1. Introduction
The global demographic shift toward population aging has profound implications for public health. One of the most pressing concerns is the growing prevalence of dementia and the associated psychological burden experienced by both patients and caregivers. Depression and anxiety are projected to increase alongside the demographic transition, with dementia representing a major driver of disability and dependency in later life. In 2019, it was estimated that the number of people living with dementia could reach 152.8 million by 2050, primarily due to increased life expectancy and demographic aging. More recent studies, however, have challenged these projections, noting potential underestimation of prevalence in minority populations such as Black and Hispanic groups [
1,
2], while others argue that lifestyle interventions may contribute to a decline in incidence over time [
3,
4]. According to the World Health Organization (WHO), approximately 57 million people were living with dementia in 2021, with 10 million new cases diagnosed each year, reflecting a constantly rising global burden [
5].
Dementia prevalence increases exponentially with age, doubling every five years after age 65 [
6]. The condition is particularly prevalent in aging societies such as Japan, Italy and Germany [
7], with Alzheimer’s disease ranked as the most common neurodegenerative disorder worldwide, followed by Parkinson’s disease [
6,
8,
9]. Between 2021 and 2023, WHO reports identified Alzheimer’s disease and other dementias among the top three causes of death in Great Britain [
10]. Pathophysiologically, dementia involves progressive neuronal degeneration, hippocampal and cortical atrophy, synaptic loss and the accumulation of neurotoxic proteins including amyloid-β plaques and tau neurofibrillary tangles [
11,
12,
13,
14]. These changes lead to cognitive decline, behavioral alterations and loss of independence, making dementia the leading cause of disability and death among neurological conditions [
15].
Dementia caregiving entails profound emotional, physical and social challenges. A large European survey in 2006 reported that one-third of caregivers provided more than 10 hours of daily care, regardless of dementia severity [
16]. More recently, a study of over 1,400 caregivers across five European countries revealed that nearly 20% received no information at diagnosis, 58% expressed persistent worry about the future, 34% reported depressive symptoms and many described loneliness as a major consequence of their role [
17].
Consistently, caregivers of individuals with dementia experience greater psychological distress than caregivers of other chronic conditions [
18,
19]. A meta-analysis demonstrated that dementia family caregivers are significantly more stressed and report more depressive symptoms and physical problems compared to other caregivers [
20]. Risk factors for heightened distress include demographic variables (female gender, older age, spouse or child relationship to the care recipient), lower socioeconomic status and limited social support [
21,
22,
23,
24]. The severity of the care recipient’s cognitive impairment, often measured by the Mini-Mental State Examination (MMSE), has also been shown to correlate directly with caregiver burden [
25].
Beyond distress, research has increasingly focused on the psychological well-being of caregivers, assessed across multiple domains such as autonomy, self-acceptance, personal growth and purpose in life using Ryff’s Psychological Well-Being Scale [
26,
27,
28]. Evidence suggests that well-being often declines as caregiving responsibilities intensify. For example, Wister et al. (2022) found that caregivers with lower well-being scores were more likely to develop depressive and anxiety symptoms, highlighting the importance of multidimensional assessments [
29]. Coping strategies are equally critical; caregivers who adopt adaptive strategies such as seeking social support or maintaining personal control exhibit better mental health outcomes, whereas reliance on maladaptive coping predicts poorer outcomes [
30,
31].
Depression and anxiety are the two most prevalent mental health concerns among caregivers. According to Pinquart and Sörensen (2007), caregivers consistently report higher levels of depression than non-caregivers, with the gap being most pronounced among those caring for dementia patients [
32]. Depression in caregivers is exacerbated by lack of social support, physical exhaustion and isolation [
33], while anxiety often stems from uncertainty about the future, financial strain and the overwhelming nature of caregiving responsibilities.
Existing research demonstrates that dementia caregiving is associated with profound psychological challenges, but also that individual, relational and socio-economic resources can shape outcomes. However, most studies treat caregivers as a homogeneous group, overlooking the possibility of latent subgroups that differ in their levels of depression, anxiety and well-being. Identifying such profiles is essential for developing tailored interventions. Moreover, socio-economic resources such as education and income may function as resilience factors that buffer against psychological burden, though evidence remains limited.
The present study addresses these gaps by applying Latent Profile Analysis (LPA) to depressive and anxiety symptoms among family caregivers of dementia patients, following three objectives: identifying distinct psychological profiles of caregivers, examining their associations with dimensions of psychological well-being and exploring whether education and income act as protective moderators.
2. Materials and Methods
This was a single-center, observational, analytical cross-sectional study. We included 73 family caregivers of patients diagnosed with dementia who accessed medical care for their care recipients between November 2023 and April 2024 in the Neurology–Psychiatry Department of the C.F.2 Clinical Hospital (Bucharest, Romania). Caregivers were eligible if they were ≥30 years old, a family member of the person with dementia, had provided care for at least six months, were currently caring for a patient with dementia and were able to understand and complete the study instruments. Of the 120 individuals who sought this service during the six-month period, 73 met the inclusion/exclusion criteria and were enrolled. Individuals who provided care to a person with dementia without being a family member and respondents who did not fully complete the questionnaires were excluded.
Data collection employed a battery of instruments, chosen to capture both psychological outcomes and relevant contextual factors. These included Ryff’s Psychological Well-Being Scales (54 items), the Patient Health Questionnaire-9 (PHQ-9), the COVI Anxiety Scale, the Mini-Mental State Examination (MMSE; extracted from medical records) and an Anthropological Questionnaire (AQ) specifically developed for this study to gather socio-demographic information.
Ryff’s Psychological Well-Being Scales (Romanian adaptation) [
26,
27,
34] were used to evaluate caregivers’ positive psychological functioning. The instrument consists of six conceptually established dimensions: autonomy, personal growth, positive relations, self-acceptance, purpose in life and environmental mastery. Each dimension is assessed using nine distinct items. Responses are rated on a 6-point Likert scale ranging from strongly disagree to strongly agree, with 28 items reverse-coded to control for acquiescence bias. Subscales can be analyzed separately, but they can also be aggregated into a higher-order well-being index. Previous studies have demonstrated the reliability, factorial validity and cross-cultural robustness of this measure, including in Romanian populations [
35,
36,
37,
38].
Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9). This widely used self-report measure is aligned with DSM-IV and DSM-5 diagnostic criteria for major depression. Scores are interpreted according to established clinical cut-offs: 5–9 = mild, 10–14 = moderate, 15–19 = moderately severe and 20–27 = severe depression. The PHQ-9 has been extensively validated in both clinical and community samples, consistently demonstrating strong psychometric properties [
39,
40,
41,
42,
43]. In Romania, several validation studies have confirmed its reliability and screening utility across diverse patient groups [
44].
Anxiety was evaluated using the COVI Anxiety Scale, a clinician-rated instrument designed to quantify the severity of anxiety symptoms. The scale categorizes scores into four severity levels: 3–5 = minimal or no anxiety, 6–8 = mild anxiety, 9–11 = moderate anxiety and 12–15 = severe anxiety. The COVI scale is recognized in both research and practice as a brief yet sensitive tool for the assessment of anxiety and it is frequently employed to guide treatment planning and targeted interventions [
45].
Cognitive functioning of the care recipients was assessed using the Mini-Mental State Examination (MMSE). This 30-item screening tool evaluates orientation, attention, memory and language abilities, yielding a total score between 0 and 30, with lower scores indicating greater cognitive impairment. A threshold of 24 or below is commonly used to suggest the presence of clinically significant impairment. In this study, MMSE scores were extracted directly from patients’ medical records under institutional ethics approval. Because the data were de-identified, separate patient consent was not required. The MMSE is one of the most extensively validated instruments in geriatric and neurocognitive assessment and remains a gold standard in the field [
46,
47,
48].
The Ryff scales, PHQ-9 and the AQ were self-administered by participants in a private setting within the physician’s office at C.F.2 Clinical Hospital. In contrast, the COVI Anxiety Scale was clinician-rated by the attending psychiatrist. On average, the full assessment procedure required approximately 45 minutes per participant. To ensure clarity and appropriateness of the socio-demographic instrument (AQ), a pilot test was conducted with 15 formal caregivers; their feedback was carefully reviewed and integrated into the final version of the questionnaire.
All procedures adhered to established ethical standards for research involving human participants. Written informed consent was obtained from all caregivers prior to their participation in the study. Only caregivers were required to sign consent forms, as data regarding the cognitive status of care recipients (MMSE scores) were retrieved exclusively from medical records. These data were used in a fully de-identified format, thereby ensuring participant confidentiality and eliminating the need for separate patient consent. .
The overall study protocol was reviewed and approved by the Ethics Committee of C.F.2 Clinical Hospital (Reference No. 1781/06.02.2023) and data collection commenced only after ethics approval had been granted.
To further safeguard ethical compliance, participants were informed about the purpose, procedures, potential risks and benefits of the study and were assured that their participation was entirely voluntary and could be withdrawn at any point without affecting their or their relatives’ access to medical care. Data were stored and analyzed in aggregate form only, thereby preventing the identification of individual participants.
Statistical analyses were performed in order to explore latent heterogeneity in caregivers’ affective symptomatology and to examine its associations with psychological well-being. Prior to modeling, all continuous variables were standardized (z-scores) to place them on a comparable metric and reduce scale-related biases.
To identify distinct caregiver subgroups, we conducted a Latent Profile Analysis (LPA) applied to depression (PHQ-9) and anxiety (COVI) scores. Competing models with one to five classes were estimated. Model adequacy was evaluated using multiple fit indices, with particular emphasis on the Bayesian Information Criterion (BIC) as the primary criterion for model selection and the Akaike Information Criterion (AIC) considered secondarily. Beyond statistical indices, model selection also considered the theoretical interpretability of the extracted profiles, the convergence stability across random starts and the practical relevance of the class solutions.
Once the optimal latent profile solution was established, group differences across profiles were tested using one-way analyses of variance (ANOVAs) for both PHQ-9 and COVI scores, followed by Tukey’s Honest Significant Difference (HSD) tests for pairwise comparisons. Effect sizes (η²) were calculated to assess the magnitude of observed differences.
In addition, Pearson correlation coefficients were computed to examine the associations between affective measures (PHQ-9, COVI) and the six Ryff dimensions of psychological well-being. These analyses were conducted to determine whether higher levels of depressive or anxiety symptoms were systematically related to lower well-being in specific domains.
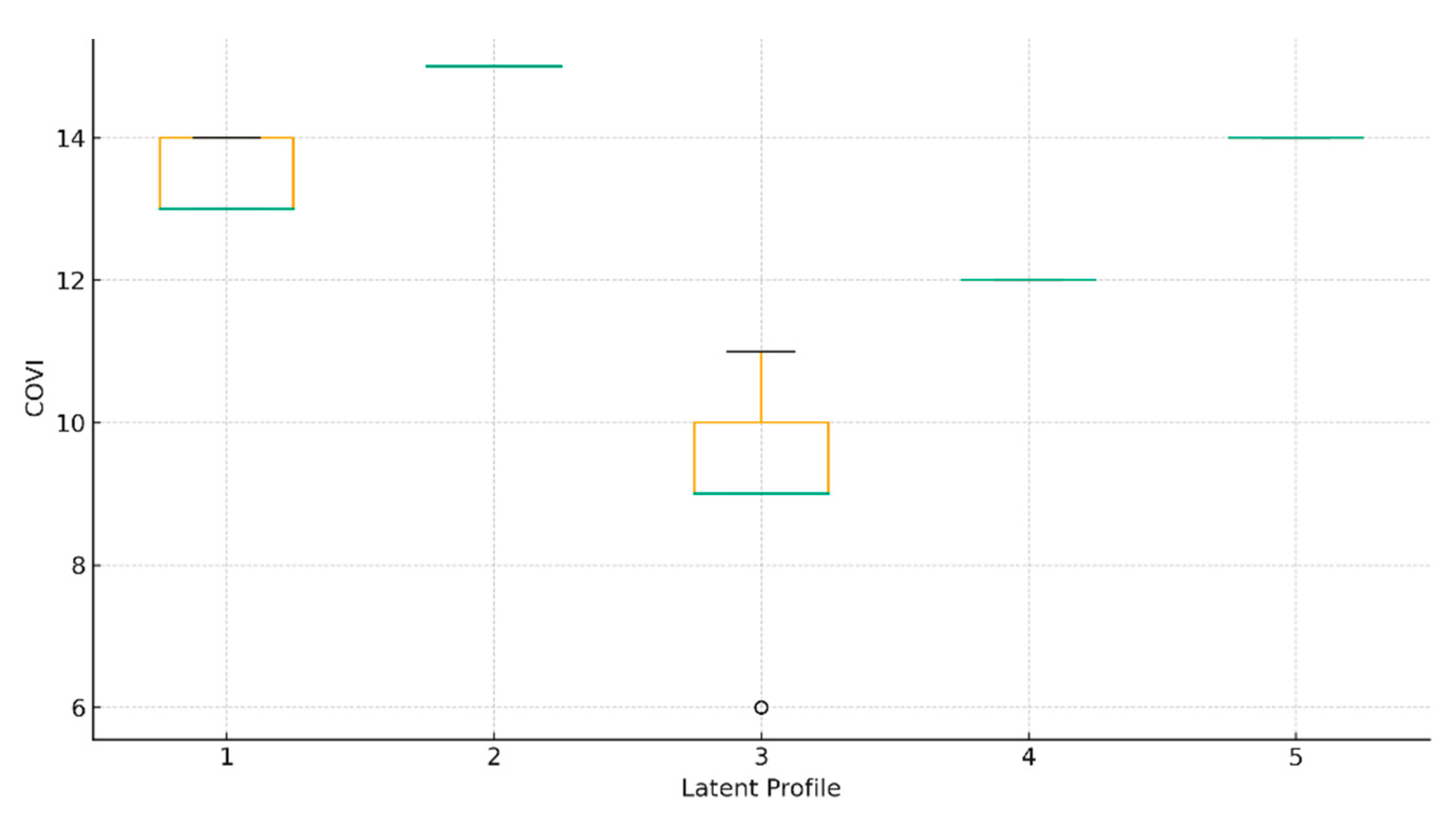
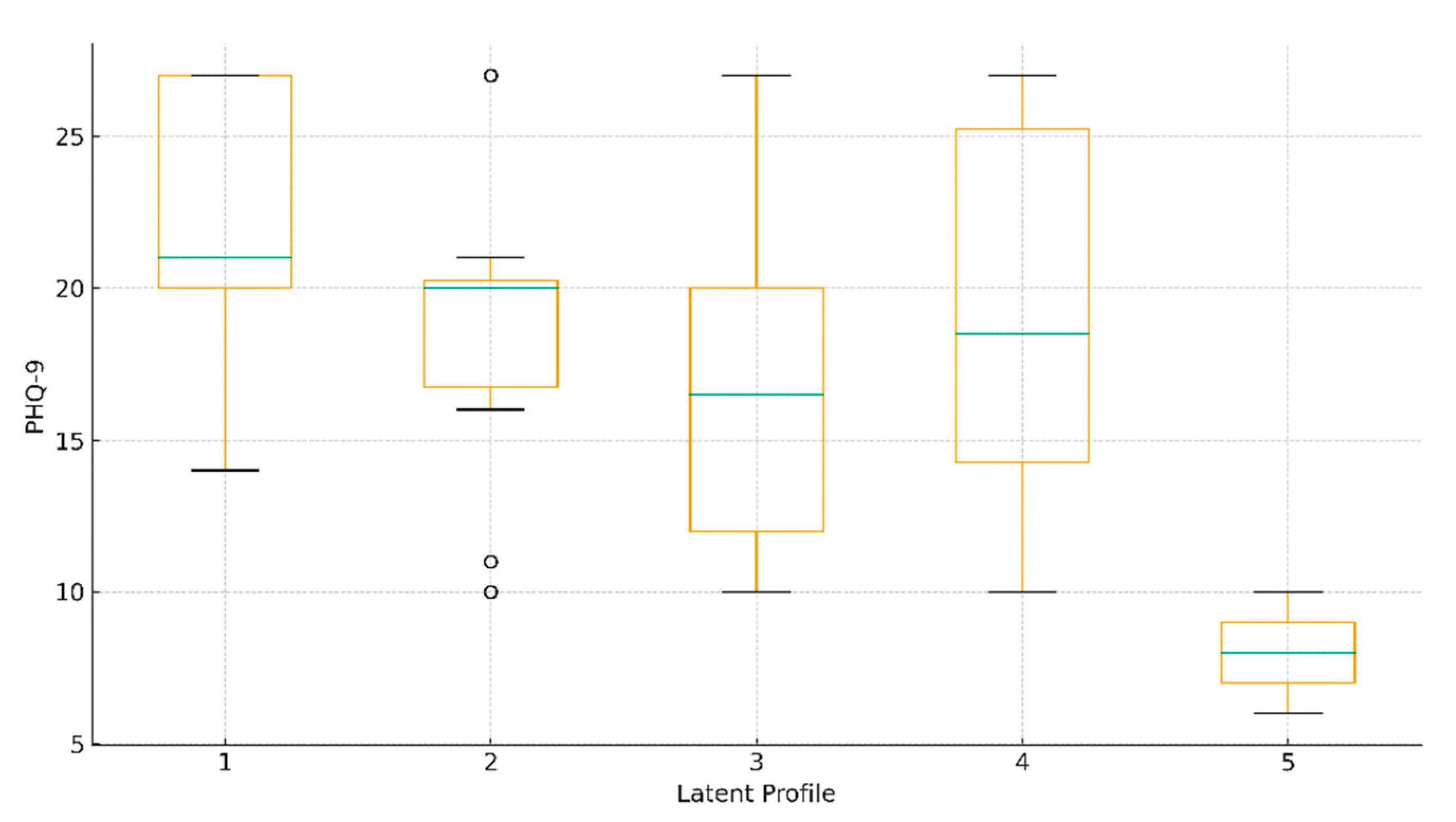
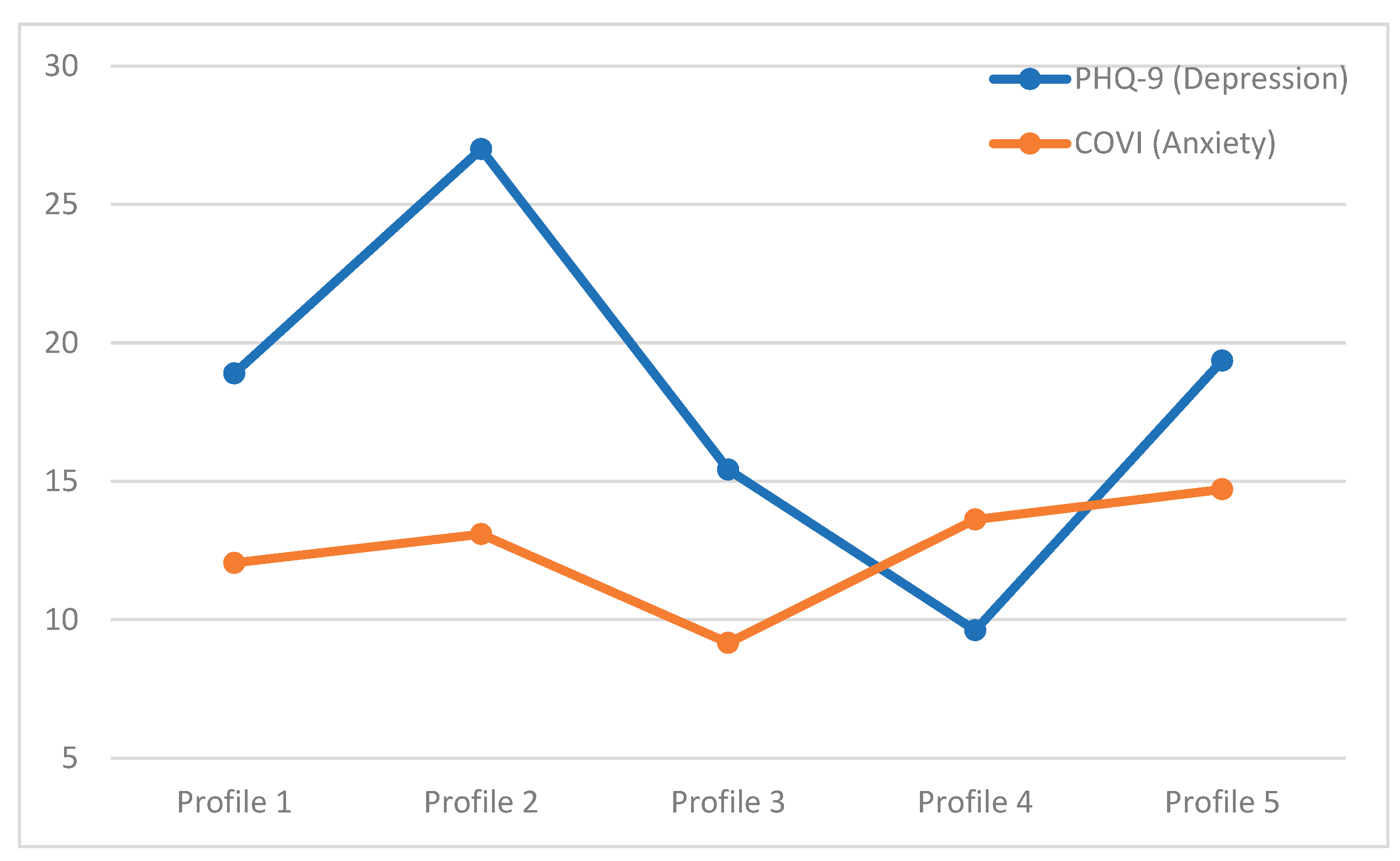
Finally, results were synthesized through a combination of tabular and graphical outputs. Descriptive statistics (means and standard deviations) for each latent profile were presented in tabular format. Boxplots were generated to illustrate the distribution of PHQ-9 and COVI scores across latent profiles and correlation results were displayed in summary tables to aid interpretation.
To explore the potential protective role of socio-economic resources, additional analyses were conducted with education and household income as moderators of the associations between caregivers’ affective symptoms and psychological well-being. The focus was on whether higher levels of education or income attenuated the negative impact of depressive (PHQ-9) and anxiety (COVI) symptoms on Ryff’s well-being dimensions.
3. Results
A total of 73 family caregivers met the inclusion criteria and completed the study protocol. The majority of participants were women (75.3%), reflecting the gendered nature of caregiving responsibilities commonly observed in dementia care. Caregivers’ ages ranged from 34 to 78 years, with a mean age of 57.1 years (SD = 10.4), indicating a predominantly middle-aged to older adult sample. Educational backgrounds were heterogeneous, spanning from secondary education to higher education, while household income varied considerably, with many participants reporting modest resources. Most caregivers resided in urban areas, although a notable proportion came from rural settings, thereby reflecting the mixed socio-demographic composition of the catchment area of the C.F.2 Clinical Hospital.
In terms of their caregiving role, all participants were close family members of the care recipients, most frequently adult children or spouses. The minimum caregiving duration was six months, but in many cases, the caregiving relationship had extended for several years, highlighting the chronic and demanding nature of dementia care in this population.
With respect to the cognitive functioning of the patients, as measured by the Mini-Mental State Examination (MMSE), most were documented as presenting moderate to severe impairment, consistent with the advanced clinical stages at which families typically seek specialized neurological and psychiatric services. These contextual factors underscore the considerable emotional, cognitive and practical demands placed upon family caregivers in the present study.
To identify distinct psychological subgroups among caregivers, a latent profile analysis (LPA) was performed on standardized scores of depression (PHQ-9) and anxiety (COVI). Models with one to five classes were estimated and fit indices are reported in
Table 1.
Although all three indices (AIC, BIC, SABIC) favored the four-profile solution as the optimal statistical fit, with the lowest values observed for the 4-class model, upon careful analysis, the five-profile solution was chosen for it provided clinically meaningful distinctions between caregiver subgroups, separating profiles characterized by “low depression with severe anxiety” versus “moderately severe depression with very severe anxiety.” For this reason and consistent with recommendations that interpretability and theoretical plausibility should complement statistical criteria in mixture modeling, the five-profile solution was retained for subsequent analyses.The five profiles exhibited marked differences in affective symptomatology (
Table 2).
Group differences were statistically robust.. For depression, the omnibus ANOVA was significant (F(4, 68) = 36.16, p < .001, η² = .68). For anxiety, differences were even more pronounced (F(4, 68) = 73.33, p < .001, η² = .81). Boxplots illustrating the distribution of PHQ-9 and COVI scores are shown in
Figure 1 and
Figure 2 and mean profiles in
Figure 3.
The six dimensions of Ryff’s Psychological Well-Being Scales were compared across the five profiles. A trend was observed for purpose in life (F(4, 68) = 1.98, p = .107, η² = .10), with lower scores among profiles characterized by severe depression and anxiety.
Pearson correlations further examined associations between affectivity and well-being (
Table 3). Higher PHQ-9 scores were weakly but significantly related to lower self-acceptance (r = .25, p = .033) and lower autonomy (r = .24, p = .044). Other associations with PHQ-9 were nonsignificant. COVI anxiety scores showed no meaningful correlations with any of the well-being dimensions (all p > .10).
To examine whether socio-economic resources buffer the psychological burden of caregiving, we tested education and household income as moderators of the links between affective symptoms and psychological well-being. We created an overall well-being index (Ryff_total = mean of the six Ryff dimensions) and also examined three theoretically salient subscales (self-acceptance, autonomy, purpose in life). Education was coded as an ordered factor (Secondary < High school < Higher education) and income as Up to 400 EUR < 400–1000 EUR < Over 1000 EUR. Continuous variables (PHQ-9, COVI, outcomes) were z-standardized. Robust OLS models (HC3 SEs) included the two interaction terms per predictor (e.g., PHQ-9 × education, PHQ-9 × income), estimated separately for depression and anxiety for each outcome.
Across outcomes, none of the interaction terms reached statistical significance at α = .05. In other words, with this sample (N = 73), education and income did not significantly attenuate the association of depression or anxiety with psychological well-being. A compact summary of interaction estimates can be found in
Table 4 (dependent variables: Ryff_total, Self-acceptance, Autonomy, Purpose in life).
4. Discussion
The present study applied latent profile analysis to depressive and anxiety symptoms among family caregivers of patients with dementia, revealing five distinct psychological subgroups. These findings confirm that caregivers are not a homogeneous population but rather exhibit diverse constellations of emotional distress, underscoring the importance of individualized assessment and intervention.
Interpretation of caregiver profiles
Two of the profiles were characterized by convergent high distress: Profile 2 (severe depression + severe anxiety) and Profile 5 (moderately severe depression + very severe anxiety). These groups represent caregivers at the highest risk of clinical psychopathology, consistent with previous reports showing that comorbid depressive and anxiety symptoms are common among caregivers exposed to long-term burden, role captivity and reduced social support (Pinquart & Sörensen, 2003; Joling et al., 2015). Caregivers in these categories are particularly vulnerable to burnout, impaired physical health and reduced caregiving capacity.
Other profiles reflected discordant patterns of distress. Profile 4 (low depression + severe anxiety) illustrates caregivers who may not experience pervasive depressive mood but who present elevated physiological or cognitive anxiety. This pattern resonates with evidence that hypervigilance and anticipatory worry often dominate early stages of caregiving, even before depressive symptoms become entrenched. Conversely, Profile 3 (moderate depression + low anxiety) suggests a subgroup experiencing emotional blunting, demoralization, or fatigue without overt anxiety. Such distinctions are clinically important because they suggest that depression and anxiety, while correlated, may manifest independently in caregivers, requiring different screening and therapeutic strategies.
Profile 1 (moderate depression + elevated anxiety) represented the largest group, capturing nearly one-third of the sample. This profile may reflect the “typical” caregiver experience: sustained moderate levels of emotional distress that are clinically relevant but may not always reach psychiatric thresholds. These caregivers remain at risk for progression to more severe states if stressors intensify or resources decline.
Implications for caregiver well-being
Interestingly, psychological well-being, as measured by Ryff’s dimensions, did not differ significantly across profiles. Only a non-significant trend emerged for purpose in life, which tended to be lower in high-distress groups. This suggests that while depression and anxiety clearly discriminate subgroups, well-being dimensions may be more stable or influenced by other factors such as personality, coping style, or cultural expectations of family caregiving. Weak but significant correlations indicated that higher depression was associated with lower self-acceptance and autonomy, in line with prior research linking affective disorders to impaired self-evaluation and diminished sense of agency.
Resilience through education and income
Exploratory moderation models suggested a potential buffering effect of education on the relationship between depressive symptoms and psychological well-being, particularly for self-acceptance and autonomy. Among caregivers with lower education, higher depression scores tended to be associated with lower well-being, whereas this pattern appeared weaker among those with higher education. However, these effects did not reach conventional levels of statistical significance and should be interpreted as indicative rather than conclusive. No significant moderating effects of education were observed for anxiety symptoms, suggesting that educational resources are more protective against depressive than anxious distress.
A similar descriptive pattern was observed for income, where caregivers with lower income showed greater declines in purpose in life as depressive symptoms increased. Yet, these effects were not statistically robust. Thus, while education and income may represent resilience resources, our findings are best interpreted as preliminary trends that warrant replication in larger samples.
This finding points to the potential role of financial resources in maintaining a future orientation and meaning-making capacity under conditions of psychological strain. Income did not significantly moderate the association between anxiety and well-being, although a descriptive trend suggested that higher income may dampen the impact of anxiety on environmental mastery.
Taken together, these analyses point to the possible importance of socio-economic resources as resilience factors, results similar to other studies [
49,
50,
51,
52,
53,
54,
55,
56,
57,
58], although moderation effects were not statistically significant in this sample. Education and income may play a role in shaping caregiver resilience, but our results should be regarded as exploratory trends. Larger, adequately powered studies are needed to clarify whether these resources reliably buffer the impact of depressive and anxiety symptoms on psychological well-being.
These findings underscore that interventions to support caregivers should consider not only psychological risk but also the structural and resource-based context in which caregiving occurs
Clinical and practical significance
From a clinical perspective, these findings highlight the necessity of differentiated approaches to caregiver support. Routine screening for both depressive and anxiety symptoms should be implemented in clinical settings serving dementia patients. Moreover, interventions should be tailored. Profiles 2 and 5 (caregivers with combined severe depression and anxiety) may benefit from comprehensive psychiatric care, including pharmacotherapy and psychotherapy. Those with predominant anxiety (Profile 4) might benefit more from stress management, relaxation training, or cognitive-behavioral interventions targeting anxiety and caregivers moderate depression but low anxiety (Profile 3) may be more responsive to behavioral activation and social support interventions.
Such personalized approaches could prevent escalation of symptoms and help sustain caregivers’ long-term capacity to provide care.
5. Conclusions
This study demonstrates that family caregivers of dementia patients fall into five distinct psychological profiles, ranging from moderate mixed distress to severe comorbid depression and anxiety. These heterogeneous patterns of affective symptoms underscore the need for individualized screening and intervention strategies in caregiver support programs. Addressing caregiver mental health is not only critical for their own well-being but also for the sustained quality of care delivered to patients with dementia.
6. Limitations and Future Directions
Several limitations warrant consideration. The study was based on a single-center, cross-sectional design, which limits generalizability and precludes causal inferences. The sample size, though sufficient for exploratory LPA, was modest and may have constrained statistical power for detecting differences in well-being outcomes. Additionally, the use of self-report measures, although validated, may be subject to reporting bias. Future research should replicate these findings in larger, multi-center cohorts, employ longitudinal designs to track profile stability over time and explore moderators such as coping strategies, resilience and social support.
Author Contributions
Conceptualization, C.S.G., L.F.T. and S.T.; formal analysis, C.S.G., L.F.T. and S.T.; investigation, L.F.T.; methodology, C.S.G., L.F.T. and S.T.; software, C.S.G., L.F.T. and S.T.; supervision, C.S.G., L.F.T. and S.T.; validation C.S.G., L.F.T. and S.T.; writing—original draft, C.S.G., L.F.T. and S.T.; writing—review and editing, C.S.G., L.F.T. and S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of C.F.2 Clinical Hospital (Ref. Number: 1781; and the approval date is 6 February 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- 2024 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2024, 20, 3708–3821. [CrossRef] [PubMed]
- Stallard, P.J.E.; Ukraintseva, S.V.; Doraiswamy, P.M. Changing Story of the Dementia Epidemic. JAMA 2025, 333, 1579. [Google Scholar] [CrossRef] [PubMed]
- Mukadam, N.; Wolters, F.J.; Walsh, S.; Wallace, L.; Brayne, C.; Matthews, F.E.; Sacuiu, S.; Skoog, I.; Seshadri, S.; Beiser, A.; et al. Changes in Prevalence and Incidence of Dementia and Risk Factors for Dementia: An Analysis from Cohort Studies. Lancet Public Health 2024, 9, e443–e460. [Google Scholar] [CrossRef]
- Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 18 May 2025).
- Licher, S.; Darweesh, S.K.L.; Wolters, F.J.; Fani, L.; Heshmatollah, A.; Mutlu, U.; Koudstaal, P.J.; Heeringa, J.; Leening, M.J.G.; Ikram, M.K.; et al. Lifetime Risk of Common Neurological Diseases in the Elderly Population. J. Neurol. Neurosurg. Psychiatry 2019, 90, 148–156. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2023: OECD Indicators; Health at a Glance; OECD: Paris, France, 2023; ISBN 978-92-64-95793-0. [Google Scholar]
- Dorsey, E.R.; Sherer, T.; Okun, M.S.; Bloem, B.R. The Emerging Evidence of the Parkinson Pandemic. J. Park. Dis. 2018, 8, S3–S8. [Google Scholar] [CrossRef]
- Furdu-Lunguț, E.; Antal, C.; Turcu, S.; Costea, D.-G.; Mitran, M.; Mitran, L.; Diaconescu, A.-S.; Novac, M.-B.; Gorecki, G.-P. Study on Pharmacological Treatment of Impulse Control Disorders in Parkinson’s Disease. J. Clin. Med. 2024, 13, 6708. [Google Scholar] [CrossRef]
- United Kingdom of Great Britain and Northern Ireland. Available online: https://data.who.int/countries/826 (accessed on 16 May 2025).
- Ye, J.; Wan, H.; Chen, S.; Liu, G.-P. Targeting Tau in Alzheimer’s Disease: From Mechanisms to Clinical Therapy. Neural Regen. Res. 2024, 19, 1489–1498. [Google Scholar] [CrossRef]
- Rapoport, M.; Dawson, H.N.; Binder, L.I.; Vitek, M.P.; Ferreira, A. Tau Is Essential to β-Amyloid-Induced Neurotoxicity. Proc. Natl. Acad. Sci. USA 2002, 99, 6364–6369. [Google Scholar] [CrossRef]
- Hardy, J.; Selkoe, D.J. The Amyloid Hypothesis of Alzheimer’s Disease: Progress and Problems on the Road to Therapeutics. Science 2002, 297, 353–356. [Google Scholar] [CrossRef]
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.; et al. NIA-AA Research Framework: Toward a Biological Definition of Alzheimer’s Disease. Alzheimer’s Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef]
- Georges, J.; Jansen, S.; Jackson, J.; Meyrieux, A.; Sadowska, A.; Selmes, M. Alzheimer’s Disease in Real Life—The Dementia Carer’s Survey. Int. J. Geriat. Psychiatry 2008, 23, 546–551. [Google Scholar] [CrossRef]
- Alzheimer Europe. 2006 Alzheimer Europe Survey: Who Cares? The State of Dementia Care in Europe; Alzheimer Europe: Lux-embourg, 2006; p. 12. [Google Scholar]
- Alzheimer Europe. European Carers’ Report 2018: Carers’ Experiences of Diagnosis in Five European Countries; Alzheimer Europe: Luxembourg, 2018; ISBN 978-999959-995-2-0. [Google Scholar]
- Pinquart, M.; Sörensen, S. Differences between Caregivers and Noncaregivers in Psychological Health and Physical Health: A Meta-Analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef] [PubMed]
- Abdelhalim, D.S.; Ahmed, M.M.; Hussein, H.A.; Khalaf, O.O.; Sarhan, M.D. Burden of Care, Depression and Anxiety Among Family Caregivers of People with Dementia. J. Prim. Care Community Health 2024, 15, 21501319241288029. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.-T. Dementia Caregiver Burden: A Research Update and Critical Analysis. Curr. Psychiatry Rep. 2017, 19, 64. [Google Scholar] [CrossRef] [PubMed]
- Grande, G.; Shield, T.; Bayliss, K.; Rowland, C.; Flynn, J.; Bee, P.; Hodkinson, A.; Panagioti, M.; Farquhar, M.; Harris, D.; et al. Understanding the Potential Factors Affecting Carers’ Mental Health during End-of-Life Home Care: A Meta Synthesis of the Research Literature. Health Soc. Care Deliv. Res. 2022, 8, 1–78. [Google Scholar] [CrossRef]
- Pacheco Barzallo, D.; Schnyder, A.; Zanini, C.; Gemperli, A. Gender Differences in Family Caregiving. Do Female Caregivers Do More or Undertake Different Tasks? BMC Health Serv. Res. 2024, 24, 730. [Google Scholar] [CrossRef]
- Sörensen, S.; Conwell, Y. Issues in Dementia Caregiving: Effects on Mental and Physical Health, Intervention Strategies and Research Needs. Am. J. Geriatr. Psychiatry 2011, 19, 491–496. [Google Scholar] [CrossRef]
- González-Fernández, M.; Davis, C.; Molitoris, J.J.; Newhart, M.; Leigh, R.; Hillis, A.E. Formal Education, Socioeconomic Status and the Severity of Aphasia After Stroke. Arch. Phys. Med. Rehabil. 2011, 92, 1809–1813. [Google Scholar] [CrossRef]
- Brodaty, H.; Donkin, M. Family Caregivers of People with Dementia. Dialogues Clin. Neurosci. 2009, 11, 217–228. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness Is Everything, or Is It? Explorations on the Meaning of Psychological Well-Being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Ryff, C.D. Beyond Ponce de Leon and Life Satisfaction: New Directions in Quest of Successful Ageing. Int. J. Behav. Dev. 1989, 12, 35–55. [Google Scholar] [CrossRef]
- Ryff, C.D.; Keyes, C.L.M. The Structure of Psychological Well-Being Revisited. J. Personal. Soc. Psychol. 1995, 69, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Wister, A.; Li, L.; Mitchell, B.; Wolfson, C.; McMillan, J.; Griffith, L.E.; Kirkland, S.; Raina, P. ; Canadian Longitudinal Study on Aging (CLSA) Team; Costa, A. ; et al. Levels of Depression and Anxiety Among Informal Caregivers During the COVID-19 Pandemic: A Study Based on the Canadian Longitudinal Study on Aging. J. Gerontol. Ser. B 2022, 77, 1740–1757. [Google Scholar] [CrossRef]
- Ashley, N.R.; Kleinpeter, C.H. Gender Differences in Coping Strategies of Spousal Dementia Caregivers. J. Hum. Behav. Soc. Environ. 2002, 6, 29–46. [Google Scholar] [CrossRef]
- Geiger, J.R.; Wilks, S.E.; Lovelace, L.L.; Chen, Z.; Spivey, C.A. Burden Among Male Alzheimer’s Caregivers: Effects of Distinct Coping Strategies. Am. J. Alzheimer’s Dis. Other Dement. 2015, 30, 238–246. [Google Scholar] [CrossRef]
- Pinquart, M.; Sorensen, S. Correlates of Physical Health of Informal Caregivers: A Meta-Analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2007, 62, P126–P137. [Google Scholar] [CrossRef]
- Schulz, R.; Martire, L.M. Family Caregiving of Persons with Dementia: Prevalence, Health Effects and Support Strategies. Am. J. Geriatr. Psychiatry 2004, 12, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Costea-Bărluțiu, C.; Bălaș-Baconschi, C.; Hathazi, A. Romanian Adaptation of the Ryff’s Psychological Well-Being Scale: Brief Report of the Factor Structure and Psychometric Properties. J. Evid.-Based Psychother. 2018, 18, 21–34. [Google Scholar] [CrossRef]
- Luştrea, A.; Ghazi, L.A.; Predescu, M. Adapting and Validating Ryff`s Psychological Well-Being Scale on Romanian Student Population. Educ. 21, 2018, 16, 118. [Google Scholar] [CrossRef]
- García, M.J.; Del Valle, M.V.; López Morales, H.; Urquijo, S. Propiedades Psicométricas de La Escala de Bienestar Psicológico de Ryff En Argentina. Cienc. Psicol. 2024, 18, e–3739. [Google Scholar] [CrossRef]
- Ruini, C.; Ottolini, F.; Rafanelli, C.; Ryff, C.; Fava, G.A. La Validazione Italiana Delle Psychological Well-Being Scales (PWB). Riv. Psichiatr. 2003, 38, 117–130. [Google Scholar]
- Van Dierendonck, D. The Construct Validity of Ryff’s Scales of Psychological Well-Being and Its Extension with Spiritual Well-Being. Personal. Individ. Differ. 2004, 36, 629–643. [Google Scholar] [CrossRef]
- Bains, N.; Abdijadid, S. Major Depressive Disorder. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Sawaya, H.; Atoui, M.; Hamadeh, A.; Zeinoun, P.; Nahas, Z. Adaptation and Initial Validation of the Patient Health Ques-tionnaire—9 (PHQ-9) and the Generalized Anxiety Disorder—7 Questionnaire (GAD-7) in an Arabic Speaking Lebanese Psychiatric Outpatient Sample. Psychiatry Res. 2016, 239, 245–252. [Google Scholar] [CrossRef]
- Huang, F.Y.; Chung, H.; Kroenke, K.; Delucchi, K.L.; Spitzer, R.L. Using the Patient Health Questionnaire-9 to Measure De-pression among Racially and Ethnically Diverse Primary Care Patients. J. Gen. Intern. Med. 2006, 21, 547–552. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Lipman, R.S.; Covi, L.; Downing, R.; Fisher, S.; Kahn, R.; McNair, D.; Rickels, K.; Smith, V. Pharmacotherapy of Anxiety and Depression. Psychopharmacol. Bull. 1981, 17, 91–103. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-Mental State. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The Mini-Mental State Examination: A Comprehensive Review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Monroe, T.; Carter, M. Using the Folstein Mini Mental State Exam (MMSE) to Explore Methodological Issues in Cognitive Aging Research. Eur. J. Ageing 2012, 9, 265–274. [Google Scholar] [CrossRef]
- García-Mochón, L.; Peña-Longobardo, L.M.; Del Río-Lozano, M.; Oliva-Moreno, J.; Larrañaga-Padilla, I.; García-Calvente, M.D.M. Determinants of Burden and Satisfaction in Informal Caregivers: Two Sides of the Same Coin? The CUIDAR-SE Study. Int. J. Environ. Res. Public Health 2019, 16, 4378. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Echeverria, D.; Yi, J.; Phillips, P.E.M.; Young, H.; Siegler, I.C. Psychophysiological Mediators of Caregiver Stress and Differential Cognitive Decline. Psychol. Aging 2005, 20, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Cejalvo, E.; Martí-Vilar, M.; Merino-Soto, C.; Aguirre-Morales, M.T. Caregiving Role and Psychosocial and Individual Factors: A Systematic Review. Healthcare 2021, 9, 1690. [Google Scholar] [CrossRef] [PubMed]
- Romão, M.E.; Setti, I.; Alfano, G.; Barello, S. Exploring Risk and Protective Factors for Burnout in Professionals Working in Death-Related Settings: A Scoping Review. Public Health 2025, 241, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Haro, J.M.; Kahle-Wrobleski, K.; Bruno, G.; Belger, M.; Dell’Agnello, G.; Dodel, R.; Jones, R.W.; Reed, C.C.; Vellas, B.; Wimo, A.; et al. Analysis of Burden in Caregivers of People with Alzheimer’s Disease Using Self-Report and Supervision Hours. J. Nutr. Health Aging 2014, 18, 677–684. [Google Scholar] [CrossRef]
- Mahoney, R.; Regan, C.; Katona, C.; Livingston, G. Anxiety and Depression in Family Caregivers of People With Alzheimer Disease: The LASER-AD Study. Am. J. Geriatr. Psychiatry 2005, 13, 795–801. [Google Scholar] [CrossRef]
- Chiao, C.-Y.; Wu, H.-S.; Hsiao, C.-Y. Caregiver Burden for Informal Caregivers of Patients with Dementia: A Systematic Review. Int. Nurs. Rev. 2015, 62, 340–350. [Google Scholar] [CrossRef]
- Liang, X.; Guo, Q.; Luo, J.; Li, F.; Ding, D.; Zhao, Q.; Hong, Z. Anxiety and Depression Symptoms among Caregivers of Care-Recipients with Subjective Cognitive Decline and Cognitive Impairment. BMC Neurol. 2016, 16, 191. [Google Scholar] [CrossRef]
- Rada, C. Factors Associated with Depression in Middle-Aged and Elderly People in Romania. Psichologija 2020, 61, 33–50. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and Mental Health Effects of Family Caregiving. Am. J. Nurs. 2008, 108, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Tatomirescu, L. F. , Glavce, C. S., Prada, G. I., Borosanu, A., & Turcu, S. (2025). Socio-Demographic Factors Linked to Psychological Well-Being in Dementia Caregivers. Healthcare, 13(17), 2235. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).