1. Introduction
Extensive jaw defects occur in treatment of patients with oral and maxillofacial diseases such as malignant tumor, benign tumor, cleft lip and palate, trauma, medication-related osteonecrosis of the jaw, and osteoradionecrosis (ORN). These patients are treated with usual dental prostheses, such as dental bridges, denture, and maxillofacial prosthesis, but may have difficulty with recovery of masticatory and swallowing function and esthetic appearance [
1]. Functional recovery using dental implants is an effective procedure in such patients [
2,
3].
In Japan, treatment with dental implants for functional recovery of jaw defects has been covered by Japanese public health insurance since 2012 [
4]. Thus, the economic burden has been substantially reduced for patients with jaw defects who desire functional recovery using dental implants [
5]. The survival rate of dental implants in patients with extensive jaw defects is likely to be lower than that in patients with a usual dent-alveolar defects due to periodontal disease, dental trauma, and dental caries [
6].
In this study, in order to know the current situation of the dental implant treatments in patients with extensive jaw defects after treatment for various oral and maxillofacial diseases in our hospital, we investigated the clinical background of those patients and prognosis of the dental implants. Additionally, we extracted factors related to the loss of dental implants and assessed the recovery of the masticatory function of the patients.
2. Patients, Materials and Methods
2.1. Patients
We examined 43 patients who underwent dental implant treatment that was covered by the Japanese public health insurance system at Dokkyo Medical University Hospital between 2012 and March 2024. All patients had previously undergone treatment for malignant or benign tumors, cleft lip and palate, trauma or ORN.
2.2. Examined Items
The following information was retrospectively retrieved from the electronic medical records: the patients’ gender, age, primary maxillofacial disease, method of anesthesia for implant surgery, type of bone for implant placement (existing bone or grafted bone), number of dental implants, implant placement site (maxilla or mandible), type of prosthesis (fixed or removable, cantilever or others), prognosis of the dental implants and masticatory function of the patients.
2.3. Assessment of the Masticatory Function of the Patients After Dental Implant Treatments
The masticatory function of ten patients who had undergone dental implant treatment and agreed to participate in the study was measured quantitatively using gummy jellies [
7]. The instruction to patients was to chew gummy containing glucose (Glucorum
®, GC, Tokyo, Japan) for 20 seconds, rinse the mouth with 10 mL of water, and spit out the gummy and water into a mesh filter. The glucose concentration in the collected filtrate was measured using a glucose-measuring device (Gluco Sensor GS-II
®, GC, Tokyo, Japan), with a higher concentration indicating a higher masticatory function. Seven patients with removable dentures underwent tests three times before and after placing the dentures, and 3 patients with fixed prosthesis underwent tests three times. The masticatory function of the patients was compared with that of 3 healthy individuals with natural dentition.
2.4. Statistical Analysis
The survival rates of dental implants for 40 patients who had completed the final prosthesis process were analyzed by gender, age (≥75/<75 years), primary disease (malignant tumor/others), implant site (maxilla/mandible), type of bone (existing bone/grafted bone), type of prosthesis (cantilever/others), and whether or not the patient received radiotherapy by univariate and multivariate analyses. A two-sided 95% confidence interval (CI) was estimated using Cox proportional hazards models. Differences in masticatory function of the patients from before to after denture placement over dental implants were examined by Friedman test. Differences of the masticatory function between patients with fixed prosthesis on dental implants and individuals with natural dentition were examined by Mann-Whitney test. All analyses were conducted using IBM SPSS ver. 30.0 (IBM SPSS, Inc., Tokyo, Japan) with a significance level of 0.05.
2.5. Ethics
The study was approved by Dokkyo Medical University Hospital Ethics Committee (R-72-13J) as an opt-out study. No patients or their representatives requested to be excluded from the study.
3. Results
3.1. Characteristics of the Patients
3.1.1. Gender and Age
The patients comprised 26 males and 17 females aged from 19 to 89 years (mean: 59.8 years, 33 patients over 75 years and 10 patients under 75 years) at the time of dental implant treatments (
Table 1).
3.1.2. Background of Primary Deseases of the Patients
The primary diseases of the patients were malignant tumor (n=24), benign tumor (n=12), cleft lip and palate (n=3), trauma (n=2), and ORN (n=2) (
Table 1). Malignant tumor included lower gingival carcinoma (n=13), upper gingival carcinoma (n=8), buccal mucosa carcinoma (n=1), carcinoma of the oral floor (n=1), and maxillary sinus carcinoma (n=1). The clinical stages of malignant tumor were I (no cases), II (n=4), III (n=2), IVa (n=16) and IVb (n=2). Benign tumor included ameloblastoma (n=9) and odontogenic keratocyst (referred to as keratocystic odontogenic tumor until 2017) (n=3).
Of the 3 patients with cleft lip and palate, one patient underwent an operation at our hospital for cleft lip and palate, and had subsequent placement of dental implants of the grafted iliac cancellous bone on the cleft. The second patient underwent an operation for cleft lip and palate at another hospital. The third patient underwent an operation for cleft lip and palate and iliac cancellous bone graft on the cleft, and an operation for jaw deformity at another hospital. However, in this patient, oronasal fistula remained, a titanium plate used for the jaw deformity surgery was exposed, and two residual roots in the maxillary teeth were found.
One patient with trauma had extensive dent-alveolar defects from the maxillary right canine tooth to the maxillary left first molar.
Two patients had ORN developed after chemoradiotherapy for oropharyngeal cancer in the Department of Otolaryngology/Head and Neck Surgery.
3.1.3. Treatment of the Primary Oral and Maxillofacial Diseases
All patients with malignant tumor were treated in our department except 1 patient with maxillary sinus carcinoma. Malignant tumors were treated by partial maxillectomy (n=7), subtotal maxillectomy (unilateral subtotal maxillectomy + sphenoid pterygoid process resection) (n=2), marginal mandibulectomy (n=4), segmental mandibulectomy + titanium plate reconstruction (n=4), segmental mandibulectomy + vascularized fibular flap (n=5), partial maxillectomy + marginal mandibulectomy (n=1), and partial maxillectomy + segmental mandibulectomy + titanium plate reconstruction (n=1). Radiotherapy was performed before dental implant placement in 3 patients with a malignant tumor (lower gingival carcinoma, upper gingival carcinoma, and maxillary sinus carcinoma). One patient with maxillary sinus carcinoma underwent chemoradiotherapy in the Department of Otorhinolaryngology/Head and Neck Surgery. Radiotherapy was performed after dental implant placement in 2 patients with upper gingival carcinoma and buccal mucosa carcinoma, respectively.
Treatment of benign tumors included partial maxillectomy (n=1), removal of mandibular tumor (n=2), marginal mandibulectomy (n=5), segmental mandibulectomy + iliac crest flap (n=3) (2 free iliac crests and 1 vascularized iliac crest) and segmental mandibulectomy + vascularized fibular flap (n=1). Two patients with ORN underwent segmental mandibulectomy + vascularized fibular flap (
Table 1).
3.2. Dental Implant Treatment
3.2.1. Anesthesia, Timing of Dental Implant Placement and Bone Grafting
Anesthesia for placement of dental implants was done under general anesthesia (n=30), intravenous sedation (n=2) and local anesthesia (n=11). Of the patients under general anesthesia, 9 patients underwent surgery for the primary disease and dental implants simultaneously. Dental implants were done in the existing bone after resection of the primary maxillary tumor (n=8), or after marginal mandibulectomy (n=1). For patients with a tumor (either benign or malignant), the period from tumor resection to dental implant placement ranged from the same day to 10 years.
Eight patients with malignant tumors underwent dental implant placements on the reconstructed fibular flap under general anesthesia. These patients received the dental implant surgery simultaneously with removal of titanium plates and screws used in reconstruction or reduction of the volume of a reconstructed soft tissue flap. One patient underwent free iliac crest (block bone) graft 4 years after marginal mandibulectomy, and then received dental implants surgery 1 years after bone grafting. One patient underwent free gingival graft on the grafted fibular bone before dental implant placements.
Of the patients with benign tumor, 2 patients underwent the iliac cancellous bone grafts and one patient underwent free iliac crest (block bone) graft after marginal mandibulectomy and then dental implant surgery was performed later. One patient with a benign tumor who underwent partial maxillectomy, and he underwent reconstruction with the vascularized fibula flap 2 years after maxillectomy, and then dental implant surgery was performed later. Of the patients with trauma, one patient with extensive dent-alveolar defects underwent iliac cancellous bone graft, and then dental implant surgery was performed later.
3.2.2. Dental Implant Placement Sites and Number of Implants
Several types of dental implants (bone level or tissue level) from several manufacturers (Nobel Biocare, Zurich, Switzerland; Straumann, Basel, Switzerland; Nippon Piston Ring Co. Ltd., Saitama, Japan) were used at the discretion of surgeons. The placement sites and number of dental implants (114 in total) were 25 in maxillary anterior tooth sites, 15 in maxillary molar sites, 30 in mandibular anterior tooth sites, and 44 in mandibular molar sites (
Table 2). Of the dental implants, 20 were placed in the grafted fibula of 10 patients and 27 in the grafted iliac bone of 9 patients (16 dental implants on block bone, 11 dental implants on cancellous bone) (
Table 2). The number of dental implants placed ranged from 1 to 5 per patient.
3.2.3. Type of Prosthesis and Outcomes
Forty of 43 patients completed the final prosthesis with a total of 108 dental implants. Three patients did not complete the final prosthesis after dental implant placement: one had poor general condition; one had cervical lymph node metastasis after primary surgery; and one died due to tumor recurrence. Of the 40 patients with completion of the final prosthesis, 18 had fixed prosthesis (dental crown or bridge) and 22 had removable dentures. Implant over denture was retained with a Dolder bar (n=1) and with locator abutments (n=21). The follow-up period after completion of final prosthesis ranged from 6 months to 78 months. In 1 patient (1 dental implant), a dental implant was lost before the final prothesis, and in 6 patients (8 dental implants), 8 dental implants were lost after denture placement. In 5 patients (5 dental implants), 5 dental implants were left sleeping due to the condition of the implant sites or the soft tissue, although dental implants seemed to have an osteointegration.
3.2.4. Assessment of Masticatory Function
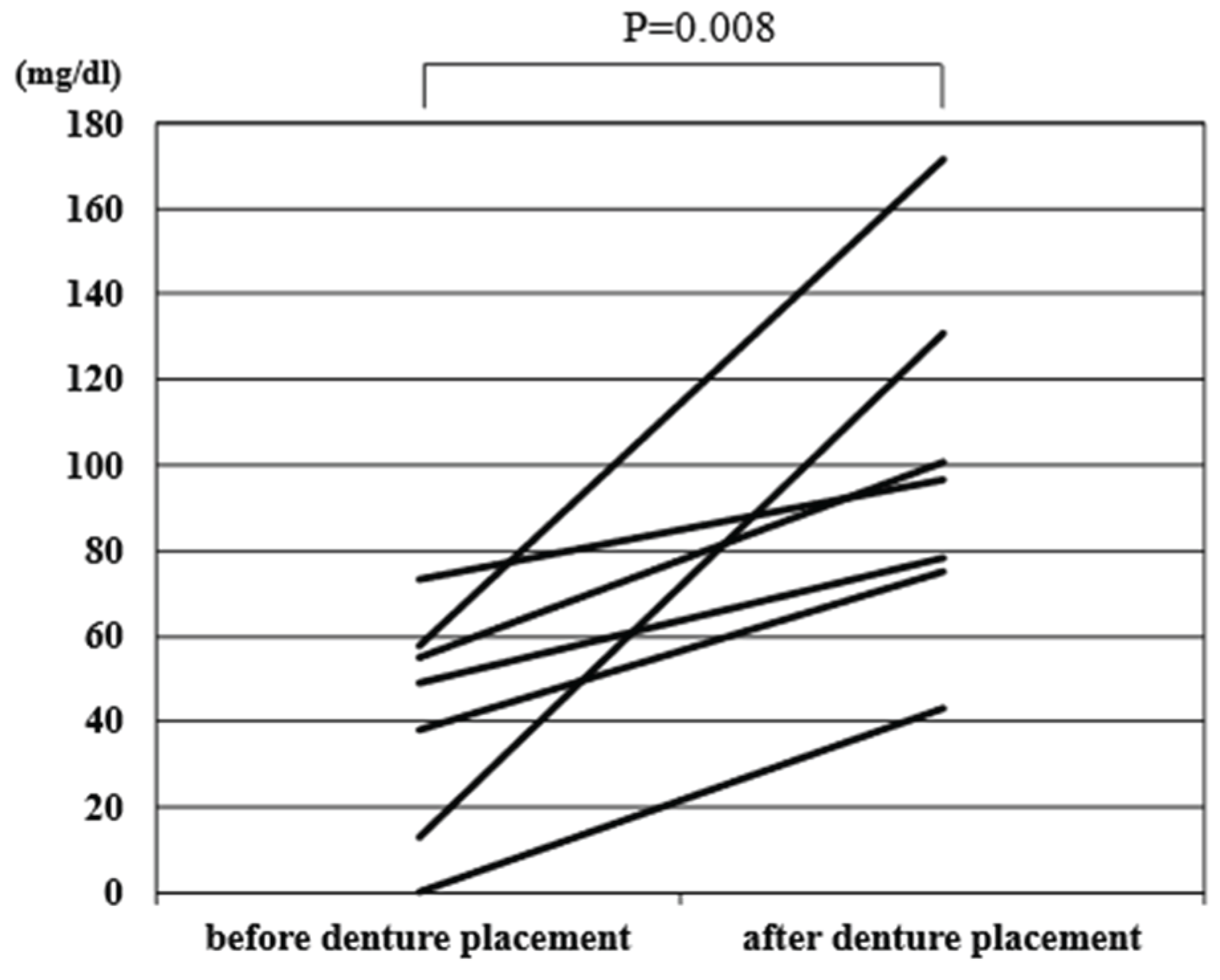
In an assessment of masticatory function, the mean glucose level in 7 patients with a removable denture increased significantly from before to after denture placement (40.9 vs. 99.4 mg/dL, p=0.008) (
Figure 1), indicating improved masticatory function. Masticatory function in 3 patients with fixed prosthesis (glucose: 170.7 mg/dL) was similar to that in 3 persons with natural dentition (glucose: 199 mg/dL) (p=0.08).
The mean glucose level in 7 patients with a removable denture increased significantly from before to after denture placement (40.9 vs. 99.4 mg/dL, p=0.008).
3.3. Prognosis of Dental Implants for Patients with Extensive Jaw Defects After Treatment of Oral and Maxillofacial Diseases
In univariate analysis, loss of dental implants was higher in patients with maxillary dental implants (p=0.025), maxillary cantilever denture retained with implants on existing maxillary bone (p=0.032), and patients who received radiotherapy (p=0.034) (
Table 3). There was no significant difference of the prognosis of dental implants on gender, age, primary disease, or type of bone (existing or grafted) (
Table 3). In multivariate analysis, p value did not reach significant level on implant site (maxilla or mandible) (p=0.102), type of prosthesis (maxillary cantilever denture retained with implants on existing maxillary bone or others) (p=0.783), and whether or not patients received radiotherapy (p=0.084) (
Table 3).
4. Discussion
In this study, we demonstrated that patients with extensive jaw defects after treatment of various oral and maxillofacial diseases could be treated with dental implants with good results. The survival rate of dental implants was 92%, and masticatory function tests showed functional recovery to close to 50% of that in healthy individuals in patients with a removable denture, and to a level similar to that of healthy individuals in patients with fixed prosthesis.
In Japan, dental implant treatments for extensive jaw defects after tumor treatment have been covered by public health insurance since 2012. However, only 43 patients underwent dental implant treatments at our hospital in the past 12 years, out of an estimated 700 patients who could have been treated with insurance-covered implants. Only a few patients want dental implant treatments, probably because patients with a malignant tumor have already undergone highly invasive surgery and are reluctant to undergo reoperation or may be satisfied with their current masticatory function.
Oral squamous cell carcinoma, if it recurs, is known to occur mostly within 2 years. [
8], we believe that postoperative dental implants are best performed 2 years after cancer treatment, when the risk of recurrence has decreased. In most patients with dental implants on existing bone after maxillectomy, the placement of dental implants was performed on the same day of the primary surgery. The survival rate of dental implants in our hospital was 92%, which is higher than those at other hospitals reported (81% to 86.3%) [
6,
9,
10,
11]. We left the 5 dental implants sleeping because they were covered by thick non-keratinized mucosa. Although dental implants were placed with the consideration of the relationship of the opposing teeth, we had difficulty performing prosthesis due to the condition of the peri-implant soft tissue.
Risk factors for loss of dental implants analyzed in 40 patients, including 4 patients at less than 2 years observation after placement of prostheses. In univariate analysis, implant site (maxilla/mandible), type of prosthesis (cantilever/others), and whether or not the patient received radiotherapy were identified as significant risk factors, but none of these factors were significant in multivariate analysis. Of the 9 lost dental implants, 8 dental implants were in the existing maxillary bone and 5 dental implants supported a cantilever prosthesis on a big defect of maxillary bone. The reason why no independent risk factors were identified in the multivariate analysis is that only a small number of implants were lost (9 in total out of 114 placements), and risk factors extracted in univariate analysis might be confounding. Reconstruction using vascularized flap after maxillectomy is not usually performed at our hospital, and maxillofacial prosthesis is used for treatment instead. When a maxillofacial prosthesis is retained by dental implants on remaining bone after a maxillectomy, the available bone volume and site for implant placement are limited. Then, the dental implants on the existing bone need to support a large cantilever maxillofacial prosthesis. Therefore, these dental implants may be lost due to overload.
Of the 3 patients who underwent radiotherapy before dental implants, 2 patients had lost dental implants. One of these 2 patients underwent radiotherapy after segmental mandibulectomy for cancer treatment. Then, the patient received 2 dental implant placements on both canine regions 2 years later. After one more year, the patient was suffered ORN, and 1 dental implant was removed by the additional segmental mandibulectomy for ORN treatment. This patient lost an implant in segmental mandibulectomy, but dental implant on the opposite side were stable. The other patient had chemoradiotherapy for a maxillary sinus carcinoma, and subsequently underwent subtotal maxillectomy due to ORN. Two dental implants were placed in the existing bone and seemed to be osteointegrated in the early period, but 2 implants lost after loading to support a cantilever maxillofacial prosthesis. Radiotherapy was performed after dental implants placement in 2 patients. The dental implant lost in one patient with upper gingival carcinoma, in whom cervical lymph node metastasis occurred after primary surgery and received radiotherapy on the neck. There are many reports of low survival rate of dental implant after radiotherapy [
12,
13,
14]. However, in this study, radiotherapy was not extracted as a poor prognostic factor in multivariate analysis. Because the patients who underwent or were likely to undergo radiotherapy were intended to be avoided for implant placement in this study, careful consideration is required for the effect of radiation on dental implants.
Hessling et al. reported differences in the survival rates of dental implants in existing and grafted bones. [
15], while Teoh et al. showed no differences between them [
16]. Our results also showed no significant difference, but further studies are needed.
There are some limitations in the study. Because this study is a retrospective observational study, patient background, clinical experience of oral and maxillofacial surgeons, bone conditions, types of dental implants and prosthesis on dental implants were not completely standardized. Thus, it might be difficult to extract risk factors on survival rate of dental implants in the selected patients. In this pilot study, some patients were observed for only a short period of time (6 months) and only a limited number of dental implants in a limited number of patients (114 dental implants, 43 patients) could be observed, which may reduce the statistical power of the study. Multicenter prospective studies should be conducted to examine the risk factors of implants for patients with extensive jaw defects after treatment for oral and maxillofacial diseases.
5. Conclusions
Only a limited number of the patients with extensive jaw defects after treatment for oral and maxillofacial diseases received dental implant treatments which were covered by Japanese public health insurance. Despite the complicated surgical conditions and limited option of prosthesis in these patients, good outcomes were achieved and the dental implant treatments improved their masticatory function.
Author Contributions
Conceptualization: W.K., T.H (Tomonori Hasegawa). and H.K.; Methodology: W.K., T.H (Tomonori Hasegawa). and H.K.; Investigation: R.S., T.H (Toshiki Hyodo)., Y.K (Yosuke Kunitomi)., Y.K (Yoshiaki Kitsukawa)., S.Y., M.T-O., and C.F.; Visualization: W.K., T.H (Tomonori Hasegawa). and Y.K(Yuske Komiyama).; Project administration: Y.K. and E.Y.; Supervision: T.W. and H.K., Writing—original draft: W.K. and T.H (Tomonori Hasegawa).; Writing—review and editing: W.K. and T.H (Tomonori Hasegawa) and H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects issued by the Japan Ministry of Health, Labor and Welfare and approved by the Ethics Committee of Dokkyo Medical University (Approval as No. R-72-13J on 21 May 2025).
Informed Consent Statement
This was an opt-out study and no patients or their representatives. requested exclusion from the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of this study; in the collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:.
References
- Zierden, K.; Koch, C.J.; Wöstmann, B.; Rehmann, P. Clinical Longevity of Obturators in Patients with Jaw Defects: a Retrospective Cohort Study. Clin. Oral Investig. 2024, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tanir, K. Ö. , Avag C, Tosun E, Akkocaoglu M. Evaluation of quality of life and masticatory function in patients treated with mandibular reconstruction followed by occlusal rehabilitation with dental implants: A preliminary report. J. Prosthodontics 2023, 32, 801–6. [Google Scholar]
- Laverty, D.P.; Kelly, R.; Addison, O. Survival of dental implants placed in autogenous bone grafts and bone flaps in head and neck oncology patients: a systematic review. Int. J. Implant. Dent. 2018, 4, 19. [Google Scholar] [CrossRef] [PubMed]
- Sarukawa S, Noguchi T, Nishino H, Sugawara Y. The Dental Implant Covered by Japanese Health Insurance in a Patient Viewpoint. Journal of Japanese Society of Oral Implantology 2014, 27, 4–9.
- Garrett, N.; Roumanas, E.D.; Blackwell, K.E.; Freymiller, E.; Abemayor, E.; Wong, W.K.; Gerratt, B.; Berke, G.; Beumer, J.; Kapur, K.K. Efficacy of conventional and implant-supported mandibular resection prostheses: Study overview and treatment outcomes. J. Prosthet. Dent. 2006, 96, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.; Burg, S.; Speth, U.; Cotter, M.-L.; Smeets, R.; Gosau, M.; König, D. Outcomes and influencing factors of dental implants in fibula, iliac crest, and scapula free flaps: a retrospective case–control study. Int. J. Implant. Dent. 2024, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jawad, S.; Barclay, C.; Whittaker, W.; Tickle, M.; Walsh, T. A pilot randomised controlled trial evaluating mini and conventional implant retained dentures on the function and quality of life of patients with an edentulous mandible. BMC Oral Heal. 2017, 17, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Fukumoto, C.; Oshima, R.; Sawatani, Y.; Shiraishi, R.; Hyodo, T.; Kamimura, R.; Hasegawa, T.; Komiyama, Y.; Izumi, S.; Fujita, A.; et al. Surveillance for Patients with Oral Squamous Cell Carcinoma after Complete Surgical Resection as Primary Treatment: A Single-Center Retrospective Cohort Study. Cancers 2021, 13, 5843. [Google Scholar] [CrossRef] [PubMed]
- Ko, H.-H.; Chou, C.-H.; Cheng, S.-J. The dental implant survival rate in 18 patients with post-operation revolutionary jaw reconstruction using free fibular flap, dental implants, and overdentures. J. Dent. Sci. 2024, 19, 1819–1826. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Van Dessel, J.; Shujaat, S.; Bila, M.; Sun, Y.; Politis, C.; Jacobs, R. Long-term survival of implant-based oral rehabilitation following maxillofacial reconstruction with vascularized bone flap. Int. J. Implant. Dent. 2022, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, D.; Suzuki, H.; Komori, T. A clinical study of 103 dental implants in oral cancer patients after jaw resection. J. Oral Maxillofac. Surgery, Med. Pathol. 2018, 30, 206–211. [Google Scholar] [CrossRef]
- Gorjizad, M.; Aryannejad, M.; Shahriari, A.; Khiavi, M.A.; Dashtkhaki, M.B.; Rigi, A.; Mohamadi, Z.; Asgari, P.; Shirazi, S.; Ziaei, S.; et al. Osteoradionecrosis Incidence and Dental Implant Survival in Irradiated Head and Neck Cancer Patients: A Systematic Review and Meta-Analysis. Spéc. Care Dent. 2025, 45, e70022. [Google Scholar] [CrossRef] [PubMed]
- Saini, R.S.; Vyas, R.; Mosaddad, S.A.; Heboyan, A. Efficacy of Oral Rehabilitation Techniques in Patients With Oral Cancer: A Systematic Review and Meta-Analysis. J. Surg. Oncol. 2024, 131, 1272–1283. [Google Scholar] [CrossRef] [PubMed]
- Lodders, J.N.; Leusink, F.K.; Ridwan-Pramana, A.; Winters, H.A.; Karagozoglu, K.H.; Dekker, H.; Forouzanfar, T.; Schulten, E.A. Long-term outcomes of implant-based dental rehabilitation in head and neck cancer patients after reconstruction with the free vascularized fibula flap. J. Cranio-Maxillofacial Surg. 2021, 49, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Hessling, S.A.; Wehrhan, F.; Schmitt, C.M.; Weber, M.; Schlittenbauer, T.; Scheer, M. Implant-Based Rehabilitation in Oncology Patients Can Be Performed With High Long-Term Success. J. Oral Maxillofac. Surg. 2015, 73, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Teoh, K.H.; Huryn, J.M.; Patel, S.; Halpern, J.; Tunick, S.; Wong, H.B.; Zlotolow, I.M. Implant prosthodontic rehabilitation of fibula free-flap reconstructed mandibles: a Memorial Sloan-Kettering Cancer Center review of prognostic factors and implant outcomes. . 2005, 20, 738–46. [Google Scholar] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).