1. Introduction
Delirium is a complex clinical syndrome which often presents as an acute onset confusion along with sudden fluctuating disturbance of intellectual and mental function. It is commonly associated with hallucinations or inattention. [
1]. Delirium can usually be treated by addressing the underlying medical or surgical cause. It differs from dementia due to its nature of more acute onset, fluctuating presentation and usually resolves upon treatment of the underlying precipitating factors whereas Dementia is more progressive in nature and involving more than two cognitive domains over more than six-months. [
2]
Delirium is comparatively more common in the older people and can be a sole presentation of serious medical conditions like acute myocardial infarction or sepsis [
3]. A recent systematic review showed that delirium is present in approximately 50% of hospitalized older patients (aged 65 years or older) [
4]. Moreover, the risk of developing delirium in the elderly can range from 15-20% after planned surgeries which could increase to over half of the patients undergoing more complex surgical procedures including traumatic femoral fracture or cardiac-thoracic surgeries [
5,
6]. Delirium diagnosis in the older people is associated with higher risk of adverse clinical outcomes [
7]. Delirium has been associated with poor mortality outcomes which have not improved over the last thirty years, whereas in comparison other medical conditions have shown consistent improvement in mortality over the years [
8].
In addition to the worse hospital outcomes including longer length of hospital stays and recurrent hospital admissions, delirium has also been associated with worsening cognition and decline in functional state, which increases risk of developing dementia [
9,
10,
11]. Delirium not only increases morbidity burden for patients but also adds to family and care-giver stress. Additionally, it leads to increased pressures and financial costs on the healthcare system [
12].
Most of the existing literature and research highlights clinical outcomes in the delirium patients admitted to the high-dependency units (HDU) or intensive care units (ICU) [
13]. However, there is scarcity of data on the impact of delirium on causative relations or health-related outcomes in the older patients admitted to general medical wards or acute medical assessment units [
14,
15,
16].
The main purpose of this study was to evaluate the impact of delirium on clinical outcomes such as mortality, readmissions and length of hospital stay in the older patients (≥65 years) admitted to a local general hospital. The additional objective is to observe any findings which might predispose these patients to development of delirium.
2. Methods
2.1. Study Design
This was a retrospective observational cohort study based on analysis of hospital notes of patients older than 65 years admitted acutely to medical assessment unit (MAU) at Ysbyty Ystrad Fawr (YYF) Hospital. Short-term health outcomes were defined as the length of stay (LOS), in-hospital mortality, 30-day and 90 days all-cause mortality and 30-day readmission. Discharge date, mortality and readmission information were gathered from the clinical works station (CWS). CWS is a software which provides access to scanned hospital notes and other clinical information.
2.2. Setting
Medical assessment unit (MAU) at YYF Hospital is a critical component of the hospital’s acute medical services, designed to provide rapid and comprehensive assessment, diagnosis, and treatment for patients presenting with acute medical conditions. Patients are typically referred to the MAU by the general practitioners, paramedics, or other healthcare practitioners.
The existing coded data for all the patients above the age of 65 years admitted in the year 2023 was reviewed. All patients less than 65 years of age and unidentifiable patients were excluded. 100 consecutive patients with delirium and 100 consecutive patients without delirium were selected from this sample.
2.3. Data and Statistical Analysis
All the relevant data including information on screening for delirium, co-morbidities, clinical outcomes such as LOS care needs before admission and at discharge, mortality, and readmission, was collected retrospectively from the clerking proformas and electronically scanned medical notes on the clinical work station. The data was reviewed between 1st January 2024 and 31st December 2024. The selected sample was divided into two groups: patients with delirium and patients without delirium.
The 4 A’s test (4AT) is a short screening tool for delirium and cognitive impairment developed in the UK [
17] The 4AT is a simple and short (<2 min) delirium detection tool designed for easy and effective clinical use. It does not require special training. The 4AT is the most-validated delirium tool in the literature, with >27 diagnostic test accuracy studies involving >5000 patients. It is highly sensitive and specific. It is proven in routine care, with high completion rates, and delirium detection at expected clinical rates.
Delirium was defined on the basis of case notes recording of new confusion, increased drowsiness or agitation and a 4AT of 4 or more. Patients without delirium were defined as patients who were admitted for reasons other than the ones defined as delirium and whose 4AT was less than 4.
The index admission was defined as any one episode of admission until discharge or death. The two samples were compared for adverse outcomes including LOS. Mortality analyses were done for 30 and 90 days from the date of index admission. Readmission analyses were done for 30 days following the date of discharge from the index admission. All statistics were conducted using STATISTICA StatSoft data analysis software system version 9.1 (Statistica Inc., 2010).
Ethical approval was not required for this service evaluation, however all questions and forms required to carry out the study were sent to the Aneurin Bevan University Health Board Research and Development (ABUHB R & D) Department, to assess risks to patient identification and the Health Board. ABUHB R & D approved the study with no further need for ethical approval.
3. Results
The total number of patients assessed in MAU from 1/01/2023 to 31/12/2023 were 8206. Mean age of the patients was 65 years (range = 16 to 103 years) and 56% were females. Most patients (82.1%, n=6732) were assessed out from MAU without requiring an admission to the hospital bed.
The mean age of the study sample was 82.2±8.0 years. There was no significant difference in the number of male or female patients between the two groups. The average number of drugs that patients were prescribed at the time of admission were 9.8±4.3. There was no significant difference in the average number of drugs between patients with delirium (10.2±4.2) and patients without delirium (9.5±4.4). The average clinical frailty scale was 6.0±1.2. The CFS score was significantly higher in patients with delirium 6.2±1.2 compared to patients without delirium 5.7±1.2.
The detailed patient characteristics of all patients with or without delirium are shown in
Table 1.
One-quarter (25%, n=50) of total sample had known diagnosis of dementia. Only 14% (n=7) patients without delirium had a diagnosis of dementia. In comparison, most patients with delirium (86%, n=43) had dementia and this was significantly higher when compared to patients without delirium.
Most patients (86%, n=172) of the total sample were admitted from their own home. Only 7.5% (n=15) patients were admitted from care homes. Among the patients admitted from their own home, there was no statistical difference in the incidence of delirium. However, among patients admitted from care homes, the incidence of delirium was significantly higher (93%, n=14).
The reasons for acute admission are shown in
Table 2.
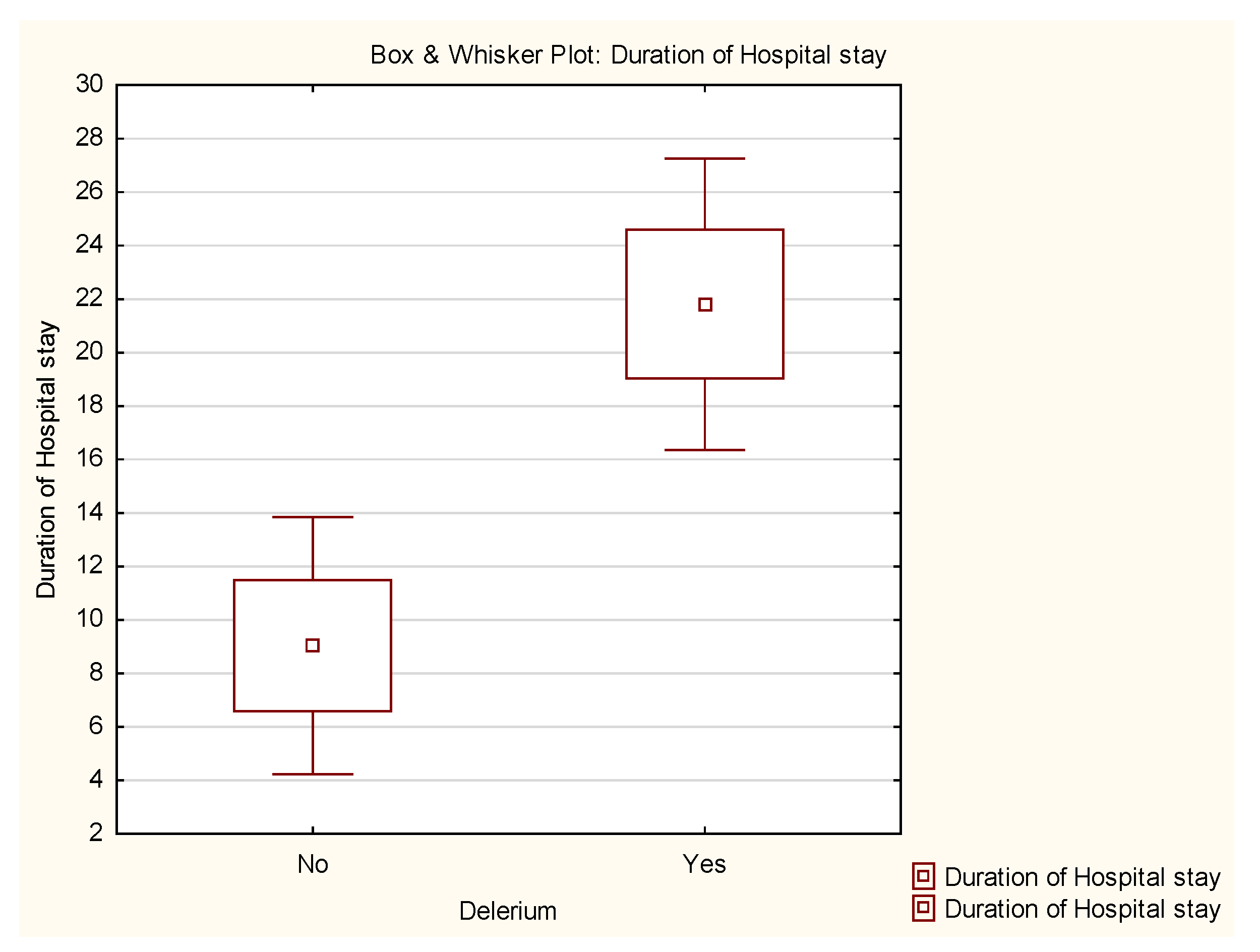
The mean LOS for the total sample was 18.5±31.3 days. Patients with delirium had a longer LOS (26.4±33.9days) as compared to patients without delirium (10.7±26.3days). The hospital stay was significantly higher in patients with delirium (p<0.001) as shown in the Box & Whisker plot (
Figure 1).
Overall, the inpatient mortality was 10% and majority (90%) who died had delirium. The inpatient mortality in patients with delirium was significantly higher (p<0.001) as compared to those without delirium. The clinical outcomes are shown in
Table 3.
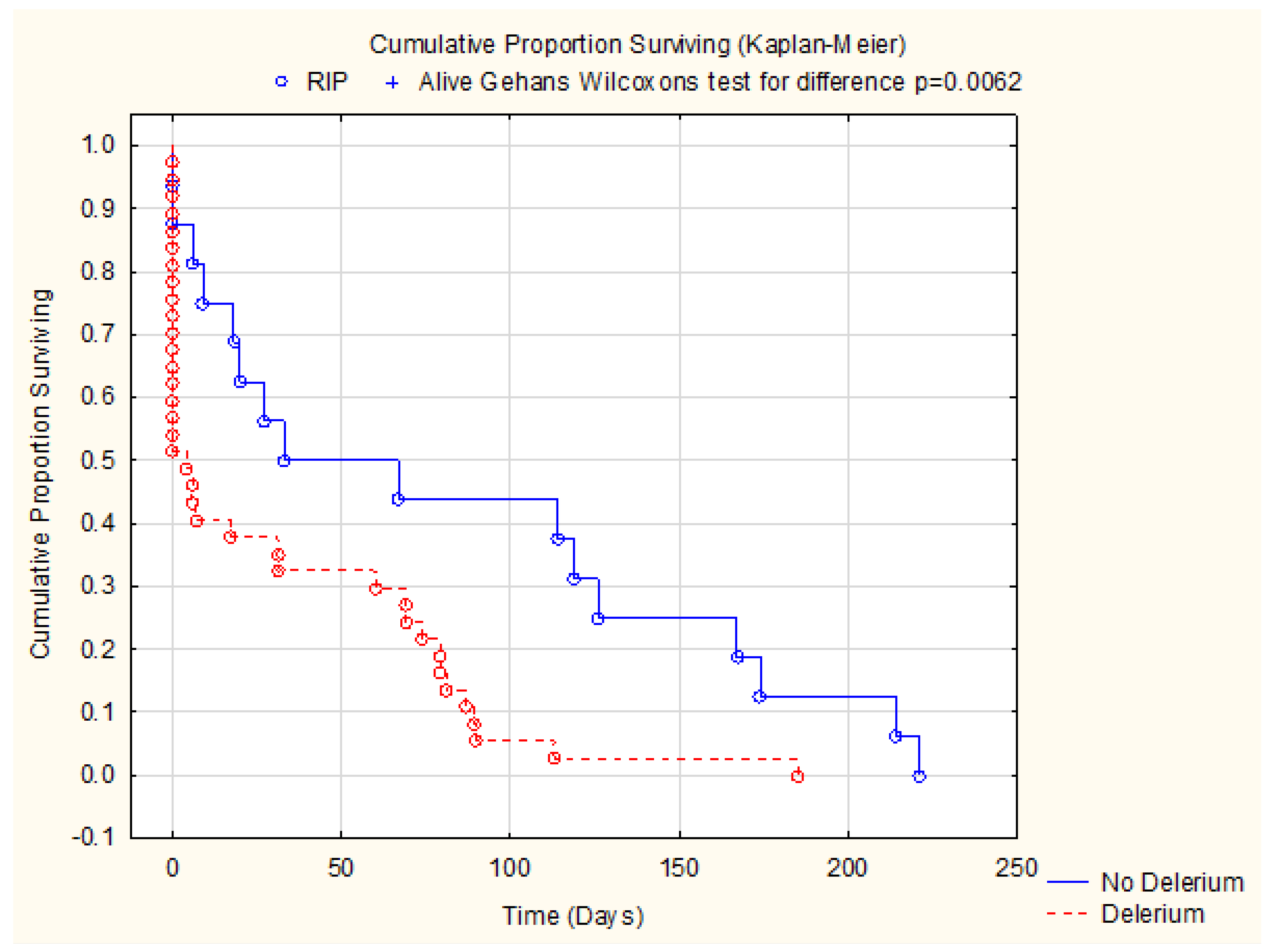
Patients with delirium also had a significantly higher 30-day mortality (23/30, 76.7%) as compared to patients without delirium (7/30, 23.3%). The mortality in patients with delirium remained significantly (35/46, 70.1%, p<0.001) higher at 90-day mortality as compared to patients without delirium (11/46, 23.9%). The patients with delirium have a significantly lower (p=0.0062) survival over time as demonstrated in the KM survival graphs (
Figure 2)
There was no significant difference in the 30-day readmission between the patients with delirium (15/35, 42.9%) and without delirium (20/35, (57.1%).
A sub-analysis was completed to appraise the impact of companionship on incidence of delirium. Over half of the patients (54%, n=108) of the total sample were living alone. There was no statistically significant association between living alone and incidence of delirium. (p=0.1)
Table 4
However, 32% (n=64) of whole study cohort were living with spouse/partner. Among those who did not develop delirium, nearly two-thirds (n=41, 64.1%) had a companion. In contrast, among patients who did develop delirium, only about one-third (n=23, 35.9%) had companionship. This difference was statistically significant (p<0.00015)
Table 4
4. Discussion
The prevalence of delirium in this study was 50% which was similar to other studies [
18]. Additionally, patients with delirium were significantly more likely to have longer hospital stays and higher rates of mortality than those without delirium.
In this study the average age of the patients was 82. There was no significant difference statistically between the age of the patients with delirium compared to the patients without delirium. This is consistent with many studies done prior to this study [
19].
We also found in this study that patients with delirium were more likely to have a higher CFS (6.2) compared to patients without delirium (5.7). This finding has been consistently demonstrated in previous studies [
20,
21]
In this study patients with dementia (n=50) were significantly more likely to develop delirium (n=43, 86%) as compared to patients without dementia (n=7, 14%). Dementia has been established as a risk factor for development of delirium [
22] and have been associated with poorer outcomes in the hospital setting [
23]. Many studies in the past have had similar findings [
24]
In our study we found that the average number of drugs patients were on was 9.8. There was no significant difference in the average number of drugs between patients with delirium (10.15±4.23) and patients without delirium (9.48±4.39). This was similar when compared to other studies [
25].
On sub-analysis of this retrospective study, we noted that a higher proportion who were living with a spouse (n=41, 64.1%) did not develop delirium. In contrast, companionship was observed in only one-third patients who developed delirium. (n=23, 35.9%) and this was significantly different (p<0.0015). There have been studies in the past looking into the impact of delirium on family caregivers [
26] but, we were unable to find any studies which looked at the impact of companionship on incidence of delirium.
In our study we also found that the incidence of delirium was significantly higher (93%, n=14) among patients admitted from care homes. This is slightly higher compared to similar studies which found incidence in the range of 10 to 60% [
27]. This may be due to several factors including the fact that the delirium screening tools used in these studies were different and the higher prevalence of dementia in our patient groups. We propose this to be investigated with higher powered study. However, this study emphasizes that delirium screening, diagnosis and early management as highlighted in the literature, particularly those living with dementia [
28].
This study has several weaknesses. It is a single centred study with a small number of patients and many other patient characteristics and impact of acute illness have not factored whilst calculating mortality. However, this study adds more knowledge and awareness that delirium is associated with poorer outcomes particularly longer hospital stay and higher mortality. This study aligns with recommended delirium screening for all patients admitted with acute medical illness as per National Audit of Dementia Care in General Hospitals in the UK [
29].
5. Conclusions
Older patients above the age of 65 admitted with medical assessment unit with delirium are likely to have as significantly higher mortality and length of hospital stay as compared to patients without delirium. This study supports that all acutely unless patients requiring admission to the general hospital should be actively screened for underlying delirium and delirium care plan should be commenced promptly. Patients who were living with a companion prior to admission had less incidence of delirium. Further studies with a larger sample size to further explore these finding.
Author Contributions
S Jayaram was responsible for the study concept; I Singh designed the methodology for the service evaluation, provided overall supervision and administration for the project. N Hlaing, S K Muthukrishnan and A Anwar collected all patient related data. I Singh completed data review for all corrections. Chris Edwards completed all data analysis and prepared graphs and tables. S Jayaram wrote the first draft and I Singh completed the critical appraisal for the manuscript. All authors contributed towards drafting and revising the paper and agree to be accountable for all aspects of the work.
Funding
No external funding was applied.
Institutional Review Board Statement
The Aneurin Bevan University Health Board’s Research and Development (ABUHB R & D) Department have reviewed this service evaluation application and it was agreed that your study does not pose any risk to the Health Board. Therefore, your service evaluation has been given a favourable opinion without need for any further ethical review was waived for this study. ABUHB R&D Reference Number: SE/1584/23
Data Availability Statement
Anonymized data will be made available on request.
Acknowledgments
The authors are grateful to all members of the Department of Geriatric Medicine, Ysbyty Ystrad Fawr for their continued support for research activities. The authors would especially like to thank all staff and therapists working in ABUHB. The authors would like to thank Jane Power for her administrative support. Authors are very grateful to Research and Development, Aneurin Bevan University Health Board for their support and guidance.
Conflicts of Interest
The authors report no other conflicts in this work.
References
- Chin YC, Koh GC, Tay YK, Tan CH, Merchant RA. Underdiagnosis of delirium on admission and prediction of patients who will develop delirium during their inpatient stay: a pilot study. Singapore Med J. 2016 Jan;57(1):18-21. [CrossRef] [PubMed] [PubMed Central]
- Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009 Apr;5(4):210-20. [CrossRef] [PubMed] [PubMed Central]
- Francis J, Kapoor WN. Delirium in hospitalized elderly. J Gen Intern Med. 1990 Jan-Feb;5(1):65-79. [CrossRef] [PubMed]
- Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014 Mar 8;383(9920):911-22. [CrossRef] [PubMed] [PubMed Central]
- Gleason LJ, Schmitt EM, Kosar CM, Tabloski P, Saczynski JS, Robinson T, Cooper Z, Rogers SO Jr, Jones RN, Marcantonio ER, Inouye SK. Effect of Delirium and Other Major Complications on Outcomes After Elective Surgery in Older Adults. JAMA Surg. 2015 Dec;150(12):1134-40. [CrossRef] [PubMed] [PubMed Central]
- Wang CG, Qin YF, Wan X, Song LC, Li ZJ, Li H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. 2018 Jul 27;13(1):186. [CrossRef] [PubMed] [PubMed Central]
- Fiest KM, Soo A, Hee Lee C, Niven DJ, Ely EW, Doig CJ, Stelfox HT. Long-Term Outcomes in ICU Patients with Delirium: A Population-based Cohort Study. Am J Respir Crit Care Med. 2021 Aug 15;204(4):412-420. [CrossRef] [PubMed] [PubMed Central]
- Aung Thein MZ, Pereira JV, Nitchingham A, Caplan GA. A call to action for delirium research: Meta-analysis and regression of delirium associated mortality. BMC Geriatr. 2020 Sep 7;20(1):325. [CrossRef] [PubMed] [PubMed Central]
- Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006 Jul;35(4):350-64. [CrossRef] [PubMed]
- Andrew MK, Freter SH, Rockwood K. Incomplete functional recovery after delirium in elderly people: a prospective cohort study. BMC Geriatr. 2005 Mar 17;5:5. [CrossRef] [PubMed] [PubMed Central]
- Rockwood K, Cosway S, Carver D, Jarrett P, Stadnyk K, Fisk J. The risk of dementia and death after delirium. Age Ageing. 1999 Oct;28(6):551-6. [CrossRef] [PubMed]
- Wass S, Webster PJ, Nair BR. Delirium in the elderly: a review. Oman Med J. 2008 Jul;23(3):150-7. PMCID: PMC3282320. [PubMed]
- Sahle BW, Pilcher D, Litton E, Ofori-Asenso R, Peter K, McFadyen J, Bucknall T. Association between frailty, delirium, and mortality in older critically ill patients: a binational registry study. Ann Intensive Care. 2022 Nov 17;12(1):108. [CrossRef] [PubMed] [PubMed Central]
- Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc. 1994 Aug;42(8):809-15. [CrossRef] [PubMed]
- Pereira FB, Lopes MA. Delirium in elderly inpatients admitted to clinical wards Prevalence and investigation of clinical conditions in a Brazilian sample. Dement Neuropsychol. 2018 Apr-Jun;12(2):152-156. [CrossRef] [PubMed] [PubMed Central]
- Díez-Manglano J, Palazón-Fraile C, Diez-Massó F, Martínez-Álvarez R, Del Corral-Beamonte E, Carreño-Borrego P, Pueyo-Tejedor P, Gomes-Martín J. Factors associated with onset of delirium among internal medicine inpatients in Spain. Nurs Res. 2013 Nov-Dec;62(6):445-9. [CrossRef] [PubMed]
- Arnold E, Finucane AM, Taylor S, Spiller JA, O’Rourke S, Spenceley J, Carduff E, Tieges Z, MacLullich AM. The 4AT, a rapid delirium detection tool for use in hospice inpatient units: Findings from a validation study. Palliat Med. 2024 May;38(5):535-545. [CrossRef] [PubMed] [PubMed Central]
- Guidance on Delirium: Delirium : diagnosis, prevention and management. London: National Institute for Health and Clinical Excellence, 2010. Available at: Overview | Delirium: prevention, diagnosis and management in hospital and long-term care | Guidance | NICE Accessed June 30, 2025.
- Kate Gibb, Anna Seeley, Terry Quinn, Najma Siddiqi, Susan Shenkin, Kenneth Rockwood, Daniel Davis, The consistent burden in published estimates of delirium occurrence in medical inpatients over four decades: a systematic review and meta-analysis study, Age and Ageing, Volume 49, Issue 3, May 2020, Pages 352–360. [CrossRef]
- Ticinesi A, Parise A, Delmonte D, Coppi C, Prati B, Cerundolo N, Guerra A, Nouvenne A, Meschi T. Factors associated with delirium in a real-world acute-care setting: analysis considering the interdependence of clinical variables with the frailty syndrome. Eur Geriatr Med. 2024 Apr;15(2):411-421. [CrossRef] [PubMed] [PubMed Central]
- Geriatric Medicine Research Collaborative. Increasing frailty is associated with higher prevalence and reduced recognition of delirium in older hospitalised inpatients: results of a multi-centre study. Eur Geriatr Med 14, 325–332 (2023). [CrossRef]
- Fong TG, Vasunilashorn SM, Libermann T, Marcantonio ER, Inouye SK. Delirium and Alzheimer disease: A proposed model for shared pathophysiology. Int J Geriatr Psychiatry. 2019 Jun;34(6):781-789. [CrossRef] [PubMed] [PubMed Central]
- Singh I, Edwards C, Duric D, Rasuly A, Musa SO, Anwar A. Dementia in an Acute Hospital Setting: Health Service Research to Profile Patient Characteristics and Predictors of Adverse Clinical Outcomes. Geriatrics (Basel). 2019 Jan 2;4(1):7. [CrossRef] [PubMed] [PubMed Central]
- Fong TG, Inouye SK. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat Rev Neurol. 2022 Oct;18(10):579-596. [CrossRef] [PubMed] [PubMed Central]
- van Velthuijsen EL, Zwakhalen SMG, Pijpers E, van de Ven LI, Ambergen T, Mulder WJ, Verhey FRJ, Kempen GIJM. Effects of a Medication Review on Delirium in Older Hospitalised Patients: A Comparative Retrospective Cohort Study. Drugs Aging. 2018 Feb;35(2):153-161. [CrossRef] [PubMed] [PubMed Central]
- Meredith K. Carbone, Marilyn R. Gugliucci, Delirium and the Family Caregiver: The Need for Evidence-based Education Interventions, The Gerontologist, Volume 55, Issue 3, June 2015, Pages 345–352. [CrossRef]
- Komici K, Guerra G, Addona F, Fantini C. Delirium in Nursing Home Residents: A Narrative Review. Healthcare (Basel). 2022 Aug 15;10(8):1544. [CrossRef] [PubMed] [PubMed Central]
- Singh I, Varanasi A, Williamson K. Assessment and management of dementia in the general hospital setting. Reviews in Clinical Gerontology. 2014;24(3):205-218. [CrossRef]
- Royal College of Psychiatrists (2024) National Audit of Dementia Care in General Hospitals Audit Round 6 Regional Report 2023/2024. London: Royal College of Psychiatrists. Available from: National Audit of Dementia (NAD) | Royal College of Psychiatrists (rcpsych.ac.uk).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).