Submitted:
30 July 2025
Posted:
07 August 2025
You are already at the latest version
Abstract
Keywords:
INTRODUCTION
The Military Health System of the United States Department of Defense
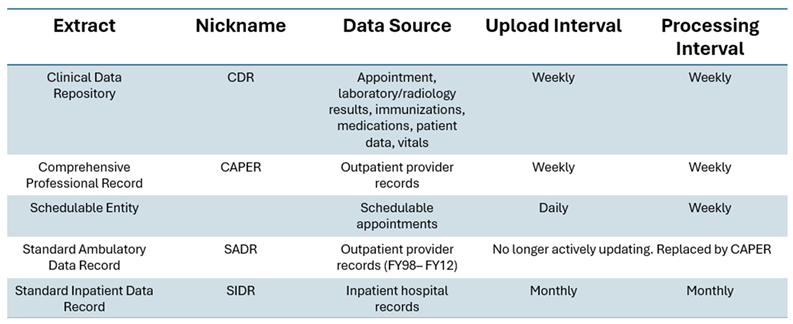
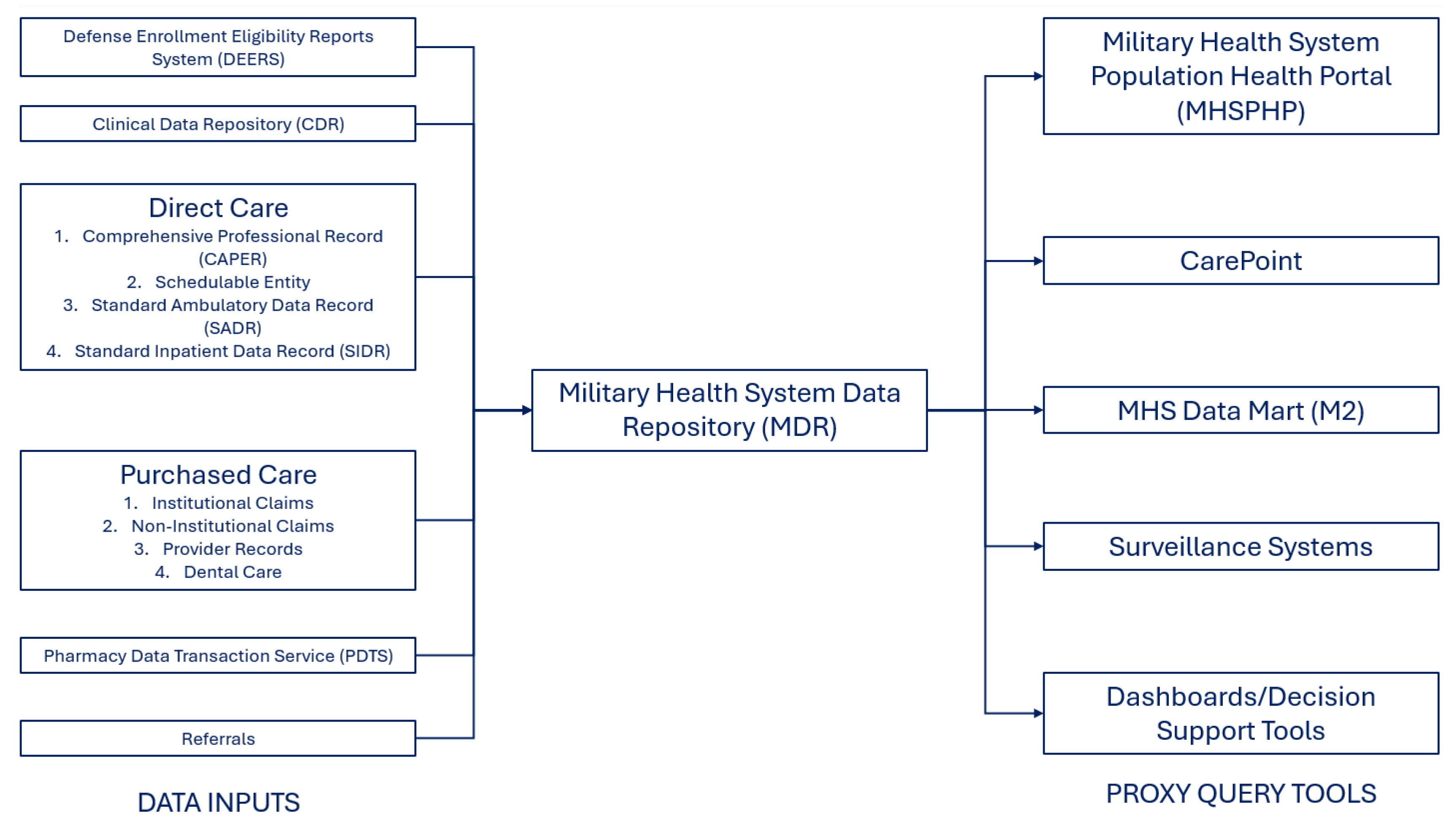
DESCRIPTION OF THE DATA SOURCE
Defense Enrollment Eligibility Reports System (DEERS)
Clinical Data Repository (CDR)
Private Sector Care
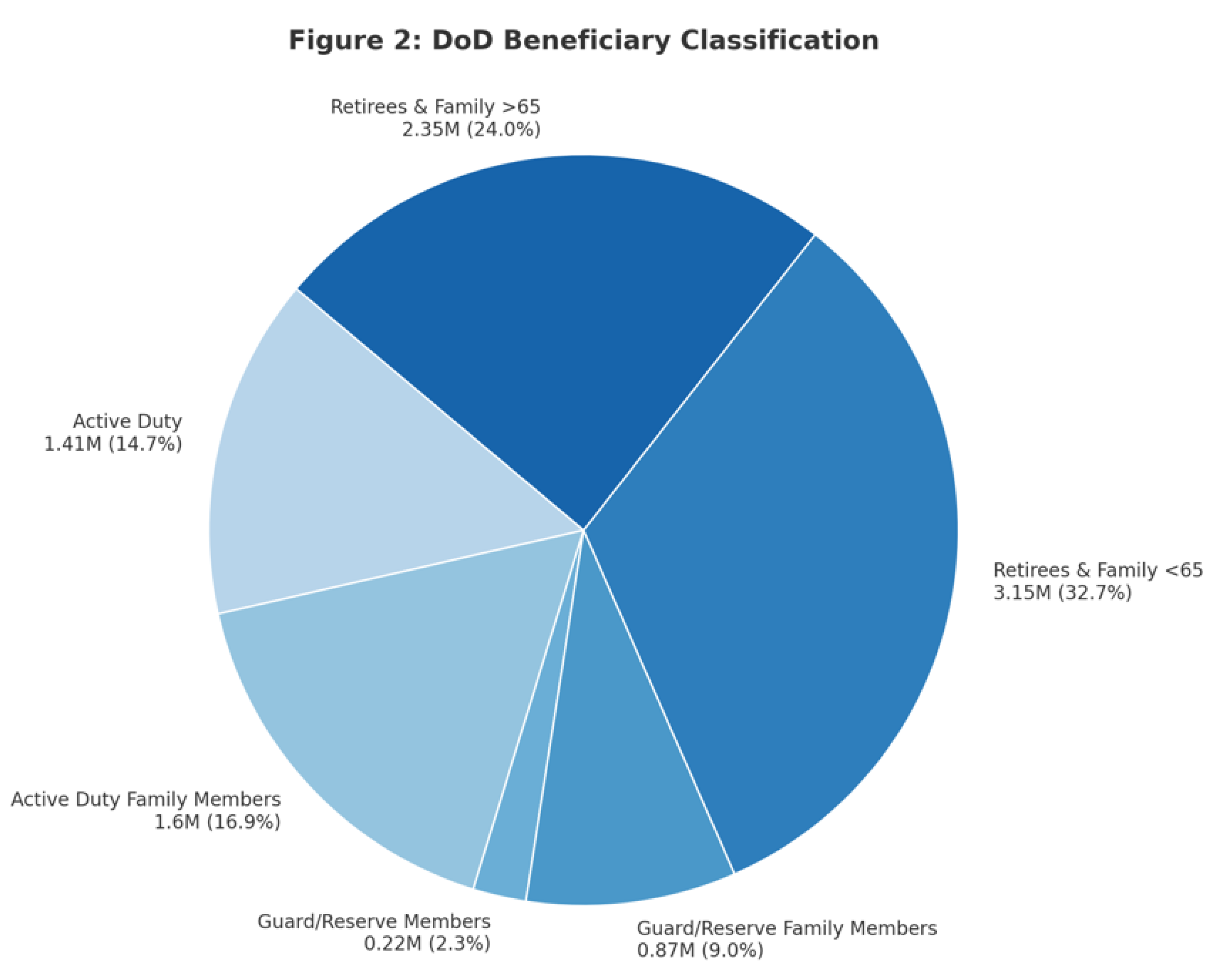
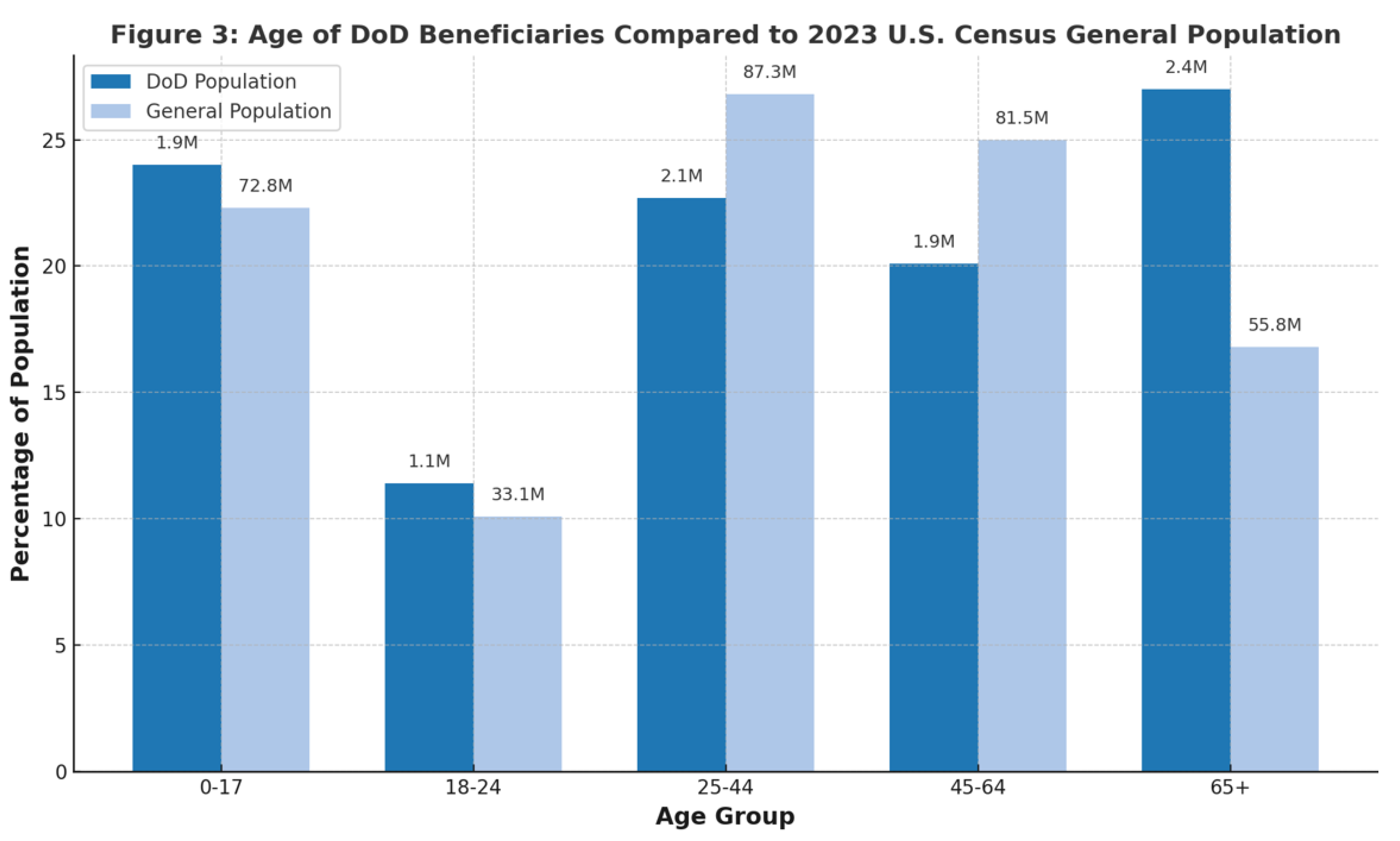
PATIENT POPULATION AND GENERALIZABILITY
Patient Population
Mother-Child Linkage
Strengths and Limitations
- Figure Legends
- Figure 1.
References
- Dreyer NA. Advancing a framework for regulatory use of real-world evidence: When real is reliable. Ther Innov Regul Sci. 2018;52(3): 362-368. [CrossRef]
- Reynolds MW, Bourke A, Dreyer NA. Considerations when evaluating real-world data quality in the context of fitness for purpose. Pharmacoepidemiol Drug Saf. 2020 Oct;29(10): 1316-1318.
- Hall GC, Sauer B, Bourke A, Brown JS, Reynolds MW, LoCasale R. Guidelines for good database selection and use in pharmacoepidemiology research. Pharmacoepidemiol Drug Saf. 2012 Jan;21(1): 1-10. [CrossRef]
- Tanielian T, Farmer C. The US Military Health System: Promoting readiness and providing health care. Health Affairs 2019 Aug;38(8). [CrossRef]
- Military Health System. Department of Defense serum repository. URL: https://www.health.mil/Military-Health-Topics/Health-Readiness/AFHSD/Functional-Information-Technology-Support/Department-of-Defense-Serum-Repository.
- Hofmann LJ, Lee S, Waddell B, Davis KG. Effect of race on colon cancer treatment and outcomes in the Department of Defense healthcare system. Diseases of the Colon & Rectum 2010 Jan;53(1): 9-15. [CrossRef]
- Rizzo JA, Sherman WE, Arciero CA. Racial disparity in survival from early breast cancer in the department of defense healthcare system. J. Surg. Oncol. 2015 Feb;111: 819-823. [CrossRef]
- Alexander M, Zhu K, Cullen J et al. Race and overall survival in men diagnosed with prostate cancer in the Department of Defense Military Health System, 1990–2010. Cancer Causes Control 2019 Apr;30: 627–635. [CrossRef]
- Gutman JR, Hall C, Khodr ZG, Bukowinski AT, Gumbs GR, Conlin AMS, Wells NY, Tan KR. Atovaquone-proguanil exposure in pregnancy and risk for adverse fetal and infant outcomes: A retrospective analysis. Travel Medicine and Infectious Disease 2019 Nov;32. [CrossRef]
- Perdue CL, Cost AAE, Rubertone MV, Lindler LE, Ludwig SL. Description and utilization of the United States Department of Defense Serum Repository: A review of published studies, 1985-2012. PLoS ONE 2015 Feb;10(2). [CrossRef]
- Woeller CF, Thatcher TH, Van Twisk D, Pollock SJ, Croasdell A, Kim N, Hopke PK, Xia X, Thakar J, Col. Mallon TM, Utell MJ, Phipps RP. Detection of serum microRNAs from Department of Defense Serum Repository: Correlation with cotinine, cytokine, and polycyclic aromatic hydrocarbon levels. Journal of Occupational and Environmental Medicine 2016 Aug;58(8): S62-S71. [CrossRef]
- Ellis GC, Lanteri CA, Hsieh HC, Graf PCF, Pineda G, Crum-Cianflone NF, Berjohn CM, Sanders T, Maves RC, Deiss R. Coccidioidomycosis seroincidence and risk among military personnel, Naval Air Station Lemoore, San Joaquin Valley, California, USA. Emerg Infect Dis. 2022 Sep;28(9):1842-1846. [CrossRef]
- Costenbader KH, DiIorio M, Chu SH, Cui J, Sparks JA, Lu B, Moss L, Kelmenson L, Feser M, Edison J, Clish C, Lasky-Su J, Deane KD, Karlson EW. Circulating blood metabolite trajectories and risk of rheumatoid arthritis among military personnel in the Department of Defense Biorepository. Annals of the Rheumatic Diseases 2021 Aug;80(8): 989-996. [CrossRef]
- Military Health System. Medical Surveillance Monthly Report. URL: https://www.health.mil/Military-Health-Topics/Health-Readiness/AFHSD/Reports-and-Publications/Medical-Surveillance-Monthly-Report.
- Military Health System. Interface Control Documents (ICDs) functional references and specifications. URL: https://www.health.mil/Military-Health-Topics/Technology/Support-Areas/MDR-M2-ICD-Functional-References-and-Specification-Documents/Interface-Control-Documents-Functional-References-and-Specifications.
- Mukherjee S. Cerner, Leidos, & Accenture win massive $4.3B Defense Department EHR contract. Healthcare Dive. URL: https://www.healthcaredive.com/news/cerner-leidos-accenture-win-massive-43b-defense-department-ehr-contra/403130/.
- Bukowinski AT et al. Department of Defense Birth and Infant Health Registry: Select reproductive health outcomes, 2003–2014. MSMR November 2017;24(11): 39-50.
- Eaglehouse YL, Shriver CD, Lin J, Bytnar JA, Darmon S, McGlynn KA, Zhu K. MilCanEpi: Increased capability for cancer care research in the Department of Defense. JCO Clin Cancer Inform. 2023 Aug;7. [CrossRef]
- Military Health System. Patient Care Numbers for the Military Health System. URL: https://www.health.mil/News/Media-Resources/Media-Center/Patient-Care-Numbers-for-the-MHS.
- Military Health System. MHS Health Facilities. URL: https://www.health.mil/News/Media-Resources/Media-Center/MHS-Health-Facilities.
- Military Health System. Patient Care Numbers for the Military Health System. URL: https://www.health.mil/News/Media-Resources/Media-Center/Patient-Care-Numbers-for-the-MHS.
- Department of Defense. 2023 Demographics: Profile of the Military Community. URL: https://download.militaryonesource.mil/12038/MOS/Reports/2023-demographics-report.
- Pew Research Center. Chapter 6: A Profile of the Modern Military. URL: https://www.pewresearch.org/social-trends/2011/10/05/chapter-6-a-profile-of-the-modern-military/.
- Cooper JD, Shou K, Sunderland K, Pham K, Thornton JA, DeStefano CB. Real-World Pitfalls of Analyzing Real-World Data: A Cautionary Note and Path Forward. JCO Clin Cancer Inform. 2023 Sep;7:e2300097. [CrossRef]
- Rhon DI, Clewley D, Young JL, Sissel CD, Cook CE. Leveraging healthcare utilization to explore outcomes from musculoskeletal disorders: methodology for defining relevant variables from a health services data repository. BMC Med Inform Decis Mak. 2018 Jan 31;18(1):10. [CrossRef]
- Sicignano NM, Revel FB, Petruschke R, Barbone FP, Nickolson K, Edison, JD. Evaluating the Real-World Use of Topical Diclofenac Sodium Gel 1% Using US Longitudinal Electronic Health Records Database: A study supporting OTC switch. Pain Ther (2025). [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




