Submitted:
15 July 2025
Posted:
17 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
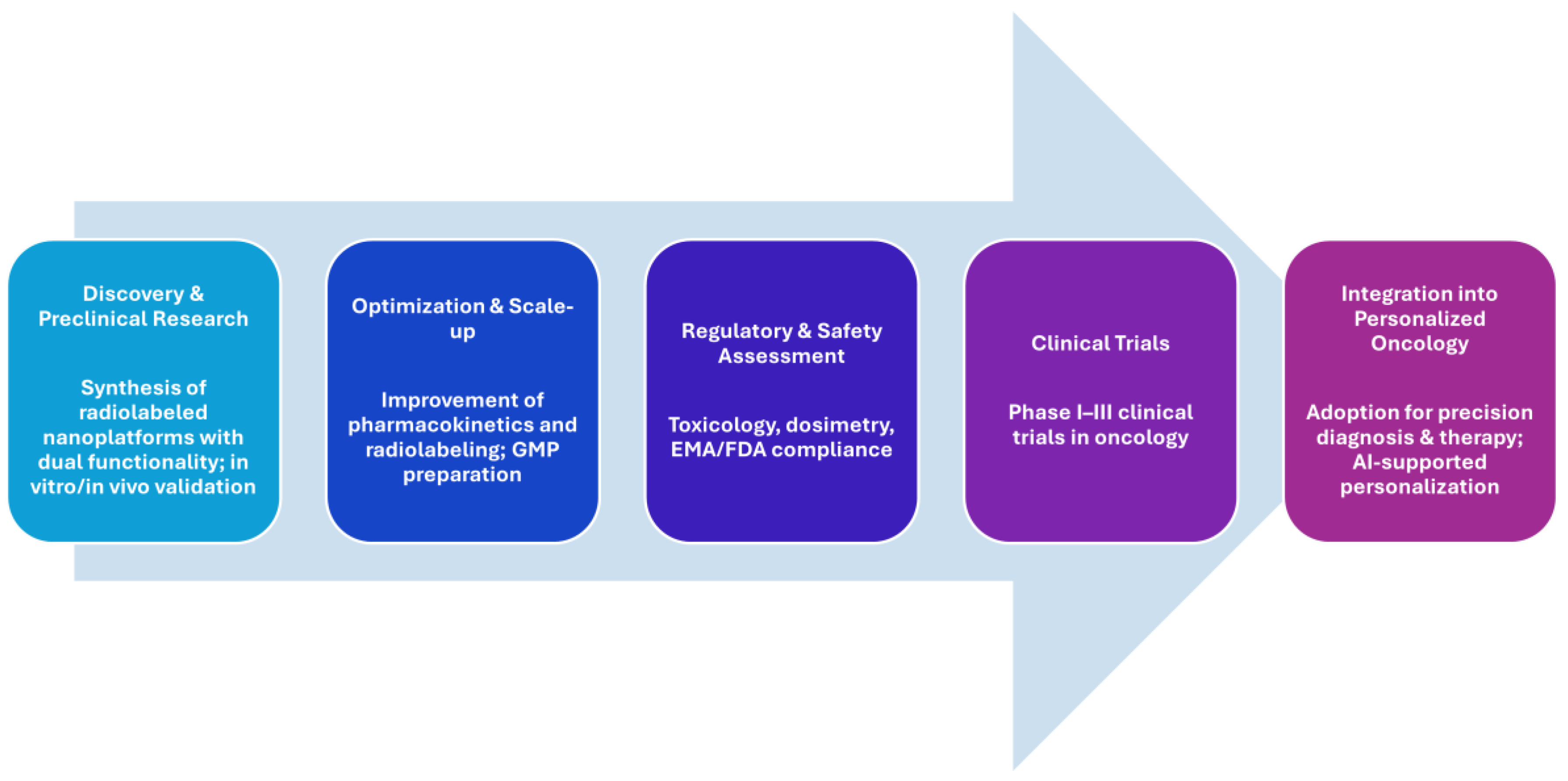
1.1. Background: From Monotherapy to Integrated Theranostics
1.2. The Convergence of Nanotechnology and Nuclear Medicine
1.3. Advances in Nanoplatform Design and Their Pharmacokinetic and Functional Benefits
1.4. Scope of This Review
2. Theranostic Principles and the Role of Nanoplatforms
2.1. Definition and Conceptual Evolution of Theranostics
2.2. Main categories of Nanoplatoforms used in nuclear theranostics
2.2.1. Organic nanoplatforms
2.2.2. Inorganic nanoplatforms
2.2.3. Hybrid and Multifunctional Nanostructures
2.3. Rationale for Combining Diagnostic and Therapeutic Modalities
3. Radioisotope Selection, Radiolabelling Strategies and Stability Concerns
3.1. Radioisotopes for Diagnostic
3.2. Radioisotopes for therapy
3.3. Radioisotopes pairing strategies
3.4. Radiolabeling Strategies
3.4.1. Regulatory Perspectives and GMP Considerations
- Radiochemical and pharmaceutical purity: Must be above 95%, verified by radio-Thin Layer Chromatography, High-Performance Liquid Chromatography, or gamma spectrometry.
- Sterility and apyrogenicity: Especially critical for parenteral formulations.
- Batch reproducibility: Challenging in nanoscale systems, requiring robust standard operating procedures (SOPs).
- Molar activity control: Particularly relevant for receptor-saturating theranostic agents.
- Documentation and traceability: Extensively detailed records for precursor synthesis, labeling conditions, and control quality testing are mandatory.
3.4.2. Final Remarks and Conclusion
Conflicts of Interest
Abbreviations
| ATMP | Advanced Therapy Medicinal Product |
| AuNPs | Gold nanoparticles |
| BFCAs | Bifunctional Chelating Agents |
| CT | Computed Tomography |
| DAPTA | D-Ala-peptide T-amide |
| DFO | Deferoxamine |
| DOTA | 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid |
| DOTAGA | 2-[1,4,7,10-Tetraazacyclododecane-4,7,10-tris(t-butyl acetate)]-pentanedioic acid-1t-butyl ester |
| DOX | Doxorubicin |
| DTPA | diethylenetriaminepentaacetic acid |
| EC | Electron Capture |
| EGFR | Epidermal Growth Factor Receptor |
| EMA | European Medicines Agency |
| EPR | Enhanced Permeability and Retention |
| FDA | Food and Drug Administration |
| Fn | Ferritin nanocages |
| FR | Folate Receptor |
| GLP | Good Laboratory Practice |
| GMP | Good Manufacturing Practices |
| GRPR | Gastrin-Releasing Peptide Receptor |
| HBED | N, N’-bis(2-hydroxybenzyl)ethylenediamine-N,N’-diacetic acid |
| HER2 | Human Epidermal Growth Factor Receptor 2 |
| IAEA | International Atomic Energy Agency |
| IMPs | investigational Medicinal Products |
| MOFs | Metal Organic Frameworks |
| MRI | Magnetic Resonance Imaging |
| MSNs | Mesoporous silica nanoparticles |
| NODAGA | 2-[4,7-bis(carboxymethyl)-1,4,7-triazonan-1-yl]-5-(2,5-dioxopyrrolidin-1-yl)oxy-5-oxopentanoic acid |
| NOTA | 1,4,7-Triazacyclononane-1,4,7-triacetic acid |
| NP | Nanoparticles |
| PAMAM | Poly(amidoamine) |
| PCL | Polycaprolactone |
| PEG | Polyethylene glycol |
| PET | Positron Emission Tomography |
| PLGA | poly(lactic-co-glycolic acid) |
| PNPs | Polymeric nanoparticles |
| PSMA | Prostate Specific Membrane Antigen |
| QDs | Quantum Dots |
| RES | Reticuloendothelial System |
| RGD | Arginylglycylaspartic acid |
| SPECT | Single Photon Emission Tomography |
| SPIONs | iron oxide nanoparticles |
| WHO | World Health Organization |
References
- James ML, Gambhir SS. A molecular imaging primer: modalities, imaging agents, and applications. Physiol Rev. 2012;92(2):897–965. [CrossRef]
- Kelkar SS, Reineke TM. Theranostics: combining imaging and therapy. Bioconjug Chem. 2011;22(10):1879–1903. [CrossRef]
- Yordanova A, Eppard E, Kürpig S, Bundschuh RA, Schönberger S, Gonzalez-Carmona M, Feldmann G, Ahmadzadehfar H, Essler M. Theranostics in nuclear medicine practice. Onco Targets Ther. 2017 Oct 3;10:4821-4828. [CrossRef]
- Dash A, Chakraborty S, Pillai MRA, Knapp FF. Peptide receptor radionuclide therapy: an overview. Cancer Biother Radiopharm. 2015;30(2):47–71. [CrossRef]
- Baum RP, Kulkarni HR. Theranostics: From Molecular Imaging Using Ga-68 Labeled Tracers and PET/CT to Personalized Radionuclide Therapy—The Bad Berka Experience. Theranostics. 2012;2(5):437–447. [CrossRef]
- Zhang, S., Wang, X., Gao, X., Chen, X., Li, L., Li, G., Liu, C., Miao, Y., Wang, R., & Hu, K. Radiopharmaceuticals and their applications in medicine. Signal transduction and targeted therapy, 2025; 10(1), 1. [CrossRef]
- Fani, M., André, J. P., & Maecke, H. R. 68Ga-PET: a powerful generator-based alternative to cyclotron-based PET radiopharmaceuticals. Contrast media & molecular imaging, 2008; 3(2), 67–77. [CrossRef]
- Hofman MS, Violet J, Hicks RJ, et al. [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19(6):825–833. [CrossRef]
- Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33(9):941–951. [CrossRef]
- Siafaka PI, Okur NÜ, Karantas ID, Okur ME, Gündoğdu EA. Current update on nanoplatforms as therapeutic and diagnostic tools: A review for the materials used as nanotheranostics and imaging modalities. Asian J Pharm Sci. 2021 Jan;16(1):24-46. [CrossRef]
- Lee DE, Koo H, Sun IC, et al. Multifunctional nanoparticles for multimodal imaging and theragnosis. Chem Soc Rev. 2012;41(7):2656–2672. [CrossRef]
- Hare JI, Lammers T, Ashford MB, Puri S, Storm G, Barry ST. Challenges and strategies in anti-cancer nanomedicine development: an industry perspective. Adv Drug Deliv Rev. 2017;108:25–38. [CrossRef]
- Lankoff, A.M.; Czerwińska, M.; Kruszewski, M. Advances in Nanotheranostic Systems for Concurrent Cancer Imaging and Therapy: An Overview of the Last 5 Years. Molecules 2024, 29, 5985. [CrossRef]
- Muthu MS, Leong DT, Mei L, Feng SS. Nanotheranostics—application and further development of nanomedicine strategies for advanced theranostics. Theranostics. 2014;4(6):660–677. [CrossRef]
- Albanese A, Tang PS, Chan WC. The effect of nanoparticle size, shape, and surface chemistry on biological systems. Annu Rev Biomed Eng. 2012;14:1–16. [CrossRef]
- Yu B, Tai HC, Xue W, Lee LJ, Lee RJ. Receptor-targeted nanocarriers for therapeutic delivery to cancer. Molecular Membrane Biology. 2010;(7):286-298. [CrossRef]
- Lankoff, A.; Czerwińska, M.; Kruszewski, M. Nanoparticle-Based Radioconjugates for Targeted Imaging and Therapy of Prostate Cancer. Molecules 2023, 28, 4122. [CrossRef]
- Perez-Medina C, Abdel-Atti D, Tang J, et al. Nanoreporter PET predicts the efficacy of anti-cancer nanotherapy. Nat Commun. 2016;7:11838. [CrossRef]
- Zhang C, Jugold M, Woenne EC, et al. Specific targeting of tumor angiogenesis by RGD-conjugated ultrasmall superparamagnetic iron oxide particles using a clinical 1.5-T magnetic resonance scanner. Cancer Res. 2007;67(4):1555–1562. [CrossRef]
- Kotb, S., Detappe, A., Lux, F., Appaix, F., Barbier, E. L., Tran, V. L., Plissonneau, M., Gehan, H., Lefranc, F., Rodriguez-Lafrasse, C., Verry, C., Berbeco, R., Tillement, O., & Sancey, L. Gadolinium-based nanoparticles and radiation therapy for multiple brain melanoma metastases: proof of concept before phase I trial. Theranostics. 2016;6(3):418–427. [CrossRef]
- Altai M, Membreno R, Cook B, Tolmachev V, Zeglis BM. Pretargeted imaging and therapy. J Nucl Med. 2017;58(10):1553–1559. [CrossRef]
- Boros, E., Gale, E. M., Caravan, P. MR imaging probes: design and applications. Dalton transactions. 2015, 44(11), 4804–4818. [CrossRef]
- van der Meel, R., Sulheim, E., Shi, Y., Kiessling, F., Mulder, W. J. M., & Lammers, T. Smart cancer nanomedicine. Nat Nanotechnol. 2019;14(11):1007–1017. [CrossRef]
- Xie, J., Lee, S., Chen, X. Nanoparticle-based theranostic agents. Advanced Drug Delivery Reviews, 2010; 62(11), 1064–1079. [CrossRef]
- Silberstein EB. Radioiodine: the classic theranostic agent. Seminars in nuclear medicine, 2012; 42(3), 164–170. [CrossRef]
- Kassis, AI., Korideck, H., Wang, K., Pospisil, P., Adelstein, S. J. Novel prodrugs for targeting diagnostic and therapeutic radionuclides to solid tumors. Molecules (Basel, Switzerland), 2008; 13(2), 391–404. [CrossRef]
- Srinivasarao, M., Galliford, C. V., Low, P. S. Principles in the design of ligand-targeted cancer therapeutics and imaging agents. Nature Reviews Drug Discovery, 2015; 14(3), 203–219. [CrossRef]
- Mura, S., Couvreur, P. Nanotheranostics for personalized medicine. Advanced Drug Delivery Reviews, 2012; 64(13), 1394–1416. [CrossRef]
- Lammers, T., Kiessling, F., Hennink, W. E., Storm, G. Drug targeting to tumors: Principles, pitfalls and (pre-)clinical progress. Journal of Controlled Release, 2012;161(2), 175–187. [CrossRef]
- Louie, A. Multimodality imaging probes: Design and challenges. Chemical Reviews, 2010; 110(5), 3146–3195. [CrossRef]
- Hernot, S., Klibanov, A. L. Microbubbles in ultrasound-triggered drug and gene delivery. Advanced Drug Delivery Reviews, 2008; 60(10), 1153–1166. [CrossRef]
- Peer, D., Karp, J. M., Hong, S., Farokhzad, O. C., Margalit, R.,Langer, R. Nanocarriers as an emerging platform for cancer therapy. Nature Nanotechnology, 2007; 2(12), 751–760. [CrossRef]
- Sercombe L, Veerati T, Moheimani F, Wu SY, Sood AK, Hua S. Advances and challenges of liposome assisted drug delivery. Front Pharmacol. 2015;6:286. [CrossRef]
- Zhang Y, Chan HF, Leong KW. Advanced materials and processing for drug delivery: the past and the future. Adv Drug Deliv Rev. 2013;65(1):104–120. [CrossRef]
- Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal Doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42(5):419–436. [CrossRef]
- Phillips WT, Goins B, Bao A. Radioactive liposomes. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2009;1(1):69–83. [CrossRef]
- Torchilin, V. P. Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov. 2014; 13(11), 813–827. [CrossRef]
- Franco MS, Gomes ER, Roque MC, Oliveira MC. Triggered Drug Release From Liposomes: Exploiting the Outer and Inner Tumor Environment. Front Oncol. 2021; 11:623760. [CrossRef]
- Konda SD, Aref M, Brechbiel M, Wiener EC. Development of a tumor-targeting MR contrast agent using the high-affinity folate receptor: work in progress. Invest Radiol. 2000;35(1):50–57. [CrossRef]
- Patri, A. K., Majoros, I. J., Baker, J. R. Dendritic polymer macromolecular carriers for drug delivery. Curr Opin Chem Biol. 2002; 6(4), 466–471. [CrossRef]
- Pijeira, M. S. O., Viltres, H., Kozempel, J., Sakmár, M., Vlk, M., İlem-Özdemir, D., Ekinci, M., Srinivasan, S., Rajabzadeh, A. R., Ricci-Junior, E., Alencar, L. M. R., Al Qahtani, M., & Santos-Oliveira, R. Radiolabeled nanomaterials for biomedical applications: radiopharmacy in the era of nanotechnology. EJNMMI radiopharmacy and chemistry, 2022; 7(1), 8. [CrossRef]
- Janjua, T. I., Cao, Y., Yu, C., & Popat, A. Clinical translation of silica nanoparticles. Nature reviews. Materials, 2021; 6(12), 1072–1074. [CrossRef]
- Jayakumar, R., Prabaharan, M., Nair, S. V., Tokura, S., Tamura, H., Selvamurugan, N. Novel chitin and chitosan nanofibers in biomedical applications. Biotechnol Adv., 2010; 28(1), 142–150. [CrossRef]
- Pérez-Campaña, C., Gómez-Vallejo, V., Puigivila, M., Martín, A., Calvo-Fernández, T., Moya, S. E., & Llop, J. Biodistribution of different sized nanoparticles assessed by positron emission tomography: A general strategy for direct activation of metal oxide particles. ACS Nano, 2013; 7(4), 3498–3505. [CrossRef]
- Guo J, Hong H, Chen G, Shi S, Zheng Q, Zhang Y, Theuer CP, Barnhart TE, Cai W, Gong S. Image-guided and tumor-targeted drug delivery with radiolabeled unimolecular micelles. Biomaterials. 2013 Nov;34(33):8323-8332. [CrossRef]
- Liu, Y., Yuan, H., Fales, A. M., Register, J. K., Vo-Dinh, T. Multifunctional gold nanostars for molecular imaging and cancer therapy. Frontiers in chemistry, 2015; 3, 51. [CrossRef]
- Michalet, X., Pinaud, F. F., Bentolila, L. A., Tsay, J. M., Doose, S., Li, J. J., Sundaresan, G., Wu, A. M., Gambhir, S. S., Weiss, S. Quantum dots for live cells, in vivo imaging, and diagnostics. Science (New York, N.Y.), 2005; 307(5709), 538–544. [CrossRef]
- Pellico J, Ruiz-Cabello J, Herranz F. Radiolabeled Iron Oxide Nanomaterials for Multimodal Nuclear Imaging and Positive Contrast Magnetic Resonance Imaging (MRI): A Review. ACS Applied Nano Materials 2023 6 (22), 20523-20538. [CrossRef]
- Salvanou EA, Kolokithas-Ntoukas A, Prokopiou D, Theodosiou M, Efthimiadou E, Koźmiński P, Xanthopoulos S, Avgoustakis K, Bouziotis P. 177Lu-Labeled Iron Oxide Nanoparticles Functionalized with Doxorubicin and Bevacizumab as Nanobrachytherapy Agents against Breast Cancer. Molecules. 2024;29(5):1030. [CrossRef]
- Zhao Y, Trewyn BG, Slowing II, Lin VSY. Mesoporous silica nanoparticle-based double drug delivery system for glucose-responsive controlled release of insulin and cyclic AMP. J Am Chem Soc. 2009;131(24):8398–8400. [CrossRef]
- Pang, B., Zhao, Y., Luehmann, H., Yang, X., Detering, L., You, M., Zhang, C., Zhang, L., Li, Z. Y., Ren, Q., Liu, Y., Xia, Y. 64Cu-Doped PdCu@Au Tripods: A Multifunctional Nanomaterial for Positron Emission Tomography and Image-Guided Photothermal Cancer Treatment. ACS nano, 2016; 10(3), 3121–3131. [CrossRef]
- Mendoza-Nava, H., Ferro-Flores, G., Ramírez, F. M., Ocampo-García, B., Santos-Cuevas, C., Azorín-Vega, E., Jiménez-Mancilla, N., Luna-Gutiérrez, M., Isaac-Olivé, K. Fluorescent, Plasmonic, and Radiotherapeutic Properties of the 177Lu-Dendrimer-AuNP-Folate-Bombesin Nanoprobe Located Inside Cancer Cells. Molecular imaging, 2017; 16, 1536012117704768. [CrossRef]
- Tian Q, HuJ, Zhu Y, Zou R, ChenZ, Yang S, Li R, Su Q, Han Y, Liu X. Sub-10 nm Fe3O4@Cu2–xS Core–Shell Nanoparticles for Dual-Modal Imaging and Photothermal Therapy. Journal of the American Chemical Society 2013 135 (23), 8571-8577. [CrossRef]
- Wu, Q., Hou, Y., Han, G., Liu, X., Tang, X., Li, H., Song, X., Zhang, G. Mixed shell mesoporous silica nanoparticles for controlled drug encapsulation and delivery. Nanomedicine (London, England), 2017; 12(22), 2699–2711. [CrossRef]
- Zichang Shi, Shan Qing, Zhumei Luo, Yiqin Liu, Jiachen Li, Thermal physical and magnetic properties of water-based yolk-shell Fe3O4@C nanofluids, Inorganic Chemistry Communications. 2023. 151: 110562. [CrossRef]
- Liang R, Li F, Chen X, Tan F, Lan T, Yang J, Liao J, Yang Y, Liu N. Multimodal Imaging-Guided Strategy for Developing 177Lu-Labeled Metal–Organic Framework Nanomedicine with Potential in Cancer Therapy. ACS Applied Materials & Interfaces 2023 15 (39), 45713-45724. [CrossRef]
- Krasnovskaya OO, Abramchuck D, Erofeev A, Gorelkin P, Kuznetsov A, Shemukhin A, Beloglazkina EK. Recent Advances in 64Cu/67Cu-Based Radiopharmaceuticals. Int J Mol Sci. 2023 May 23;24(11):9154. [CrossRef]
- Ferreira, C. A., Ni, D., Cai, W. Radiolabeled nanomaterials for imaging and therapy. Chem Soc Rev.,2020; 49(24), 8174–8204. [CrossRef]
- Lee, H., Shields, A. F., Siegel, B. A., Miller, K. D., Krop, I., Ma, C. X., LoRusso, P. M., Munster, P. N., Campbell, K., Gaddy, D. F., Leonard, S. C., Geretti, E., Blocker, S. J., Kirpotin, D. B., Moyo, V., Wickham, T. J., Hendriks, B. S. 64Cu-MM-302 Positron Emission Tomography Quantifies Variability of Enhanced Permeability and Retention of Nanoparticles in Relation to Treatment Response in Patients with Metastatic Breast Cancer. Clinical cancer research : an official journal of the American Association for Cancer Research, 2017; 23(15), 4190–4202. [CrossRef]
- Bertrand, N., Wu, J., Xu, X., Kamaly, N., Farokhzad, O. C. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Advanced Drug Delivery Reviews,2014; 66, 2–25. [CrossRef]
- Wang AZ, Langer R, Farokhzad OC. Nanoparticle delivery of cancer drugs. Annu Rev Med. 2012;63:185–198. [CrossRef]
- Topol, E. J. High-performance medicine: the convergence of human and artificial intelligence. Nature Medicine, 2019; 25(1), 44–56. [CrossRef]
- Cañellas CO, Salgueiro MJ, Zubillaga M. Radiofármacos: del laboratorio al paciente. 1° Ed. 2017. CJP Ediciones. Ciudad Autónoma de Buenos Aires, Argentina. URL: http://www.phd-online.com.ar/radiofarmacos/.
- Roy, I., Krishnan, S., Kabashin, A. V., Zavestovskaya, I. N., Prasad, P. N. Transforming Nuclear Medicine with Nanoradiopharmaceuticals. ACS nano, 2022; 16(4), 5036–5061. [CrossRef]
- Maecke H. R.. Radiolabeled peptides in nuclear oncology: influence of peptide structure and labeling strategy on pharmacology. Ernst Schering Research Foundation workshop, 2005 (49), 43–72. [CrossRef]
- Krutzek, F., Donat, C.K. , Stadlbauer, S. Chelator impact: investigating the pharmacokinetic behavior of copper-64 labeled PD-L1 radioligands. EJNMMI radiopharm. chem. 2024; 9, 14 . [CrossRef]
- Xu, J., Cai, F., Luo, Z., Fan, W., Dai, J., Cui, J., Li, S., Geng, C., Zheng, Q., Wang, Z., Tang, X. Design, synthesis, and preclinical evaluation of a novel bifunctional macrocyclic chelator for theranostics of cancers. European journal of nuclear medicine and molecular imaging, 2022; 49(8), 2618–2633. [CrossRef]
- von Witting, E., Garousi, J., Lindbo, S., Vorobyeva, A., Altai, M., Oroujeni, M., Mitran, B., Orlova, A., Hober, S., Tolmachev, V. Selection of the optimal macrocyclic chelators for labeling with 111In and 68Ga improves contrast of HER2 imaging using engineered scaffold protein ADAPT6. European journal of pharmaceutics and biopharmaceutics : official journal of Arbeitsgemeinschaft fur Pharmazeutische Verfahrenstechnik e.V, 2019; 140, 109–120. [CrossRef]
- Phua, V. J. X., Yang, C. T., Xia, B., Yan, S. X., Liu, J., Aw, S. E., He, T., Ng, D. C. E. Nanomaterial Probes for Nuclear Imaging. Nanomaterials. 2022;12(4):582. [CrossRef]
- Goel S, Chen F, Ehlerding EB, Cai W. Intrinsically radiolabeled nanoparticles: an emerging paradigm. Small. 2014: 10(19):3825-30. [CrossRef]
- Garcés, M.; Magnani, N.D.; Pecorelli, A.; Calabró, V.; Marchini, T.; Cáceres, L.; Pambianchi, E.; Galdoporpora, J.; Vico, T.; Salgueiro, J.; et al. Alterations in oxygen metabolism are associated to lung toxicity triggered by silver nanoparticles exposure. Free Radic. Biol. Med. 2021, 166, 324–336. [CrossRef]
- Garcés, M.; Marchini, T.; Cáceres, L.; Calabró, V.; Mebert, A.M.; Tuttolomondo, M.V.; Vico, T.; Vanasco, V.; Tesan, F.; Salgueiro, J.; et al. Oxidative metabolism in the cardiorespiratory system after an acute exposure to nickel-doped nanoparticles in mice. Toxicology 2021, 464, 153020. [CrossRef]
- Fuentes, P.; Bernabeu, E.; Bertera, F.; Garces, M.; Oppezzo, J.; Zubillaga, M.; Evelson, P.; Salgueiro, M.J.; Moretton, M.A.; Höcht, C.; et al. Dual strategy to improve the oral bioavailability of efavirenz employing nanomicelles and curcumin as a bio-enhancer. Int. J. Pharm. 2024, 651, 123734. [CrossRef]
- Galdopórpora, J.M.; Martinena, C.; Bernabeu, E.; Riedel, J.; Palmas, L.; Castangia, I.; Manca, M.L.; Garcés, M.; Lázaro-Martinez, J.; Salgueiro, M.J.; et al. Inhalable Mannosylated Rifampicin-Curcumin Co-Loaded Nanomicelles with Enhanced In Vitro Antimicrobial Efficacy for an Optimized Pulmonary Tuberculosis Therapy. Pharmaceutics 2022, 14, 959. [CrossRef]
- Grotz, E.; Tateosian, N.L.; Salgueiro, J.; Bernabeu, E.; Gonzalez, L.; Manca, M.L.; Amiano, N.O.; Valenti, D.; Manconi, M.; García, V.E.; et al. Pulmonary delivery of rifampicin-loaded soluplus micelles against Mycobacterium tuberculosis. J. Drug Deliv. Sci. Technol. 2019, 53, 101170. [CrossRef]
- Martín Giménez, V.M.; Moretton, M.A.; Chiappetta, D.A.; Salgueiro, M.J.; Fornés, M.W.; Manucha, W. Polymeric Nanomicelles Loaded with Anandamide and Their Renal Effects as a Therapeutic Alternative for Hypertension Treatment by Passive Targeting. Pharmaceutics 2023, 15, 176. [CrossRef]
- Chakravarty, R., Goel, S., Dash, A., Cai, W. Radiolabeled inorganic nanoparticles for positron emission tomography imaging of cancer: an overview. The quarterly journal of nuclear medicine and molecular imaging : official publication of the Italian Association of Nuclear Medicine (AIMN) [and] the International Association of Radiopharmacology (IAR), [and] Section of the Society of..2017; 61(2), 181–204. [CrossRef]
- Ni, D., Jiang D, Ehlerding EB, Huang P, Cai W. et al. Radiolabeling Silica-Based Nanoparticles via Coordination Chemistry: Basic Principles, Strategies, and Applications. Acc Chem Res. 2018;51(3):778–788. [CrossRef]
- Cheng, L., Shen, S., Jiang, D., Jin, Q., Ellison, P. A., Ehlerding, E. B., Goel, S., Song, G., Huang, P., Barnhart, T. E., Liu, Z., Cai, W. Chelator-Free Labeling of Metal Oxide Nanostructures with Zirconium-89 for Positron Emission Tomography Imaging. ACS nano, 2017; 11(12), 12193–12201. [CrossRef]
- Shaffer, T. M., Wall, M. A., Harmsen, S., Longo, V. A., Drain, C. M., Kircher, M. F., Grimm, J. Silica nanoparticles as substrates for chelator-free labeling of oxophilic radioisotopes. Nano letters, 2015; 15(2), 864–868. [CrossRef]
- Shi, S., Xu, C., Yang, K., Goel, S., Valdovinos, H. F., Luo, H., Ehlerding, E. B., England, C. G., Cheng, L., Chen, F., Nickles, R. J., Liu, Z., Cai, W. Chelator-Free Radiolabeling of Nanographene: Breaking the Stereotype of Chelation. Angewandte Chemie (International ed. in English), 2017; 56(11), 2889–2892. [CrossRef]
- Tian, L., Yi, X., Dong, Z., Xu, J., Liang, C., Chao, Y., Wang, Y., Yang, K., Liu, Z. Calcium Bisphosphonate Nanoparticles with Chelator-Free Radiolabeling to Deplete Tumor-Associated Macrophages for Enhanced Cancer Radioisotope Therapy. ACS nano, 2018; 12(11), 11541–11551. [CrossRef]
- Cui L, Xiong C, Zhou M, Shi S, Chow DS, Li C. Integrin αvβ3-Targeted [64Cu]CuS Nanoparticles for PET/CT Imaging and Photothermal Ablation Therapy. Bioconjug Chem. 2018;29(12):4062-4071. [CrossRef]
- Mavridi-Printezi, A.; Guernelli, M.; Menichetti, A.; Montalti, M. Bio-Applications of Multifunctional Melanin Nanoparticles: From Nanomedicine to Nanocosmetics. Nanomaterials 2020, 10, 2276. [CrossRef]
- Fan Q, Cheng K, Hu X, Ma X, Zhang R, Yang M, Lu X, Xing L, Huang W, Gambhir SS, Cheng Z. Transferring biomarker into molecular probe: melanin nanoparticle as a naturally active platform for multimodality imaging. J Am Chem Soc. 2014;136(43):15185-94. [CrossRef]
- Khorshidi A. Gold nanoparticles production using reactor and cyclotron based methods in assessment of (196,198)Au production yields by (197)Au neutron absorption for therapeutic purposes. Mater Sci Eng C Mater Biol Appl. 2016;68:449-454. [CrossRef]
- Zyuzin MV, Antuganov D, Tarakanchikova YV, Karpov TE, Mashel TV, Gerasimova EN, Peltek OO, Alexandre N, Bruyere S, Kondratenko YA, Muslimov AR, Timin AS. Radiolabeling Strategies of Micron- and Submicron-Sized Core-Shell Carriers for In Vivo Studies. ACS Appl Mater Interfaces. 2020;12(28):31137-31147. [CrossRef]
- Zhai D, Wang Y, Yu S, Zhou J, Song J, Hao S, Chen X. Design and evaluation of 32P-labeled hydroxyapatite nanoparticles for bone tumor therapy. Drug Deliv. 2023;30(1):2168791. [CrossRef]
- Ghosh S, Banerjee D, Guleria A, Chakravarty R. Production, purification and formulation of nanoradiopharmaceutical with 211At: An emerging candidate for targeted alpha therapy. Nucl Med Biol. 2024;138-139:108947. [CrossRef]
- Kukleva E, Suchánková P, Štamberg K, Vlk M, Šlouf M, Kozempel J. Surface protolytic property characterization of hydroxyapatite and titanium dioxide nanoparticles. RSC Adv. 2019 ;9(38):21989-21995. [CrossRef]
- Suchánková P, Kukleva E, Nykl E, Nykl P, Sakmár M, Vlk M, Kozempel J. Hydroxyapatite and Titanium Dioxide Nanoparticles: Radiolabelling and In Vitro Stability of Prospective Theranostic Nanocarriers for 223Ra and 99mTc. Nanomaterials (Basel). 2020;10(9):1632. [CrossRef]
- Suchánková P, Kukleva E, Štamberg K, Nykl P, Sakmár M, Vlk M, Kozempel J. Determination, Modeling and Evaluation of Kinetics of 223Ra Sorption on Hydroxyapatite and Titanium Dioxide Nanoparticles. Materials (Basel). 2020;13(8):1915. [CrossRef]
- Li RG, Napoli E, Jorstad IS, Bønsdorff TB, Juzeniene A, Bruland ØS, Larsen RH, Westrøm S. Calcium Carbonate Microparticles as Carriers of 224Ra: Impact of Specific Activity in Mice with Intraperitoneal Ovarian Cancer. Curr Radiopharm. 2021;14(2):145-153. [CrossRef]
- Korde A, Mikolajczak R, Kolenc P, et al. Practical considerations for navigating the regulatory landscape of non-clinical studies for clinical translation of radiopharmaceuticals. EJNMMI Radiopharm Chem. 2022;7(1):18. [CrossRef]
- Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use. Official Journal L 311, 28/11/2001 P. 0067-0128; OPOCE. Available from: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:32001L0083:EN:HTML.
- Directive 2013/59/Euratom: BSS for protection against the dangers arising from exposure to ionising radiationEUR-Lex-32013L0059-EN-EUR-Lex [Internet]. Available from: https://eur-lex.europa.eu/eli/dir/2013/59/oj.
- Anonymous. ICH M3 (R2) Non-clinical safety studies for the conduct of human clinical trials pharmaceuticals [Internet]. EMA/CPMP/ICH/286/1995, European Medicines Agency. 2009. Available from: https://www.ema.europa.eu/en/ich-m3-r2-non-clinical-safety-studies-conduct-human-clinical-trials-pharmaceuticals.
- Anonymous. ICH S9 Non-clinical evaluation for anticancer pharmaceuticals [Internet]. EMA/CHMP/ICH/646107/2008, European Medicines Agency. 2010. Available from: https://www.ema.europa.eu/en/ich-s9-nonclinical-evaluation-anticancer-pharmaceuticals.
- EMA. Radiopharmaceuticals [Internet]. European Medicines Agency. 2018. Available from: https://www.ema.europa.eu/en/radiopharmaceuticals.
- Annex 2 International Atomic Energy Agency and World Health Organization guideline on good manufacturing practices for radiopharmaceutical product [Internet]. WHO Technical Report Series, No. 1025, World Health Organization; 2020. Available from: https://cdn.who.int/media/docs/default-source/medicines/who-technical-report-series-who-expert-committee-on-specifications-for-pharmaceutical-preparations/trs1025-annex2.pdf?sfvrsn=7aceb0c1_6.
| Radioisotope | Decay mode | T1/2 | Energy of the main photon in keV (abundance %) | Diagnostic method |
|---|---|---|---|---|
| 99mTc | γ | 6 h | 140 (89) | SPECT |
| 131I | β- | 8 d | 364 (81) | SPECT |
| 123I | EC | 13.2 h | 159 (83) | SPECT |
| 67Ga | EC | 78.3 h | 93 (37); 185 (20); 300 (17); 395 (5) | SPECT |
| 111In | EC | 2.8 d | 171 (90); 245 (94) | SPECT |
| 11C | Β+ | 20 min | 511 | PET |
| 18F | β+ | 110 min | 511 | PET |
| 68Ga | β+ | 68 min | 511 | PET |
| Radioisotope | T1/2 | Emitted particle (Energy MeV) | Max range in soft tissue |
|---|---|---|---|
| 131I | 8 d | β- (0.606) | 2.3 mm |
| 223Ra | 11.43 d | 4α 2β- (5.64, 5.715) | <100 µm |
| 90Y | 64.1 h | β- (2.27) | 11.3 mm |
| 177Lu | 6.65 d | β- γ (0.497) | 1.8 mm |
| 188Re | 0.7 d | β- (2.12) | 10 mm |
| 225Ac | 10 d | 4α 2β- (6.83) | 47-85 μm |
| Diagnostic / Therapeutic Pair | Chelator | Nanotheragnostic Suitability | Clinical Application |
|---|---|---|---|
| [68Ga]/[177Lu]-DOTA-TATE | DOTA | High – stable coordination, mild labeling conditions | NETs (neuroendocrine tumors) |
| [68Ga]/[177Lu]-PSMA-617 | DOTA / DOTAGA | High – widely adapted to nanocarriers | Prostate cancer |
| [64Cu]/[67Cu]-Chelate | NOTA / SarAr | Moderate–High – versatile chelation, redox sensitivity requires stabilization | Experimental – solid tumors |
| [89Zr]/[90Y]-Chelate | DFO (for 89Zr), DOTA (for 90Y) | Moderate – DFO less stable long-term, 90Y well adapted | Antibody labeling / solid tumors |
| [123I]/[131I]-MIBG | Direct iodination | Low for nanoplatforms – instability in vivo without encapsulation | Neuroblastoma, pheochromocytoma |
| [68Ga]/[225Ac]-PSMA | DOTA / Macropa | High – α-emitter integration into nanoparticles for targeted delivery | mCRPC, α-therapy under investigation |
| Technological Innovation Level | Radionuclide Type | Regulatory Classification | Non-Clinical Requirements | GMP Considerations |
|---|---|---|---|---|
| Incremental (e.g., liposomes + 99mTc) | Conventional (99mTc, 111In, 131I) | IMP / Radiopharmaceutical | Reduced studies if vector known | Standard GMP processes apply |
| Intermediate (e.g., new polymers + 177Lu) | Emerging therapeutic (177Lu, 90Y) | Radiotherapeutic | Toxicology (S9), biodistribution, dosimetry | Process validation, radiochemical stability |
| Disruptive (e.g., hybrid NP + 225Ac) | High-risk a-emitter (225Ac, 213Bi, 223Ra) | Advanced Radiotherapeutic / ATMP | Full toxicology, genotoxicity, organ dosimetry | Custom GMP: shielding, purity, retention |
| ? Increasing Regulatory Complexity | Greater innovation and risk demand more stringent regulatory oversight and tailored GMP solutions. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





