Submitted:
11 July 2025
Posted:
11 July 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
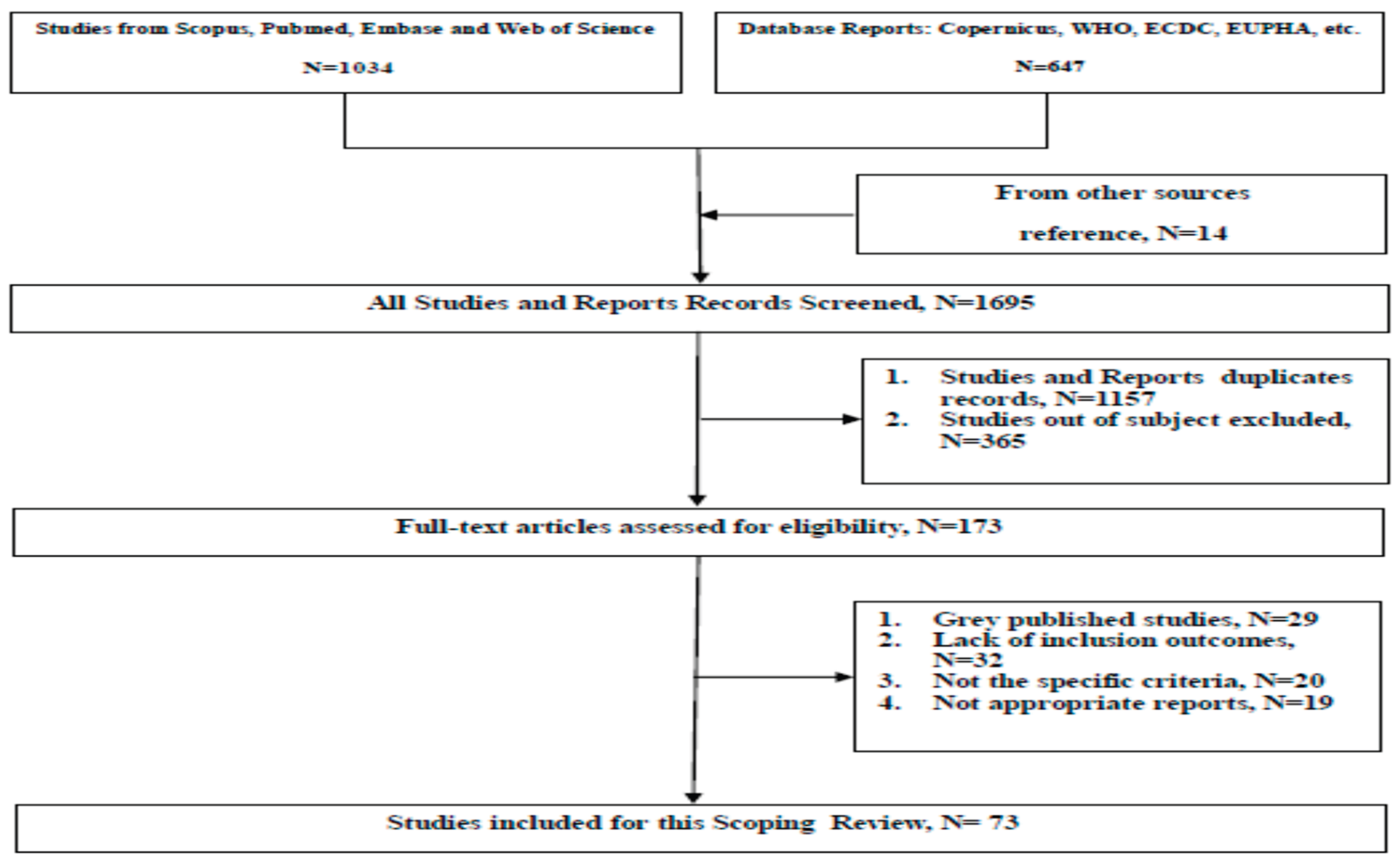
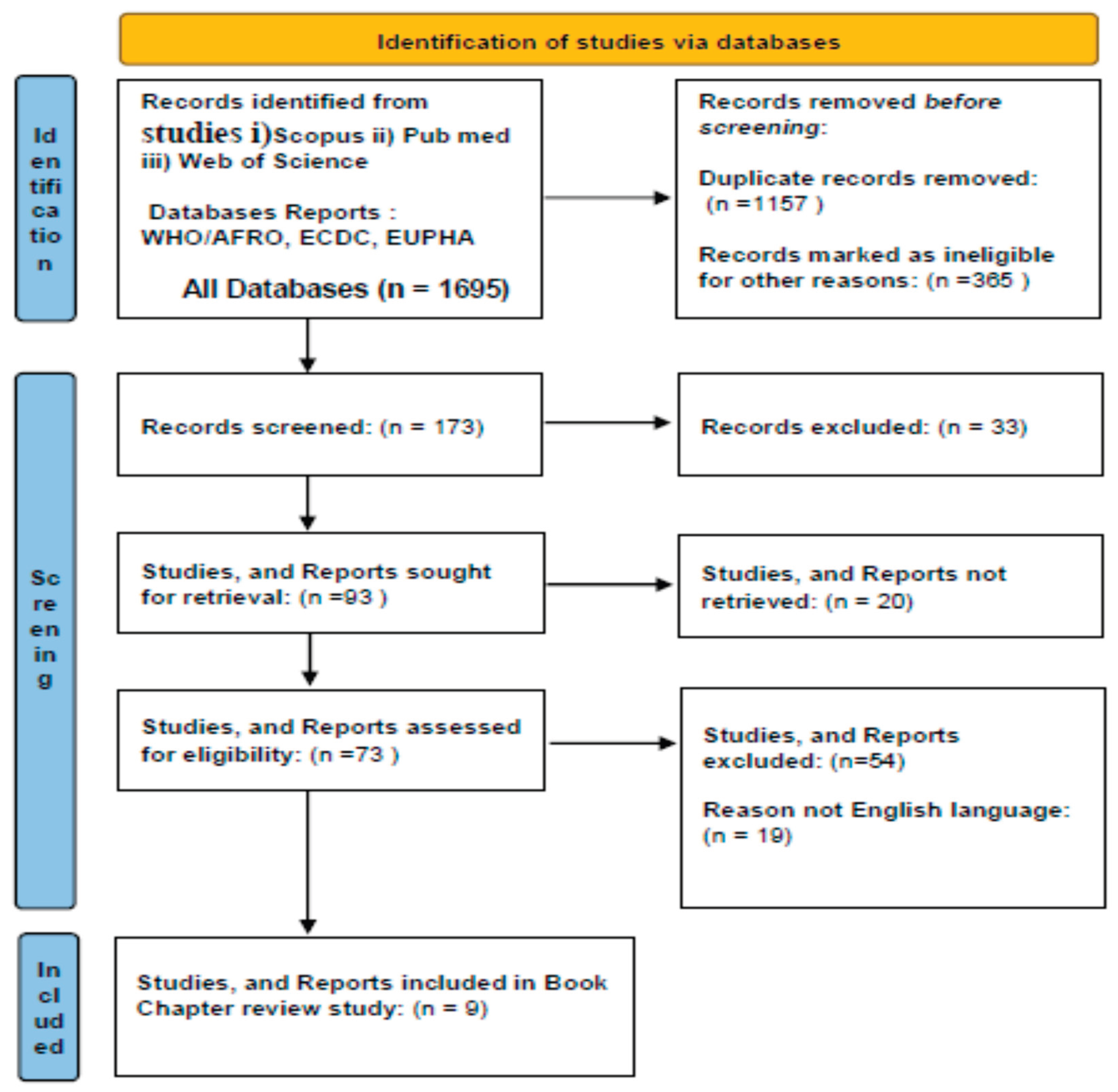
Methodology
Search Strategy
Inclusion and Exclusion Criteria
Methodological Constraints
Results of Meta-Analysis
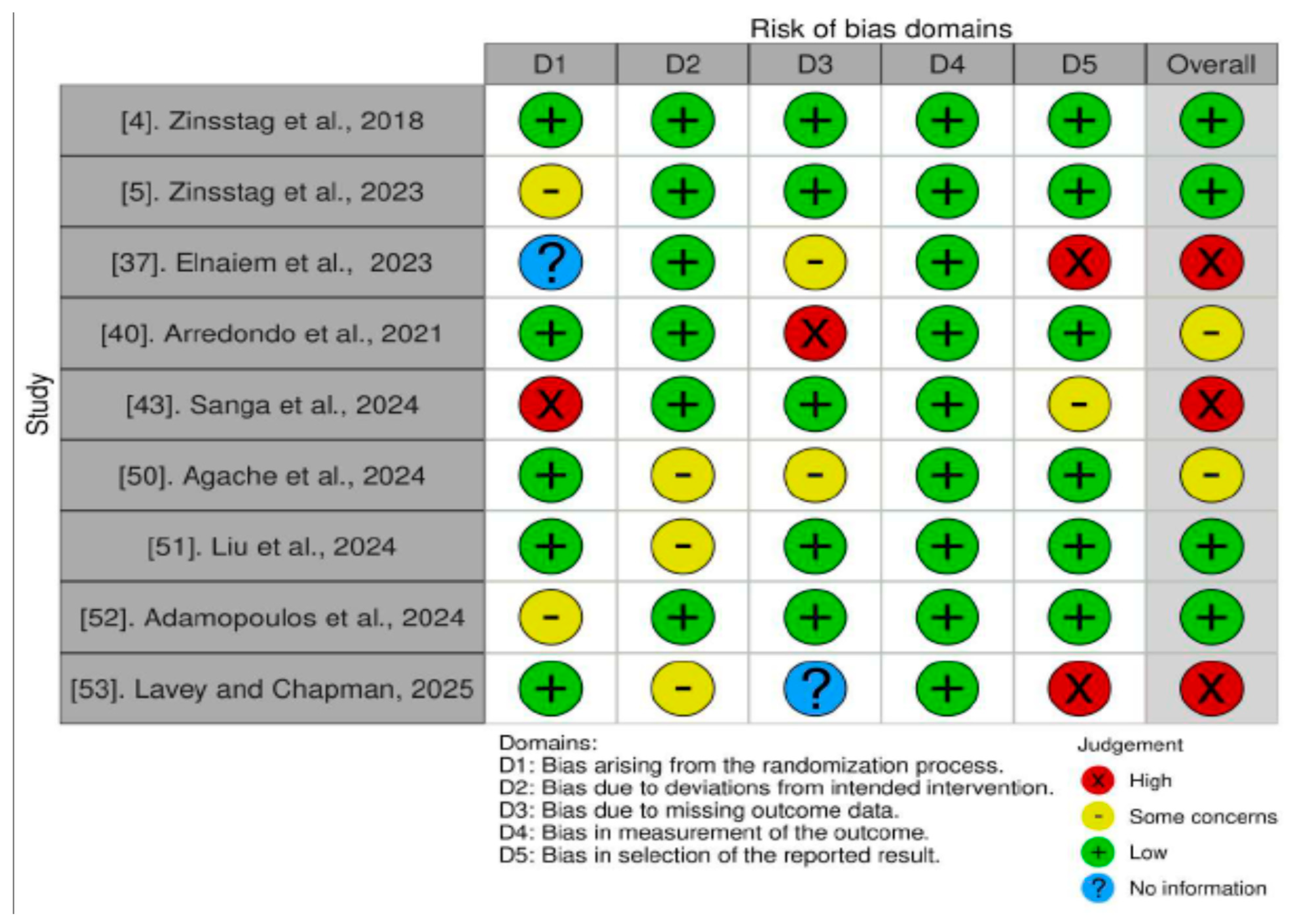
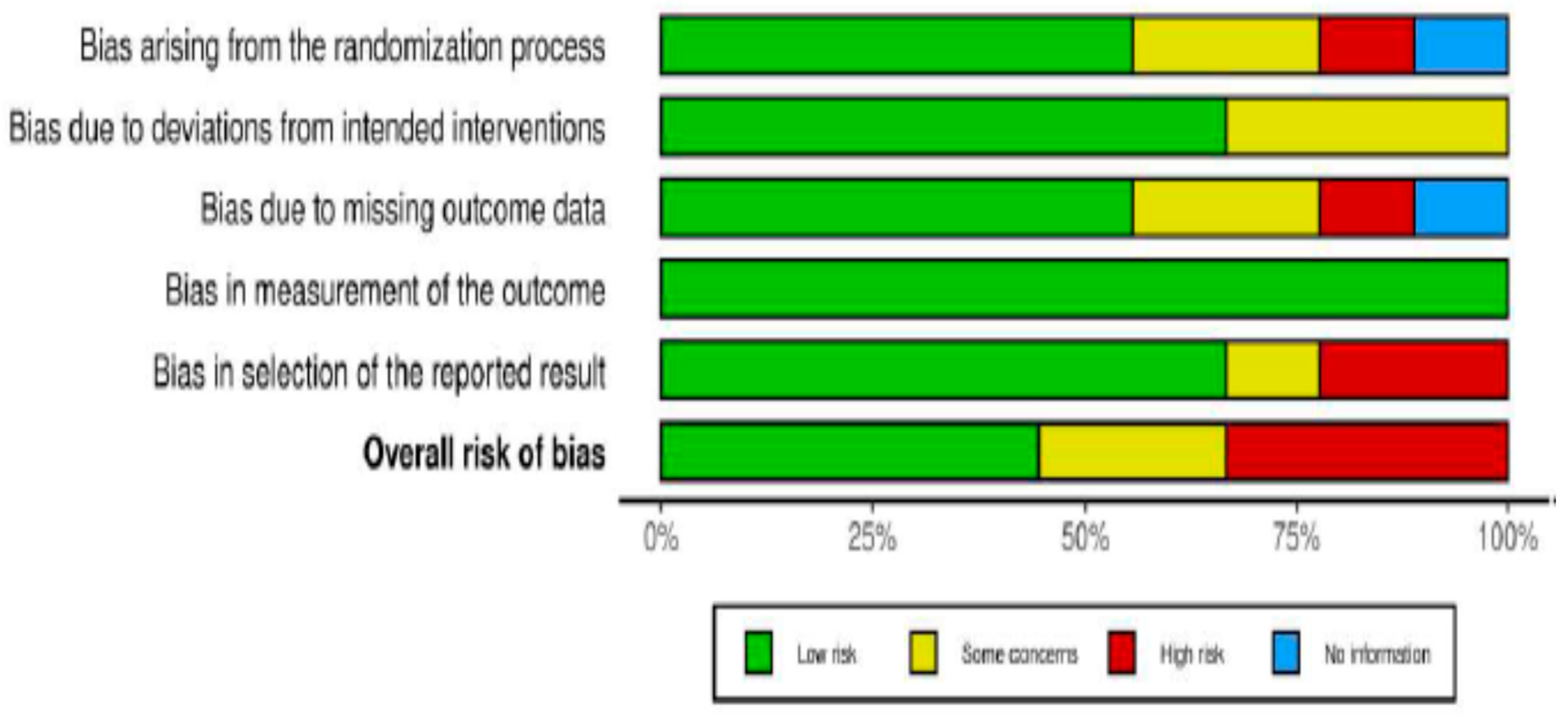
Quality Assessment of Reviews
Statistical Analysis
Challenges Data Gaps and Limitations
Results from Literature Review Studies
Impacts of Climate Change on Health
One Health Framework in Climate Change
Integration of Health Systems
Key Findings Results
Discussion
Policy Responses to Climate Change
Global Policies
National and International Strategies
Policy Recommendations and Future Research Directions
Limitations
Conclusions
Author Contributions
Funding
Ethics approval and consent to participate
Consent for publication
Data availability
Acknowledgements
Competing interests
Abbreviations
| AI | Artificial Intelligent |
| ECDC | European Centre for Disease Prevention and Control |
| EUPHA | European Public Health Association |
| E.U. | European Union |
| WHO | World Health Organization |
| PRISMA | Preferred Reporting Items for Systematic and Met-analysis |
| ML | Machine Learning |
References
- Ebi, Kristie L., et al. "Extreme weather and climate change: population health and health system implications." Annual review of public health 42.1 (2021): 293-315. [CrossRef]
- Morufu Olalekan Raimi, Tonye Vivien Odubo & Adedoyin Oluwatoyin Omidiji (2021) Creating the Healthiest Nation: Climate Change and Environmental Health Impacts in Nigeria: A Narrative Review. Scholink Sustainability in Environment. ISSN (2021).
- Abbass, Kashif, et al. "A review of the global climate change impacts, adaptation, and sustainable mitigation measures." Environmental science and pollution research 29.28 (2022): 42539-42559. [CrossRef]
- Zinsstag, A. Kaiser-Grolimund, K. Heitz-Tokpa, et al., "Advancing One human–animal–environment Health for global health security: what does the evidence say?" The Lancet, 2023. [CrossRef]
- Zinsstag, J., Crump, L., Schelling, E., Hattendorf, J., Osman Maidane, Y., Osman Ali, K., Muhummed, A., Adem Umer, A., Aliyi, F., Nooh, F., Ibrahim Abdikadir, M., Mohammed Ali, S., Hartinger, S., Mäusezahl, D., Berger Gonzalez de White, M., Cordon-Rosales, C., Alvarez Castillo, D., McCracken, J., Abakar, F., Cercamondi, C., Emmenegger, S., Maier, E., Karanja, S., Bolon, I., Ruiz de Castañeda, R., Bonfoh, B., Tschopp, R., Probst-Hensch, N., and Cissé, G. "Climate change and One Health." 2018. [CrossRef]
- Johnson, D., Parsons, M., and Fisher, K. "Engaging Indigenous perspectives on health, wellbeing and climate change. A new research agenda for holistic climate action in Aotearoa and beyond." Local Environment, 2021. [CrossRef]
- Timothy R., et al. "A conceptual framework for cross-border impacts of climate change." Global Environmental Change 69 (2021): 102307. [CrossRef]
- Arshad, Kashaf, et al. "Air pollution and climate change as grand challenges to sustainability." Science of The Total Environment (2024): 172370. [CrossRef]
- Bezgrebelna, Mariya, et al. "Climate change, weather, housing precarity, and homelessness: A systematic review of reviews." International Journal of Environmental Research and Public Health 18.11 (2021): 5812. [CrossRef]
- A. Iacovino and L. Randazzo, "Climate change and food security in the One Health perspective," BioLaw Journal-Rivista di BioDiritto, 2023.
- A.S. Bernstein, A.W. Ando, T. Loch-Temzelides, et al., "The costs and benefits of primary prevention of zoonotic pandemics," *Science*, 2022. [CrossRef]
- S. Singh, P. Sharma, N. Pal, D. K. Sarma, "Holistic one health surveillance framework: synergizing environmental, animal, and human determinants for enhanced infectious disease management," ACS Infectious Diseases, 2024. [CrossRef]
- J. Charlier, H. W. Barkema, P. Becher, et al., "Disease control tools to secure animal and public health in a densely populated world," Planetary Health, vol. 2022. thelancet.com. [CrossRef]
- L. Yajie, M. G. M. Johar, and A. I. Hajamydeen, "Poultry disease early detection methods using deep learning technology," *Indonesian Journal of …*, 2023. [CrossRef]
- C. Yenew, G. M. Bayeh, A. A. Gebeyehu, A. S. Enawgaw, et al., "Scoping review on assessing climate-sensitive health risks," BMC Public Health, 2025. [CrossRef]
- U. Sesay and A. Osborne, "Building climate-resilient health systems in Sierra Leone: addressing the dual burden of infectious and climate-related diseases," Infectious Diseases of Poverty, 2025. [CrossRef]
- M. I. Kabir, D. M. Hossain, M. T. H. Shawon, M. M. A. Khan, "Understanding climate-sensitive diseases in Bangladesh using systematic review and government data repository," PloS One, vol. 2025. [CrossRef]
- T. Alcayna, I. Fletcher, R. Gibb, L. Tremblay, S. Funk, "Climate-sensitive disease outbreaks in the aftermath of extreme climatic events: A scoping review," One Earth, vol. 5, no. 2, pp. 123-135, 2022. [CrossRef]
- D. J. Moriah, "Climate Change and Its Effects on Environmental Health: Challenges and Solutions for Vulnerable Populations," Social Sciences, 2025.
- A. Dimitrova, A. Gershunov, M. C. Levy, et al., "Uncovering social and environmental factors that increase the burden of climate-sensitive diarrheal infections on children," Proceedings of the National Academy of Sciences, vol. 2023. [CrossRef]
- R. H. Tantia and S. Patil, "Evaluating Climate-Sensitive Diseases in Maharashtra and the Essential Role of Preventive Social Medicine in Their Control.," Frontiers in Health Informatics, 2024.
- M. M. Khine and U. Langkulsen, "The implications of climate change on health among vulnerable populations in South Africa: a systematic review," Journal of Environmental Research and Public Health, vol. 2023. [CrossRef]
- R. P. Moreira, F. B. B. de Oliveira, T. L. de Araujo, et al., "Health interventions for preventing climate-sensitive diseases: scoping Review," Journal of Urban, vol. 2022, Springer. [CrossRef]
- C. Q. Hoang, Q. P. H. Nguyen, T. P. H. Nguyen, H. T. Nguyen, et al., "Identification of climate-sensitive disease incidences in Vietnam: A longitudinal retrospective analysis of infectious disease rates between 2014 and 2022," Heliyon, 2025. [CrossRef]
- A. Rossati Global Warming and Its Health Impact. Int J Occup Environ Med. 2017;8(1):7-20.
- A. J. Rodriguez-Morales and A. E. Paniz-Mondolfi, "The constant threat of zoonotic and vector-borne emerging tropical diseases: living on the edge," Frontiers in Tropical Diseases, 2021. [CrossRef]
- B. Mubemba, M. M. Mburu, K. Changula, "… of vector-borne zoonotic pathogens in Zambia: A clarion call to scaling-up 'One Health' research in the wake of emerging and re-emerging infectious diseases," PLOS Neglected Tropical Diseases, vol. 2022. [CrossRef]
- W. Socha, M. Kwasnik, M. Larska, J. Rola, "Vector-borne viral diseases as a current threat for human and animal health—One Health perspective," Journal of Clinical …, vol. 2022. [CrossRef]
- S. P. Dash, P. Dipankar, and P. S. Burange, "Climate change: how it impacts the emergence, transmission, resistance and consequences of viral infections in animals and plants," Critical Reviews in..., vol. 2021, Taylor & Francis. [CrossRef]
- I. Secretariat, M. L. Gullino, R. Albajes, and I. Al-Jboory, "Scientific review of the impact of climate change on plant pests," 2021.
- J. M. Tiedje, M. A. Bruns, A. Casadevall, C. S. Criddle, et al., "Microbes and climate change: a research prospectus for the future," MBio, 2022. [CrossRef]
- I. Agache, V. Sampath, J. Aguilera, C. A. Akdis, M. Akdis, et al., "Climate change and global health: a call to more research and more action," Allergy, vol. 77, no. 1, pp. 123-134, 2022. [CrossRef]
- W. M. de Souza and S. C. Weaver, "Effects of climate change and human activities on vector-borne diseases," Nature Reviews Microbiology, 2024. [CrossRef]
- M. K. Gislason, A. M. Kennedy, and S. M. Witham, "The interplay between social and ecological determinants of mental health for children and youth in the climate crisis," Journal of Environmental, vol. 2021. [CrossRef]
- L. Berrang-Ford, A. J. Sietsma, M. Callaghan, et al., "Systematic mapping of global research on climate and health: a machine learning review," Planetary Health, 2021. [CrossRef]
- E. L. Lawrance and R. Thompson, "The impact of climate change on mental health and emotional wellbeing: a narrative review of current evidence, and its implications," *Review of Psychiatry*, vol. 2022, Taylor & Francis. [CrossRef]
- A. Elnaiem, O. Mohamed-Ahmed, A. Zumla, J. Mecaskey, "Global and regional governance of One Health and implications for global health security," The Lancet, 2023. [CrossRef]
- F. Sultana, "Climate change, COVID-19, and the co-production of injustices: A feminist reading of overlapping crises," Social & Cultural Geography, 2021. [CrossRef]
- K. Goniewicz, F. M. Burkle, and A. Khorram-Manesh, "Transforming global public health: climate collaboration, political challenges, and systemic change," Journal of Infection and Public Health, vol. 2024, Elsevier. [CrossRef]
- AMP Arredondo, S. Yasobant, W. Bruchhausen, et al., "Intersectoral collaboration shaping One Health in the policy agenda: A comparative analysis of Ghana and India," One Health, vol. 12, pp. 100201, 2021. [CrossRef]
- M. Birley and R. Bos, "10. Health impact assessment: a tool for intersectoral collaboration," Innovative strategies for vector control, 2021.
- A. S. Gousse-Lessard, P. Gachon, L. Lessard, et al., "Intersectoral approaches: The key to mitigating psychosocial and health consequences of disasters and systemic risks," in *… and Management: An …*, 2022. [CrossRef]
- V. T. Sanga, E. D. Karimuribo, and A. S. Hoza, "One Health in practice: Benefits and challenges of multisectoral coordination and collaboration in managing public health risks: A meta-analysis," Journal of One Health, 2024. [CrossRef]
- M. Amri, A. Chatur, and P. O'Campo, "Intersectoral and multisectoral approaches to health policy: an umbrella review protocol," Health Research Policy and Systems, 2022. [CrossRef]
- J. A. Roth and J. Galyon, "Food security: The ultimate one-health challenge," One Health, 2024. [CrossRef]
- A. Wijerathna-Yapa and R. Pathirana, "Sustainable agro-food systems for addressing climate change and food security," Agriculture, 2022. [CrossRef]
- J. C. Prata, J. P. da Costa, I. Lopes, A. L. Andrady, et al., "A One Health perspective of the impacts of microplastics on animal, human and environmental health," *Science of the Total Environment*, vol. 2021, Elsevier. [CrossRef]
- M. G. Muluneh, "Impact of climate change on biodiversity and food security: a global perspective—a review article," Agriculture & Food Security, 2021. [CrossRef]
- B. K. Singh, M. Delgado-Baquerizo, E. Egidi, et al., "Climate change impacts on plant pathogens, food security and paths forward," Nature Reviews, 2023. [CrossRef]
- I. Agache, M. L. Hernandez, J. M. Radbel, H. Renz, "An overview of climate changes and its effects on health–from mechanisms to One Health," The Journal of Allergy, 2024. [CrossRef]
- J. S. Liu, X. C. Li, Q. Y. Zhang, L. F. Han, S. Xia, K. Kassegne, "China's application of the One Health approach in addressing public health threats at the human-animal-environment interface: Advances and challenges," One Health, vol. 2023, Elsevier. [CrossRef]
- Adamopoulos, I.; Frantzana, A.; Syrou, N. Climate Crises Associated with Epidemiological, Environmental, and Ecosystem Effects of a Storm: Flooding, Landslides, and Damage to Urban and Rural Areas (Extreme Weather Events of Storm Daniel in Thessaly, Greece). Med. Sci. Forum 2024, 25, 7.
- WG Lavey and HJ Chapman, "Present and Future Climate Change Crisis–One Health Challenges and Solutions," Global One Health and Infectious Diseases, 2025.
- T. S. Lu, J. Olsen, and P. L. Kinney, "Climate change and temperature-related mortality: implications for health-related climate policy," Biomedical and Environmental Sciences, 2021. [CrossRef]
- M. Dellar, G. Geerling, K. Kok, P. van Bodegom, "Creating the Dutch One Health Shared Socio-economic Pathways (SSPs), Regional Environmental Change, 2024. [CrossRef]
- E. W. Ansah, M. Amoadu, P. Obeng, and J. O. Sarfo, "Health systems response to climate change adaptation: a scoping review of global evidence," BMC public health, 2024. [CrossRef]
- A. D. Hoeben, I. M. Otto, and M. F. Chersich, "Integrating public health in European climate change adaptation policy and planning," Climate Policy, 2023. [CrossRef]
- E. Such, K. Smith, H. B. Woods, and others, "Governance of intersectoral collaborations for population health and to reduce health inequalities in high-income countries: a complexity-informed systematic review," *Journal of Health Policy*, vol. 2022. [CrossRef]
- S. J. Kobrin, "Managing political risk assessment: Strategic response to environmental change," 2022.
- Y. Sun, Y. Zou, J. Jiang, and Y. Yang, "Climate change risks and financial performance of the electric power sector: Evidence from listed companies in China," Climate Risk Management, 2023. [CrossRef]
- L. Berrang-Ford, A. R. Siders, A. Lesnikowski, et al., "A systematic global stocktake of evidence on human adaptation to climate change," *Nature Climate Change*, vol. 11, no. 11, pp. 1-11, 2021. [CrossRef]
- F. Ma, J. Cao, Y. Wang, S. A. Vigne et al., "Dissecting climate change risk and financial market instability: Implications for ecological risk management," Risk Analysis, 2025. [CrossRef]
- F. S. Khatibi, A. Dedekorkut-Howes, M. Howes, et al., "Can public awareness, knowledge and engagement improve climate change adaptation policies?" Discover, vol. 2021, Springer. [CrossRef]
- A. Raihan, "A review of the global climate change impacts, adaptation strategies, and mitigation options in the socio-economic and environmental sectors," Journal of Environmental Science and Economics, 2023. [CrossRef]
- O. Renn, M. Laubichler, K. Lucas, and W. Kröger, "Systemic risks from different perspectives," in *… analysis*, 2022. [CrossRef]
- P. Antwi-Agyei and L. C. Stringer, "Improving the effectiveness of agricultural extension services in supporting farmers to adapt to climate change: Insights from northeastern Ghana," Climate Risk Management, 2021. [CrossRef]
- Adamopoulos, I.; Frantzana, A.; Adamopoulou, J.; Syrou, N. Climate Change and Adverse Public Health Impacts on Human Health and Water Resources. Environ. Sci. Proc. 2023, 26, 178. [Google Scholar]
- Adamopoulos, I.; Valamontes, A.; Tsirkas, P.; Dounias, G. Predicting Workplace Hazard, Stress and Burnout Among Public Health Inspectors: An AI-Driven Analysis in the Context of Climate Change. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Adamopoulos, I.; Syrou, N.; Mpourazanis, G.; Constantinidis, T.C.; Dounias, G. The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene. Med. Sci. Forum 2025, 33, 2. [Google Scholar] [CrossRef]
- Ioannis Adamopoulos et al. “The Impact of PFAS on the Public Health and Safety of Future Food Supply in Europe: Challenges and AI-Driven Solutions”. In: European Journal of Sustainable Development Research (2025). [CrossRef]
- Adamopoulos, I.; Syrou, N.; Vito, D. Climate Change Risks and Impacts on Public Health Correlated with Air Pollution—African Dust in South Europe. Med. Sci. Forum 2025, 33, 1. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Syrou, N. Climate Change, Air Pollution, African Dust Impacts on Public Health and Sustainability in Europe. Eur. J. Public Health 2024, 34, ckae144.1374. [Google Scholar] [CrossRef]
- Adamopoulos, I.P.; Syrou, N.F.; Mijwil, M.; Thapa, P.; Ali, G.; Dávid, L.D. Quality of indoor air in educational institutions and adverse public health in Europe: A scoping review. Electron. J. Gen. Med. 2025, 22, em632. [Google Scholar] [CrossRef] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [CrossRef]
- McGuinness, LA, Higgins, JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2020; 1- 7. [CrossRef]
| Author | Type of study | Sample | Treatment conditions | Main findings | Total number of cases investigated | Follow up | Limitations | |
|---|---|---|---|---|---|---|---|---|
| 1 | Shanga et al. 2024 | Meta-analysis | 157 | OHA | 69.6% it is a beneficial to adopt OHA to enhance early detection and response to outbreaks and other health threats | Not mentioned | Not mentioned | Inadequate coordination and funding |
| 2 | Adamopoulos et al 2024 | Review | 25.000 | Not mentioned | Climate crisis and disasters can have serious repercussions for public health | 12.000 | Not mentioned | Not mentioned |
| 3 | Agache et al. 2024 | Review | 4.4% of GHG emissions | Not mentioned | The evidence on the impact of climate change on health should inform the management plan for allergic diseases by inclusion of risk evaluation and of adaptation and mitigation measures tailored to the type of environmental stressor by shared decision-making with the patient | Not mentioned | Not mentioned | Numerous climate policies have failed to stop climate change |
| 4 | Jing-Shu Liu et al. 2023 | Retrospective study | 596 | ELISA, biological therapy | The prevalence of EGPA in the SA population was 3.9% in cohort study | 23 | 10 years | Cost and patient’s preferences for biological therapy |
| 5 | Jing-Shu Liu et al. 2023 | Review | 56.34 | SPO model | China ranks highest in food security (scores 72.56 and ranks 6th), and lowest in climate change (48.74, 11th) | Not mentioned | Not mentioned | Challenges in translating policies into practical measures |
| 6 | Zinsstag et al. 2023 | Review | Not mentioned | IHR monitoring and evaluation framework and OIE performance of veterinary services pathway | The FAO, OIE and WHO currently play pivotal roles in stimulating OHO at the national and regional levels but will need increased support and allies to both strengthen current activities as well as address a wider set of health hazards across the Socio Ecological System | Not mentioned | Not mentioned | Not mentioned |
| 7 | Elnaiem et al. 2023 | Review | Not mentioned | Not mentioned | Financing mechanisms that predominantly focus on response to crises, and the chronic underinvestment for epidemic and emergency prevention, mitigation, and preparedness activities | East Africa | Not mentioned | Not mentioned |
| 8 | Arredondo et al. 2021 | Comparative analysis | Not mentioned | Not mentioned | The management of the impact of flood and droughts on health provided a good example of intersectoral collaborations achieved by sectoral integration | Ghana and India | Not mentioned | The onset of the global epidemic of AI became one among other successful cases of ISC for OH in most parts of the globe |
| 9 | Zinsstag 2018 et al. | Mini-Review | Not mentioned | PEP against rabies | Not mentioned | Not mentioned | Not mentioned | Failure of communication of public, animal health surveillance systems |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





