1. Introduction
Negative attitudes towards mental health problems (ATMHP), often termed mental health stigma, continue to pose a major barrier to seeking psychological support, especially in low- and middle-income countries [
1,
2,
3,
4,
5,
6,
7,
8,
9]. Negative attitudes are common even among caregivers and emerging medical professionals [
10,
11,
12,
13,
14,
15]. Despite growing awareness, mental illness continues to be perceived through a lens of shame, fear, and social exclusion, often rooted in cultural beliefs [
16,
17]. Such negative attitude is compounded by societal norms that associate mental health issues with personal weakness or spiritual failings, leading to discrimination and marginalization of affected individuals [
18,
19,
20,
21]. Therefore, measuring ATMHP is crucial, as it significantly contributes to stigma reduction and ensures better mental health care—especially in the context of Nepal, a lower-middle-income country where such mental health shame remains pervasive [
2,
5,
6,
7,
8,
22,
23,
24].
1.1. Measuring ATMHP
There are well developed measurement scales to measure attitudes of community people towards mental health issues. “Attitudes Towards Mental Health Problems (ATMHP)” developed by Gilbert et al. (2007) offers a comprehensive framework for assessing such attitudes, encompassing dimensions like internal and external shame, and reflected shame [
16]. In the Portuguese validation study of the ATMHP, the original model showed poor fit in confirmatory factor analysis (CFA), but an alternative model with an added factor demonstrated good model fit. Further analysis confirmed that the revised version had good psychometric properties, supporting its suitability for assessing attitudes toward mental illness in Portuguese-speaking populations [
25].
Later, studies have developed and validated a shorter 14-item shorter version of the ATMHPS (i.e., SATMHPS) that demonstrated good internal consistency and replicated the original seven-factor structure, providing a reliable and user-friendly tool to assess attitudes and shame toward mental health problems among UK university students [
26]. Similarly, a cross-cultural validation of the Japanese Short version of Attitudes Towards Mental Health Problems Scale (J-SATMHPS) demonstrated its reliable seven-factor structure and applicability in Japanese populations, highlighting cultural differences between the UK and Japan in external and internal shame related to mental health [
27]. The scale has already been used in measuring attitudes of college students in Nepal; however, the applicability of this scale in the Nepalese context has not been thoroughly examined [
6].
1.2. Conceptual Framework of ATMHP Scale
The development of the ATMHP scale was grounded in a rich body of cross-cultural and psychosocial research examining how cultural norms shape perceptions of mental health, shame, and stigma. Culture acts as a framework through which individuals interpret their experiences, including attitudes toward mental illness [
24,
28,
29]. Studies have emphasized obvious differences between Eastern and Western societies regarding the conceptualization of mental health, expectations of coping behaviors, and engagement with mental health services [
30,
31,
32]. Research with British South Asian women underscored the role of shame—particularly tied to cultural values such as izzat (family honor)—in deterring help-seeking and promoting silence around psychological distress [
33,
34,
35]. These findings informed the scale’s theoretical basis, incorporating dimensions of external shame (fear of social judgment), internal shame (self-criticism), and reflected shame (concern over bringing dishonor to one’s family) [
36,
37,
38]. These constructs provide a culturally sensitive framework for assessing attitudes toward mental health.
1.3. Study Gap
While studies have utilized the ATMHP scale in various cultural settings without formal validation [
6,
39,
40,
41], formal validation has been performed in Portugal [
25] and Japan [
27]. Additionally, it has been used in cross-cultural studies, comparing Arabs, South Asians, and others living in the United Arab Emirates [
42], British Caucasians and Arabians [
43], and British Asians and non-Asians [
16]. The Japanese shorter version of ATMHPS (J-SATMHPS) has been developed and validated in a collectivistic culture [
27]; however, there are no such validation studies in South Asian sub-continent, including Nepal. Although Poudel et al. (2024) reported high internal consistency (α = 0.94) and strong convergent validity (with Pearson correlation ranging from .66 to .86 between subscales and the global scale), a significant gap remains in the formal validation of the ATMHP scale within Nepal’s unique socio-cultural context [
6]. Without such validation, the applicability and accuracy of the scale in capturing culturally embedded attitudes – such as those influenced by shame, family honor, and spiritual beliefs – remain uncertain. Though Nepal is a culturally collectivistic society similar to Japan, it also differs from the Japanese cultural context due to a complex interplay of cultural factors. Therefore, it is essential to develop and validate a Nepalese Shorter version of ATMHPS (N-SATMHPS).
1.4. Study Aim
This study aims to validate the ATMHP scale in the cross-cultural context of Nepal, ensuring its reliability and relevance for assessing attitudes toward mental health problems among Nepali populations. By doing so, it seeks to provide a culturally sensitive tool that can inform interventions aimed at reducing stigma and promoting mental well-being in Nepal.
This study can contribute to the Nepalese mental health field by validating the ATMHP scale for use in Nepal. It ensures the tool’s cultural relevance and reliability in assessing negative attitudes rooted in societal shame, stigma, and family honor, which are prominent in Nepalese culture. By offering a validated, context-sensitive instrument, the study lays the groundwork for more effective stigma-reduction interventions and evidence-based mental health strategies tailored to the Nepalese population.
2. Materials and Methods
2.1. Research Design
Two different cross-sectional survey designs were utilized simultaneously to develop the Nepalese Short version of Attitudes Towards Mental Health Problems Scale (N-SATMHPS); evaluate the structural validity of the N-SATMHPS; and to assess the discriminant validity between the N-SATMHPS and Mental Health Literacy Young Adult (MHLQ–YA; Dias et al.,2018) [
44], including their respective dimensions. Dataset 1, from previous study by Poudel et al. (2024) [
6], was utilized to develop the scale, while Dataset 2 was used to evaluate the structure in a Confirmatory Factory Analysis (CFA).
2.2. Participants and Procedures
For Dataset 1, the required sample size was determined using Cochran’s formula for a population with an unknown proportion: n0 = (Z2pq)/e2, where n0 is the sample size, Z is the z-score for the desired confidence level, p is the estimated proportion of the population, q is 1 − p, and e is the desired level of precision (i.e., marginal error) [
45]. Assuming a 95% confidence level (Z = 1.96), a proportion estimate of 0.5 (p = 0.5, q = 0.5), and a 5% margin of error (e = 0.05), the minimum required sample size was calculated as ((1.96)2 (0.5) (0.5))/(0.05)2 = 385 [
45]. Based on this, a total of 384 participants aged 18 to 24 years were included (one was excluded due to sensitivity), from Chitwan and Kathmandu districts (i.e., Dataset 1), which was used for developing the tool, also previously used in a study [
6]. For Dataset 2, we included 803 participants from across Nepal, encompassing both students and individuals from the general population from very remote areas such as Karnali in the west and Jhapa in the east including Kathmandu and Chitwan, which was used for CFA. The sample comprised diverse demographic characteristics, including various demographic components such as genders, religious and ethnic groups within the country.
Opportunity sampling was used to recruit all the participants mostly college students, a population considered crucial for understanding and shaping societal attitudes toward mental health [
46,
47], and general individuals for broader representation.
2.3. Instruments
Two standardized self-report instruments were employed: the ATMHP scale [
16] and MHLQ-YA [
44] in online google forms and paper-based questionnaires. The tools used in the study were translated into Nepali following rigorous cross-cultural adaptation procedures to reduce language-related biases. The forward translation was conducted by a professional language teacher, a native Nepali speaker with bilingual competence, who was also working in the field of translation. The back translation was carried out by another professional language teacher, also a native Nepali speaker with bilingual competence and experience in translation. Again, the translated version underwent evaluation by five other English language teachers to identify any linguistic ambiguities. Finally, a psychology lecturer with expertise in mental health in Nepal reviewed the translation for accuracy and cultural relevance. The final version was then reviewed by a Nepali language expert for spelling, punctuation, and grammar. These steps helped ensure linguistic and conceptual equivalence in the adapted tools.
Google forms were distributed via platforms such as Facebook, LinkedIn and Instagram. For the paper-based method, participants were approached directly on campuses. The online survey was administered between 26 June and 24 October 2021, while the paper-pencil survey was conducted from 27 September to 4 October 2021.
2.4. Ethical Consideration
Ethical approval for the first study (Dataset 1, n = 384) was obtained from the Nepal Health Research Council under Ethics Review Board protocol registration no. 309/2021 (ref. no. 3543, approval date: 15 June 2021) [
6] and for the second study (Dataset 2, n = 803), we obtained approval from college authorities according to their rules and regulations; college–1 (reference no. 151/2077/78; date: 20th June 2021), College–2 (reference no. 105/077/078; date: 22nd June, 2021); college–3 (reference no. 423; date: 1st Oct. 2021); college–4 (reference no. 433; 4th Oct, 2021) college–5 (Dispatch no. 544; 4th Oct. 2021). Informed consent was obtained after participants were briefed on confidentiality, data security, and their right to withdraw at any time. The study adhered to the ethical principles of the Declaration of Helsinki, ensuring participant rights and autonomy throughout [
48]. Licensed and free software tools (MS Office - 16, Stata version 18, semdiag and Google Forms/Sheets) were used for data collection, analysis, the path diagram creation and manuscript preparation [
49].
2.5. Data Analysis
Data were analyzed using Stata 18.0, following the methods of a similar UK study [
26], and the path diagram was created using semdiag [
49]. Dataset 1 (n = 384) was used for item reduction and Dataset 2 (n = 803) for validation. Outliers in Dataset 1 were removed by visually inspecting total scores; perfect scores (105) were excluded to improve sensitivity. Descriptive statistics summarized demographic data. Pearson correlations identified two items with the highest inter-item correlations within each of the seven ATMHPS subscales, producing a 14-item N-SATMHPS. Internal consistency was assessed using Cronbach’s alpha, and item-total correlations evaluated item performance. Convergent validity was tested by correlating subscale totals between the original and shortened scales. Confirmatory factor analysis (CFA) was conducted to assess model fit using χ
2/df, CFI, TLI, RMSEA, and SRMR as fit indices. Dataset 2 was used to replicate the procedures and confirm the reliability and structural validity of the N-SATMHPS. The threshold for The comparative fit index (CFI) and the Tucker–Lewis index (TLI) was assumed over 0.90, while for the root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR) [
50].
3. Results
3.1. Dataset Overview
We developed the N-SATMHPS using Dataset 1 (n = 384) and validated it with Dataset 2 (n = 805). Each dataset contained the full ATMHPS items, labelled atmhp1 to atmhp35. One response in Dataset 1 with a perfect total score (105 points) was excluded, as it may reflect an extreme response style such as acquiescence bias or social desirability rather than genuine attitudes [
51]. This exclusion followed best practices in psychometric research to improve the sensitivity and interpretability of scale performance. The analytical methods were based on prior work by Kotera et al. (2023b) [
26], and analyses were conducted using Stata 18.0. A path diagram was generated using the semdiag package [
49].
3.2. Confirmation of Background Factors
Next, we examined the background factors of the participants in each dataset. Demographic characteristics differed between the two datasets. Participants in Dataset 1 were younger, predominantly female, and mostly students. In contrast, Dataset 2 included a broader age range with more occupational diversity (
Table 1 and
Table 2).
3.3. Extraction of Two Questions for Correlation Analysis for N-SATMHPS
A correlation analysis was conducted on the group in Dataset 1 (
Table 3). We evaluated the correlations between the questions within each subscale and selected the two items with the highest correlation.
3.4. Performance Evaluation of the Developed N-SATMHPS
Next, we evaluated the correlation (item-total correlations), p-values of the selected questions and each subscale. The results are presented in
Table 4.
Unlike the benchmark validation study [
26], the correlation coefficients ranged from 0.59 to 0.83, showing low values for some items. Next, we calculated the average, standard deviation, and α for each item (scored 0-3) for each subscale (
Table 5). Next, we calculated the average, standard deviation, and αfor each item (scored 0-3) for each subscale (
Table 5).
Alpha (α) had a reliability of 0.79-0.92 in ATMHPS and 0.71-0.89 in SATMHPS, which was not as reliable as the reference paper. The table below shows the correlation of the sums of the subscales for ATMHPS and N-SATMHPS.
Table 6.
Correaltion between Full ATMHP & N-SATMHPS.
Table 6.
Correaltion between Full ATMHP & N-SATMHPS.
| |
r |
| Community Attitudes |
.90 |
| Family Attitudes |
.90 |
| Community External Shame |
.94 |
| Family External Shame |
.93 |
| Internal Shame |
.89 |
| Family Reflected Shame |
.79 |
| Self-Reflected Shame |
.94 |
Except for the Family Reflected Shame, a strong correlation was obtained.
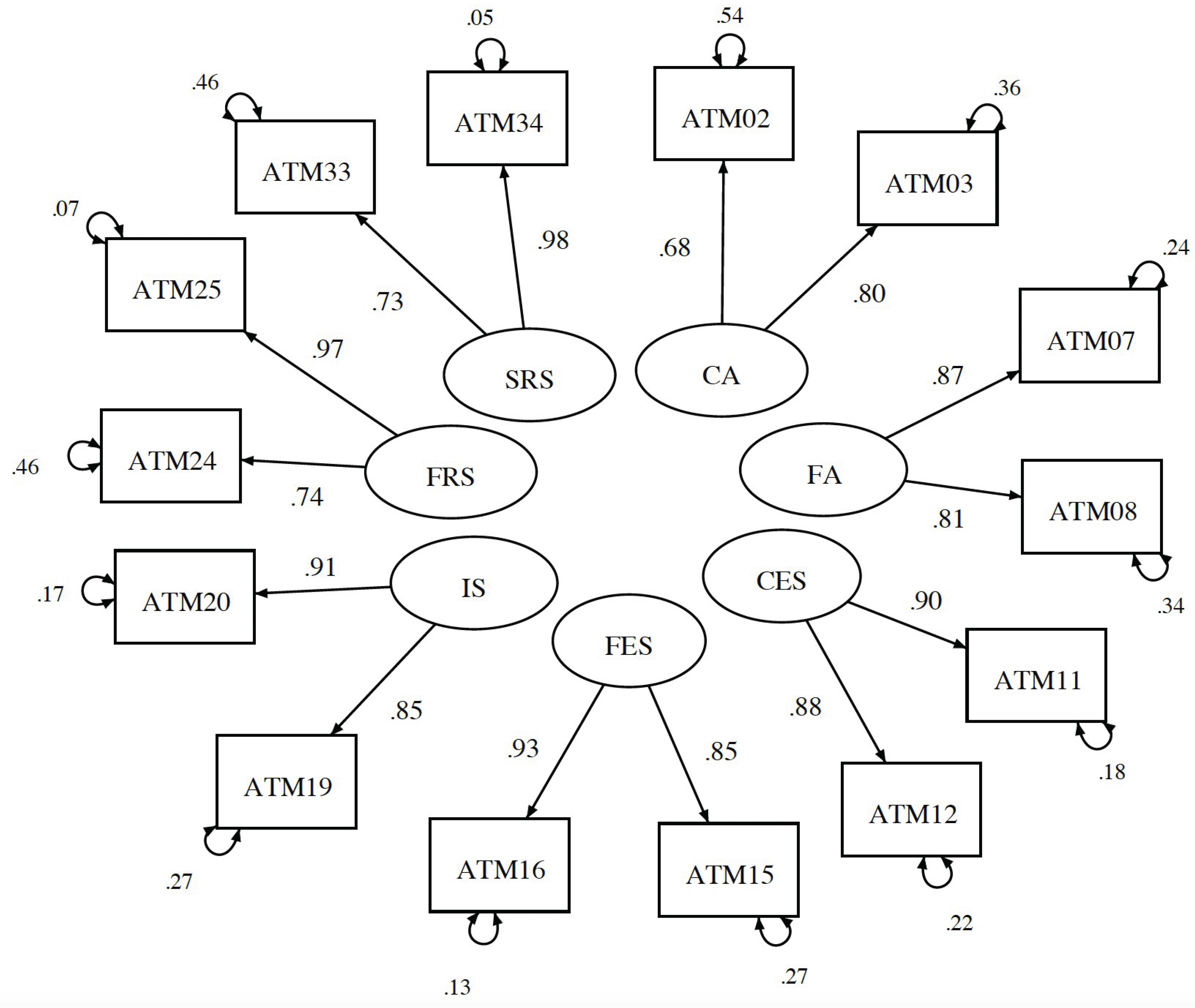
Finally, a path diagram was created and the goodness of fit of the model was evaluated (
Figure 1).
The confirmatory factor analysis (CFA) indicated a good model fit, with all fit indices falling within acceptable ranges. The chi-square to degrees of freedom ratio (χ2/df) was 107.32/56 = 1.92, suggesting an adequate fit. The comparative fit index (CFI) was 0.98, and the Tucker–Lewis index (TLI) was 0.97, both exceeding the recommended threshold of 0.90. Additionally, the root mean square error of approximation (RMSEA) was 0.049, and the standardized root mean square residual (SRMR) was 0.026, both indicating a good fit according to conventional guidelines.
3.5. Validation
We developed and validated the N-SATMHPS using dataset–1 and dataset–2 respectively. First, we confirmed the internal consistency. The results are presented in
Table 7.
The results showed that the alpha for ATMHPS was 0.84-0.94, and for N-SATMHPS it was 0.74-0.92, indicating that the coefficients for the shortened versions were generally lower than those of the current versions. However, the alpha values themselves were within an acceptable range.
Finally, as in development, the following table confirms the correlation of the sums of each subscale of N-SATMHPS (
Table 8).
The results showed that the correlation coefficients were generally higher than those from development.
3.6. Discriminant Validity
Several significant but weak correlations were observed between MHLQ-YA factors and N-SATMHPS subscales, supporting discriminant validity. Notably, MHLQ-YA Factor 1 was positively correlated with N-SATMHPS Community Attitudes and Total Score. Factor 2 showed negative correlations with Family Attitudes, Family External Shame, Self-Reflected Shame, and the Total Score. Factor 3 was negatively associated with Family Attitudes, Family External Shame, Internal Shame, and the Total Score. No significant associations emerged for Factor 4 or the MHLQ-YA Total Score. The details are presented in the
Table 9.
The validated N-SATMHPS and manual are available in the Appendixes.
4. Discussion
The development and validation of N-SATMHPS represent a significant advancement in culturally sensitive mental health assessment tools. We aimed to create a concise yet reliable instrument to measure attitudes towards mental health problems within the Nepali context, ensuring both psychometric robustness and practical applicability.
4.1. Model Fit
The N-SATMHPS demonstrated satisfactory internal consistency across subscales. While slightly lower than the reliability scores of the full ATMHPS and the short form J-SATMHPS, the values remain within acceptable thresholds for psychological tools, supporting the scale’s reliability [
16,
27]. CFA supported the seven-factor structure of the N-SATMHPS, with fit indices indicating a good model fit. These findings are consistent with the CFA results of the SATMHPS and J-SATMHPS, both of which demonstrated strong model fit [
26,
27].
4.2. Correlation Analyses
The N-SATMHPS subscales exhibited strong correlations with their corresponding subscales in the full ATMHPS, ranging from 0.79 to 0.96. This consistency underscores the N-SATMHPS’s capability to effectively capture the constructs measured by the full scale [
26].
Discriminant validity of The N-SATMHPS was assessed through correlations with the MHLQ-YA [
44]. Significant but weak correlations were observed between certain N-SATMHPS subscales and MHLQ-YA factors, suggesting that while related, the constructs measured by the two instruments are distinct. For instance, MHLQ-YA Factor 1 (Knowledge of Mental Health Problems) showed a positive correlation with the Community Attitudes subscale of the N-SATMHPS, suggesting higher knowledge of mental health increases negative community attitudes whereas Factor 2 (Erroneous Beliefs/Stereotypes) exhibited negative correlations with several N-SATMHPS subscales, indicating higher awareness against erroneous beliefs/stereotypes promotes positive attitudes. Studies have found that mental health literacy reduces mental health shame [
52,
53,
54]. However, Poudel et al. (2024) have found no relation between mental health knowledge and mental health shame [
6].
4.3. Cultural Considerations and Implications
The adaptation of the ATMHPS into the Nepali context required careful consideration of cultural nuances related to mental health stigma and shame. The strong internal consistency and model fit indices suggest that the N-SATMHPS effectively captures culturally relevant attitudes towards mental health problems in Nepal.
The successful cultural adaptation of the ATMHPS into the Nepalese context underscores the scale’s utility in collectivist societies where community and family perceptions deeply influence individual behavior [
55]. Unlike Western cultures, which generally prioritize individual autonomy [
56], Nepalese society often views mental health through a communal lens, where family honor (izzat) and societal expectations play a critical role [
33,
57]. Concepts such as reflected shame (i.e., feeling disgrace on behalf of the family) and external shame (i.e., fear of judgment by the community) are embedded in everyday attitudes. In our study, these constructs remained relevant and strongly endorsed, validating the theoretical structure of the N-SATMHPS. This aligns with prior cross-cultural work in Japan [
58]. Moreover, despite some subcultural diversity in Nepal, our results showed consistency across gender, caste, and religious affiliations, suggesting the scale captures common cultural attitudes rather than group-specific perspectives. The validation of the N-SATMHPS contributes not only to Nepalese mental health research but also offers a model for culturally contextualizing global tools in diverse settings.
Assessing mental health shame is particularly valuable because it can directly in-form interventions that encourage help-seeking and self-compassion [
59]. High levels of shame often prevent individuals from accessing mental health services due to fear of judgment or loss of social standing [
60]. By identifying these attitudes, targeted psychoeducation and compassion-focused approaches can be developed to reduce shame, normalize help-seeking, and promote a more accepting self-view. Evidence suggests that lower shame and higher self-compassion are linked to greater willingness to seek professional support and improved mental health outcomes [
61]. Therefore, the N-SATMHPS not only measures attitudes but also offers practical insights for designing culturally appropriate mental health interventions in Nepal.
4.4. Limitation
This study has several limitations. First, while the sample was large and geographically diverse, it was limited to young adults and used opportunity sampling, which may restrict generalizability [
62]. Second, the study did not assess test-retest reliability, limiting insights into the scale’s stability over time [
63]. Third, reliance on self-report measures introduces potential response biases, especially given the sensitive nature of mental health stigma [
27]. Fourth, no qualitative methods were used, which could have deepened understanding of how shame and stigma are experienced in context. Finally, the clinical and applied utility of the N-SATMHPS was not evaluated; future work should explore its usability in real-world mental health practice.
5. Conclusions
The N-SATMHPS emerges as a reliable and valid instrument for assessing attitudes towards mental health problems in Nepal. Its brevity and cultural relevance make it a practical tool for both research and clinical settings. By facilitating the assessment of mental health attitudes, the N-SATMHPS can contribute to the development of targeted interventions aimed at reducing stigma and promoting mental well-being within the Nepali context.
Author Contributions
Conceptualization, D.B.P.; methodology, T.Y.; software, T.Y.; validation, D.B.P., T.Y., R.C., and Y.K..; formal analysis, T.Y.; investigation, D.B.P.; resources, D.B.P. and Y.K..; data curation, D.B.P.; writing—original draft preparation, D.B.P.; writing—review and editing, D.B.P., T.Y., R.C., and Y.K; visualization, D.B.P. and T.Y.; supervision, Y.K.; project administration, D.B.P.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Nepal Health Research Council (NHRC) (ERB protocol no. 309/2021, ref. no. 3543, approval date: 15 June 2021) for dataset 1 [
6]; and dataset 2 was approved by internal board of different colleges: college–1 (reference no. 151/2077/78; date: 20th June 2021), College–2 (reference no. 105/077/078; date: 22nd June, 2021); college–3 (reference no. 423; date: 1st Oct. 2021); college–4 (reference no. 433; 4th Oct, 2021) college–5 (Dispatch no. 544; 4th Oct. 2021). It followed the ethical guidelines of the Declaration of Helsinki, ensuring participants’ rights were protected throughout the research
.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Certain data is available upon reasonable request from the corresponding author.
Acknowledgments
We sincerely thank the colleges’ authorities and participants from the colleges involved in this study for their support and participation. We also acknowledge the Nepal Health Research Council (NHRC) for granting ethical approval for dataset 1. We acknowledge all the authors cited in this article for their contributions. During the preparation of this manuscript, the authors used ChatGPT (GPT-5, OpenAI, 2025) for the purposes of language refinement. The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ATMHP |
Attitudes Towards Mental Health Problems |
| CFA |
Confirmatory Factor Analysis |
| CFI |
Comparative Fit Index |
| df |
Degrees of Freedom |
| J-SATMHPS |
Japanese Shorter Version of Attitudes Towards Mental Health Problems Scale |
| MHLQ–YA |
Mental Health Literacy Questionnaire – Young Adult |
| N-SATMHPS |
Nepalese Shorter Version of Attitudes towards Mental Health Problems Scale |
| RMSEA |
Root Mean Square Error of Approximation |
| SATMHPS |
Shorter Version of the Attitudes Towards Mental Health Problems |
| SD |
Standard Deviation |
| SRMR |
Standardized Root Mean Square Residual |
| TLI |
Tucker–Lewis Index |
Appendix A
The following
Appendix A1 and
Appendix A2 contains the validated scale and it’s scoring procedure in Nepali language. The instruction to the participants have also been given same language to capture cultural values more appropriately.
Appendix A.1
नेपाली छोटो मानसिक स्वास्थ्य समस्याप्रतिको मनोभाव प्रश्नावली
हामी मानसिक स्वास्थ्य समस्याका बारेमा मानिसहरूले के सोच्छन र कसरी लिन्छन, मानसिक स्वास्थ्य समस्यालाई कसरी हेर्छन भन्ने कुरामा जान्न चाहन्छौं । तपाईंलाई थाहै होला, केही मानिसहरू डिप्रेसन (निराशा) र एन्जाइटी (चिन्ता) जस्ता मानसिक स्वास्थ्य समस्याबाट पीडित रहेका हुन्छन । यी समस्याहरूले उनीहरूको लागि दैनिक जीवनमा सहजरुपमा अघि बढ्न वा दैनिक जीवनको सामना गर्न कठिनाइ उत्पन्न गराउन सक्छन । डिप्रेसन भएका मानिसहरू थकित महसुस गर्न सक्छन, जीवनमा रमाउन सक्दैनन, आफूलाई एकान्तमा राख्न चाहन्छन र पारिवारिक जीवनदेखि पर बस्ने हुन सक्छन । तल केही भनाइरकथनहरू छन जुन तपाईंले, तपाईंको समुदायले वा तपाईंको परिवारले मानसिक स्वास्थ्यसँग सम्बन्धित समस्यालाई कसरी हेर्ने गरेको छ भन्ने देखाउँछ । हरेक कथन ध्यानपूर्वक पढी ती कथनहरूसँग तपाईं कत्तिको समहत हुनुहुन्छ भन्ने देखाउन उपयुक्त कुनै एउटा अंकमा गोलो घेरा लगाउनुहोस।
कृपया तलको मापनस्तर प्रयोग गर्नुहोस
० . पटक्कै सहमत छैन १ . अलिअलि सहमत २ . धेरै हदसम्म सहमत ३ . पूर्ण सहमत
यहाँ कोष्ठमा भएको अंकले मूल प्रश्नावलीको प्रश्न नम्बरलाई जनाउँछ।
मानसिकस्वास्थ्यप्रतिकोमनोभाव
प्रश्नहरूको यस पहिलो समूहको लागि, दैनिक जीवनको सामना गर्न कठिन बनाउने डिप्रेसन र एन्जाइटी जस्ता मानसिक स्वास्थ्य समस्यालाई तपाईंको समुदाय र परिवारले कसरी हेर्छन भन्नेबारे केहीबेर सोचविचार गरी तलको कुनै उपयुक्त अंकमा गोलो घेरा लगाउनुहोस ।
समुदायको मनोवृत्ति
| १. (२) मेरोसमुदायलेमानसिकस्वास्थ्यसमस्यालाईव्यक्तिगतकमजोरीकोरुपमाहेर्छ। |
० |
१ |
२ |
३ |
| २. (३) मेरोसमुदायमामानसिकस्वास्थ्यसमस्याभएकोमानिसलाईतिरस्कारकोनजरलेहेरिन्छ। |
० |
१ |
२ |
३ |
पारिवारिक मनोवृत्ति
| ३. (७) मेरोपरिवारमामानसिकस्वास्थ्यसमस्याभएकोमानिसलाईतिरस्कारकोनजरलेहेरिन्छ। |
० |
१ |
२ |
३ |
| ४. (८) मेरोपरिवारमानसिकस्वास्थ्यसमस्याभएकामानिसहरूबाटपरबस्नचाहन्छ। |
० |
१ |
२ |
३ |
बाहिरी लाज
अब अर्को प्रश्नहरूको समूहको लागि, दैनिक जीवनको सामना गर्न कठिन बनाउने डिप्रेसन र एन्जाइटी जस्ता मानसिक स्वास्थ्य समस्याबाट यदि तपाईं पिडित हुनुभएमा तपाईंलाई तपाईंको समुदाय वा परिवारले कसरी हेर्छ होला, केहीबेर सोचविचार गरी तलका कुनै उपयुक्त अंकमा गोलो घेरा लगाउनुहोस ।
सामुदायिक बाहिरी लाज
| ५. (११) मलाईलाग्छमेरोसमुदायलेमलाईकामनलाग्नेमानिसकोरुपमाहेर्नेछ। |
० |
१ |
२ |
३ |
| ६. (१२) मलाईलाग्छमेरोसमुदायलेमलाईकमजोरमानिसकोरुपमाहेर्नेछ। |
० |
१ |
२ |
३ |
पारिवारिक बाहिरी लाज
| ७. (१५) मलाईलाग्छमेरोपरिवारलेमलाईनिकृष्ट (तल्लो) व्यक्तिकोरुपमाहेर्नेछ। |
० |
१ |
२ |
३ |
| ८. (१६) मलाईलाग्छमेरोपरिवारलेमलाईकामनलाग्नेमानिसकोरुपमाहेर्नेछ। |
० |
१ |
२ |
३ |
आन्तरिक लाज
अब अर्को प्रश्नहरूको समूहको लागि, दैनिक जीवनको सामना गर्न कठिन बनाउने डिप्रेसन र एन्जाइटी जस्ता मानसिक स्वास्थ्य समस्याबाट तपाईं पिडित हुनुभएको अवस्थामा तपाईं आफूलाई कस्तो महसुस हुन्छ होला, केहीबेर सोचविचार गरी तलका कुनै उपयुक्त अंकमा गोलो घेरा लगाउनुहोस ।
| ९. (१९) मआफूलाईतल्लोव्यक्तिकोरुपमाहेर्नेछु। |
० |
१ |
२ |
३ |
| १०. (२०) मआफूलाईकामनलाग्नेव्यक्तिकोरुपमाहेर्नेछु। |
० |
१ |
२ |
३ |
परिवार प्रतिबिम्बित लाज
अब अर्को प्रश्नहरूको समूहको लागि, दैनिक जीवनको सामना गर्न कठिन बनाउने डिप्रेसन र एन्जाइटी जस्ता मानसिक स्वास्थ्य समस्याबाट तपाईं पिडित हुनुभएको अवस्थामा तपाईं कस्तो महसुस हुन्छ होला । यसपटक ती समस्याका कारण तपाईंको परिवारमा पर्ने प्रभावबारे तपाईं कत्तिको चिन्तित हुनुहुनेछ
, केहीबेर सोचविचार गरी तलका कुनै उपयुक्त अंकमा गोलो घेरा लगाउनुहोस ।
| ११. (२४) मेरोपरिवारलाईतल्लोरुपमाहेरिनेछ। |
० |
१ |
२ |
३ |
| १२. (२५) मेरोपरिवारलाईकामनलाग्नेरुपमाहेरिनेछ। |
० |
१ |
२ |
३ |
आत्म प्रतिबिम्बित लाज
अब अर्को प्रश्नहरूको समूहको लागि, दैनिक जीवनको सामना गर्न कठिन बनाउने डिप्रेसन र एन्जाइटी जस्ता मानसिक स्वास्थ्य समस्याबाट तपाईंको कुनै नजिकको नातेदार पिडित हुनुभएको अवस्थामा तपाईं कस्तो महसुस हुन्छ होला । यसपटक ती समस्याका कारण तपाईंमा पर्ने प्रभावबारे तपाईं कत्तिको चिन्तित हुनुहुनेछ
, केहीबेर सोचविचार गरी तलका कुनै उपयुक्त अंकमा गोलो घेरा लगाउनुहोस ।
| १३. (३३) मेरोआफ्नैमानसम्मानमाहानिपुग्लाकिभनेरमचिन्तितहुनेछु। |
० |
१ |
२ |
३ |
| १४. (३४) यदियोकुराथाहाभयोभनेमेरोसमुदायमामेरोप्रतिष्ठाघट्नेछभनेरमलाईचिन्तालाग्नेछ। |
० |
१ |
२ |
३ |
Appendix A.2
मूल्याङ्कन (SCORING)
प्रत्येक आयामका प्रश्नहरूको जोड गरेर जम्मा स्कोर निकाल्नुहोस्।
विवरण(DESCRIPTION)
अघिल्लो अनुसन्धान Gilbert et al. (२००४) [
33] ले एसियाली महिलाहरूमा लाजसँग सम्बन्धित धेरै चिन्ताहरू उजागर गरेको थियो — जुन समुदाय, परिवार र व्यक्तिगत आत्म-मूल्यांकनसँग जोडिएका छन्। यीमध्ये केही बाहिरी लाज (external shame) को रूपमा हुन्छन्, जहाँ व्यक्तिले अरूले आफूलाई कसरी हेर्छन् भन्नेमा ध्यान केन्द्रित गर्छन् । यसका साथै, प्रतिबिम्बित लाज (reflected shame) र “इज्जत” को अवधारणा—अर्थात् एक जनाको कारणले पूरै परिवारलाई लाज हुन सक्छ वा परिवारका अरू सदस्यको समस्याले आफूमा लाजको अनुभूति हुन सक्छ—यी पनि नेपाली संदर्भमा महत्त्वपूर्ण छन् [
33,
36,
37]।
हामीले मानसिक स्वास्थ्य समस्याप्रतिको धारणा मापन गर्ने मूल ३५ प्रश्नको मानसिक स्वास्थ्य समस्याप्रतिको मनोभाव (Attitudes Towards Mental Health Problems; ATMHP, Gilbert, 2007) [
16] बाट नेपाली संदर्भको लागि एउटा छोटो संस्करण विकास गरेका छौं
, जसलाई नेपाली छोटो मानसिक स्वास्थ्य समस्याप्रतिको मनोभाव प्रश्नावली (Nepalese Shorter Version of Attitudes Towards Mental Health Problems Scale; N-SATMHPS) भनिन्छ। यसमा मूल ३५ प्रश्नमध्ये केवल १४ वटा प्रश्नहरू समावेश गरिएका छन्
, जुन ७ वटा मुख्य आयामहरूलाई प्रतिनिधित्व गर्ने गरी चयन गरिएका छन्:
यस प्रश्नावलीले मानसिक स्वास्थ्य समस्यासँग जोडिएको लाज, सामाजिक धारणा र व्यक्तिगत अनुभूतिलाई नेपाली संदर्भमा विश्वसनीय रूपमा मापन गर्न सक्छ।
यस १४ प्रश्नको प्रश्नावलीले तलका ७ आयामहरूलाई प्रतिनिधित्व गर्दछ:
१
.
समुदायको मनोवृत्ति
प्रश्न १ (२): मेरो समुदायले मानसिक स्वास्थ्य समस्यालाई व्यक्तिगत कमजोरीको रूपमा हेर्छ।
प्रश्न २ (३): मेरो समुदायमा मानसिक स्वास्थ्य समस्या भएको मानिसलाई तिरस्कारको नजरले हेरिन्छ।
२
.
पारिवारिक मनोवृत्ति
प्रश्न ३ (७): मेरो परिवारमा मानसिक स्वास्थ्य समस्या भएको मानिसलाई तिरस्कारको नजरले हेरिन्छ।
प्रश्न ४ (८): मेरो परिवार मानसिक स्वास्थ्य समस्या भएका मानिसहरूबाट पर बस्न चाहन्छ।
३. सामुदायिक बाहिरी लाज
प्रश्न ५ (११): मलाई लाग्छ मेरो समुदायले मलाई काम नलाग्ने मानिसको रूपमा हेर्नेछ।
प्रश्न ६ (१२): मलाई लाग्छ मेरो समुदायले मलाई कमजोर मानिसको रूपमा हेर्नेछ।
४. पारिवारिक बाहिरी लाज
प्रश्न ७ (१५): मलाई लाग्छ मेरो परिवारले मलाई निकृष्ट (तल्लो) व्यक्तिको रूपमा हेर्नेछ।
प्रश्न ८ (१६): मलाई लाग्छ मेरो परिवारले मलाई काम नलाग्ने मानिसको रूपमा हेर्नेछ।
५. आन्तरिक लाज
प्रश्न ९ (१९): म आफूलाई तल्लो व्यक्तिको रूपमा हेर्नेछु।
प्रश्न १० (२०): म आफूलाई काम नलाग्ने व्यक्तिको रूपमा हेर्नेछु।
६. परिवार प्रतिबिम्बित लाज
प्रश्न ११ (२४): मेरो परिवारलाई तल्लो रूपमा हेरिनेछ।
प्रश्न १२ (२५): मेरो परिवारलाई काम नलाग्ने रूपमा हेरिनेछ।
७. आत्म प्रतिबिम्बित लाज
प्रश्न १३ (३३): मेरो आफ्नै मानसम्मानमा हानि पुग्ला कि भनेर म चिन्तित हुनेछु।
प्रश्न १४ (३४): यदि यो कुरा थाहा भयो भने मेरो समुदायमा मेरो प्रतिष्ठा घट्नेछ भनेर मलाई चिन्ता लाग्नेछ।
मूल्यांकन प्रणाली:
यहाँ कोष्ठमा भएको अंकले मूल प्रश्नावलीको प्रश्न नम्बरलाई जनाउँछ। सबै प्रश्नहरू ४-बिन्दु लिकर्ट प्रणालीमा आधारित छन्:
० = पटक्कै सहमत छैन, १ = अलिअलि सहमत, २ = धेरै हदसम्म सहमत, ३ = पूर्ण सहमत
प्राप्त हुन सक्ने जम्मा स्कोर ० देखि ४२ सम्म छ। जति बढी स्कोर, त्यति नै बढी नकारात्मक मनोवृत्ति/प्रतिकूल मनोवृत्तिलाई जनाउँछ।
References
- Corrigan, P. How stigma interferes with mental health care. Am Psychol. 2004, 59, 614–625. [Google Scholar] [CrossRef] [PubMed]
- Gurung D, Poudyal A, Wang YL, Neupane M, Bhattarai K, Wahid SS, et al. Stigma against mental health disorders in Nepal conceptualised with a “what matters most” framework: A scoping review. Epidemiol Psychiatr Sci. 2022, 31. [Google Scholar]
- Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013, 103, 777–780. [Google Scholar] [CrossRef]
- Kotera Y, Tsuda-McCaie F, Maughan G, Green P. Cross-cultural comparison of mental health in social work students between UK and Ireland: Mental health shame and self-compassion. Br J Soc Work [Internet]. 2021, 52, 3247–3267. [Google Scholar] [CrossRef]
- Maharjan S, Panthee B. Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese teaching hospital: A cross-sectional study. BMC Psychiatry. 2019, 19, 1–8. [Google Scholar]
- Poudel DB, Sharif LS, Acharya S, Mahsoon A, Sharif K, Wright R. Mental health literacy and attitudes towards mental health problems among college students, Nepal. Behav Sci (Basel). 2024, 14, 1–18. [Google Scholar]
- Poudel DB, Dhakal S, Khatri BB. Review Articles Attitudes Towards Mental Health Problems : A Scoping Review. Birat J Helath Sci [Internet]. 2025, 9, 3–13, Available from: https://bjhs.com.np/bjhs/index.php/bjhs/article/view/523/533. [Google Scholar]
- Rai Y, Gurung D, Gautam K. Insight and challenges: mental health services in Nepal. BJPsych Int [Internet]. 2021, 18, 1–3, Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8274424/pdf/S2056474020000586a.pdf. [Google Scholar]
- Thornicroft G, Kassam A. Public attitudes, stigma and discrimination against people with mental illness. Morgan C, McKenzie K, Fearon P, editors. Society and Psychosis. Cambridge University Press; 2008. 179–197 p.
- Adewuya AO, Oguntade AA. Doctors’ attitude towards people with mental illness in Western Nigeria. Soc Psychiatry Psychiatr Epidemiol. 2007, 42, 931–936. [Google Scholar] [CrossRef]
- Jalan, R. Attitudes of Undergraduate Medical Students towards the Persons with Mental Illness in a Medical College of Western Region of Nepal. J Nepalgunj Med Coll. 2018, 16, 48–53. [Google Scholar] [CrossRef]
- Kotera Y, Kotera H, Taylor E, Wilkes J, Colman R, Riswani R. Mental health of Indonesian university students: U.K. comparison and relationship between mental health shame and self-compassion. Stigma Heal. 2024, 9, 239–248. [Google Scholar] [CrossRef]
- Neupane D, Dhakal S, Thapa S, Bhandari PM, Mishra SR. Caregivers’ attitude towards people with mental illness and perceived stigma: A cross- sectional study in a tertiary hospital in Nepal. PLoS One. 2016, 11, 1–12. [Google Scholar]
- Sahile Y, Yitayih S, Yeshanew B, Ayelegne D, Mihiretu A. Primary health care nurses attitude towards people with severe mental disorders in Addis Ababa, Ethiopia: A cross sectional study. Int J Ment Heal Syst [Internet]. 2019, 13, 1–8. [Google Scholar] [CrossRef]
- Tungchama FP, Egbokhare O, Omigbodun O, Ani C. Health workers’ attitude towards children and adolescents with mental illness in a teaching hospital in north-central Nigeria. J Child Adolesc Ment Health. 2019, 31, 125–137. [Google Scholar] [CrossRef]
- Gilbert P, Bhundia R, Mitra R, McEwan K, Irons C, Sanghera J. Cultural differences in shame-focused attitudes towards mental health problems in Asian and non-Asian student women. Ment Heal Relig Cult [Internet]. 2007, 10, 127–141, Available from: https://www.tandfonline.com/doi/abs/10.1080/13694670500415124. [Google Scholar] [CrossRef]
- Kotera Y, Sheffield D, Green P, Asano K. Cross-cultural comparison of mental health shame: Negative attitudes, external, internal and reflected shame about mental health in Japanese and UK workers. In: Mayer CH, Vanderheiden E, Wong. P., editors. New York: Springer; 2021. p. 55-71.
- Ahad AA, Sanchez-Gonzalez M, Junquera P. Understanding and addressing mental health stigma acrosscCultures for improving psychiatric care: A narrative review. Cureus. 2023, 15, 1–8. [Google Scholar]
- Brohan E, Thornicroft G. Stigma and discrimination of mental health problems: workplace implications. Occup Med (Chic Ill) [Internet]. 2010, 60, 414–415. [Google Scholar] [CrossRef]
- Girma E, Tesfaye M, Froeschl G, Möller-Leimkühler AM, Müller N, Dehning S. Public stigma against people with mental illness in the Gilgel Gibe Field Research Center (GGFRC) in Southwest Ethiopia. PLoS One [Internet]. 2013, 8, 1–9, Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0082116. [Google Scholar]
- Yang LH, Kleinman A. ‘Face’ and the embodiment of stigma in China: The cases of schizophrenia and AIDS. Soc Sci Med [Internet]. 2008, 67, 398–408. [Google Scholar] [CrossRef]
- NHRC. Report of national mental health survey 2020 [Internet]. Vol. 5, Goverment of Nepal, Nepal Health Research Council. 2021. Available from: https://nhrc.gov.np/wp-content/uploads/2022/10/National-Mental-Health-Survey-Report2020.
- Worldbank. World Bank Country and Lending Groups [Internet]. Datahelpdesk.worldbank.org. 2025 [cited 2025 Apr 15]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups?utm_source=chatgpt.
- Lindisfarne N. Gender, shame, and culture: An anthropological perspective. In: Andrews PGB, editor. Oxford University Press; 1998. p. 246–260.
- Cabral Master JM, Barreto Carvalho CM de O, Motta CD, Sousa MC, Gilbert P. Attitudes towards mental health problems scale: Confirmatory factor analysis and validation in the Portuguese population. Am J Psychiatr Rehabil. 2016, 19, 206–222. [Google Scholar] [CrossRef]
- Kotera Y, Taylor E, Wilkes J, Veasey C, Maybury S, Jackson J, et al. Construction and factorial validation of a short version of the Attitudes Towards Mental Health Problems Scale (SATMHPS). Ment Heal Relig Cult [Internet]. 2023;(August). Available from: https://www.tandfonline.com/doi/full/10.1080/13674676.2022.2114441.
- Kotera Y, Asano K, Jones J, Colman R, Taylor E, Aledeh M, et al. The development of the Japanese version of the full and short form of Attitudes Towards Mental Health Problems Scale (J-(S) ATMHPS). Ment Heal Relig Cult. 2023;(June).
- Netto G, Gaag S, Thanki M, Bondi L, Munro M. A Suitable Space. Improving counselling services forAsian people [Internet]. 1st ed. Islam Zeitschrift Für Geschichte Und Kultur Des Islamischen Orients. Policy Press; 2001. pp. 48. Available from: https://www.amazon.com/suitable-space-Improving-counselling-services/dp/1861343175.
- Hsiao FH, Klimidis S, Minas H, Tan ES. Cultural attribution of mental health suffering in Chinese societies: The views of Chinese patients with mental illness and their caregivers. J Clin Nurs. 2006, 15, 998–1006. [Google Scholar] [CrossRef] [PubMed]
- Fernando DS, Keating F, editors. Mental Health in a Multi-Ethnic Society: A Multidisciplinary Handbook. 2nd ed. London: Routledge; 2008. 320 p.
- Rao AV. Indian and Western Psychiatry: A Comparison. In: Cox JL, editor. Transcultural Psychiatry [Internet]. First. London: Routledge; 1986. p. 15. Available from: https://www.taylorfrancis.com/chapters/edit/10.4324/9780429447464-17/indian-western-psychiatry-comparison-venkoba-rao.
- Stanhope, V. Culture, control, and family involvement: A comparison of psychosocial rehabilitation in India and the United States. Psychiatr Rehabil J [Internet]. 2002, 25, 273–280, Available from: https://psycnet.apa.org/record/2002-00859-007. [Google Scholar] [CrossRef]
- Gilbert P, Gilbert J, Sanghera J. A focus group exploration of the impact of izzat, shame, subordination and entrapment on mental health and service use in South Asian women living in Derby. Ment Heal Relig Cult. 2004, 7, 109–130. [Google Scholar] [CrossRef]
- Kassam N, editor. Telling it Like it is: Young Asian Women Talk (Livewire) [Internet]. Livewire Books for Teenagers; 1997. 192 p. Available from: https://www.amazon.co.uk/Telling-Like-Young-Asian-Livewire/dp/0704349418.
- Chew-Graham C, Bashir C, Chantier K, Burman E, Batsleer J. South Asian women, psychological distress and self-harm: Lessons for primary care trusts. Heal Soc Care Community. 2002, 10, 339–347. [Google Scholar]
- Gilbert P, Andrews B. Shame: Interpersonal Behavior, Psychopathology, and Culture [Internet]. Oxford University Press; 1998. Available from. [CrossRef]
- Gilbert P, Miles J, editors. Body Shame: Conceptualisation, Research and Treatment [Internet]. London: Routledge; 2002. 320 p. Available from: https://www.taylorfrancis.com/books/edit/10.4324/9781315820255/body-shame-paul-gilbert-jeremy-miles.
- Nathanson DL, editor. Knowing Feeling: Affect, Script, and Psychotherapy [Internet]. 1st ed. W. W. Norton & Company; 1996. pp. 425. Available from: https://www.amazon.com/Knowing-Feeling-Psychotherapy-Professional-Hardcover/dp/0393702146.
- Babu B, Sinha A. Attitude towards mental health problems and seeking professional help. Int J Indian Psychol [Internet]. 2023;(March). Available from: https://www.researchgate.net/publication/369453431_Attitude_Towards_Mental_Health_Problems_and_Seeking_Professional_Help.
- Joji, S. Attitude Towards Mental Health Problems : A Survey Among College Students. 2020;(September).
- Kumar RS, Pathak A. Gender-based shame-focused attitude of general public toward mental illness : Evidence from Jharkhand, India. J Ment Heal Hum Behav [Internet]. 2021, 26, 132–138, Available from: https://journals.lww.com/mhhb/fulltext/2021/26020/gender_based_shame_focused_attitude_of_general.7.aspx. [Google Scholar] [CrossRef]
- Andrade G, Bedewy D, Elamin ABA, Abdelmonem KYA, Teir HJ, Alqaderi N. Attitudes towards mental health problems in a sample of United Arab Emirates’ residents. Middle East Curr Psychiatry [Internet]. 2022, 29, 2–6. [Google Scholar] [CrossRef]
- Hamid A, Furnham A. Factors affecting attitude towards seeking professional help for mental illness: A UK Arab perspective. Ment Heal Relig Cult. 2013, 16, 741–758. [Google Scholar] [CrossRef]
- Dias P, Campos L, Almeida H, Palha F. Mental health literacy in young adults: Adaptation and psychometric properties of the mental health literacy questionnaire. Int J Environ Res Public Health.
- Cochran, WG. Sampling Techniques [Internet]. 2nd ed. John Wiley & Sons; 1963. 413 p. Available from: https://books.google.com.np/books/about/Sampling_techniques_2nd_edition.html?id=YSxXwAACAAJ&redir_esc=y.
- Lange, RS. Pascarella, T. and Terenzin, P. (2005). How College Affects Students, A Third decade of Research (2nd ed.) San Francisco: Jossey-Bass. J Student Aff Africa. 2014, 2, 47–50. [Google Scholar] [CrossRef]
- Peterson RA, Merunka DR. Convenience samples of college students and research reproducibility. J Bus Res [Internet]. 2014, 67, 1035–1041. [Google Scholar] [CrossRef]
- Association, WM. World medical association declaration of Helsinki ethical principles for medical research involving human subjects. JAMA [Internet]. 2013, 310, 2191–2194, Available from: https://jamanetwork.com/journals/jama/fullarticle/1760318. [Google Scholar]
- Mai Y, Xu Z, Zhang Z, Yuan KH. An open-source WYSIWYG web application for drawing path diagrams of structural equation models. Struct Equ Model [Internet]. 2023, 30, 328–335, Available from: https://semdiag.psychstat.org/. [Google Scholar] [CrossRef]
- Hu L, Bentler PM, Hu L. Cutoff criteria for fit indexes in covariance structure analysis : Conventional criteria versus new alternatives Cutoff Criteria for Fit Indexes in Covariance Structure Analysis : Conventional Criteria Versus New Alternatives. 2009;5511.
- Meade AW, Craig SB. Identifying careless responses in survey data. Psychol Methods [Internet]. 2012, 17, 437–455, Available from: https://psycnet.apa.org/doiLanding?doi=10.1037%2Fa0028085. [Google Scholar] [CrossRef]
- Lee HY, Hwang J, Ball JG, Lee J, Yu Y, Albright DL. Mental health literacy affects mental health attitude: Is there a gender difference? Am J Health Behav. 2020, 44, 283–291. [Google Scholar]
- Riffel T, Chen SP. Exploring the knowledge, attitudes, and behavioural responses of healthcare students towards mental illnesses—A qualitative study. Int J Environ Res Public Health. 2020, 17, 1–11. [Google Scholar]
- Schröder R, Hamer T, Suhr R, König L. Attitudes toward Psychotherapeutic treatment and mealth literacy in a large sample of the general population in germany: Cross-sectional study. JMIR Public Heal Surveill [Internet]. 2025 Jan;11:e67078. Available from: http://www.ncbi.nlm.nih.gov/pubmed/39854696.
- Kotera Y, Lieu J, Kirkman A, Barnes K, Liu GHT, Jackson J, et al. Mental wellbeing of Indonesian students: Mean comparison with UK students and relationships with self-compassion and academic engagement. Healthc [Internet]. 2022, 10, 1–13, Available from: https://psycnet.apa.org/doiLanding?doi=10.1037%2Fa0028085. [Google Scholar]
- Kotera Y, Ronaldson A, Takhi S, Felix S, Namasaba M, Lawrence S, et al. Cultural influences on fidelity components in recovery colleges: a study across 28 countries and territories. Gen Psychiatry [Internet]. 2025 May 27;38(3):e102010. Available from: https://gpsychsite-bmj.vercel.app/content/38/3/e102010.
- Kotera Y, Ronaldson A, Takhi S, Felix S, Namasaba M, Lawrence S, et al. Cultural influences on fidelity components in recovery colleges : a study across 28 countries and territories. Gen Psychiatry [Internet]. 2025;38:1–12. Available from: https://gpsych.bmj.com/content/38/3/e102010.
- Kotera Y, Gilbert P, Asano K, Ishimura I, Sheffield D. Self-criticism and self-reassurance as mediators between mental health attitudes and symptoms: Attitudes toward mental health problems in Japanese workers. Asian J Soc Psychol [Internet]. 2019, 22, 183–192, Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/ajsp.12355. [Google Scholar] [CrossRef]
- Kotera, Y. De-stigmatising self-care: impact of self-care webinar during COVID-19. Int J Spa Wellness [Internet]. 2021;4(2–3):213–7. Available from. [CrossRef]
- Asano K, Tsuchiya M, Ishimura I, Lin S, Matsumoto Y, Miyata H, et al. The development of fears of compassion scale Japanese version. PLoS One [Internet]. 2017, 12, 1–17. [Google Scholar] [CrossRef]
- Kotera Y, Tsuda-Mccaie F, Edwards AM, Bhandari D, Williams D, Neary S. Mental Health Shame, Caregiver Identity, and Self-Compassion in UK Education Students. Healthc. 2022, 10, 1–10. [Google Scholar]
- Bornstein MH, Jager J, Putnick DL. Sampling in developmental science: Situations, shortcomings, solutions, and standards. Dev Rev [Internet]. 2013, 33, 357–370, Available from: https://www.sciencedirect.com/science/article/pii/S0273229713000385. [Google Scholar] [CrossRef]
- Kotera Y, Hara A, Newby C, Miyamoto Y, Ozaki A, Ali Y, et al. Development and evaluation of a mental health recovery priority measure for cross-cultural research: Global INSPIRE. Under Rev. 2025.
Figure 1.
N-SATMHPS Items and their Relation to Factors.
Figure 1.
N-SATMHPS Items and their Relation to Factors.
Table 1.
Background Characteristics of Participants (Dataset 1, n=384).
Table 1.
Background Characteristics of Participants (Dataset 1, n=384).
| Variables |
n (%) |
| Age (Mean, SD) |
20.7 (1.7) |
| Gender (Female) |
236 (61.6) |
| Caste/Ethnicity (Brahmin/Kshetri) |
269 (70.6) |
| Religion (Hindu) |
344 (89.6) |
| Districts (Chitwan) |
348 (90.4) |
| Marital status (Unmarried) |
369 (95.8) |
| Academic qualification (Bachelor’s degree) |
325 (84.4) |
Table 2.
Background Characteristics of Participants (Dataset 2, n=803).
Table 2.
Background Characteristics of Participants (Dataset 2, n=803).
| Variables |
n (%) |
Missing (n) |
| Age (Mean, SD) |
27.9 (8.7) |
21 |
| Gender (Female) |
351 (44.4) |
12 |
| Caste/Ethnicity (Brahmin/Kshetri) |
524 (66.0) |
9 |
| Religion (Hindu) |
660 (84.0) |
17 |
| Districts (Chitwan) |
247 (32.1) |
34 |
| Marital status (Unmarried) |
489 (61.6) |
9 |
| Academic qualification (Bachelor’s degree) |
352 (44.7) |
15 |
| Working status (Student) |
287 (36.0) |
6 |
| Caste/Ethnicity (Brahmin/Kshetri) |
524 (66.0) |
9 |
| Religion (Hindu) |
660 (84.0) |
17 |
Table 3.
Correlation Between Items in Each Factor of the ATMHPS for Dataset 1.
Table 3.
Correlation Between Items in Each Factor of the ATMHPS for Dataset 1.
| Community Attitudes |
|
|
|
|
|
|
|
| |
Item01 |
Item02 |
Item03 |
Item04 |
|
|
|
| Item01 |
— |
|
|
|
|
|
|
| Item02 |
0.52 |
— |
|
|
|
|
|
| Item03 |
0.47 |
0.55 |
— |
|
|
|
|
| Item04 |
0.45 |
0.37 |
0.54 |
— |
|
|
|
| Family Attitudes |
|
|
|
|
|
|
|
| |
Item05 |
Item06 |
Item07 |
Item08 |
|
|
|
| Item05 |
— |
|
|
|
|
|
|
| Item06 |
0.57 |
— |
|
|
|
|
|
| Item07 |
0.51 |
0.57 |
— |
|
|
|
|
| Item08 |
0.48 |
0.55 |
0.71 |
— |
|
|
|
| Community External Shame |
|
|
|
|
|
|
|
| |
Item09 |
Item10 |
Item11 |
Item12 |
Item13 |
|
|
| Item09 |
— |
|
|
|
|
|
|
| Item10 |
0.71 |
— |
|
|
|
|
|
| Item11 |
0.65 |
0.75 |
— |
|
|
|
|
| Item12 |
0.61 |
0.70 |
0.80 |
— |
|
|
|
| Item13 |
0.58 |
0.65 |
0.67 |
0.74 |
— |
|
|
| Family External Shame |
|
|
|
|
|
|
|
| |
Item14 |
Item15 |
Item16 |
Item17 |
Item18 |
|
|
| Item14 |
— |
|
|
|
|
|
|
| Item15 |
0.73 |
— |
|
|
|
|
|
| Item16 |
0.69 |
0.80 |
— |
|
|
|
|
| Item17 |
0.55 |
0.59 |
0.64 |
— |
|
|
|
| Item18 |
0.63 |
0.66 |
0.71 |
0.70 |
— |
|
|
| Internal Shame |
|
|
|
|
|
|
|
| |
Item19 |
Item20 |
Item21 |
Item22 |
Item23 |
|
|
| Item19 |
— |
|
|
|
|
|
|
| Item20 |
0.77 |
— |
|
|
|
|
|
| Item21 |
0.46 |
0.45 |
— |
|
|
|
|
| Item22 |
0.60 |
0.65 |
0.45 |
— |
|
|
|
| Item23 |
0.54 |
0.56 |
0.39 |
0.65 |
— |
|
|
| Family-reflected Shame |
|
|
|
|
|
|
|
| |
Item24 |
Item25 |
Item26 |
Item27 |
Item28 |
Item29 |
Item30 |
| Item24 |
— |
|
|
|
|
|
|
| Item25 |
0.71 |
— |
|
|
|
|
|
| Item26 |
0.58 |
0.57 |
— |
|
|
|
|
| Item27 |
0.59 |
0.60 |
0.57 |
— |
|
|
|
| Item28 |
0.33 |
0.33 |
0.40 |
0.42 |
— |
|
|
| Item29 |
0.37 |
0.39 |
0.38 |
0.46 |
0.70 |
— |
|
| Item30 |
0.36 |
0.37 |
0.40 |
0.51 |
0.54 |
0.69 |
— |
| Self-reflected Shame |
|
|
|
|
|
|
|
| |
Item31 |
Item32 |
Item33 |
Item34 |
Item35 |
|
|
| Item31 |
— |
|
|
|
|
|
|
| Item32 |
0.66 |
— |
|
|
|
|
|
| Item33 |
0.67 |
0.70 |
— |
|
|
|
|
| Item34 |
0.68 |
0.67 |
0.72 |
— |
|
|
|
| Item35 |
0.61 |
0.58 |
0.59 |
0.67 |
— |
|
|
Table 4.
Correlation Coefficients and P-values of the N-SATMHPS.
Table 4.
Correlation Coefficients and P-values of the N-SATMHPS.
| |
N-SATMHPS items |
Subscale |
Correlation coefficients |
p |
| 2 |
|
Community Attitudes |
0.59 |
<0.001 |
| 3 |
|
Community Attitudes |
0.65 |
<0.001 |
| 7 |
|
Family Attitudes |
0.71 |
<0.001 |
| 8 |
|
Family Attitudes |
0.69 |
<0.001 |
| 11 |
|
Community External Shame |
0.83 |
<0.001 |
| 12 |
|
Community External Shame |
0.82 |
<0.001 |
| 15 |
|
Family External Shame |
0.80 |
<0.001 |
| 16 |
|
Family External Shame |
0.82 |
<0.001 |
| 19 |
|
Internal Shame |
0.73 |
<0.001 |
| 20 |
|
Internal Shame |
0.76 |
<0.001 |
| 24 |
|
Family Reflected Shame |
0.63 |
<0.001 |
| 25 |
|
Family Reflected Shame |
0.64 |
<0.001 |
| 33 |
|
Self-reflected Shame |
0.78 |
<0.001 |
| 34 |
|
Self-reflected Shame |
0.80 |
<0.001 |
Table 5.
Comparision of Mean, SD and Correlation between Full ATMHP & N-SATMHPS.
Table 5.
Comparision of Mean, SD and Correlation between Full ATMHP & N-SATMHPS.
| |
Mean |
|
SD |
|
α |
|
| |
ATMHPS |
N-SATMHPS |
ATMHPS |
N-SATMHPS |
ATMHPS |
N-SATMHPS |
| Community Attitudes |
1.60 |
1.64 |
.81 |
.88 |
.79 |
.71 |
| Family Attitudes |
.65 |
.54 |
.73 |
.79 |
.84 |
.83 |
| Community External Shame |
1.21 |
1.26 |
.92 |
1.03 |
.92 |
.89 |
| Family External Shame |
.45 |
.39 |
.67 |
.70 |
.91 |
.89 |
| Internal Shame |
.73 |
.60 |
.74 |
.83 |
.86 |
.87 |
| Family Reflected Shame |
1.11 |
.71 |
.76 |
.82 |
.87 |
.83 |
| Self-Reflected Shame |
1.11 |
1.11 |
.92 |
1.00 |
.90 |
.84 |
Table 7.
Comparision of Reliability Scores (α) between Full ATMHP & N-SATMHPS.
Table 7.
Comparision of Reliability Scores (α) between Full ATMHP & N-SATMHPS.
| Factors |
α |
|
| |
ATMHPS |
N-SATMHPS |
| Community Attitudes |
.84 |
.74 |
| Family Attitudes |
.87 |
.84 |
| Community External Shame |
.94 |
.91 |
| Family External Shame |
.94 |
.92 |
| Internal Shame |
.89 |
.89 |
| Family External Shame |
.91 |
.91 |
| Family Reflected Shame |
.93 |
.89 |
Table 8.
Correaltions of Each Factors in N-SATMHPS.
Table 8.
Correaltions of Each Factors in N-SATMHPS.
| |
r |
| Community Attitudes |
.94 |
| Family Attitudes |
.91 |
| Community External Shame |
.96 |
| Family External Shame |
.96 |
| Internal Shame |
.90 |
| Family Reflected Shame |
.85 |
| Self-Reflected Shame |
.95 |
Table 9.
Discriminant Validity between N-SATMHPS & MHLQ-YA.
Table 9.
Discriminant Validity between N-SATMHPS & MHLQ-YA.
| |
MHLQ-YA
Factor 1
Knowledge of Mental Health Problems |
MHLQ-YA
Factor 2
Erroneous Beliefs/Stereotypes |
MHLQ-YA
Factor 3
First Aid Skills and Help Seeking Behavior |
MHLQ-YA
Factor 4
Self-Help Strategies |
MHLQ-YA
Total Score |
| |
Correlation
coefficients |
Correlation
coefficients |
Correlation
coefficients |
Correlation
coefficients |
Correlation
coefficients |
N-SATMHPS
Community Attitudes
|
.19** |
-.07 |
-.03 |
-.06 |
.04 |
N-SATMHPS
Family Attitudes
|
.07 |
-.13* |
-.14** |
-.05 |
-.08 |
N-SATMHPS
Community External Shame
|
.12* |
.01 |
-.06 |
.01 |
.04 |
N-SATMHPS
Family External Shame
|
.03 |
-.11* |
-.12* |
.00 |
-.07 |
N-SATMHPS
Internal Shame
|
.05 |
-.04 |
-.13** |
.03 |
-.03 |
N-SATMHPS
Family Reflected Shame
|
.06 |
-.04 |
-.03 |
-.01 |
0.01 |
N-SATMHPS
Self Reflected Shame
|
-.03 |
-.13* |
-.09 |
.04 |
-0.09 |
N-SATMPHS
Total Score
|
.11* |
-.10* |
-.13* |
-.00 |
-0.04 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).