554. [Google Scholar] [CrossRef]
- Ummarino, A.; Gambaro, F.M.; Kon, E.; Torres Andón, F. Therapeutic Manipulation of Macrophages Using Nanotechnological Approaches for the Treatment of Osteoarthritis. Nanomaterials (Basel, Switzerland) 2020, 10. [Google Scholar] [CrossRef]
- Hamasaki, M.; Terkawi, M.A.; Onodera, T.; Homan, K.; Iwasaki, N. A Novel Cartilage Fragments Stimulation Model Revealed that Macrophage Inflammatory Response Causes an Upregulation of Catabolic Factors of Chondrocytes In Vitro. Cartilage 2021, 12, 354–361. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Kubota, K.; Asawa, Y.; Hoshi, K.; Hikita, A. M1-like macrophage contributes to chondrogenesis in vitro. Scientific Reports 2021, 11, 21307. [Google Scholar] [CrossRef]
- Olivotto, E.; Minguzzi, M.; D’Adamo, S.; Astolfi, A.; Santi, S.; Uguccioni, M.; Marcu, K.B.; Borzì, R.M. Basal and IL-1β enhanced chondrocyte chemotactic activity on monocytes are co-dependent on both IKKα and IKKβ NF-κB activating kinases. Scientific Reports 2021, 11, 21697. [Google Scholar] [CrossRef]
- Jin, Z.; Chang, B.; Wei, Y.; Yang, Y.; Zhang, H.; Liu, J.; Piao, L.; Bai, L. Curcumin exerts chondroprotective effects against osteoarthritis by promoting AMPK/PINK1/Parkin-mediated mitophagy. Biomed Pharmacother 2022, 151, 113092. [Google Scholar] [CrossRef] [PubMed]
- Csaki, C.; Mobasheri, A.; Shakibaei, M. Synergistic chondroprotective effects of curcumin and resveratrol in human articular chondrocytes: inhibition of IL-1beta-induced NF-kappaB-mediated inflammation and apoptosis. Arthritis Res Ther 2009, 11, R165–R165. [Google Scholar] [CrossRef]
- Basak, S.; Hridayanka, K.S.N.; Duttaroy, A.K. Bioactives and their roles in bone metabolism of osteoarthritis: evidence and mechanisms on gut-bone axis. Frontiers in Immunology 2024, 14. [Google Scholar] [CrossRef]
- Hridayanka, K.S.N.; Duttaroy, A.K.; Basak, S. Bioactive Compounds and Their Chondroprotective Effects for Osteoarthritis Amelioration: A Focus on Nanotherapeutic Strategies, Epigenetic Modifications, and Gut Microbiota. Nutrients 2024, 16. [Google Scholar] [CrossRef]
- Ratanavaraporn, J.; Soontornvipart, K.; Shuangshoti, S.; Shuangshoti, S.; Damrongsakkul, S. Localized delivery of curcumin from injectable gelatin/Thai silk fibroin microspheres for anti-inflammatory treatment of osteoarthritis in a rat model. Inflammopharmacology 2017, 25, 211–221. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, Z.; Wang, X.; Liang, J.; Zhao, L.; Zhang, Y.; Ren, J.; Zhang, S.; Liu, Y. A Core-Brush Nanoplatform with Enhanced Lubrication and Anti-Inflammatory Properties for Osteoarthritis Treatment. Advanced science (Weinheim, Baden-Wurttemberg, Germany) 2024, 11, e2406027. [Google Scholar] [CrossRef] [PubMed]
- Hamdalla, H.M.; Ahmed, R.R.; Galaly, S.R.; Naguib, I.A.; Alghamdi, B.S.; Ahmed, O.M.; Farghali, A.; Abdul-Hamid, M. Ameliorative Effect of Curcumin Nanoparticles against Monosodium Iodoacetate-Induced Knee Osteoarthritis in Rats. Mediators of inflammation 2022, 2022, 8353472. [Google Scholar] [CrossRef] [PubMed]
- El-Haddad, M.E.; El-Refaie, W.M.; Hammad, G.O.; El-Massik, M.A. Intra-articular metformin-curcumin cationic PLGA nanoparticles rejuvenate articular structure in MIA induced osteoarthritis model via modulating the crosstalk between miR93, TNFAIP3/TLR/NF-κB and AMPK/SIRT1 trajectories. International journal of biological macromolecules 2025, 315, 144482. [Google Scholar] [CrossRef]
- Xiong, Y.; Mi, B.B.; Shahbazi, M.A.; Xia, T.; Xiao, J. Microenvironment-responsive nanomedicines: a promising direction for tissue regeneration. Military Medical Research 2024, 11, 69. [Google Scholar] [CrossRef]
- Yabas, M.; Orhan, C.; Er, B.; Tuzcu, M.; Durmus, A.S.; Ozercan, I.H.; Sahin, N.; Bhanuse, P.; Morde, A.A.; Padigaru, M.; et al. A Next Generation Formulation of Curcumin Ameliorates Experimentally Induced Osteoarthritis in Rats via Regulation of Inflammatory Mediators. Front Immunol 2021, 12, 609629. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Lee, C.K.; Song, S.H.; Yun, J.H.; Lee, A.; Park, H.J. Highly bioavailable curcumin powder suppresses articular cartilage damage in rats with mono-iodoacetate (MIA)-induced osteoarthritis. Food Sci Biotechnol 2020, 29, 251–263. [Google Scholar] [CrossRef]
- Mimpen, J.Y.; Hedley, R.; Ridley, A.; Baldwin, M.J.; Windell, D.; Bhalla, A.; Ramos-Mucci, L.; Buckley, C.D.; Coles, M.C.; Alvand, A.; et al. Cellular characterisation of advanced osteoarthritis knee synovium. Arthritis Res Ther 2023, 25, 154. [Google Scholar] [CrossRef] [PubMed]
- Roebuck, M.M.; Jamal, J.; Lane, B.; Wood, A.; Santini, A.; Wong, P.F.; Bou-Gharios, G.; Frostick, S.P. Cartilage debris and osteoarthritis risk factors influence gene expression in the synovium in end stage osteoarthritis. The Knee 2022, 37, 47–59. [Google Scholar] [CrossRef]
- Chou, C.H.; Jain, V.; Gibson, J.; Attarian, D.E.; Haraden, C.A.; Yohn, C.B.; Laberge, R.M.; Gregory, S.; Kraus, V.B. Synovial cell cross-talk with cartilage plays a major role in the pathogenesis of osteoarthritis. Sci Rep 2020, 10, 10868. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.H.; Ghosh, D.; Attari, S.; Ude, C.C.; Laurencin, C.T. Animal Models of Osteoarthritis: Updated Models and Outcome Measures 2016-2023. Regenerative engineering and translational medicine 2024, 10, 127–146. [Google Scholar] [CrossRef]
- Takahashi, I.; Ikeshima, K.; Matsuzaki, T.; Hoso, M. Histopathological changes in joint capsule and synovial membrane in a rat model of osteoarthritis. Osteoarthritis and cartilage 2016, 24, S398. [Google Scholar] [CrossRef]
- Holzer, L.A.; Kraiger, M.; Talakic, E.; Fritz, G.A.; Avian, A.; Hofmeister, A.; Leithner, A.; Holzer, G. Microstructural analysis of subchondral bone in knee osteoarthritis. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2020, 31, 2037–2045. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Liu, G.; Yan, J.; Zhang, Q.; Meng, F.; Wang, L. Curcumin alleviates osteoarthritis in mice by suppressing osteoclastogenesis in subchondral bone via inhibiting NF-κB/JNK signaling pathway. PLoS One 2024, 19, e0309807. [Google Scholar] [CrossRef]
- Nwosu, L.N.; Mapp, P.I.; Chapman, V.; Walsh, D.A. Relationship between structural pathology and pain behaviour in a model of osteoarthritis (OA). Osteoarthritis and cartilage 2016, 24, 1910–1917. [Google Scholar] [CrossRef]
- Mende, L.K.; Kuthati, Y.; Wong, C.S. Curcumin and Vitamin D Supplement Attenuates Knee Osteoarthritis Progression in ACLT + MMx Rat Model: Effect on Cartilage Protection and Pain Reduction. Nutrients 2025, 17. [Google Scholar] [CrossRef]
- Jhun, J.; Lee, D.; Na, H.S.; Cho, K.H.; Lee, S.Y.; Lee, J.S.; Lee, Y.J.; Kim, S.J.; Park, S.H.; Cho, M.L. Curcumin and omega-3 ameliorate experimental osteoarthritis progression in terms of joint pain and mitochondrial dysfunction. Journal of inflammation (London, England) 2025, 22, 27. [Google Scholar] [CrossRef]
- Altindag, O.; Erel, O.; Aksoy, N.; Selek, S.; Celik, H.; Karaoglanoglu, M. Increased oxidative stress and its relation with collagen metabolism in knee osteoarthritis. Rheumatology international 2007, 27, 339–344. [Google Scholar] [CrossRef]
- Chen, B.; He, Q.; Chen, C.; Lin, Y.; Xiao, J.; Pan, Z.; Li, M.; Li, S.; Yang, J.; Wang, F.; et al. Combination of curcumin and catalase protects against chondrocyte injury and knee osteoarthritis progression by suppressing oxidative stress. Biomed Pharmacother 2023, 168, 115751. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Zhu, Y.; Wei, K.; Pu, H.; Peng, R.; Xiao, J.; Liu, C.; Sun, X. Metformin Attenuates the Inflammatory Response via the Regulation of Synovial M1 Macrophage in Osteoarthritis. Int J Mol Sci 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, Z.; Chen, C.; Wei, W.; Li, Z.; Zhou, H.; He, W.; Xia, J.; Li, B.; Yang, Y. SRGN promotes macrophage recruitment through CCL3 in osteoarthritis. Connective tissue research 2024, 65, 330–342. [Google Scholar] [CrossRef]
- Sasaki, Y.; Kijima, K.; Yoshioka, K. Validity evaluation of a rat model of monoiodoacetate-induced osteoarthritis with clinically effective drugs. BMC musculoskeletal disorders 2024, 25, 975. [Google Scholar] [CrossRef] [PubMed]
- Bryk, M.; Chwastek, J.; Mlost, J.; Kostrzewa, M.; Starowicz, K. Sodium Monoiodoacetate Dose-Dependent Changes in Matrix Metalloproteinases and Inflammatory Components as Prognostic Factors for the Progression of Osteoarthritis. Front Pharmacol 2021, 12, 643605. [Google Scholar] [CrossRef]
- van Beuningen, H.M.; van der Kraan, P.M.; Arntz, O.J.; van den Berg, W.B. Transforming growth factor-beta 1 stimulates articular chondrocyte proteoglycan synthesis and induces osteophyte formation in the murine knee joint. Laboratory investigation; a journal of technical methods and pathology 1994, 71, 279–290. [Google Scholar]
- Yang, X.; Chen, L.; Xu, X.; Li, C.; Huang, C.; Deng, C.X. TGF-beta/Smad3 signals repress chondrocyte hypertrophic differentiation and are required for maintaining articular cartilage. The Journal of cell biology 2001, 153, 35–46. [Google Scholar] [CrossRef]
- Zhou, Y.; Ming, J.; Deng, M.; Li, Y.; Li, B.; Li, J.; Ma, Y.; Chen, Z.; Wang, G.; Liu, S. Chemically modified curcumin (CMC2.24) alleviates osteoarthritis progression by restoring cartilage homeostasis and inhibiting chondrocyte apoptosis via the NF-κB/HIF-2α axis. Journal of molecular medicine (Berlin, Germany) 2020, 98, 1479–1491. [Google Scholar] [CrossRef]
- Clutterbuck, A.L.; Mobasheri, A.; Shakibaei, M.; Allaway, D.; Harris, P. Interleukin-1beta-induced extracellular matrix degradation and glycosaminoglycan release is inhibited by curcumin in an explant model of cartilage inflammation. Ann N Y Acad Sci 2009, 1171, 428–435. [Google Scholar] [CrossRef]
- Wu, M.; Wu, S.; Chen, W.; Li, Y.-P. The roles and regulatory mechanisms of TGF-β and BMP signaling in bone and cartilage development, homeostasis and disease. Cell Research 2024, 34, 101–123. [Google Scholar] [CrossRef]
- Luyten, F.P.; Yu, Y.M.; Yanagishita, M.; Vukicevic, S.; Hammonds, R.G.; Reddi, A.H. Natural bovine osteogenin and recombinant human bone morphogenetic protein-2B are equipotent in the maintenance of proteoglycans in bovine articular cartilage explant cultures. The Journal of biological chemistry 1992, 267, 3691–3695. [Google Scholar] [CrossRef]
- Lee, H.; Kim, H.; Seo, J.; Choi, K.; Lee, Y.; Park, K.; Kim, S.; Mobasheri, A.; Choi, H. TissueGene-C promotes an anti-inflammatory micro-environment in a rat monoiodoacetate model of osteoarthritis via polarization of M2 macrophages leading to pain relief and structural improvement. Inflammopharmacology 2020, 28, 1237–1252. [Google Scholar] [CrossRef]
- Lin, S.; Li, H.; Wu, B.; Shang, J.; Jiang, N.; Peng, R.; Xing, B.; Xu, X.; Lu, H. TGF-β1 regulates chondrocyte proliferation and extracellular matrix synthesis via circPhf21a-Vegfa axis in osteoarthritis. Cell Communication and Signaling 2022, 20, 75. [Google Scholar] [CrossRef] [PubMed]
- Xia, X.D.; Gill, G.; Lin, H.; Roth, D.M.; Gu, H.M.; Wang, X.J.; Su, F.Y.; Alabi, A.; Alexiou, M.; Zhang, Z.; et al. Global, but not chondrocyte-specific, MT1-MMP deficiency in adult mice causes inflammatory arthritis. Matrix biology : journal of the International Society for Matrix Biology 2023, 122, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B.; Xu, X.; Yi, P.; Hao, Y. Curcumin reinforces MSC-derived exosomes in attenuating osteoarthritis via modulating the miR-124/NF-kB and miR-143/ROCK1/TLR9 signalling pathways. J Cell Mol Med 2020, 24, 10855–10865. [Google Scholar] [CrossRef] [PubMed]
- Schulze-Tanzil, G.; Mobasheri, A.; Sendzik, J.; John, T.; Shakibaei, M. Effects of curcumin (diferuloylmethane) on nuclear factor kappaB signaling in interleukin-1beta-stimulated chondrocytes. Ann N Y Acad Sci 2004, 1030, 578–586. [Google Scholar] [CrossRef]
- Yang, Q.; Wu, S.; Mao, X.; Wang, W.; Tai, H. Inhibition effect of curcumin on TNF-α and MMP-13 expression induced by advanced glycation end products in chondrocytes. Pharmacology 2013, 91, 77–85. [Google Scholar] [CrossRef]
- Buhrmann, C.; Brockmueller, A.; Mueller, A.-L.; Shayan, P.; Shakibaei, M. Curcumin Attenuates Environment-Derived Osteoarthritis by Sox9/NF-kB Signaling Axis. International journal of molecular sciences 2021, 22, 7645. [Google Scholar] [CrossRef]
- Pitcher, T.; Sousa-Valente, J.; Malcangio, M. The Monoiodoacetate Model of Osteoarthritis Pain in the Mouse. JoVE 2016, e53746. [Google Scholar] [CrossRef]
- Nakahata, A.; Ito, A.; Nakahara, R.; Kishimoto, A.; Imaizumi, A.; Hashimoto, T.; Mukai, S.; Nakagawa, Y.; Kuroki, H. Intra-Articular Injections of Curcumin Monoglucuronide TBP1901 Suppresses Articular Cartilage Damage and Regulates Subchondral Bone Alteration in an Osteoarthritis Rat Model. Cartilage 2021, 13, 153s–167s. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clinical orthopaedics and related research 2016, 474, 1886–1893. [Google Scholar] [CrossRef]
- Horváth Á, I.; Bölcskei, K.; Szentes, N.; Borbély, É.; Tékus, V.; Botz, B.; Rusznák, K.; Futácsi, A.; Czéh, B.; Mátyus, P.; et al. Novel multitarget analgesic candidate SZV-1287 demonstrates potential disease-modifying effects in the monoiodoacetate-induced osteoarthritis mouse model. Front Pharmacol 2024, 15, 1377081. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, N.; Bendele, A.M.; Glasson, S.; Carlson, C.S. The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the rat. Osteoarthritis and cartilage 2010, 18 Suppl 3, S24–34. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, N.; Laverty, S.; Kraus, V.B.; Aigner, T. Basic methods in histopathology of joint tissues. Osteoarthritis and cartilage 2010, 18 Suppl 3, S113–116. [Google Scholar] [CrossRef] [PubMed]
- Mankin, H.J.; Dorfman, H.; Lippiello, L.; Zarins, A. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. II. Correlation of morphology with biochemical and metabolic data. The Journal of bone and joint surgery. American volume 1971, 53, 523–537. [Google Scholar]
- Takahashi, I.; Matsuzaki, T.; Kuroki, H.; Hoso, M. Joint unloading inhibits articular cartilage degeneration in knee joints of a monosodium iodoacetate-induced rat model of osteoarthritis. Osteoarthritis and cartilage 2019, 27, 1084–1093. [Google Scholar] [CrossRef]
- Varma, S.; Molangiri, A.; Mudavath, S.; Ananthan, R.; Rajanna, A.; Duttaroy, A.K.; Basak, S. Exposure to BPA and BPS during pregnancy disrupts the bone mineralization in the offspring. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 2024, 189, 114772. [Google Scholar] [CrossRef]
- Venter, C.; Niesler, C.U. Rapid quantification of cellular proliferation and migration using ImageJ. BioTechniques 2019, 66, 99–102. [Google Scholar] [CrossRef]
| Type of Gene | Gene Symbol | Control (Unstimulated) | IL1β (10ng/mL) | IL1β + Cur (10μM) | IL1β + Cur- Nanoemulsion (10μM) |
| Inflammatory modulators | |||||
| NFκB | 1.01 ± 0.04a | 4.41 ± 0.67b | 2.37 ± 0.05c | 2.47 ± 0.07c | |
| NFκB-IB | 1.01 ± 0.06a | 2.28 ± 0.32b | 3.14 ± 0.33b | 3.58 ± 0.22bc | |
| TNFα | 1.01 ± 0.04a | 1.65 ± 0.11b | 0.90 ± 0.03a | 0.97 ± 0.09a | |
| Matrix regulators | |||||
| TGFβ1 | 1.01 ± 0.02a | 0.57 ± 0.03b | 1.35 ± 0.06a | 1.24 ± 0.17a | |
| BMP2 | 1.01 ± 0.05a | 8.61 ± 2.29b | 12.78 ± 1.07b | 13.64 ± 1.31b | |
| SMAD1 | 1.01 ± 0.04a | 0.95 ± 0.05a | 2.20 ± 0.07b | 1.40 ± 0.08c | |
| SMAD5 | 1.01 ± 0.02a | 0.70 ± 0.22a | 0.52 ± 0.02a | 0.32 ± 0.02ab | |
| SPARC | 1.01 ± 0.02a | 0.39 ± 0.13b | 0.13 ± 0.01b | 0.18 ± 0.01b | |
| MMP2 | 1.01 ± 0.01a | 1.57 ± 0.10b | 1.56 ± 0.07b | 1.44 ± 0.18b | |
| MMP9 | 1.01 ± 0.02a | 1.94 ± 0.49b | 0.93 ± 0.16a | 1.94 ± 0.13b | |
| MMP14 | 1.01 ± 0.02a | 0.84 ± 0.23a | 1.52 ± 0.09b | 1.47 ± 0.04ab | |
| TIMP1 | 1.01 ± 0.03a | 1.98 ± 0.32b | 2.08 ± 0.18b | 2.53 ± 0.16b | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





