Submitted:
09 September 2025
Posted:
09 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Related Works
3. Integrated Patient Decision Support System - Architecture and Methodology
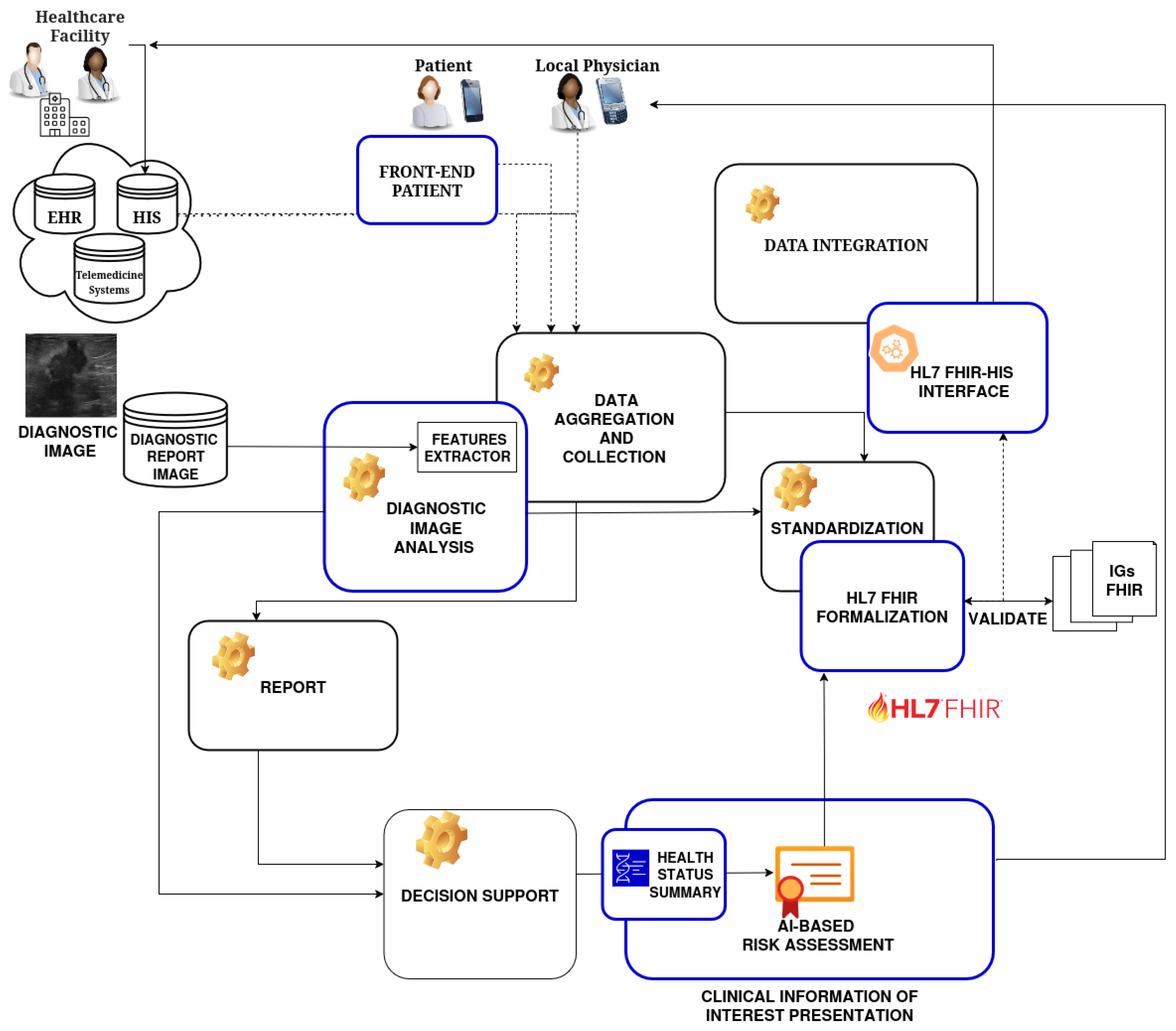
3.1. Architecture
-
Front-end PatientIt allows the patient to independently collect a range of anamnestic information (possibly specific to the clinical condition). The module allows for the management of data obtained by a form presented to the patient for the collection of medical history and other relevant information (allergies, medication, family history, symptoms, etc.). This module also allows the patient to retrieve any information present in the system through interaction with the HL7 FHIR-HIS interface module.
-
Diagnostic Image Analysis Module (DIAM)It performs processing and analysis of diagnostic images (e.g., detection, segmentation, classification, feature extraction) using Machine Learning algorithms or specific analysis tools. The aim of this module is to return an AI-based risk assessment.
-
HL7 FHIR Formalization ModuleThis module allows for formalizing, through international standard HL7 FHIR profiles, the data provided by the patient during the anamnesis phase (coming from the patient’s anamnesis form), and the results of image analysis (from the DIAM). This module uses the FHIR profiles and resources (e.g., Patient, Observation, Diagnostic Report, Allergy Intolerance, Medication Statement), which are appropriately defined to ensure compliance with FHIR standards. It manages the creation of FHIR resources and carries out validation for the aim of proposed architecture.
-
Clinical Information of Interest Presentation Module (CIIPM)This module allows identifying and collecting all and only the clinical information of interest for a specific diagnosis. It thus enables the presentation of an integrated and intuitive view of the information: Personal data, structured medical history, and image analysis results.
-
Health Status Summary ModuleIt applies logical rules and algorithms to extract and analyze integrated data (history, image results, other available data), and generates a concise summary of the patient’s health status, highlighting key information, potential risks (AI-based risk assessment), and recommendations.
-
HL7 FHIR-HIS InterfaceIt enables the CIIPM to communicate with the existing platform (EHR) using the HL7 FHIR standard, and supports FHIR operations such as Create, Read, Update of Patient resources, Observation, Diagnostic Report, and other relevant ones.
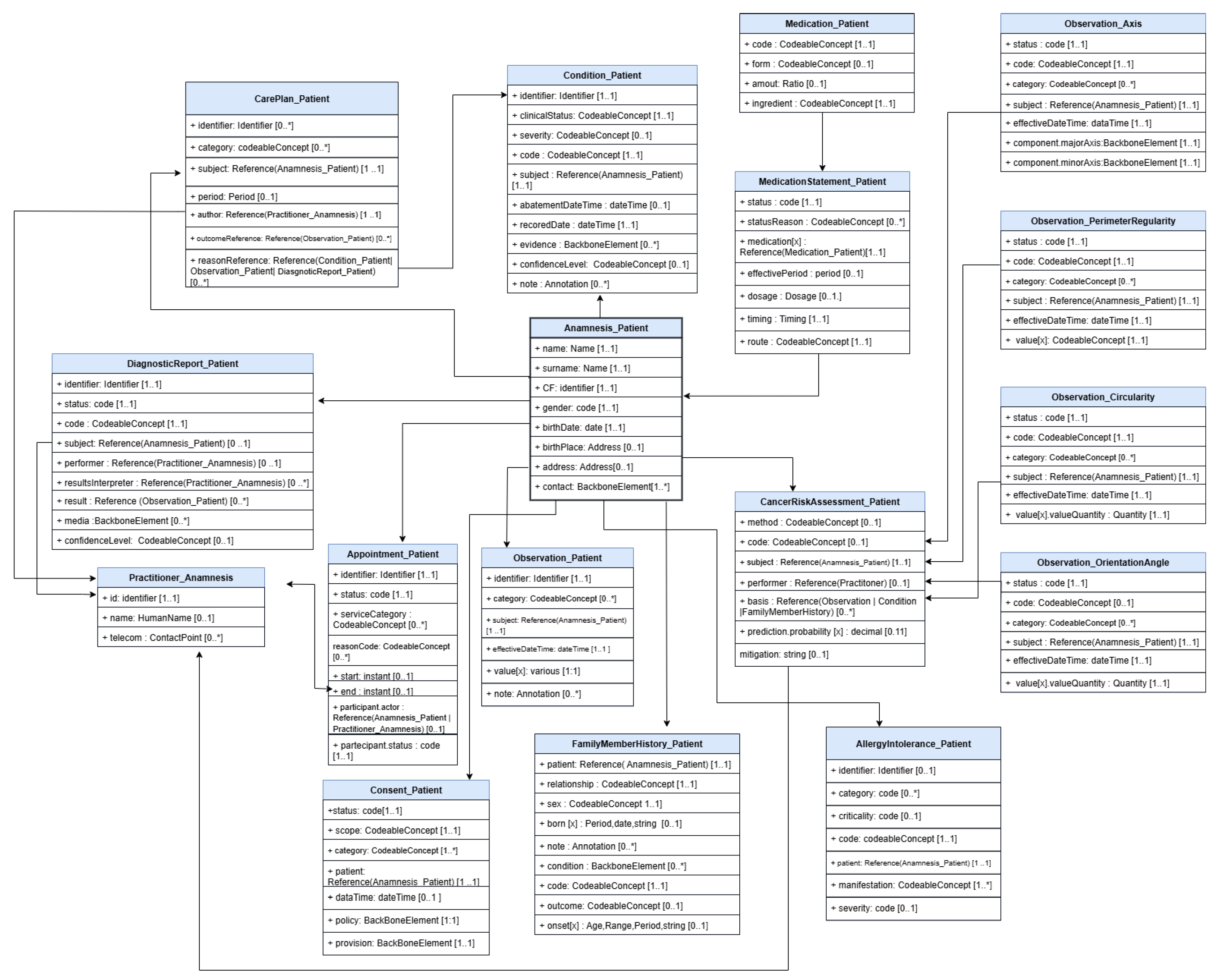
3.1.1. Data Model
3.2. Architecture Modules Details
3.2.1. Front-End Patient
3.2.2. Diagnostic Image Analysis Module (DIAM)
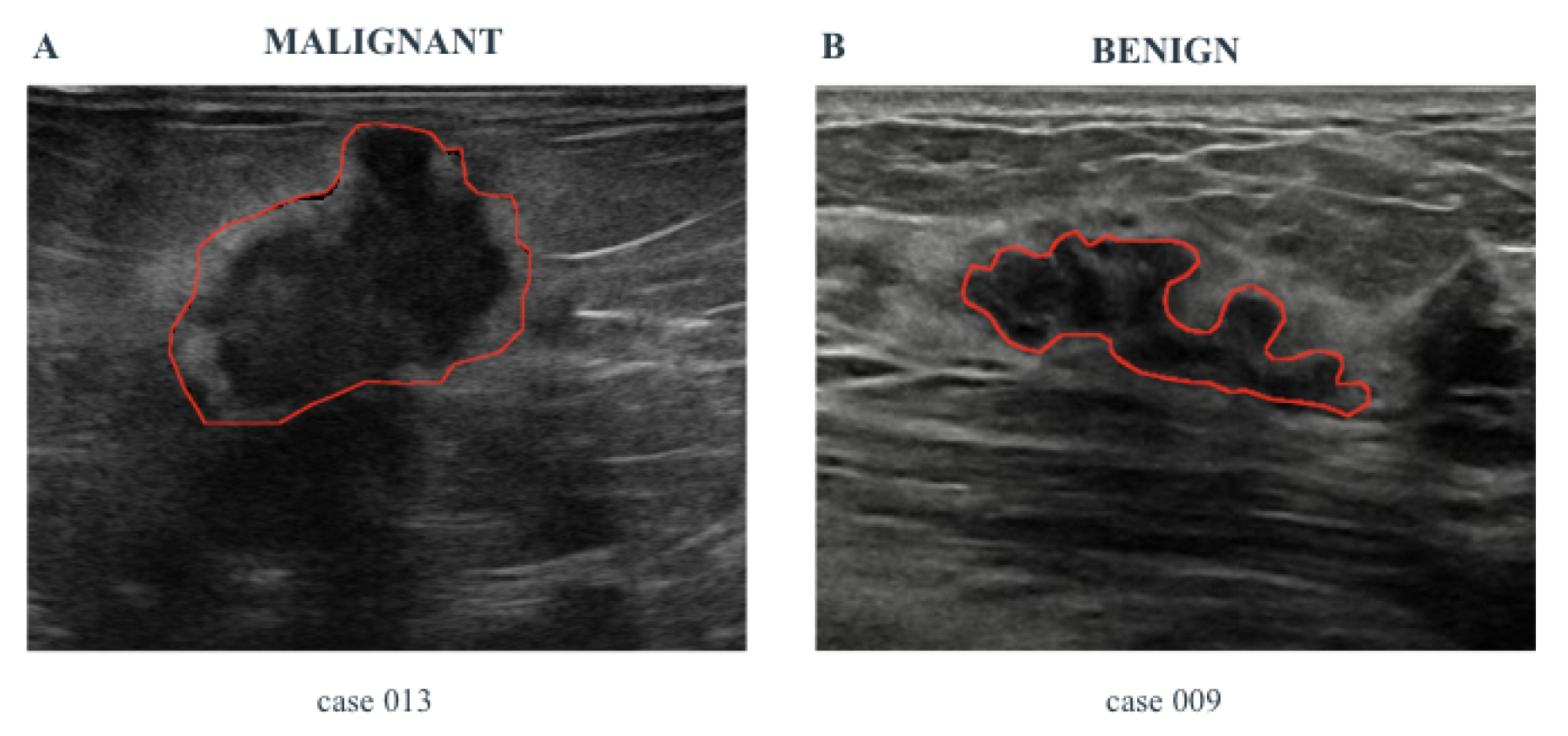
- Some specific features related to the pathology, namely Pathological Features (PF), are automatically extracted from the images, by using properly designed Computer Vision algorithms. These features are shown to the healthcare professionals and are useful to support the diagnosis.
- A risk assessment, computed by using suitably designed ML algorithms. For the computation of AI-based risk assessment, the ML methods use a set of features automatically extracted from ultrasound images, larger than PF, and called Hand-crafted Features (HF).
3.2.3. HL7 FHIR Formalization Module (HFFM)
- Anamnestic data: information provided directly by the patient through the Front-end Patient module. This includes, for example, self-reported symptom medical conditions, self-reported symptoms, etc..
- Clinical information derived from diagnostic images: includes results obtained through the automated analysis of diagnostic images (e.g., ultrasound images) by the DIAM. This information is then translated into formalized clinical observations according to the HL7 FHIR standard.
3.2.4. Clinical Information of Interest Presentation Module (CIIPM)
3.2.5. Health Status Summary Module
3.2.6. HL7 FHIR - HIS Interface
4. Case Study
4.1. DIAM
| Accuracy | Precision | Recall | F1-score | |
|---|---|---|---|---|
| DT | ||||
| MLP | 0.9767 | 0.9746 | 0.9729 | 0.9736 |
| NB | ||||
| RF |
4.2. HFFM
5. “InferCare” Android Application
5.1. IPDSS Functional Requirements
| Requirement ID | Description |
|---|---|
| FR01 | IPDSS shall enable patients to complete a structured form capturing personal data, teleconsultation history, family medical history, allergies, current medications, lifestyle habits, ongoing symptoms, and other clinically relevant information necessary for initial assessment. |
| FR02 | The form shall support multiple input types, including free text fields, multiple-choice options, checkboxes, and date pickers, to ensure flexibility and completeness of data collection. |
| FR03 | IPDSS shall implement client-side validation mechanisms to ensure data consistency, accuracy, and completeness before submission. |
| FR04 | IPDSS shall allow patients to save their progress during form completion and resume the process at a later time without data loss. |
| FR05 | IPDSS shall ensure the confidentiality and integrity of the submitted information during data transmission through secure communication protocols (e.g., HTTPS, encryption). |
| FR06 | A secure user authentication mechanism shall be provided (where applicable) to control access to the form, particularly when enabling partial form saving or editing features. |
| FR07 | IPDSS shall be responsive and accessible across various devices, including tablets and smartphones, ensuring usability and inclusivity. |
5.2. "InferCare"
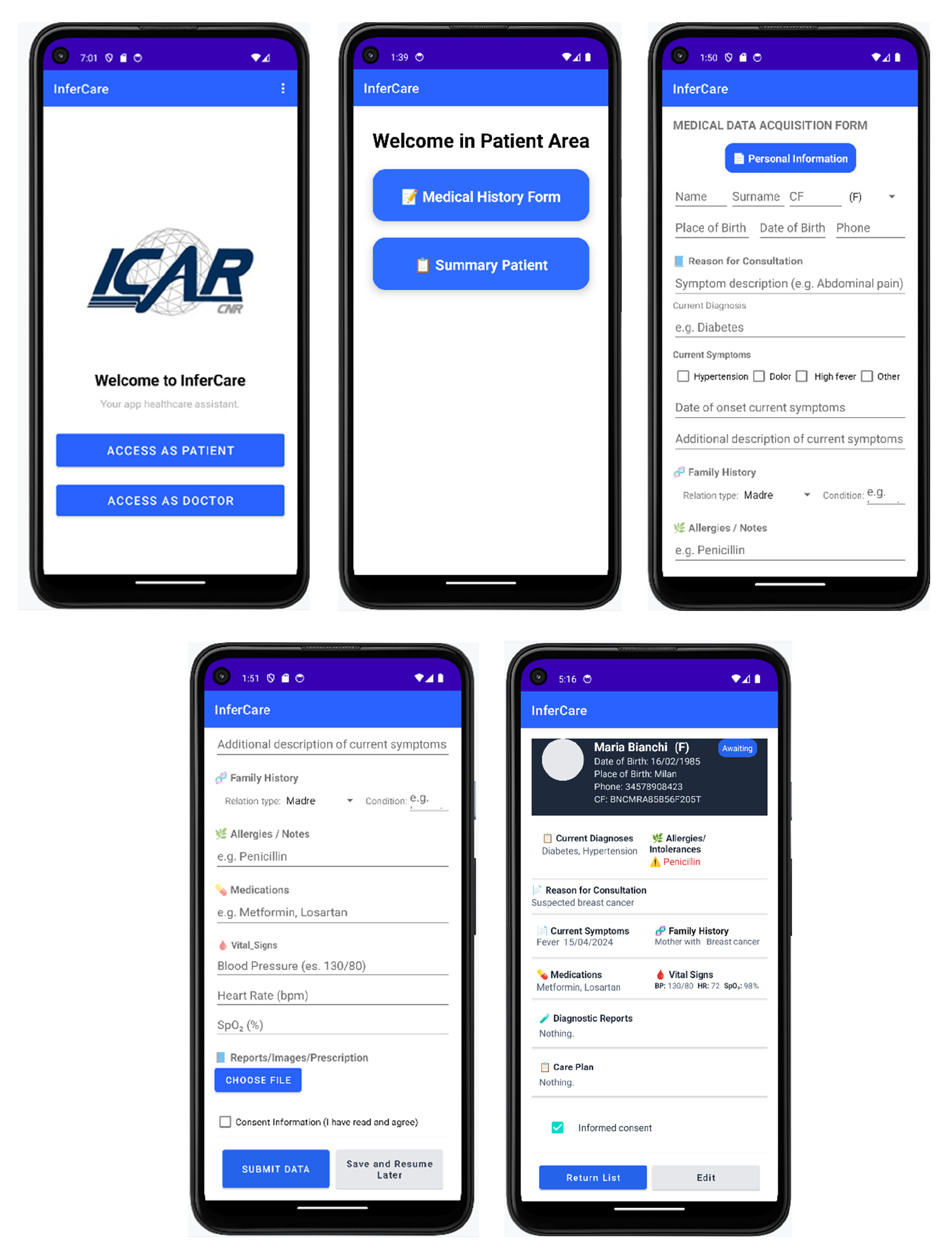
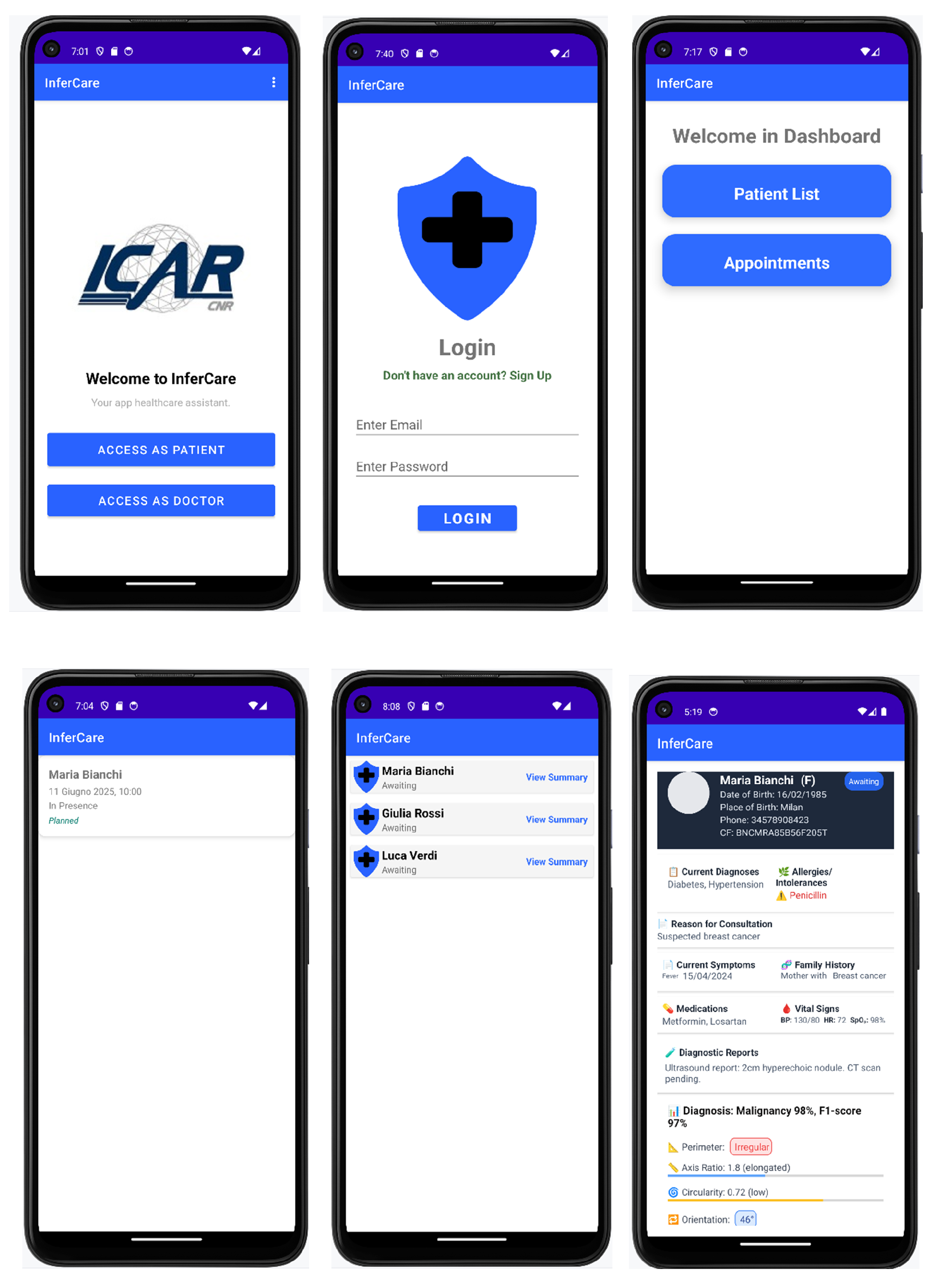
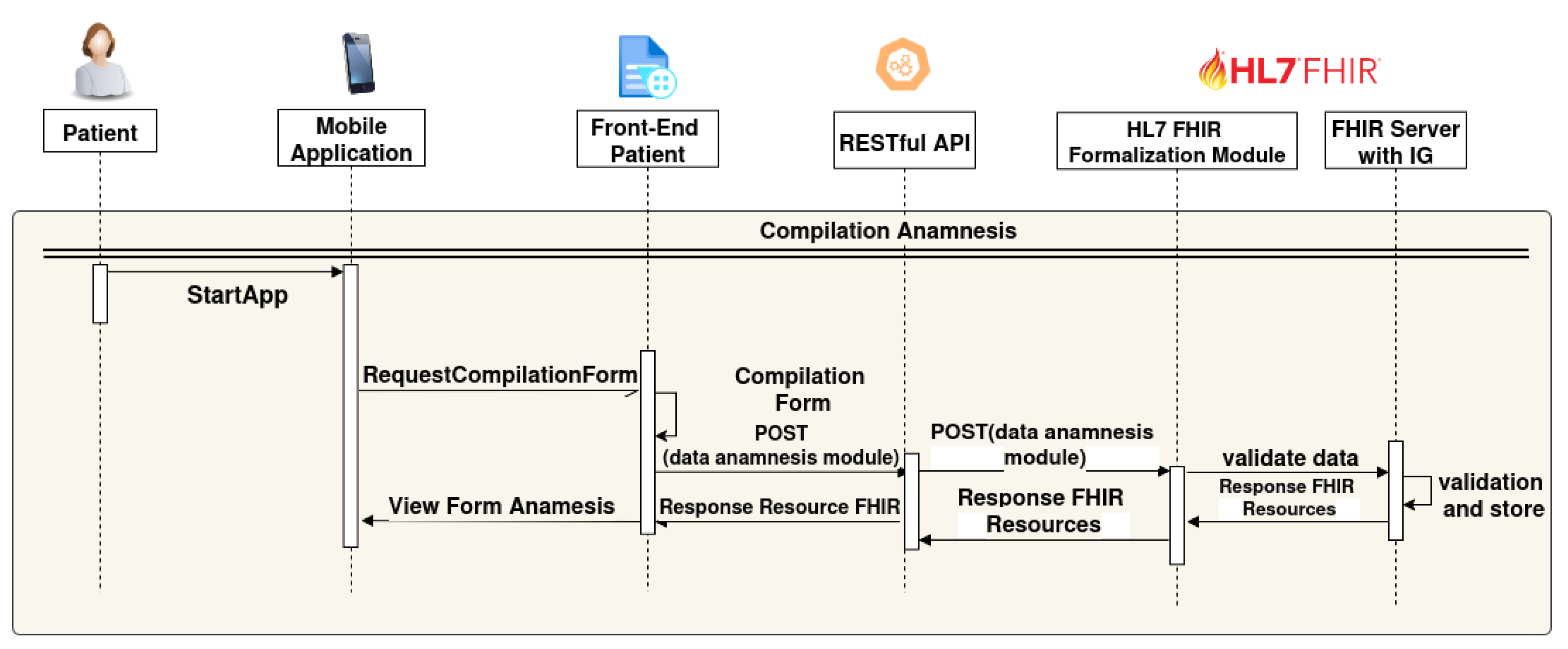
5.3. Sequence Diagrams
- The patient starts the mobile application (StartApp);
- A request is sent to the Front-end Patient to access the data entry form (RequestCompilationForm);
- The patient completes a digital form through the Front-end Patient interface;
- The Front-end Patient form sends the data to the Backend via a REST API (POST(data anamnesis module));
- The "RESTful API" forwards the "POST(data anamnesis module)" to the "HL7 FHIR Formalization Module";
- The HL7 FHIR formalization module transforms the received data into FHIR resources and sends them to the "FHIR Server with IG" for data validation ("validate data") ;
- FHIR Server with IG validates and stores the FHIR Resources , then data sends a "Response FHIR Resources" back to the HL7 FHIR Formalization module.;
- Finally, the "Front-End Patient" receives a "Response Resource FHIR" back to the mobile application as View Form anamnsesis.
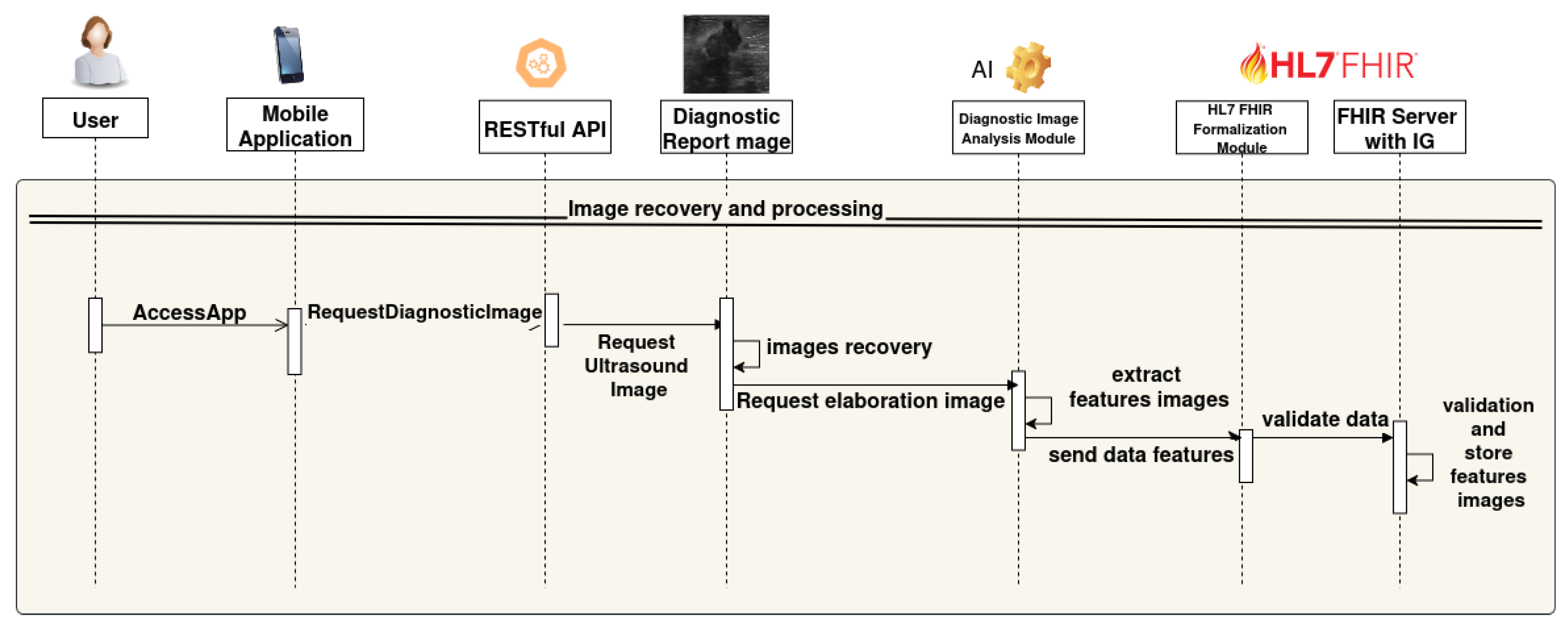
- The user accesses the mobile application (AccessApp).
- The application sends an image analysis request to the backend via RESTful API (RequestElaborationImage).
- The RESTful API performs a POST request to the module that queries the ultrasound image database.
- The database receives the request (RequestDiagnosticImage), retrieves the required ultrasound images (Images recovery), and returns them.
- The ultrasound images are sent to the AI-based image analysis module.
- The AI module extracts the clinical features from the ltrasound images (extract features images).
- The extracted data are sent to the HL7 FHIR formalization module (send data features).
- The HL7 FHIR module validates and transforms the data into FHIR format (validate data).
- Finally, the FHIR Server with IG stores the validated features (validation and store features images resource).
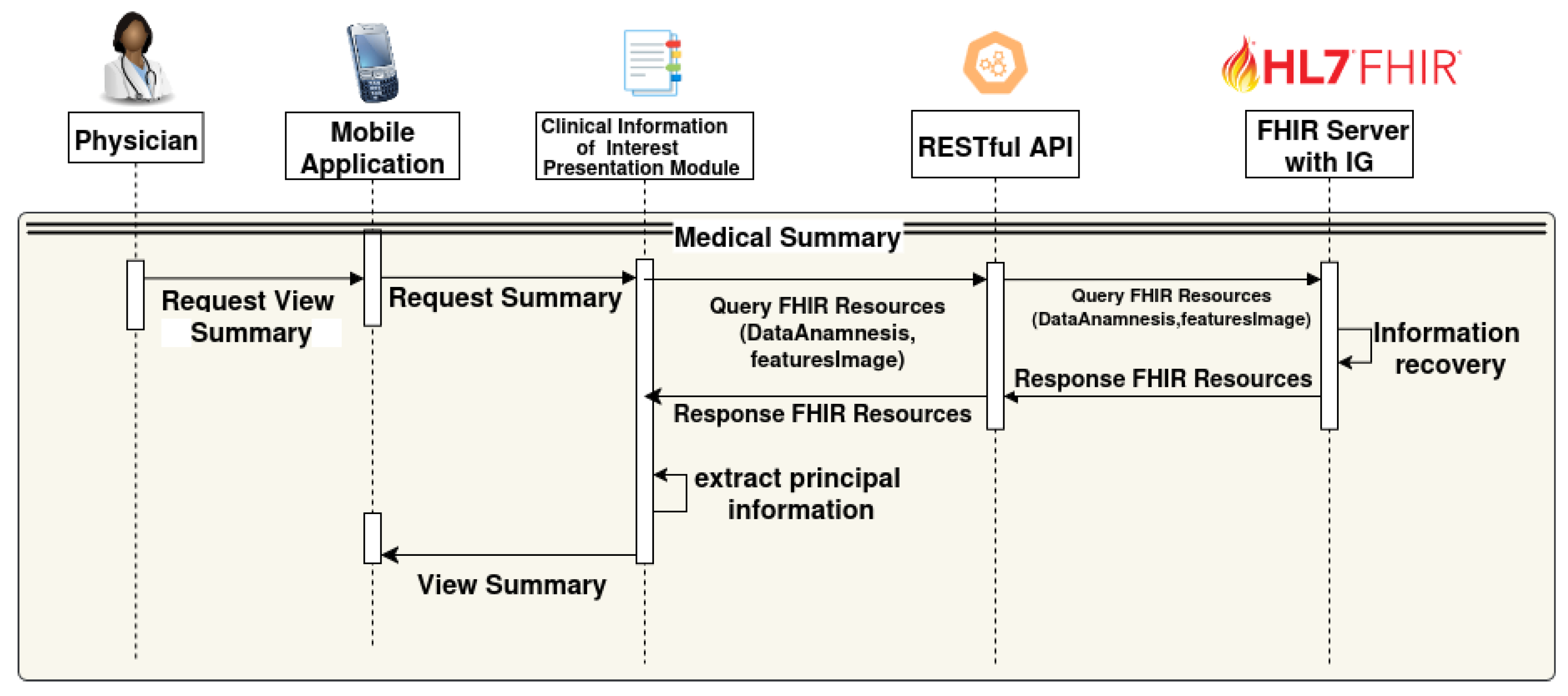
- The physician interacts with the mobile app to request the summary view (RequestViewSummary).
- The app forwards the request to the Clinical Information of Interest presentation module (RequestSummary).
- This module queries the FHIR Server through the RESTful API with a query containing the relevant data (Query FHIR Resources (DataAnamnesis, featuresImage)).
- The FHIR Server with IG retrieves the requested clinical information and returns the FHIR Resources.
- The Clinical Information of Interest presentation module extracts the main data from the received resources, creates a summary with a Health Status Summary and AI-based risk assessment, and highlights the principal information;
- The summary view is presented to the physician through the mobile interface (View Summary).
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| ABUS | Automated Breast Ultrasound System |
| API | Application Programming Interface |
| CAD | Computer-Aided Diagnosis |
| CDSS | Clinical Decision Support System |
| CIIPM | Clinical Information of Interest Presentation Module |
| CIC | Clinical Information Council |
| CIMI | Clinical Information Modeling Initiative |
| DIAM | Diagnostic Image Analysis Module |
| DT | Decision Tree |
| EHR | Electronic Health Record |
| ECG | Electrocardiogram |
| EMR | Electronic Medical Record |
| FHIR | Fast Healthcare Interoperability Resources |
| FR | Functional Requirement |
| HFFM | HL7 FHIR Formalization Module |
| HF | Hand-crafted Features |
| HIS | Health Information System |
| HL7 | Health Level Seven International |
| ICE | Integrated Clinical Environment |
| ICHOM | International Consortium for Health Outcomes Measurement |
| IG | Implementation Guide |
| IHE | Integrating the Healthcare Enterprise |
| IPDSS | Integrated Patient Decision Support System |
| IPS | International Patient Summary |
| JSON | JavaScript Object Notation |
| LR | Logistic Regression |
| mCODE | Minimal Common Oncology Data Elements |
| ML | Machine Learning |
| MLP | Multi-Layer Perceptron |
| MDIRA | Medical Device Interoperability Reference Architecture |
| mHealth | Mobile Health |
| NB | Naive Bayes |
| OSIRIS | Open Standards for Interoperable and Reusable Information in Oncology |
| PF | Pathological Features |
| RF | Random Forest |
| RFE | Recursive Feature Elimination |
| REST | Representational State Transfer |
| SMOTE | Synthetic Minority Oversampling Technique |
| XML | Extensible Markup Language |
| XDS | Cross-Enterprise Document Sharing |
References
- Sreejith, R.; Senthil, S. Smart Contract Authentication assisted GraphMap-Based HL7 FHIR architecture for interoperable e-healthcare system. Heliyon 2023, 9. [Google Scholar] [CrossRef] [PubMed]
- Ramgopal, S.; Sanchez-Pinto, L.N.; Horvat, C.M.; Carroll, M.S.; Luo, Y.; Florin, T.A. Artificial intelligence-based clinical decision support in pediatrics. Pediatric research 2023, 93, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Taber, P.; Radloff, C.; Del Fiol, G.; Staes, C.; Kawamoto, K. New standards for clinical decision support: a survey of the state of implementation. Yearbook of medical informatics 2021, 30, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jang, S.; Park, E. Design of a FHIR interface for wearable healthcare devices. In Proceedings of the 2023 Fourteenth International Conference on Ubiquitous and Future Networks (ICUFN). IEEE; 2023; pp. 730–732. [Google Scholar]
- Zhang, X.; Lin, X.; Tan, Y.; Zhu, Y.; Wang, H.; Feng, R.; Tang, G.; Zhou, X.; Li, A.; Qiao, Y. A multicenter hospital-based diagnosis study of automated breast ultrasound system in detecting breast cancer among Chinese women. Chinese Journal of Cancer Research 2018, 30, 231. [Google Scholar] [CrossRef] [PubMed]
- Duda, S.N.; Kennedy, N.; Conway, D.; Cheng, A.C.; Nguyen, V.; Zayas-Cabán, T.; Harris, P.A. HL7 FHIR-based tools and initiatives to support clinical research: a scoping review. Journal of the American Medical Informatics Association 2022, 29, 1642–1653. [Google Scholar] [CrossRef] [PubMed]
- Seiler, S.J.; Neuschler, E.I.; Butler, R.S.; Lavin, P.T.; Dogan, B.E. Optoacoustic imaging with decision support for differentiation of benign and malignant breast masses: a 15-reader retrospective study. American Journal of Roentgenology 2023, 220, 646–658. [Google Scholar] [CrossRef] [PubMed]
- Mandel, J.C.; Kreda, D.A.; Mandl, K.D.; Kohane, I.S.; Ramoni, R.B. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. Journal of the American Medical Informatics Association 2016, 23, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Eapen, B.R.; Archer, N.; Sartipi, K.; Yuan, Y. Drishti: A Sense-Plan-Act Extension to Open mHealth Framework Using FHIR. In Proceedings of the 2019 IEEE/ACM 1st International Workshop on Software Engineering for Healthcare (SEH); 2019; pp. 49–52. [Google Scholar]
- Sloane, E.B.; Cooper, T.; Silva, R. MDIRA: IEEE, IHE, and FHIR Clinical Device and Information Technology Interoperability Standards, bridging Home to Hospital to “Hospital-in-Home”. In Proceedings of the SoutheastCon 2021, 2021, pp. 1–4.
- Lee, J.; Kim, J. Design of an ECG Stream Analysis Framework Based on FHIR Data Model. In Proceedings of the 2024 Fifteenth International Conference on Ubiquitous and Future Networks (ICUFN); 2024; pp. 567–569. [Google Scholar]
- Raso, E.; Loreti, P.; Ravaziol, M.; Bracciale, L. Anonymization and Pseudonymization of FHIR Resources for Secondary Use of Healthcare Data. IEEE Access 2024, 12, 44929–44939. [Google Scholar] [CrossRef]
- Major, V.J.; Wang, W.; Aphinyanaphongs, Y. Enabling AI-Augmented Clinical Workflows by Accessing Patient Data in Real-Time with FHIR. In Proceedings of the Proceedings of the 2023 IEEE 11th International Conference on Healthcare Informatics (ICHI). IEEE, 2023, pp. 531–533.
- Chishtie, J.; Sapiro, N.; Wiebe, N.; Rabatach, L.; Lorenzetti, D.; Leung, A.A.; Rabi, D.; Quan, H.; Eastwood, C.A. Use of Epic electronic health record system for health care research: scoping review. Journal of medical Internet research 2023, 25, e51003. [Google Scholar] [CrossRef] [PubMed]
- Lamprinakos, G.C.; et al. Using FHIR to develop a healthcare mobile application. In Proceedings of the Proceedings of the 2014 4th International Conference onWireless Mobile Communication and Healthcare (MOBIHEALTH). IEEE, 2014, pp. 132–135..
- Petrakis, Y.; Kouroubali, A.; Katehakis, D. A Mobile App Architecture for Accessing EMRs Using XDS and FHIR. In Proceedings of the 2019 IEEE 19th International Conference on Bioinformatics and Bioengineering (BIBE); 2019; pp. 278–283. [Google Scholar]
- Osterman, T.J.; Terry, M.; Miller, R.S. Improving Cancer Data Interoperability: The Promise of the Minimal Common Oncology Data Elements (mCODE) Initiative. JCO Clinical Cancer Informatics 2020, 4, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; et al. Applying the Minimal Common Oncology Data Elements (mCODE) to the Asia-Pacific Region. JCO Clinical Cancer Informatics 2021, 5, 252–253. [Google Scholar] [CrossRef] [PubMed]
- Guérin, J.; Laizet, Y.; Le Texier, V.; Chanas, L.; Rance, B.; Koeppel, F.; Lion, F.; Gourgou, S.; Martin, A.L.; Tejeda, M.; et al. OSIRIS: A Minimum Data Set for Data Sharing and Interoperability in Oncology. JCO Clinical Cancer Informatics 2021, 5, 256–265. [Google Scholar] [CrossRef]
- Lambarki, M.; Kern, J.; Croft, D.; Engels, C.; Deppenwiese, N.; Kerscher, A.; Kiel, A.; Palm, S.; Lablans, M. Oncology on FHIR: A Data Model for Distributed Cancer Research. Studies in Health Technology and Informatics 2021, 278, 203–210. [Google Scholar]
- HL7 International. International Patient Summary (IPS) Implementation Guide. URL: https://build.fhir.org/ig/HL7/fhir-ips/. Accessed June 25, 2025.
- mCODE Implementation Guide. URL: https://build.fhir.org/ig/HL7/fhir-mCODE-ig/. Accessed June 25, 2025.
- HL7 International and The Breast Cancer Work Group. Breast Cancer Data Implementation Guide. URL: https://hl7.org/fhir/us/breastcancer/2018Sep/index.html. Accessed June 26, 2025.
- HL7 International. Breast Radiology Implementation Guide. URL: https://build.fhir.org/ig/HL7/fhir-breast-radiology-ig/. Accessed June 26, 2025.
- HL7 International and ICHOM. ICHOM Breast Cancer Implementation Guide. URL: https://build.fhir.org/ig/HL7/fhir-ichom-breast-cancer-ig/. Accessed June 30, 2025.
- Conte, T.; Sicuranza, M. Sistema FHIR-Based per la Raccolta Strutturata dell’Anamnesi in Remoto: Approccio, Standard e Implementazione. Rapporto Tecnico RT-ICAR-NA-2025-05, CNR-ICAR, 2025.
- Teresa Conte and Mario Sicuranza. Remote Anamnesis Implementation Guide for Technical Report. URL: https://anamnesi.na.icar.cnr.it/ . Accessed August 08, 2025.
- Teresa Conte and Mario Sicuranza. Remote Anamnesis Implementation Guide. URL: http://remote-anamnesis.na.icar.cnr . Accessed August 08, 2025.
- Guo, R.; Lu, G.; Qin, B.; Fei, B. Ultrasound imaging technologies for breast cancer detection and management: a review. Ultrasound in medicine & biology 2018, 44, 37–70. [Google Scholar]
- Kuhn, M.; Johnson, K.; et al. Applied predictive modeling; Vol. 26, Springer, 2013.
- Magee, J.F. Decision trees for decision making; Harvard Business Review, 1964.
- Rumelhart, D.E.; Hinton, G.E.; Williams, R.J. Learning internal representations by error propagation. Technical report, California Univ San Diego La Jolla Inst for Cognitive Science, 1985.
- Langley, P.; Iba, W.; Thompson, K.; et al. An analysis of Bayesian classifiers. In Proceedings of the Aaai. Citeseer; 1992; Vol. 90, pp. 223–228. [Google Scholar]
- Ho, T.K. Random decision forests. In Proceedings of the Proceedings of 3rd international conference on document analysis and recognition. IEEE, 1995, Vol. 1, pp. 278–282.
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
| 1 | |
| 2 | |
| 3 | |
| 4 | |
| 5 | |
| 6 |
| Feature | Description |
|---|---|
| Major Axis, Minor Axis | Provides intuitive size and shape information |
| Perimeter Regularity | Irregular contours may be indicative of malignancy |
| Orientation | An angle greater than 45° may suggest a malignant nature |
| Circularity | Lower circularity can reflect irregular lesion shapes |
| Feature | Description |
|---|---|
| Eccentricity | Indicates how elliptical the lesion is (0 = perfect circle, 1 = highly elongated ellipse) |
| Circularity | Measures how similar the lesion is to a circle (1 = perfect, <1 = more irregular) |
| Perimeter Regularity | Evaluates the complexity of the lesion boundary |
| Axis Ratio | Relationship between the axes of an ellipse or ellipsoid |
| Solidity | Ratio between the actual area and the convex area (1 = compact, <1 = irregular) |
| Extent | Ratio between the lesion area and its bounding box |
| Elongation | Indicates whether the lesion is stretched along a particular direction |
| Fractal Dimension | Quantifies the complexity of the lesion’s contour |
| Area | Number of pixels comprising the lesion |
| Perimeter | Length of the lesion’s contour |
| Convex Area | Area of the convex hull surrounding the lesion |
| Equivalent Diameter | Diameter of a circle having the same area as the lesion |
| Kurtosis | Measures the "peakedness" of the intensity distribution |
| Skewness | Measures the asymmetry of the intensity distribution |
| Entropy | Indicates the degree of randomness in the pixel intensity distribution |
| Contrast | Measures local intensity variation |
| Homogeneity | Quantifies how similar neighboring pixels are |
| Profile | Description |
|---|---|
| AllergyIntolerance_Patient | Used to represent the patient’s known allergies and intolerances |
| Anamnesis_Patient | Used to represent the personal identity and demographic information of the patient subject to the anamnesis |
| Appointment_Patient | Used to describe information about scheduled clinical appointments |
| CancerRiskAssessment_Patient | Used to represent the patient’s risk of developing cancer based on anamnesis and extracted clinical features |
| CarePlan_Patient | Used to represent a patient care or treatment plan |
| Condition_Patient | Used to represent a particular clinical condition of the patient |
| Consent_Patient | Used to represent the patient’s informed consent regarding the use and sharing of their clinical data |
| DiagnosticReport_Patient | Used to document diagnostic reports associated with the patient, such as ultrasound images |
| FamilyMemberHistory_Patient | Used to document the patient’s family medical history, with special reference to inherited diseases in family members |
| Medication_Patient | Used to describe the characteristics of drugs such as active ingredient, pharmaceutical form, and dosage |
| MedicationStatement_Patient | Used to represent the set of medications taken by the patient |
| Observation_Axis | Used to represent the orientation axis of a clinical image or structure, extracted from ultrasound or imaging data. |
| Observation_PerimeterRegularity | Used to represent the regularity of the perimeter of a lesion or structure observed in diagnostic imaging |
| Observation_Orientation | Used to represent the spatial orientation of a lesion as detected in clinical imaging. |
| Observation_Circularity | Used to represent the circularity of a lesion or structure, derived from diagnostic image analysis |
| Observation_Patient | Used to record observations of the patient’s health status such as vital parameters, symptoms etc. |
| Practitioner_Anamnesis | Used to represent the health professional involved in patient care, e.g., the physician in charge of the examination. |
| Procedure_Patient | Used to represent medical procedures undergone by the patient, such as surgeries, biopsies, or diagnostic interventions |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





