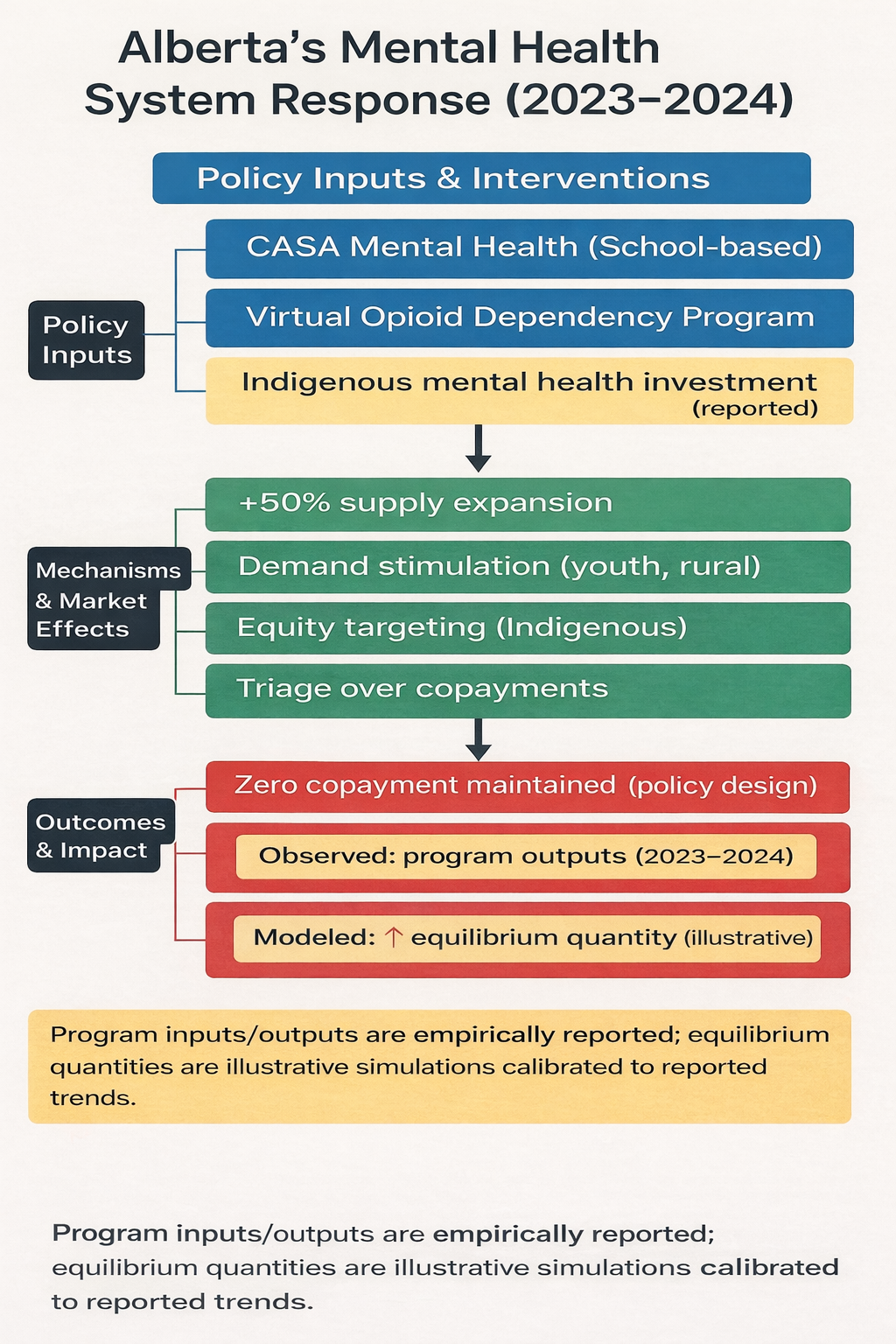
1. Plain Language Summary
During the COVID-19 pandemic, more people in Alberta needed mental health and addiction support. Alberta responded by expanding publicly funded services, including youth programs (CASA Mental Health classrooms), same-day virtual opioid treatment (VODP), tele-mental health, and recovery communities.
Using Alberta’s 2023–2024 public reporting, we summarize what programs were planned to deliver and what they actually delivered. We also use a simple, illustrative supply–demand simulation (not direct price measurement) to show how increasing service capacity at the same time as help-seeking rises can increase the number of services delivered while keeping user costs at zero.
Overall, Alberta’s approach shows how coordinated public investment and service redesign can support access during a system shock. To sustain progress, Alberta will likely need continued workforce investment, strong digital access in rural areas, and equity-focused service design for youth and Indigenous communities.
2. Introduction
The COVID-19 pandemic coincided with increased mental health needs, including anxiety, depression, and substance use across age groups, with children and youth disproportionately affected [
1]. In Canada’s publicly funded health system, access to mental health services remains uneven across provinces due to structural inequities, governance differences, and workforce constraints [
2].
Despite extensive documentation of COVID-era mental health needs and policy responses, relatively few studies quantify how publicly funded mental health systems adjust to concurrent demand shocks and supply expansions using an explicit economic framing. Using Alberta’s 2023–2024 administrative reporting, we apply a system-level supply–demand model to translate policy actions into interpretable implications for access and utilization.
Alberta is a useful case because of its decentralized delivery structure and rapid implementation of publicly funded interventions between 2020 and 2024. Key initiatives included the Virtual Opioid Dependency Program (VODP), expanded CASA Mental Health classrooms for high-needs youth, and the creation of recovery communities with additional publicly funded residential capacity [
3]. These investments were paired with efforts to expand digital access and improve mental health literacy, which may have influenced both service demand (help-seeking) and system capacity (service availability).
This study examines Alberta’s system-level response through a health economics and policy lens using two complementary components: (1) empirically reported program delivery outputs from the 2023–2024 Alberta Mental Health and Addiction Annual Report and (2) an illustrative supply–demand simulation calibrated to reported trends to assess directional shifts in demand, capacity, and the modeled equilibrium quantity under a zero-copayment design. The aim is to clarify how coordinated public interventions may support service delivery during system shocks and to identify policy-relevant considerations for equity and sustainability, without estimating cost-effectiveness outcomes.
3. Literature Review and Theoretical Framework
3.1. Supply and Demand in Mental Healthcare Markets
Mental healthcare operates in a constrained submarket with persistent market failures: supply is limited by workforce shortages and geographic maldistribution, while demand is shaped by stigma, diagnostic uncertainty, and gatekeeping. In publicly financed systems, standard “market equilibrium” concepts require adaptation because third-party payment, non-transparent pricing, and information problems weaken the link between patient prices and utilization [
4]. In this paper, we use “equilibrium” in a limited sense to describe the relationship between system capacity (service availability) and help-seeking/service uptake under a zero-copayment design.
During the COVID-19 period, Alberta experienced increased help-seeking and service uptake—particularly among youth and rural populations—alongside capacity expansion through digital modalities and targeted investments [
2,
3]. International calls following COVID-19 similarly emphasize strengthening digital access, expanding community-based care, and rebalancing hospital-centric models to improve continuity and equity [
5]. Alberta’s intervention mix provides a valuable case for examining how policy instruments may influence both capacity and uptake within a decentralized provincial system.
3.2. Economic Frictions Relevant to Mental Health Policy
Moral hazard. When out-of-pocket costs are low, utilization can increase, including for lower-acuity needs, potentially straining capacity if not managed [
4]. In Alberta, publicly funded services (including VODP and youth-focused programs such as CASA) minimize user costs. They may increase use, making triage, referral pathways, and eligibility criteria important for balancing access and capacity [
3]. Evidence from the RAND Health Insurance Experiment demonstrates that cost-sharing affects utilization across service types, including mental health, underscoring the behavioral implications of insurance design [
6].
Adverse selection. Mental health systems can face selection pressures when higher-need individuals disproportionately seek intensive services, potentially increasing resource concentration and wait times [
4]. In Alberta, targeted programs for high-need youth and other priority groups may concentrate demand within specific service lines, reinforcing the need to match the workforce and infrastructure to population needs [
1,
3].
Provider-induced demand (PID). Clinician influence on service intensity can contribute to overuse, especially where payment or performance incentives reward volume. Although PID is typically less prominent in publicly funded systems, rapid scale-up of virtual and community-based services can alter incentives and monitoring needs [
4,
7]. Where standardized protocols and performance monitoring exist, they may mitigate unnecessary repeat visits while protecting access [
8].
Information asymmetry. In mental health, low health literacy, stigma, and limited outcome transparency can distort help-seeking and reduce accountability. Alberta has pursued outreach and culturally adapted services, yet gaps in real-time outcome and equity measurement limit system learning and targeted improvement [
2,
3]. Without accessible performance information, both underuse (among underserved groups) and congestion (in high-visibility services) can persist.
3.3. Alberta’s Policy–Economic Positioning
From a health economics perspective, Alberta’s COVID-era response can be interpreted as an attempt to address multiple market failures simultaneously—improving access under a zero-copayment design while expanding capacity through digital delivery and recovery-oriented infrastructure [
3,
4]. In this study, we avoid interpreting modeled values as observed prices. Instead, we use an illustrative simulation to examine how coordinated shifts in capacity and uptake could increase equilibrium quantity under a publicly financed system, while highlighting equity-relevant constraints where Alberta-specific elasticities and marginal costs are unavailable.
3.4. Comparative Policy Context
To situate Alberta’s approach, we provide a concise comparison with selected jurisdictions that also expanded tele-mental health and community-based services during COVID-19. These comparisons are used to frame plausibility and policy relevance rather than to generate comparative effectiveness estimates.
Ontario (Canada). Ontario’s more centralized planning and performance infrastructure—via Ontario Health’s Mental Health and Addictions Centre of Excellence, which establishes provincial oversight, common performance indicators, and shared infrastructure—provides a contrast to Alberta’s decentralized and programmatic expansion [
8].
Australia and the United Kingdom. Both contexts expanded telehealth and remote access during COVID-19, but implementation barriers (digital literacy, uneven access to video platforms, and persistent uptake inequities) were reported, especially among underserved populations [
9,
10].
United States and European Union. Insurance design and reimbursement structures shaped utilization and equity, with cost-sharing and fragmented coverage creating distinct barriers and incentives compared with single-payer settings. However, persistent treatment gaps have been documented in multiple regions, highlighting that coverage expansion alone may not close disparities without culturally relevant services and targeted outreach [
11,
12,
13].
Overall, Alberta’s experience is consistent with a broader post-pandemic policy trend toward digital access and community-based recovery supports. The remaining challenge is aligning capacity expansion with equity goals and transparent performance measurement in a decentralized system.
Taken together, this literature and policy context motivates a two-part analytic approach. First, we summarize empirically reported program delivery outputs from Alberta’s 2023–2024 Mental Health and Addiction Annual Report, and aggregate public reporting to describe implementation performance during the reporting period. Second, because Alberta-specific elasticities and unit costs are not consistently available in public sources, we use an illustrative supply–demand simulation calibrated to reported trends to examine the directional implications of simultaneous shifts in service capacity and help-seeking under a zero-copayment design. The Methods section below specifies data sources, parameter assumptions, and the uncertainty analyses used to ensure that modeled outputs are interpreted transparently as simulations rather than observed market prices or utilization counts.
4. Methodology
4.1. Design
The study used a document-based policy evaluation, combined with an illustrative health economics simulation, to examine Alberta’s system-level response to pandemic-era increases in mental health service need. We applied a supply–demand framework to interpret how publicly funded interventions—particularly CASA Mental Health classroom expansion, the Virtual Opioid Dependency Program (VODP), and recovery communities—could shift service capacity and utilization during the 2023–2024 fiscal year [
3]. The analysis is intended to clarify
directional system dynamics (capacity expansion and access) rather than estimate patient-level clinical effects. The economic component is an
illustrative simulation designed to transparently communicate mechanisms and key drivers, consistent with good modeling practice guidance [
14]. Because the objective was explanatory (mechanism-focused),
no formal economic evaluation (e.g., cost-effectiveness/cost-utility), resource valuation, or health outcome valuation (e.g., QALYs) was undertaken; instead, the model is used to explore plausible directional implications under limited parameter availability, consistent with the role of early/illustrative modeling in informing decisions under uncertainty in innovations [
15].
4.2. Data Sources
Empirical inputs were extracted from the Government of Alberta’s
2023–2024 Mental Health and Addiction Annual Report [
3], including program delivery volumes, planned versus actual service outputs, indicators of service deployment, and infrastructure and system investment descriptions. We used Russell et al. (2024) to contextualize utilization trends in youth mental health care during the pandemic period in Alberta [
2]. Additional sources were used for conceptual framing and parameterization when Alberta-specific estimates were unavailable, including foundational health economics references [
4], evidence on utilization responses to cost-sharing from the RAND Health Insurance Experiment [
6], and the supplier-induced demand literature, which is used to motivate sensitivity analyses around provider behavior [
7].
4.3. Assumptions and Parameters
The simulation required simplified assumptions to translate public reporting into an interpretable supply–demand representation. Key assumptions were:
Capacity expansion modeled proportionally: The reported scale-up in service capacity during 2023–2024 was modeled as a proportional rightward shift in supply, applied uniformly across major population groups (e.g., rural, youth, and Indigenous), given the absence of stratified administrative data in public sources [
3].
Zero user copayment by design: Because Alberta’s publicly funded services maintain
zero user copayment, the user price was treated as 0 CAD. For illustrative purposes only, we used a
unit cost proxy (CAD/service) that is not an observed market price and is not a patient copayment [
6].
Quality held constant across regions and modalities: In the absence of comparable public outcome measures by geography or modality, we assumed no systematic quality differences across regions and delivery channels, consistent with published service protocols and clinical guidance [
16].
Alberta Specific Estimates: Where Alberta-specific estimates of marginal cost and price elasticity were unavailable, we used Canadian benchmarking sources to contextualize spending levels and plausible resource ranges (e.g., CIHI NHEX) [
17]. Plausible elasticity ranges were informed by evidence on utilization responses to cost-sharing [
6] and aligned with standard health economics guidance [
4].
The demand shift was calibrated to ΔD = +27 services/month (bounds 20–35), based on Russell et al. (2024), which reported a +27.24/month increase in youth GP mental health visits per 100,000 after the initial pandemic drop; this was used as an illustrative demand-shift magnitude [
2].
A complete parameter table (base values, bounds, units, and source attribution) is provided in Supporting Information and the OSF repository to support transparency and reproducibility.
4.4. Supply–Demand Simulation Modeling
We used an illustrative supply–demand simulation to represent system-level changes in Alberta’s publicly funded mental health services during the 2023–2024 fiscal year. The analytic perspective was the provincial public payer/system perspective, focusing on publicly funded capacity and program outputs rather than patient-level outcomes. The time horizon was 12 months; therefore, discounting was not applied. Monetary values are reported in Canadian dollars (CAD) and reflect the 2023–2024 reporting period; no inflation or purchasing power parity adjustments were applied.
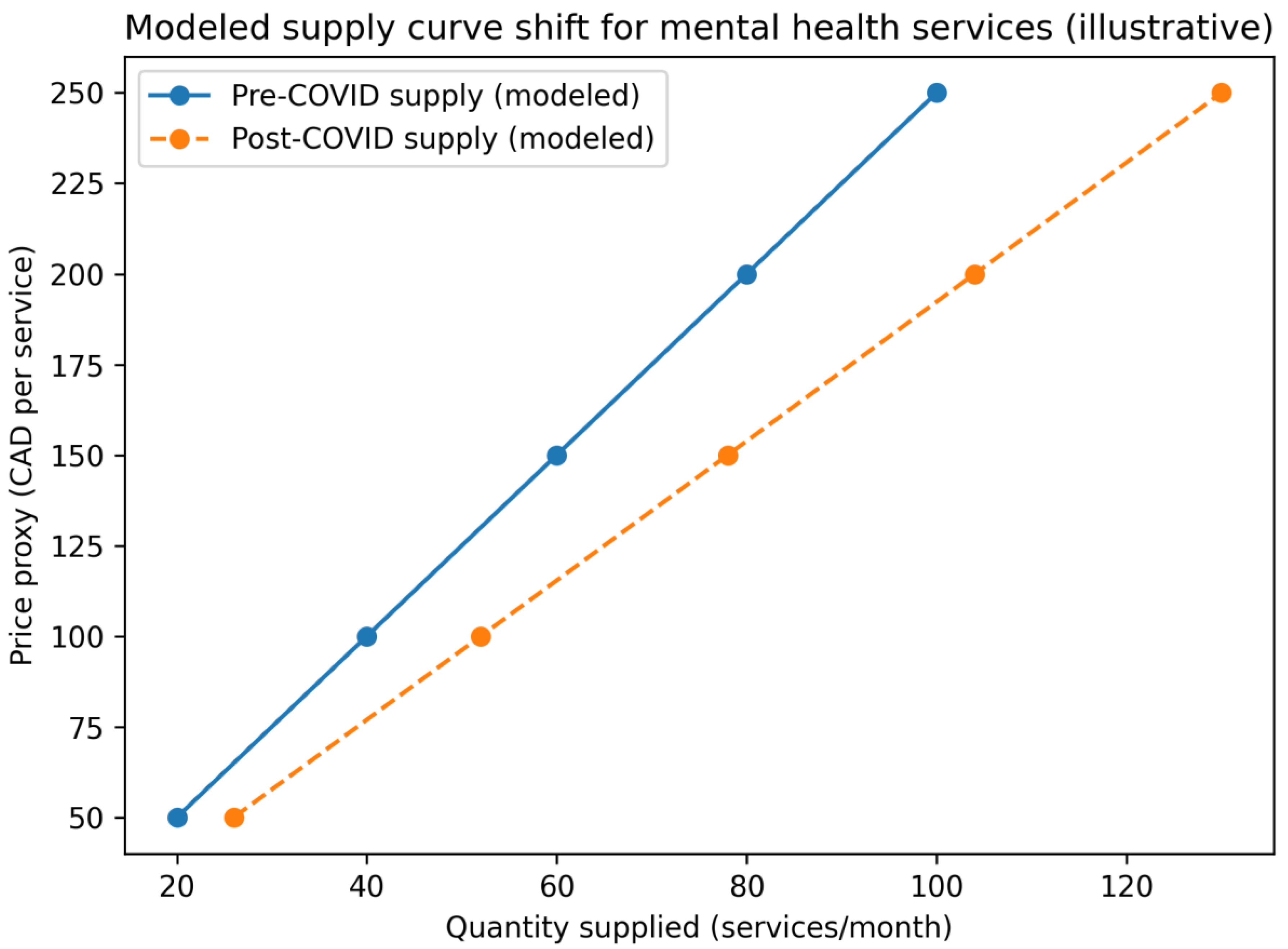
Supply Curve Shift (Modeled)
Supply expansion was modeled as a rightward shift in the supply curve, reflecting reported increases in service capacity attributable to workforce expansion, digital delivery modalities, and recovery-oriented infrastructure investments documented in Alberta’s 2023–2024 Annual Report [
3], supported by standard health economics framing [
4].
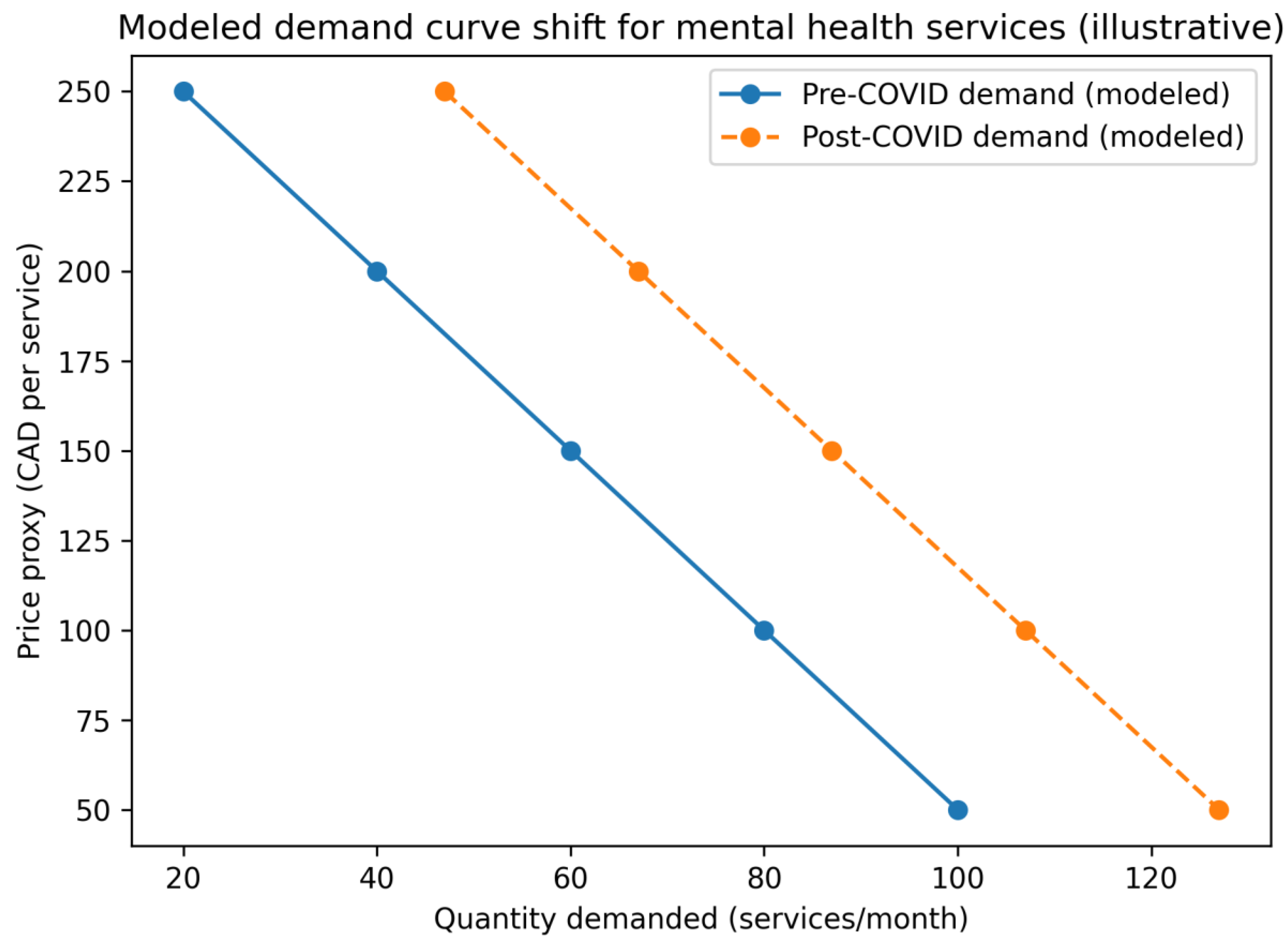
Demand Curve Shift (Modeled)
Demand growth was modeled as a rightward shift in the demand curve, reflecting increased help-seeking associated with pandemic-related distress, destigmatization, and improved accessibility through interventions such as same-day virtual opioid dependency care (VODP) and youth-focused programming [
2,
3].
Interpretation of “Price” and Equilibrium Effects
Because Alberta’s publicly funded mental health services operate under a zero-user copayment policy, the user price is treated as 0 CAD. To express equilibrium relationships in interpretable units, we used a unit-cost proxy (CAD/service) for modeling convenience. This unit cost proxy is not an observed market price and should not be interpreted as a measured transaction price; it is used only to illustrate equilibrium mechanics in a publicly financed setting.
Model outputs in Tables and Figures are synthetic simulation outputs calibrated to reported trends and explicitly labeled as modeled results to avoid confusion with empirically observed data. Empirical program delivery metrics, extracted directly from public reporting (e.g., planned versus actual services delivered), are reported separately in the Results section as observed outputs.
Software and Reproducibility
All calculations and figure/tabular outputs were produced in Microsoft Excel for Mac (Version 16.104 [build 25121423]). Data sources, parameter values (with bounds), assumptions, and sensitivity/scenario checks are archived in the OSF repository: Registration DOI: 10.17605/OSF.IO/6DBFU, associated project: https://osf.io/e6n7w, along with reproduction instructions.
Reporting and Transparency
We used the CHEERS 2022 statement to guide transparent reporting of methods and model-related assumptions where applicable; however, this study is a document-based policy analysis with an illustrative simulation and does not report a full health economic evaluation (e.g., costs and consequences comparison, ICERs/QALYs). Therefore, CHEERS items relevant to context, methods, assumptions, uncertainty, and reporting were addressed, and non-applicable items were noted in the completed checklist (Supplementary File, OSF). [
19]
5. Results
This section distinguishes empirical results (directly observed program outputs from public reports) from modeled results (synthetic supply–demand simulations calibrated to reported trends). Modeled values should not be interpreted as directly observed market prices or utilization counts unless explicitly identified as empirical.
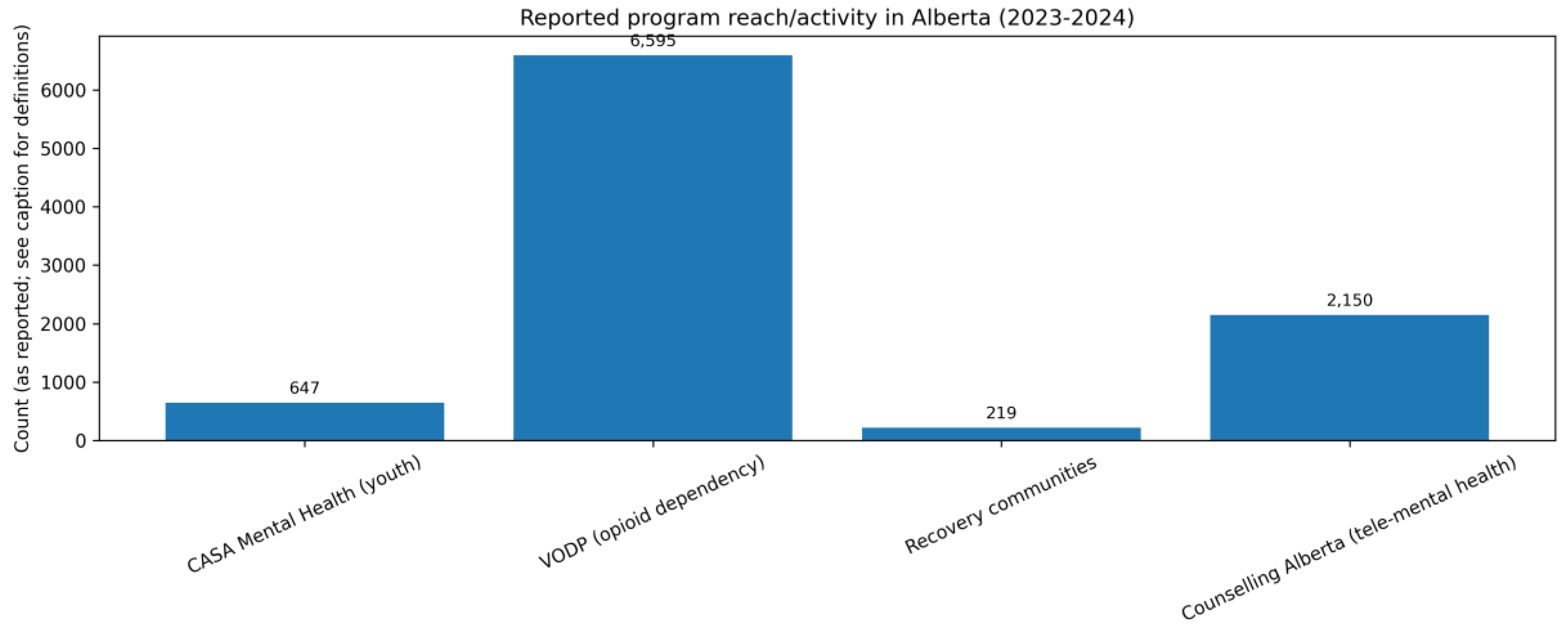
5.1. Empirical Results: Observed Program Delivery Indicators (2023–2024)
Actual delivery included 96 students in CASA classrooms (exceeding the 6 planned additions), 7,217 new VODP admissions (with expansions funded but no specific numeric target stated), 219 clients in recovery communities (toward 700 beds planned), and ~12,300 tele-mental health sessions (with 14 counsellors added). As shown in
Table 1 and
Figure 1, actual delivery exceeded planned targets for CASA, VODP, and tele-mental health, while recovery communities delivered slightly below plan.
This figure summarizes
empirically reported planned targets and actual services delivered for key publicly funded programs during the 2023–2024 fiscal year. Actual delivery exceeded planned targets for CASA, VODP, and tele-mental health, while recovery communities fell slightly below plan, which may reflect implementation timing or capacity constraints.
Source: Government of Alberta Annual Report (2023–2024). [
3]
These empirical delivery outputs indicate implementation performance during the reporting period and provide the observed context for the modeled equilibrium illustrations presented below.
5.2. Modeled Results: Supply–Demand Simulations (Illustrative Equilibrium Shifts)
We next present modeled supply–demand simulations calibrated to reported trends to illustrate how simultaneous shifts in service capacity and demand could yield a higher equilibrium quantity under a zero-copayment policy design. These modeled outputs are illustrative simulations intended to show directional effects and equilibrium mechanics; they are not direct observations of market prices or system-wide utilization.
5.2.1. Modeled Demand Shift
Modeled demand increased in response to improved awareness, reduced stigma, and expanded access (including CASA and VODP), as reflected by a rightward shift from D₁ to D₂. As shown in
Table 2 and
Figure 2, the illustrative simulation depicts a rightward shift in modeled demand (D₁→D₂), consistent with increased help-seeking and improved access reported during the period. The model and calibration are based on reported trends rather than observed utilization counts.
5.2.2. Modeled Supply Shift
Modeled supply increased following capacity expansion through workforce measures, telehealth scale-up, and recovery-oriented infrastructure, represented as a rightward shift from S₁ to S₂
. As shown in
Table 3 and
Figure 3, the illustrative simulation depicts a rightward shift in modeled supply (S₁→S₂), consistent with reported capacity expansion through workforce measures, tele-mental health scale-up, and recovery-oriented infrastructure; values are modeled and not direct measures of system-wide supply.
5.2.3. Modeled Equilibrium Comparison
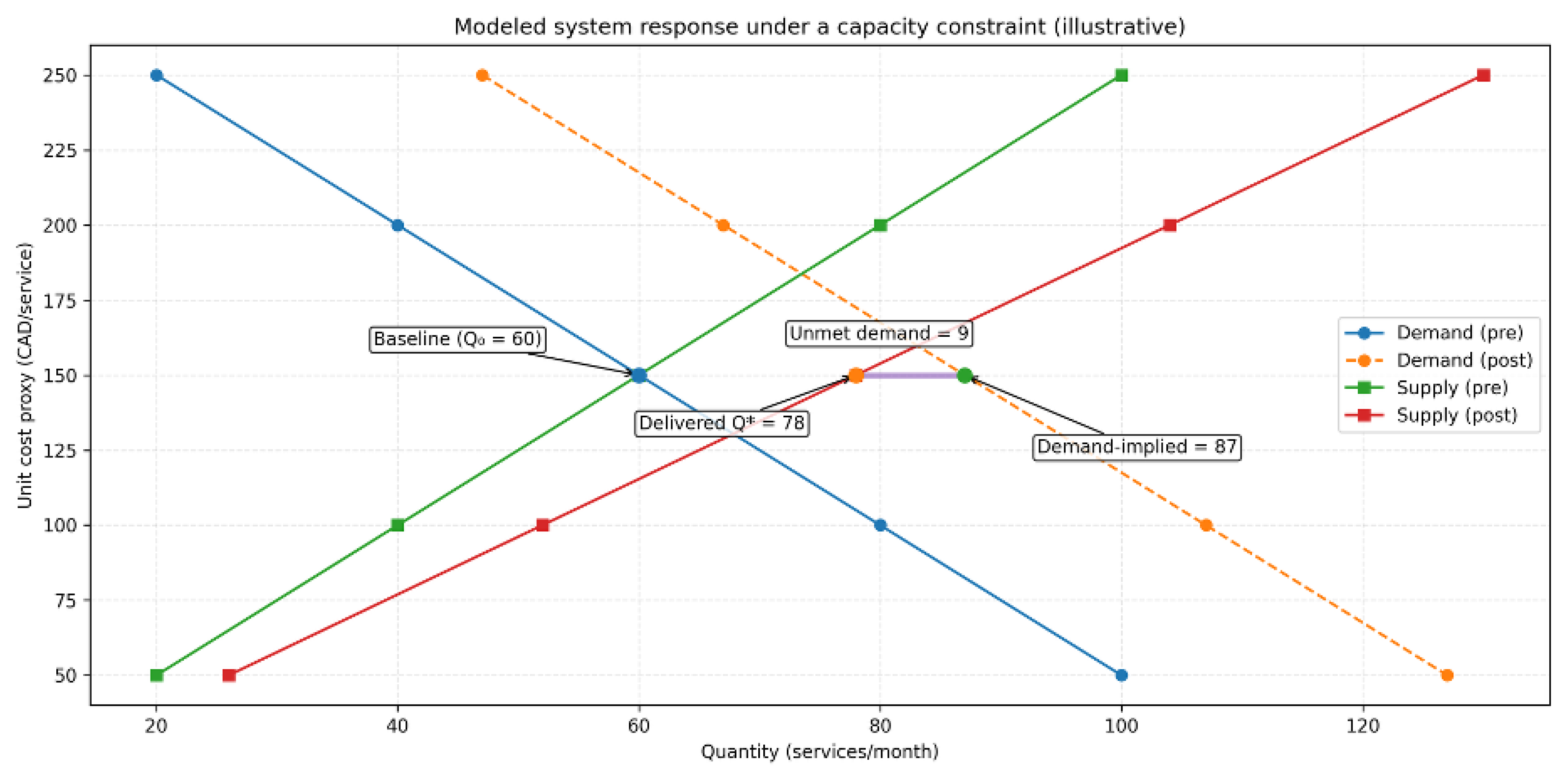
The modeled intersection of post-intervention supply and demand curves (S₂ ∩ D₂) illustrates a higher but capacity-constrained equilibrium quantity under a zero-copayment environment. Using the baseline calibration:
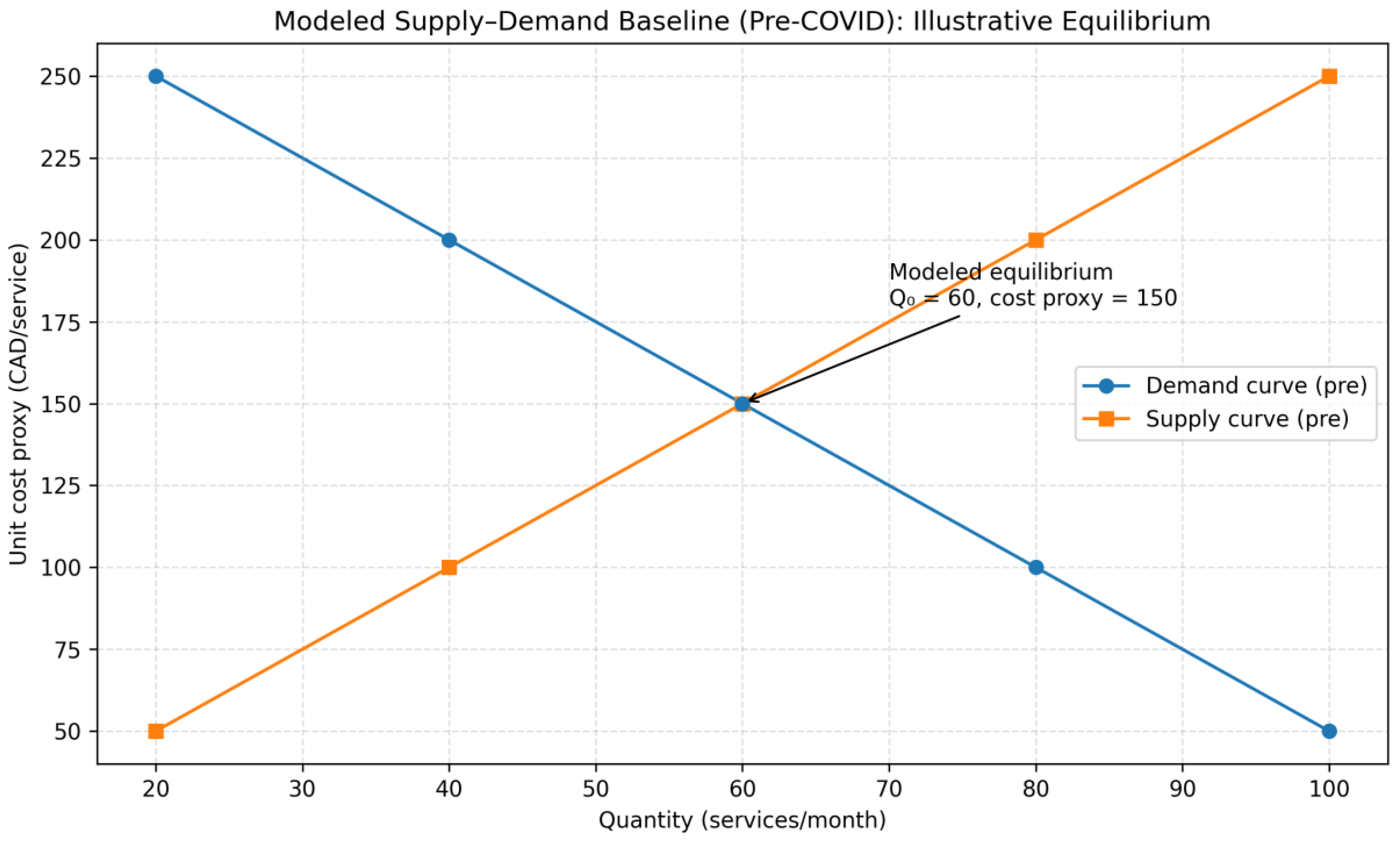
Pre-intervention modeled equilibrium: Q₀ = 60 services/month at a unit cost proxy of 150 CAD/service
Demand-implied post-intervention volume: 87 services/month at the same unit cost proxy (150 CAD/service)
Capacity-constrained post-intervention equilibrium: Q* = 78 services/month at the same unit cost proxy (150 CAD/service), implying ~9 services/month unmet demand (interpreted as potential congestion/queueing rather than additional utilization)
Because Alberta’s publicly funded services are designed to maintain zero user copayment, the unit cost proxy is used only to express modeled equilibrium relationships in interpretable units. It should not be interpreted as an observed market price. The modeled stability of the unit cost proxy alongside an increase in equilibrium quantity is consistent with the theoretical expectation that proportional outward shifts in supply and demand can increase utilization without increasing user-facing prices in publicly financed settings [
4,
6]. However, when demand growth outpaces capacity expansion (as in the base case), the simulation implies a supply-constrained system, in which additional help-seeking does not fully translate into delivered services.
Implications: The simulation suggests that coordinated capacity expansion may partially offset demand growth in a zero-copayment setting; however, the magnitude of modeled effects depends on parameter assumptions and should be interpreted directionally, with potential for unmet need if capacity lags. As shown in
Figure 4 and
Figure 5, the modeled equilibrium quantity increases from Q₀=60 to Q*=78 services/month under the illustrative calibration, while the unit-cost proxy is held constant for visualization; this proxy is not an observed market price and does not represent patient copayments (0 CAD by policy design).
5.3. Uncertainty and Robustness: Deterministic Sensitivity And Scenario Checks
Uncertainty was assessed using deterministic one-way sensitivity analyses on a small set of influential parameters specified a priori: the magnitude of capacity expansion, the magnitude of demand increase, and baseline equilibrium utilization. For each parameter, we applied conservative low–high bounds informed by public reporting when available and by benchmark/guideline sources otherwise, holding other inputs constant [
14,
19]. As shown in
Table 4, the modeled equilibrium quantity (Q*) varies across plausible bounds, indicating that the
magnitude of the modeled effect is sensitive to assumptions where Alberta-specific parameters are unavailable. Importantly, the sensitivity results also clarify a
capacity-constrained implication: when demand shifts are large relative to capacity expansion, additional need does not translate into proportionate increases in delivered volume. Instead, the model implies rising
unmet demand, operationalized as congestion/queueing pressures beyond Q*, reinforcing that expansion may stabilize access only if capacity growth keeps pace with demand growth.
Whereis the modeled demand increase (additive), andis the modeled capacity expansion (proportional). When, the system is supply-limited:reflects deliverable volume and the remainder is interpreted as unmet demand (queueing/congestion) rather than additional utilization. Ranges are conservative and intended as directional robustness checks consistent with modeling and reporting guidance [
14,
19]
. Values are rounded to whole services.
6. Discussion
6.1. Interpreting Alberta’s System Response in Context
Alberta’s pandemic-era expansion of publicly funded mental health services illustrates how policy action can support access under a zero-copayment design. Empirically, program delivery met or exceeded planned targets for several initiatives, suggesting strong implementation performance during 2023–2024 [
3]. In the illustrative supply–demand simulation, outward shifts in modeled demand and capacity increased the modeled equilibrium quantity (
Figure 2,
Figure 3,
Figure 4 and
Figure 5), consistent with the economic expectation that capacity expansion can partially offset increases in service use when financial barriers are low [
4,
6]. These outputs are simulations calibrated to reported trends and should be interpreted as mechanisms rather than observed prices or system-wide utilization counts.
6.2. Economic Frictions and Ethical Trade-Offs
Alberta’s approach is plausibly responsive to well-described frictions in health care markets, including moral hazard under low user cost and information asymmetry [
4,
6]. It also occurs in a broader context of persistent unmet need and access gaps documented across jurisdictions [
12,
13]. Supplier-induced demand is a relevant behavioral consideration when clinical discretion and service intensity interact with incentives and monitoring capacity; in this study, it is most appropriate as a rationale for sensitivity analysis around provider behavior rather than as evidence of overuse in Alberta [
7].
Equity–efficiency trade-offs remain. Expansion can still yield uneven benefits if lower-acuity users in better-served areas absorb new capacity while rural or remote communities face structural barriers to access [
13]. Even with zero user copayments, opportunity costs persist—including workforce strain, congestion, and possible diversion from other services—risks that are difficult to quantify solely through public reporting [
3,
16].
6.3. Comparative Insight and Transferability
Relative to more centralized coordination and performance-monitoring approaches (e.g., Ontario Health’s Mental Health and Addictions Centre of Excellence), Alberta’s programmatic expansion may enable faster rollout but may leave gaps in standardized outcome tracking and equity measurement [
8]. Internationally, tele-mental health scale-up has been widespread, yet uptake inequities related to digital access and literacy remain common across settings [
5,
9,
10]. Alberta’s experience is consistent with post-pandemic calls for integrated systems that combine digital access with community-based pathways [
5]. Sustained gains likely depend on strengthening data infrastructure, performance measurement, and equity-focused implementation over time [
5,
8,
10].
Taken together, Alberta’s experience suggests that rapid capacity expansion can partially accommodate pandemic-era demand pressures in a publicly financed, zero-copayment context, but that sustainability depends on workforce, equity in access, and performance infrastructure. Broader national and global guidance similarly emphasizes that mental health system strengthening requires durable financing, integrated community and digital pathways, and accountability mechanisms that make access and outcomes visible over time [
17,
20,
21,
22].
7. Policy Implications and Recommendations
Workforce capacity and distribution. Sustaining post-crisis access will likely require workforce strategies that address geographic maldistribution (e.g., rural/remote), stabilize recruitment and retention, and support supervised practice pathways for multidisciplinary teams—paired with explicit service targets and monitoring [
3,
16].
Telehealth as a permanent modality, with equity safeguards. Tele-mental health can extend reach, but equitable benefit depends on broadband availability, provider competency in virtual care, and patient-facing supports (digital literacy, navigation, language accessibility). Monitoring should explicitly track who is and is not reached by virtual pathways [
5,
9,
10].
Sustainable financing and governance beyond “surge” dynamics. If crisis-period funding enabled rapid rollout, longer-term performance depends on clearer recurrent financing arrangements and governance mechanisms that prevent volatility, define accountability, and protect equity objectives (e.g., explicit reporting requirements and outcome expectations) [
20,
21,
22].
Equity-focused implementation and culturally safe pathways. Because access gaps persist even in publicly funded systems, reforms should include explicit equity design features (e.g., navigation supports, culturally safe pathways, and community partnerships where appropriate) and the measurement of distributional effects (e.g., by geography and other policy-relevant equity markers) [
12,
13,
20].
Data-driven performance monitoring and transparency. Decentralized expansion benefits from centralized measurement capacity: standardized indicators, dashboards, and routine public reporting that link service activity to access, timeliness, and outcomes. Ontario’s emphasis on coordination and monitoring illustrates one model of system-level performance infrastructure [
8].
Demand activation paired with throughput capacity. Public awareness and stigma-reduction efforts are most defensible when paired with clear pathways to care (triage/referral clarity, wait-time transparency, stepped-care options), so increased demand does not simply translate into congestion [
5,
20,
21,
22].
8. Limitations
This analysis relies on publicly available reports and secondary sources rather than patient-level administrative data. As a result, program reporting does not consistently provide standardized, disaggregated outcomes (e.g., symptom change, functional improvement, patient-reported experience), equity-stratified utilization, or comparable effectiveness metrics across initiatives [
3]. Cost and economic inputs were also constrained: Alberta-specific marginal costs by service type, demand elasticities, and longer-term cost offsets were not available from public sources and were therefore represented using conservative ranges and bounded assumptions informed by general health economics and related evidence [
4,
6,
17]. These choices support plausibility checks but limit causal inference and precision.
Second, the empirical component focuses on a single fiscal year (2023–2024), which restricts inference about longer-term sustainability, workforce dynamics, and whether post-crisis utilization patterns persist as service models mature [
3,
16]. Third, the simulation is intentionally illustrative: it translates reported trends into an interpretable mechanism-based narrative but should not be read as an estimate of observed prices, system-wide utilization totals, or welfare impacts. Consistent with modeling good-practice guidance, the simulation is best interpreted as a structured sensitivity framework rather than a predictive or causal model [
14,
15]. Also, Public reporting lacks stratified outcomes by equity groups (e.g., Indigenous: 43% recovery capital improvement in MRP, p.20), limiting disaggregated analysis. Finally, we did not estimate program costs, QALYs, ICERs, or budget impact; these analyses were not feasible given the limits of public reporting [
18,
19].
9. Future research
Future work should prioritize five directions:
Patient-level, longitudinal evaluation. Link administrative utilization with outcomes and costs over time to support ROI, budget impact, and longer-horizon assessments where feasible, consistent with Canadian economic evaluation guidance and reporting standards [
18,
19].
Equity-focused measurement. Conduct equity audits that map access, timeliness, and outcomes across rural/remote communities and priority populations, using geographic and demographic stratification, and reflect known cross-jurisdictional disparities [
12,
13].
Program-specific effectiveness beyond volumes. Evaluate CASA, VODP, recovery communities, and tele-mental health using outcomes beyond service counts (e.g., clinical outcomes, continuity, relapse/retention, patient experience), building on the limitations of volume-based reporting [
3,
5].
Workforce sustainability. Examine recruitment/retention, workload, burnout, and skill-mix evolution to test whether capacity gains can be maintained without quality erosion [
16].
Digital equity and implementation design. Quantify barriers to tele-mental health uptake (connectivity, digital literacy, privacy constraints) and test mitigation strategies, drawing on emerging evidence that virtual care can reproduce inequities without targeted supports [
5,
9,
10].
Comparative evaluations across provinces could also clarify how governance and performance infrastructure shape equity and accountability during rapid scale-up—particularly contrasts between more centralized monitoring approaches and decentralized program expansion [
8].
10. Conclusions
Alberta’s 2023–2024 mental health system response suggests that coordinated; publicly funded interventions can expand
reported service delivery during system shocks. Public reporting indicates that several major initiatives met or exceeded planned delivery targets during the period examined [
3]. The accompanying illustrative supply–demand simulation offers a mechanism-based interpretation in which concurrent increases in capacity and help-seeking raise the modeled equilibrium quantity under a zero-copayment design; modeled values should not be interpreted as observed prices or system-wide utilization counts. Sustaining gains likely depends on workforce stabilization, digital equity supports, culturally safe and navigable care pathways, and strengthened performance monitoring so that expansion translates into equitable access rather than uneven uptake or congestion.
Author Contributions
Conceptualization:
Kola Adegoke; Abimbola Adegoke, Methodology:
Deborah Dawodu; Ayoola Bayowa; Temitope Kayode, Formal analysis:
Kola Adegoke; Deborah Dawodu; Temitope Kayode, Investigation:
Ayoola Bayowa; Deborah Dawodu; Akorede Adekoya, Data curation:
Deborah Dawodu; Temitope Kayode; Mallika Singh, Visualization:
Temitope Kayode; Ayoola Bayowa, Writing – original draft:
Kola Adegoke, Writing – review & editing:
Abimbola Adegoke; Temitope Kayode; Mallika Singh; Olajide Alfred Durojaye; Abiodun Isola Aluko; Adeyinka Adegoke, Supervision:
Kola Adegoke; Abimbola Adegoke, Project administration:
Kola Adegoke, Resources:
Akorede Adekoya; Mallika Singh; Olajide Alfred Durojaye; Adeyinka Adegoke. Equal contributions:
Kola Adegoke, Abimbola Adegoke, and Deborah Dawodu contributed equally to this work. All remaining authors also contributed equally to this work as described in the Contributions statement.
Funding
No specific grant or external funding was received for this study.
Author approval
All authors have read and approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Ethics approval and consent to participate
This study used publicly available, aggregate, non-identifiable data from the Government of Alberta and Alberta Health Services reports and published literature. No individual-level human participant data were collected or accessed, and there was no interaction with human participants. Therefore, institutional ethics review and informed consent were not required under applicable regulations and institutional policies.
Data Availability Statement
All materials supporting the findings of this study, including the extracted summary inputs from public reports, README, modeling assumptions/parameter table, analysis workbook(s), and figure files, are available on OSF: Registration DOI 10.17605/OSF.IO/6DBFU, Associated project https://osf.io/e6n7w. Underlying sources remain publicly accessible through the Government of Alberta and Alberta Health Services repositories, as well as the cited literature.
Conflicts of Interest
Author Abiodun Isola Aluko is affiliated with CASA Mental Health (Alberta), which is referenced in this manuscript. His contribution was limited to writing, reviewing, and editing. CASA Mental Health provided no funding, services, or non-public data for this study, and the affiliation did not influence the study design, analysis, interpretation, or conclusions. The remaining authors declare no competing interests.
References
- Racine, N; McArthur, BA; Cooke, JE; Eirich, R; Zhu, J; Madigan, S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatrics 2021. [Google Scholar] [CrossRef] [PubMed]
- Russell, MJ; Urichuk, L; Parker, N; Agyapong, VIO. Youth mental health care use during the COVID-19 pandemic in Alberta, Canada: an interrupted time series, population-based study. Child Adolesc Psychiatry Ment Health. 2024. Available online: https://link.springer.com/article/10.1186/s13034-024-00785-1.
- Government of Alberta. 2023–24 Mental Health and Addiction Annual Report; Alberta Health: Edmonton, 2023; Available online: https://open.alberta.ca/dataset/610118c0-60ce-4ca1-9ef6-16fa703e46b7/resource/f43fcaad-bd2b-42e9-a7b4-657000baff95/download/mha-annual-report-2023-2024.pdf.
- Folland, S; Goodman, AC; Stano, M; Danagoulian, S. The Economics of Health and Health Care, Available from, 9th ed.; Taylor & Francis: Abingdon, 2024. [Google Scholar] [CrossRef]
- Moreno, C; Wykes, T; Galderisi, S; Nordentoft, M; Crossley, N; Jones, N; et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Manning, WG; Newhouse, JP; Duan, N; Keeler, EB; Benjamin, B; Leibowitz, A; et al. Report No.: R-3476-HHS; Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. RAND Corporation: Santa Monica (CA), 1988. Available online: https://www.rand.org/content/dam/rand/pubs/reports/2005/R3476.pdf.
- Labelle, R; Stoddart, G; Rice, T. A re-examination of the meaning and importance of supplier-induced demand. Journal of Health Economics 1994, 13, 347–368. [Google Scholar] [CrossRef] [PubMed]
- Ontario Health. Mental Health and Addictions Centre of Excellence [Internet]; Ontario Health: Toronto (ON), 2025 [updated 2025 Jun 18; cited 2025 Dec 31; Available online: https://www.ontariohealth.ca/clinical/mental-health-addictions/program.
- Robinson, L; Parsons, C; Northwood, K; Siskind, D; McArdle, P. Patient and clinician experience of using telehealth during the COVID-19 pandemic in a public mental health service in Australia. Schizophr Bull Open. 2023, 4, sgad016. [Google Scholar] [CrossRef] [PubMed]
- Confederation, NHS. Mental Health Services and COVID-19: Policy and Practice Review; NHS Confederation: London, 2022; Available online: https://www.nhsconfed.org/publications/mental-health-services-and-covid-19.
- Shi, L; Singh, DA. Essentials of the US health care system, 6th ed.; Jones & Bartlett Learning: Burlington (MA), 2023; Available online: https://www.jblearning.com/catalog/productdetails/9781284235128.
- Kohn, R; Ali, AA; Puac-Polanco, V; Figueroa, C; López-Soto, V; Morgan, K; et al. Mental health in the Americas: an overview of the treatment gap. Rev Panam Salud Publica 2018, 42, e165. [Google Scholar] [CrossRef] [PubMed]
- Zigante, V; Hodin, M; Muir, T. Inequalities in access to mental health services across the EU: evidence and policy responses; European Commission: Brussels, 2022; Available online: https://data.europa.eu/doi/10.2767/854582.
- Caro, JJ; Briggs, AH; Siebert, U; Kuntz, KM. Modeling good research practices--overview: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-1. Med Decis Making 2012, 32, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Grutters, J. P.; Govers, T.; Nijboer, J.; Tummers, M.; van der Wilt, G. J.; Rovers, M. M. Problems and Promises of Health Technologies: The Role of Early Health Economic Modeling. International Journal of Health Policy and Management 2019, 8, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Alberta Health Services. 2022–2023 Annual Report; AHS: Edmonton, 2023; Available online: https://www.albertahealthservices.ca/assets/about/publications/ahs-pub-pr-2022-23-q4.pdf#page=41.
- Canadian Institute for Health Information. Public Health and Community Mental Health and Substance Use Services in NHEX — Technical Note. CIHI: Ottawa (ON), Nov 2025. Available online: https://www.cihi.ca/sites/default/files/document/public-health-community-mhsu-services-nhex-tech-note-2025-en.pdf.
- Canadian Agency for Drugs and Technologies in Health (CADTH). Guidelines for the Economic Evaluation of Health Technologies: Canada., 4th ed.; Ottawa (ON): CADTH; 2017. Available from: CADTH Methods and Guidelines page, 31 Dec 2025; Available online: https://www.cda-amc.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf.
- Husereau, D; Drummond, M; Augustovski, F; de Bekker-Grob, E; Briggs, AH; Carswell, C; et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMJ 2022, 376, e067975. [Google Scholar] [CrossRef] [PubMed]
- Canadian Mental Health Association. Federal Plan for Universal Mental Health & Substance Use Health: Background Paper; CMHA: Ottawa, 2022; Available online: https://cmha.ca/wp-content/uploads/2022/11/AfMH-White-Paper-EN-FINAL.pdf.
- World Health Organization. Mental Health Preparedness and Response for the COVID-19 Pandemic; WHO: Geneva, 2020; Available online: https://apps.who.int/gb/ebwha/pdf_files/EB148/B148_20-en.pdf.
- Patel, V; Saxena, S; Lund, C; Thornicroft, G; Baingana, F; Bolton, P; et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).