1. Introduction
Myocarditis is an inflammatory disease of the myocardium, the development of which can be caused by a variety of etiological factors and in the implementation of which various mechanisms are involved: from the direct effect of the pathogen on cardiomyocytes, causing their death, to cardiotropic autoimmune reactions. It is not always possible to determine the aetiology of myocarditis (including infectious) and carry out etiotropic treatment. Identifying the leading pathogenetic mechanism is therefore becoming increasingly important.
Myocardial biopsy remains the ‘gold standard’ for diagnosing myocarditis, as it allows to determine the persistence of viruses in the myocardium and the cellular content of inflammatory infiltrates. This information is essential for choosing myocarditis treatment (antiviral, immunosuppressive therapy). However, there is still a need for non-invasive assessment of the severity of the inflammatory process. The possibilities for such assessment in clinical practice are rather limited. Common markers of inflammation [erythrocyte sedimentation rate (ESR), leukocyte levels, fibrinogen, C-reactive protein (CRP), blood ℽ-globulins] have low sensitivity in the diagnosis of subacute and chronic myocarditis [
1]. The highest sensitivity (89%) and positive predictive value (81%) have been established for anticardiac antibodies [
2], which are a marker of autoimmune reactions and a product of B-lymphocyte activity. At the same time, there is no clear correlation between anticardiac antibodies and the severity of chronic heart failure (CHF). T-lymphocytes play a leading role in the development of cellular inflammatory response in myocarditis. B-lymphocytes (CD20-positive cells) are rarely found in infiltrates; their presence indicates an unusually severe course of myocarditis and requires special treatment approaches [
2]. The study of immunoglobulin free light chains (FLC) levels in the blood can provide valuable information on the activity of B cells and their involvement in the pathogenesis of humoral inflammation in myocarditis.
Light chains (polypeptide chains consisting of 211-217 amino acid residues and having a molecular mass of approximately 22 kDa) are part of the tetrameric composition of immunoglobulins together with heavy chains and are released into the blood in small amounts (FLC). This biomarker is also of interest in terms of its possible correlations with better studied markers of inflammation as well as with the severity of CHF [
3]. Studies of FLC in myocarditis are sporadic and inconclusive [
4]. However, there are data on the unfavourable prognostic value of FLC in CHF [
5], which leads us to search for links between myocarditis, systemic inflammation and CHF.
The aim of this study was to investigate the levels of immunoglobulin free light chains in patients with myocarditis compared with non-inflammatory heart disease and their association with the severity of CHF
2. Methods
The study included 99 patients, 41 women and 58 men, mean age 59.6±14.6 years.
The main group consisted of 50 patients with myocarditis (20 women and 30 men, mean age 54.8±13.5 years). The main manifestation of myocarditis was CHF (66% of patients): NYHA class II in 21 patients, NYHA class III in 19 patients and class IV in 3 patients. In the remaining patients, myocarditis manifested in an isolated arrhythmic form. Constant/persistent atrial fibrillation was observed in 15 patients, paroxysmal in 4 patients. In main group, 35 patients had not received any immunosuppressive therapy at the time of enrolment. The remaining 15 patients were receiving maintenance immunosuppressive therapy with methylprednisolone 4-8 mg/day (in 7 cases in combination with azathioprine 75-150 mg/day or mycophenolate mofetil 1-2 g/day) for at least 3 months. The reason for including this subgroup in the study was the persistence of CHF manifestations.
The comparison group consisted of 49 patients with non-inflammatory heart disease (21 women and 28 men, mean age 64.6±14.2 years): 13 patients suffered from coronary artery disease, 10 from acquired heart valve disease, 8 from arterial hypertension, 6 from idiopathic arrhythmias and 11 from cardiomyopathies (3 - hypertrophic, 4 - dilated, 4 - restrictive). Patients with acute coronary syndrome, systemic infectious, immunological and oncological diseases were not included. Heart failure was diagnosed in 65% of patients: NYHA Class II - in 10 patients and NYHA Class III - in 24 patients. Permanent/persistent atrial fibrillation was present in 16 patients and paroxysmal atrial fibrillation in 8 patients.
Laboratory tests included a complete blood count and biochemical panel, C-reactive protein (CRP), fibrinogen, high-sensitivity cardiac troponin test, N-terminal pro-B-type natriuretic peptide (NT-proBNP), anti-cardiac antibodies by indirect enzyme-linked immunosorbent assay and kappa and lambda immunoglobulin FLC (Cloneus S-FLC-K TIA Kit and Cloneus S-FLC-L TIA Kit; reference values: FLC kappa 4.84-14.20 mg/l, FLC lambda 7.03-22.50 mg/l, FLC kappa/lambda ratio 0.426-1.050).
Instrumental examination included electrocardiography, 24-hour Holter ECG monitoring and echocardiography (EchoCG, all patients), endomyocardial biopsy of the right ventricle (n = 20, hematoxylin and eosin and Van Gieson staining, immunohistochemistry for CD7, CD45, CD20, CD68-positive cells), coronary angiography (n=56), cardiac multispiral computed tomography (n=19) and cardiac magnetic resonance imaging (n=37) with intravenous gadolinium enhancement.
The
diagnosis of myocarditis was made on the basis of myocardial biopsy (using the Dallas criteria extended with immunohistochemical criteria) and/or two or more Lake Louise 2018 myocarditis criteria on magnetic resonance imaging [
8] in combination with elevated levels of anticardiac antibodies and other clinical, laboratory and instrumental criteria. Endomyocardial biopsy showed lymphocytic myocarditis in all but one case (neutrophilic); active and borderline in 15 and 5 patients, respectively. The parvovirus B19 genome was detected in the myocardium of 6 patients by polymerase chain reaction and varicella zoster in one patient.
Statistical processing of the material was performed using IBM SPSS v.22.0. Quantitative characteristics were expressed as M±δ (mean ± one standard deviation) or as median with 1st and 3rd quartiles. Normality of distribution was assessed using the Shapiro-Wilk test, and statistical significance of differences was assessed using the Mann-Whitney test. Differences were considered significant if p<0.05. Correlations were analyzed with Spearman's coefficient.
Ethics approval statement. All patients signed an informed consent for the study. The study was supported by the Innovative Scientific School of Sechenov University. The conduct of the study and the informed consent form were approved by the Local Ethics Committee of Sechenov University (Protocol No. 03-24 dated 08.02.2024).
3. Results
The main clinical characteristics of the patients in both groups are shown in
Table 1.
Patients with myocarditis were significantly younger than patients in the comparison group, which is explained by a later development of non-inflammatory heart disease compared to myocarditis. Although the incidence of CHF was the same in both groups, the mechanisms were different. In patients with myocarditis, the main mechanism was systolic dysfunction of the left ventricle with dilatation. In the comparison group, in addition to systolic dysfunction in patients with a history of myocardial infarction, there was CHF with preserved EF (in arterial hypertension, valvular heart disease), so the mean EF in this group was higher. Mean leukocyte, ESR, CRP and fibrinogen levels remained normal in patients in both groups.
The peculiarity of patients with myocarditis on immunosuppressive therapy was the lack of optimal response to treatment, which was the reason for hospitalisation: this explains the pronounced structural and functional disturbances in this subgroup (their comparison with the immune-inflammatory activity during treatment was as well interesting). Cardiotropic therapy varied according to the nature of the underlying disease. It was most commonly used to treat heart failure and/or arrhythmias.
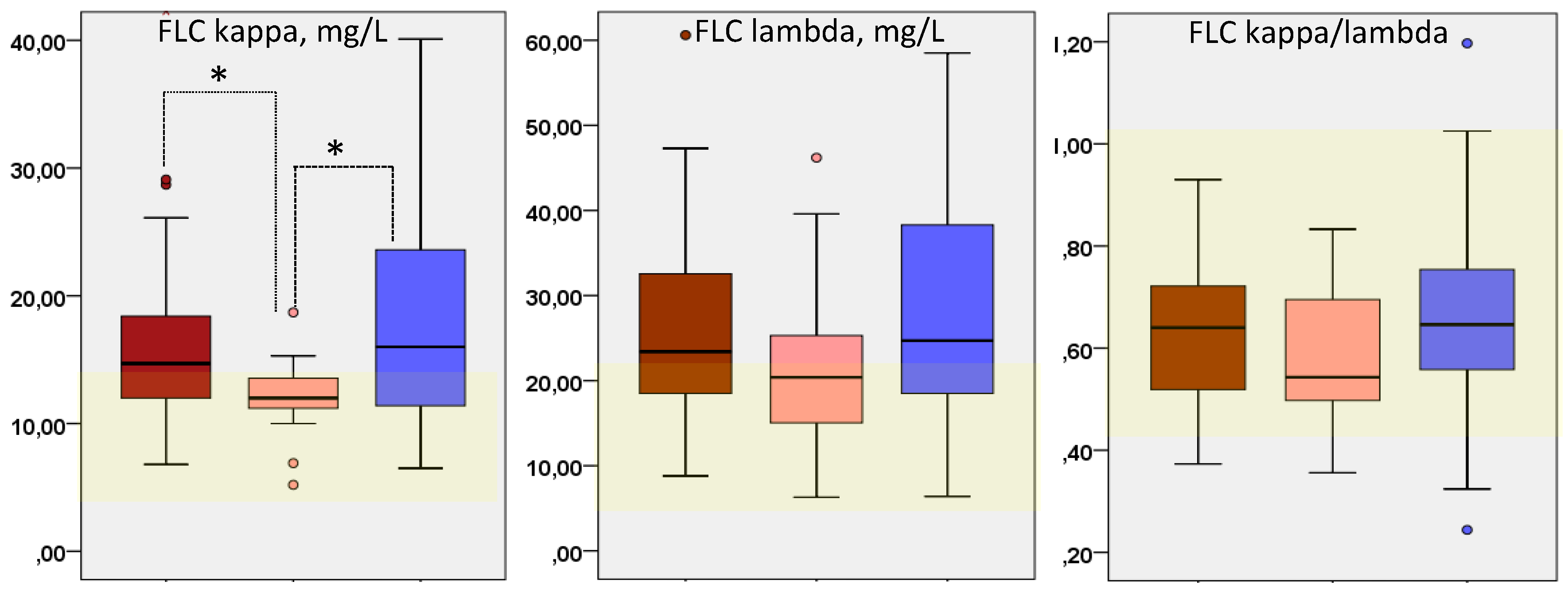
The levels of FLC kappa, lambda and their ratio in patients with myocarditis and in the comparison group are shown in
Figure 1.
In patients with myocarditis who were not receiving immunosuppressive therapy, FLC levels exceeded the normal range in 60% of patients, compared with 67% in the comparison group (differences were not significant). The lowest frequency of FLC elevation was observed in the subgroup of patients with myocarditis who was receiving immunosuppressive treatment (47%). The mean kappa and lambda FLC levels were elevated in both groups, and the kappa FLC level was significantly lower in patients with treated myocarditis than in the comparison group and in patients with untreated myocarditis. The FLC kappa/lambda ratio was within the normal range in both groups, but was lower in treated myocarditis patients (p > 0.05).
Further analysis was aimed at identifying factors associated with increased SLE levels. Correlation analysis showed that FLC levels of both types were closely correlated with general inflammatory markers in the blood (CRP, leukocytes, C-reactive protein, fibrinogen) as well as with CHF class and EF (more so in the myocarditis group),
Table 2. A strong significant correlation with NT-proBNP level was observed only in patients with myocarditis. A strong correlation between FLC and troponin levels was observed in the whole cohort.
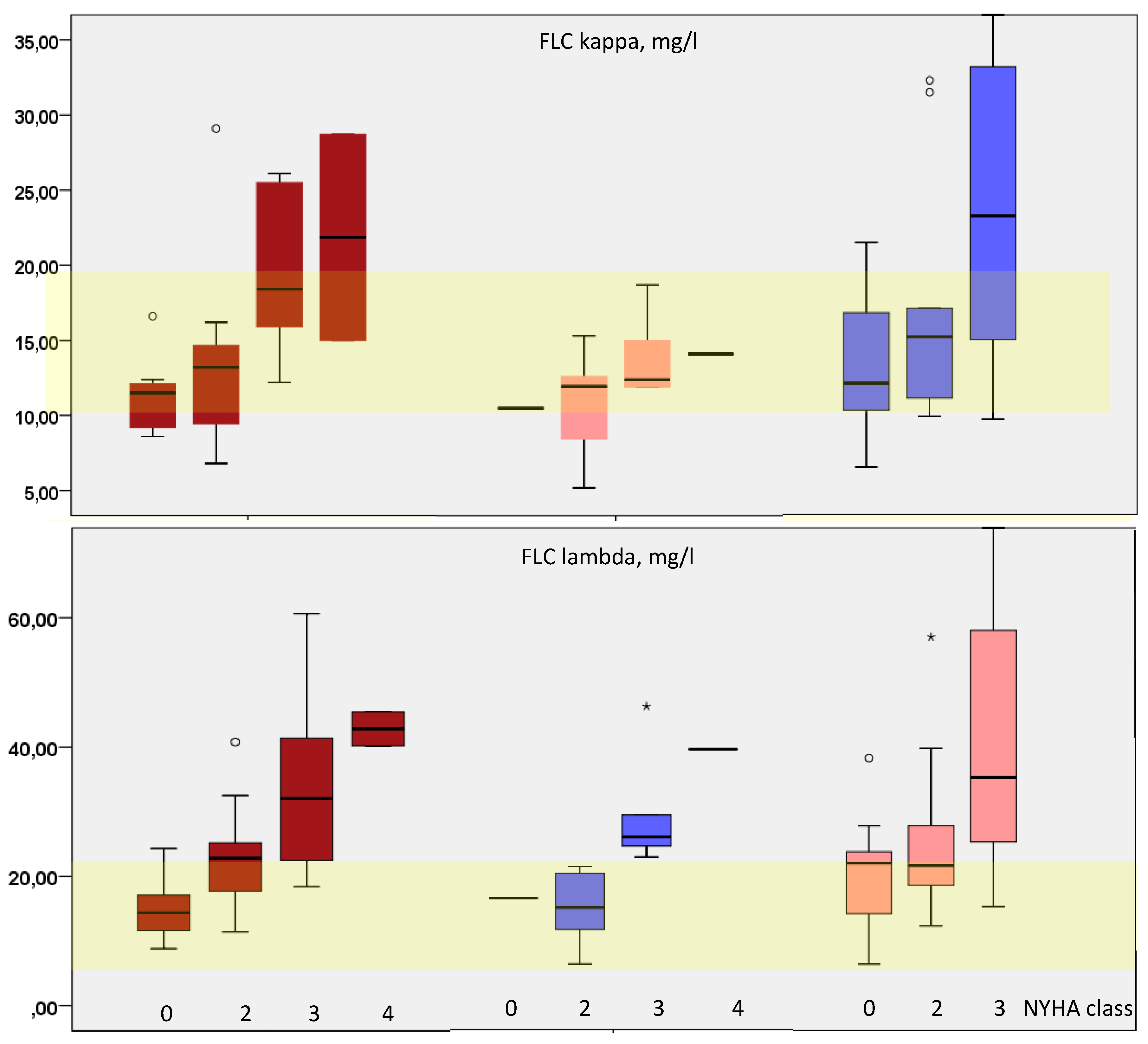
The most common relationship found in both groups was a close correlation between FLC level and CHF class, as depicted in
Figure 2. In the myocarditis group, this correlation was stronger than in the control group (
Table 2). The correlation between FLC level and CHF class was particularly clear in the subgroup of myocarditis patients not receiving immunosuppressive treatment. In myocarditis patients receiving immunosuppressive therapy, the increase in FLC level was only observed in patients with severe CHF decompensation (NYHA class III). In these patients, there was no correlation between FLC levels and the presence of CHF, which was significant only in untreated myocarditis patients (r=0.348 for FLC kappa and 0.413 for FLC lambda, p<0.05) and in the comparison group (
Table 2).
4. Discussion
The hypothesis investigated in the present study was the possible relationship between the level of immunoglobulin FLC in the blood, as a marker of B-lymphocyte activity, with the activity of myocarditis, an inflammatory heart disease. The possible relationship between inflammation and CHF, which is not uncommon in myocarditis, was also of interest.
Blood FLC levels have not been used for diagnostic or prognostic purposes in cardiology (except in cases of suspected amyloidosis). However, FLCs are one of many potential candidates for the role of a biomarker of myocardial damage. One of the first suggestions was a 2015 study [
5] that included 628 patients with decompensated CHF (46% of whom had died by the end of the 3-year follow-up period). Elevated FLC levels (in 42% of subjects) were associated with a 2.38-fold increased risk of adverse outcome and remained significant in multivariate analysis, as did NT-proBNP levels, CRP and NYHA class III-IV. The authors wonder about a possible beneficial effect of CHF therapy on SLE levels (which would allow them to be used for treatment control).
The present study showed no significant differences between the main group (patients with myocarditis) and the comparison group (patients with non-inflammatory heart diseases) in the frequency and degree of FLC elevation. At the same time, there was a significant correlation between FLC levels and the presence and severity of CHF, which was stronger in the myocarditis group. In both the main group and the comparison group, almost 2/3 of the patients had CHF. These data suggest that the increase in FLC levels is primarily associated with the presence of CHF, regardless of its aetiology and mechanisms.
The pathogenetic basis of the relationship between FLC levels and CHF is not entirely clear. In a study of patients with coronary artery disease, FLC levels were also elevated, maximally in acute heart failure and to a lesser extent in CHF [
6], such an effect was observed in patients with normal renal function and correlated with a decrease in systolic function [
7]. When comparing FLC levels in myocarditis with healthy individuals, one would expect a significantly higher FLC level in patients with myocarditis, but it would be difficult to judge whether the cause of the increased FLC level is due to the myocarditis proper or to CHF. This dilemma is illustrated by the only clinical study that found a significantly lower kappa and lambda FLC ratio in patients with morphologically verified myocarditis and CHF (EF less than 45%) compared to healthy controls [
4]. The level of kappa type FLC was significantly lower and lambda type FLC significantly higher than in the group of healthy volunteers, which contradicts the previous experimental data of these authors [
8] and the data of C.E. Jackson et al. [
5]. The authors suggest the role of a specific activation of the B-lymphocyte clone synthesising lambda-type FLCs and consider the decrease in the ratio of kappa and lambda FLCs as a marker of "myocarditis with CHF".
Our work did not confirm monoclonal activation of FLC in patients with myocarditis and in the comparison group and is more consistent with the results of C.E. Jackson [
5]. Interestingly, even in patients with AL amyloidosis, monoclonal FLC secretion had no diagnostic significance in detecting typical amyloid cardiac lesions, in contrast to BNP levels [
9]. A direct toxic effect of AL chains on cardiomyocytes has been demonstrated, which is independent of the degree of amyloid infiltration of the myocardium and is undoubtedly an unfavourable prognostic factor [
10]. By analogy with AL amyloidosis, direct damage to cytoskeletal and mitochondrial proteins under the action of FLC can be envisaged [
11].
In patients without amyloidosis, correlations of FLC levels with troponin and NT-proBNP were not studied. We obtained a strong significant correlation between FLC and NT-proBNP, which was not observed in the comparison group: this allows us to consider FLC as a possible marker of a decompensated course of myocarditis. In addition, a strong correlation between FLC and troponin levels was found in the whole cohort of patients, which may reflect a direct role of cardiomyocyte death in the induction of the immune response (including the secondary inflammatory response). It is suggested that the involvement of FLC goes beyond general inflammatory responses and involves some specific mechanisms. Correlations with interleukin-6 levels and other markers of B lymphocyte activity should be investigated.
Among the more understandable mechanisms, our study confirmed the inverse relationship between FLC level and glomerular filtration rate, explained by a decrease in renal clearance of FLC. At the same time, the prognostic value of FLC was found to remain independent of creatinine levels [
5]. Long-term persistence of FLC after acute decompensation is considered an indicator of immune dysregulation [
6]. It has been shown that levosimendan administration significantly reduces FLC in CHF patients [
12], which, given its mechanism of action (positive inotropic), probably reflects the influence of CHF severity on FLC rather than the reverse. In addition, patients treated with levosimendan are initially in a state of hypoperfusion and its administration improves renal function by increasing renal perfusion, which may also contribute to the rise in FLC clearance.
Finally, we found a significantly lower level of FLC in patients with myocarditis who received immunosuppressive therapy compared with untreated patients and patients in the comparison group (with no differences in CHF class). The study also included those patients with myocarditis in whom the treatment did not lead to a significant reduction in heart failure, which allowed us to think about a lack of effectiveness of the immunosuppressive therapy. However, the significantly lower level of FLC kappa and the lack of correlation of FLC level with the presence of CHF in this subgroup may indicate an effective suppression of immune inflammation and the involvement of other (non-inflammatory) mechanisms in the maintenance of CHF. These data indicate the sensitivity of FLC to the effect of immunosuppressants and allow us to consider the level of FLC as one of the criteria of the effectiveness of myocarditis treatment.
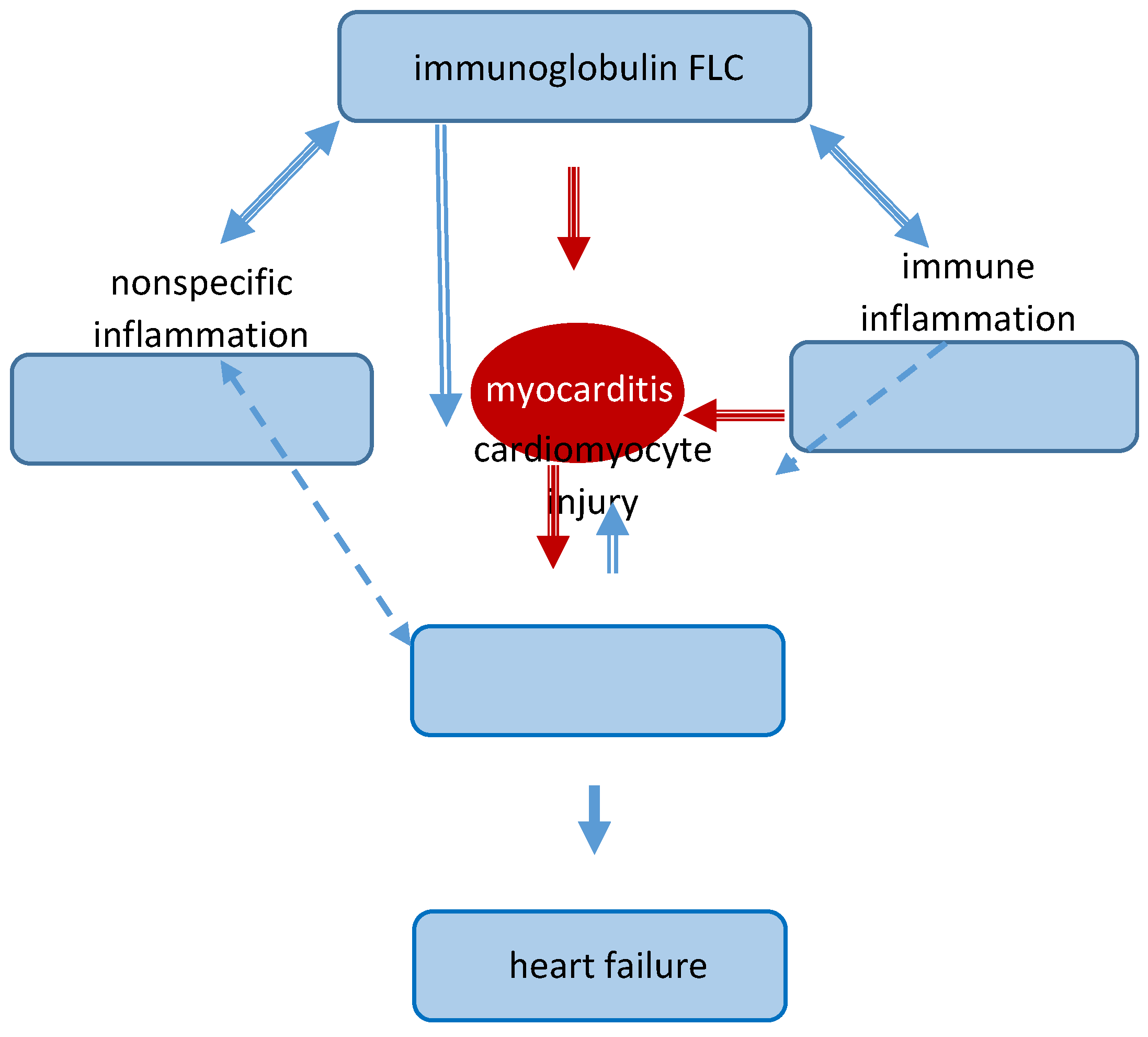
The role of FLCs in the pathogenesis of myocarditis and CHF can be illustrated schematically as follows (
Figure 3). Myocarditis appears to be a disease in which both immune (autoimmune) mechanisms and possibly a direct pathogenic effect of FLCs are realised. It can be assumed that FLCs in myocarditis are the transmitter involved in the prognostically unfavourable, decompensated variant of myocarditis and that this biomarker can be used both as a prognostic criterion and therapeutic target. It is important to note that the mean levels of general inflammatory markers remained normal in the myocarditis group, in contrast to FLC. This means that the latter can be considered as a kind of indicator (amplifier) of latent inflammation in patients with myocarditis, which makes it promising to use them also for diagnostic purposes. One of the studies showed an association between an increase in FLC and the development of atrial fibrillation - the authors conclude that this arrhythmia may have an inflammatory genesis even in the absence of CHF [
13].
There have also been single experimental attempts to use FLC in the treatment of myocarditis. The group of A. Matsumori et al. in 2010 investigated the level of FLC in experimental viral myocarditis based on the relationship between mast cell activity and FLC production [
8]. Not only did kappa FLC levels spontaneously increase in mice with myocarditis, but therapeutic administration of kappa FLC suppressed the myocarditis and administration of an FLC antagonist exacerbated the disease. The issue of predicting the results of antiviral and immunosuppressive therapy of myocarditis is poorly studied, but one of the most critical for myocarditis patients.
5. Study Limitations
The main limitation of the study is the relatively small number of patients enrolled. However, even with this number of patients, a series of patterns were established that allow us to define the directions of further studies: investigation of FLC levels in patients with myocarditis without significant CHF, influence of FLC levels on the prognosis in patients with myocarditis and CHF, and the possibility of using them to predict and evaluate the response to therapy (both myocarditis and CHF). Another limitation was the lack of morphological evidence of myocarditis in 100% of patients, which did not allow us to compare FLC levels with morphological features of myocarditis.
6. Conclusions
The level of immunoglobulin FLC of kappa and lambda types is elevated in 56% of patients with myocarditis and in 67% of patients with non-inflammatory nature of CHF. In myocarditis patients receiving maintenance immunosuppressive therapy, the level of kappa-type FLC was significantly lower than in untreated patients and in the comparison group. A direct positive correlation was found between the levels of both types of FLC and the severity of CHF (NYHA functional class), both in the presence and absence of left ventricular systolic dysfunction. Correlations were also found between FLC levels and general inflammatory markers (CRP, leukocytes, SOE) and troponin levels. Only in patients with myocarditis was there a strong correlation between FLC levels and NT-proBNP. Elevated FLC levels may reflect specific mechanisms of myocarditis as well as the severity of CHF and may be evaluated as a predictor of a decompensated variant of myocarditis and an insufficient response to immunosuppressive therapy. In the absence of a significant increase in the level of general inflammatory markers in the blood of patients with myocarditis, the determination of FLC can be used as an additional diagnostic marker. Its diagnostic and prognostic value in patients without CHF requires further study.
Funding
the work was supported by the Innovative Scientific School of Sechenov University.
Data Availability Statement
All data generated or analysed during this study are included in this article.
Conflicts of Interest
none for all authors.
List of Abbreviations
FLC, free light chains; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; EF, ejection fraction; CHF, chronic heart failure; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
References
- Blagova OV, Osipova YV, Nedostup AV et al. [Clinical, laboratory and instrumental criteria for myocarditis, established in comparison with myocardial biopsy: A non-invasive diagnostic algorithm]. Ter Arkh. 2017; 89(9):30-40. Russian. [CrossRef]
- Tschöpe C, Van Linthout S, Spillmann F et al. Targeting CD20+ B-lymphocytes in inflammatory dilated cardiomyopathy with rituximab improves clinical course: a case series. Eur Heart J Case Rep. 2019; 3(3):ytz131. [CrossRef]
- Rao A, Gupta A, Kain V, Halade GV. Extrinsic and intrinsic modulators of inflammation-resolution signaling in heart failure. Am J Physiol Heart Circ Physiol. 2023; 325(3): H433-H448. [CrossRef]
- Matsumori A, Shimada T, Nakatani E et al. Immunoglobulin free light chains as an inflammatory biomarker of heart failure with myocarditis. Clin Immunol. 2020; 217:108455. [CrossRef]
- Jackson CE, Haig C, Welsh P et al. Combined Free Light Chains Are Novel Predictors of Prognosis in Heart Failure. JACC Heart Fail. 2015; 3(8):618-25. [CrossRef]
- Shantsila E, Wrigley B, Lip GY. Free light chains in patients with acute heart failure secondary to atherosclerotic coronary artery disease. Am J Cardiol. 2014; 114(8):1243-8. [CrossRef]
- Perrone MA, Pieri M, Marchei M et al. Serum free light chains in patients with ST elevation myocardial infarction (STEMI): A possible correlation with left ventricle dysfunction. Int J Cardiol; 292:32-34. [CrossRef]
- Matsumori A, Shimada M, Jie Xet al. Effects of free immunoglobulin light chains on viral myocarditis. Circ Res. 2010; 106(9):1533-40. Wees I, Hendren NS, Kaur G at al. Natriuretic Peptides and Cardiac Troponins: Markers of Disease Progression and Risk in Light Chain Cardiac Amyloidosis. Curr Heart Fail Rep. 2023; 20(5):350-357. [CrossRef]
- Kimishima Y, Yoshihisa A, Kiko T et al. Utility of B-Type Natriuretic Peptide for Detecting Cardiac Involvement in Immunoglobulin Amyloidosis. Int Heart J. 2019; 60(5):1106-1112. [CrossRef]
- Lysenko (Kozlovskaya) L.V., Rameev V.V., Moiseev S.V. et al. Clinical guidelines for diagnosis and treatment of systemic amyloidosis. Clin Pharmacol Therapy 2020;29(1):13-24. [in Russian]. [CrossRef]
- Imperlini E, Gnecchi M, Rognoni P et al. Proteotoxicity in cardiac amyloidosis: amyloidogenic light chains affect the levels of intracellular proteins in human heart cells. Sci Rep. 2017; 7(1):15661. PMID: 29142197; PMCID: PMC5688098. [CrossRef]
- Kurt IH, Yavuzer K, Batur MK. Short-term effect of levosimendan on free light chain kappa and lambda levels in patients with decompensated chronic heart failure. Heart Vessels. 2010 Sep;25(5):392-9. [CrossRef]
- Matsumori A, Shimada T, Shimada M et al. Immunoglobulin Free Light Chains as Inflammatory Biomarkers of Atrial Fibrillation. Circ Arrhythm Electrophysiol. 2020; 13(11):e009017. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).