Introduction
Nevus comedonicus (NC) is a rare hamartomatous skin disorder characterized by grouped dilated follicular openings filled with keratinous plugs resembling comedones. Typically manifesting at birth or during early childhood, NC often progresses into inflammatory lesions such as recurrent papules, pustules, cysts, and abscesses, significantly affecting the quality of life and psychosocial well-being of patients. Although benign, NC lesions are notoriously resistant to conventional therapies such as topical retinoids, keratolytics, antibiotics, surgical excision, and standard laser treatments. These modalities frequently result in incomplete lesion clearance, recurrence, aesthetic dissatisfaction, and notable morbidity due to scarring and pigmentary changes [
1,
2,
3].
Recent studies have explicitly emphasized the inadequacy of current therapeutic approaches, highlighting frequent treatment failure, significant recurrence rates, and patient dissatisfaction [
4,
5]. Consequently, there is a clear and unmet clinical need for innovative treatments capable of targeting both the superficial and deep follicular pathology characteristic of NC, without causing collateral tissue damage or scarring. Advanced modalities that combine precise tissue ablation with regenerative mechanisms hold particular promise for overcoming these longstanding therapeutic limitations [
6,
7].
Based on the author’s 20 years of clinical expertise in treating complex scars, including challenging skin graft and burn scars, the Pinholxell Therapy was developed as a dual-mode CO₂ laser technique integrating deep pinhole ablation with fractional resurfacing [
8]. This method was applied to a refractory case of Nevus Comedonicus (NC). This case report documents 15 years of consistent treatment across 55 sessions, highlighting significant, durable improvements in lesion clearance, normalization of skin texture, and enhanced patient quality of life, positioning Pinholxell as a highly promising therapeutic option for previously intractable NC cases.
Method
Topical anesthesia was achieved with 5% lidocaine ointment applied under occlusion for 1 hour. Treatment followed the Pinholxell Therapy, a dual-mode CO₂ laser method for deep dermal remodeling and epidermal regeneration. First, a DS-40U CO₂ laser (DSE, Seoul, Korea) in ultrapulsed mode was used to create 1 mm pinhole columns, penetrating from the mid to deep dermis in the affected facial and neck regions. Laser parameters included a pulse duration of 200–900 μs and a repeat interval of 5 ms, while preserving intact zones between pinhole columns to facilitate healing.Immediately afterward, a fractional CO₂ laser (eCO2® La-54, Lutronic, Korea) was applied at 35 mJ with 100 MTZ/cm² density to uniformly resurface the epidermis and enhance regeneration.
Figure 1 illustrates this two-step laser technique and post-Pinholxell therapy skin changes.
Each Pinholxell session lasted approximately 3 hours, including preparation, laser application, and post-treatment care, and was performed at 2-month intervals to allow sufficient healing. Over 15 years, the patient underwent 55 sessions in total. Immediately post-procedure, the treated area was cooled with sterile saline-soaked gauze for 5 minutes, followed by application of a hydrocolloid dressing (DuoDERM®) maintained for up to 7 days. If fluid accumulation occurred within 72 hours, the dressing was replaced; otherwise, it remained intact. After removal, a regimen of regular emollient application was initiated to maintain skin hydration and promote healing. If comedonal eruptions appeared due to occlusion, topical retinoids were applied selectively. The postoperative strategy emphasized continuous hydration to support epidermal barrier restoration and optimal dermal remodeling. The macro-injuries induced by pinhole columns initiate a wound- healing cascade involving inflammation, proliferation, and remodeling, ultimately resulting in neocollagenesis and dermal reorganization. Maintaining hydration throughout this process is critical for keratinocyte migration, fibroblast activation, and minimizing transepidermal water loss. Clinically, this approach reduces scab formation, accelerates re-epithelialization, and enhances the potential for both structural and cosmetic recovery. In my experience, strict adherence to moisture-based wound care significantly improves Pinholxell Therapy outcomes in severe nevus comedonicus.
Written informed consent was obtained from the patient for publication of clinical details and images presented in this case report. The case study was conducted in strict accordance with the principles outlined in the Declaration of Helinki
Case Description
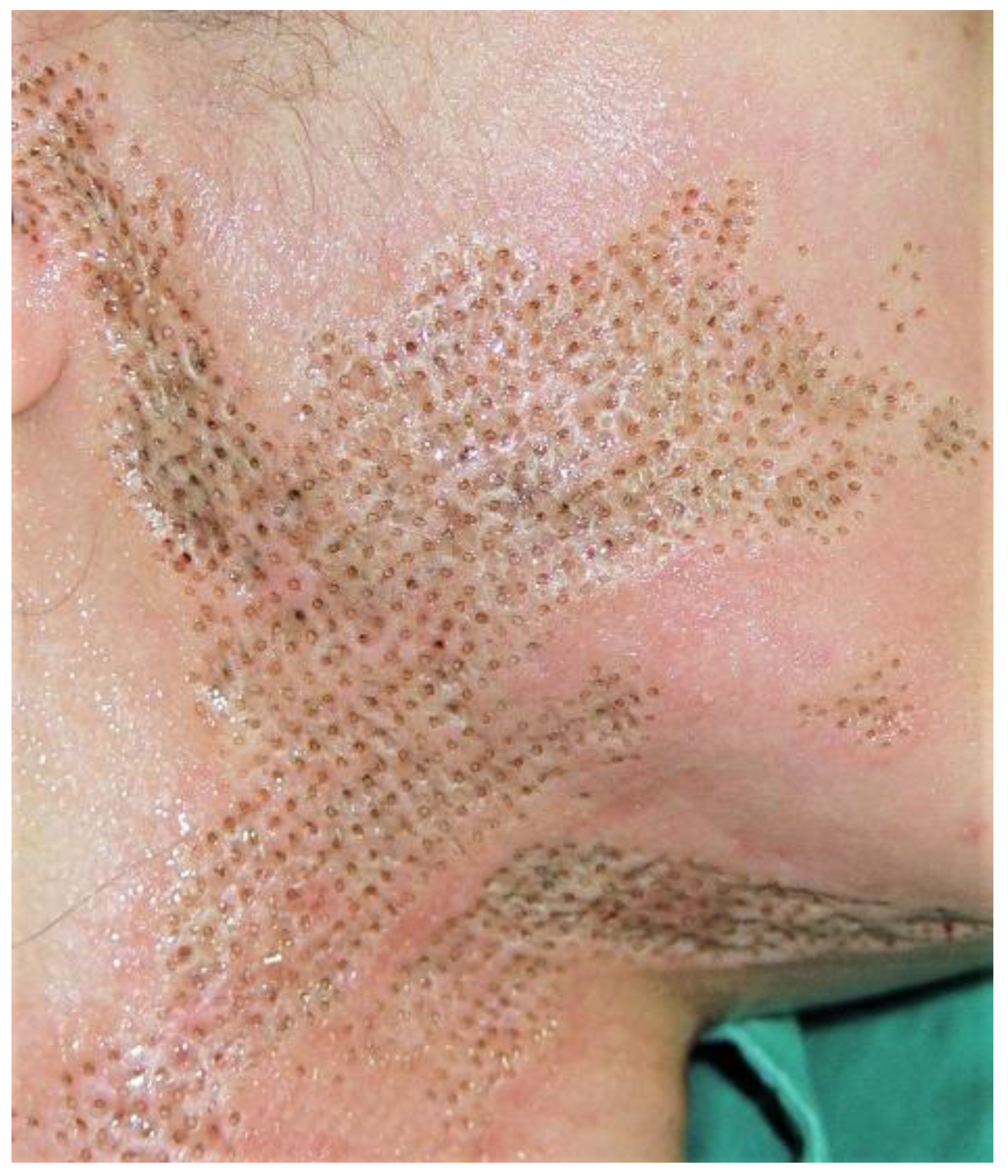
A 28-year-old Asian female presented with severe nevus comedonicus characterized by widespread comedone-like lesions extensively affecting the right preauricular area, cheek, perioral region, jawline, and neck. These lesions emerged during adolescence, progressively expanded, and reached stabilization in her mid-twenties. Clinically, she experienced intermittent pruritus and localized pain without systemic manifestations, significantly impacting her psychological and social well-being. Medical evaluation revealed no additional systemic or syndromic abnormalities, and the diagnosis was confirmed histologically by skin biopsy. Examination revealed numerous deep-set and enlarged follicular openings densely packed with keratinous debris, resulting in pronounced textural irregularities and persistent surface deformities (
Figure 2).
Due to the extensive depth and distribution of these lesions, conventional therapeutic approaches—including surgical excision and subsequent skin grafts—were assessed as impractical by the university hospital. Consequently, treatment options were limited, posing ongoing clinical and therapeutic challenges in managing her condition and alleviating associated aesthetic and psychosocial distress. Figure1 illustrates the dual-mode Pinholxell CO₂ laser technique applied in this case, highlighting the precise creation of deep dermal pinhole columns followed by fractional resurfacing, which provided a targeted therapeutic approach.
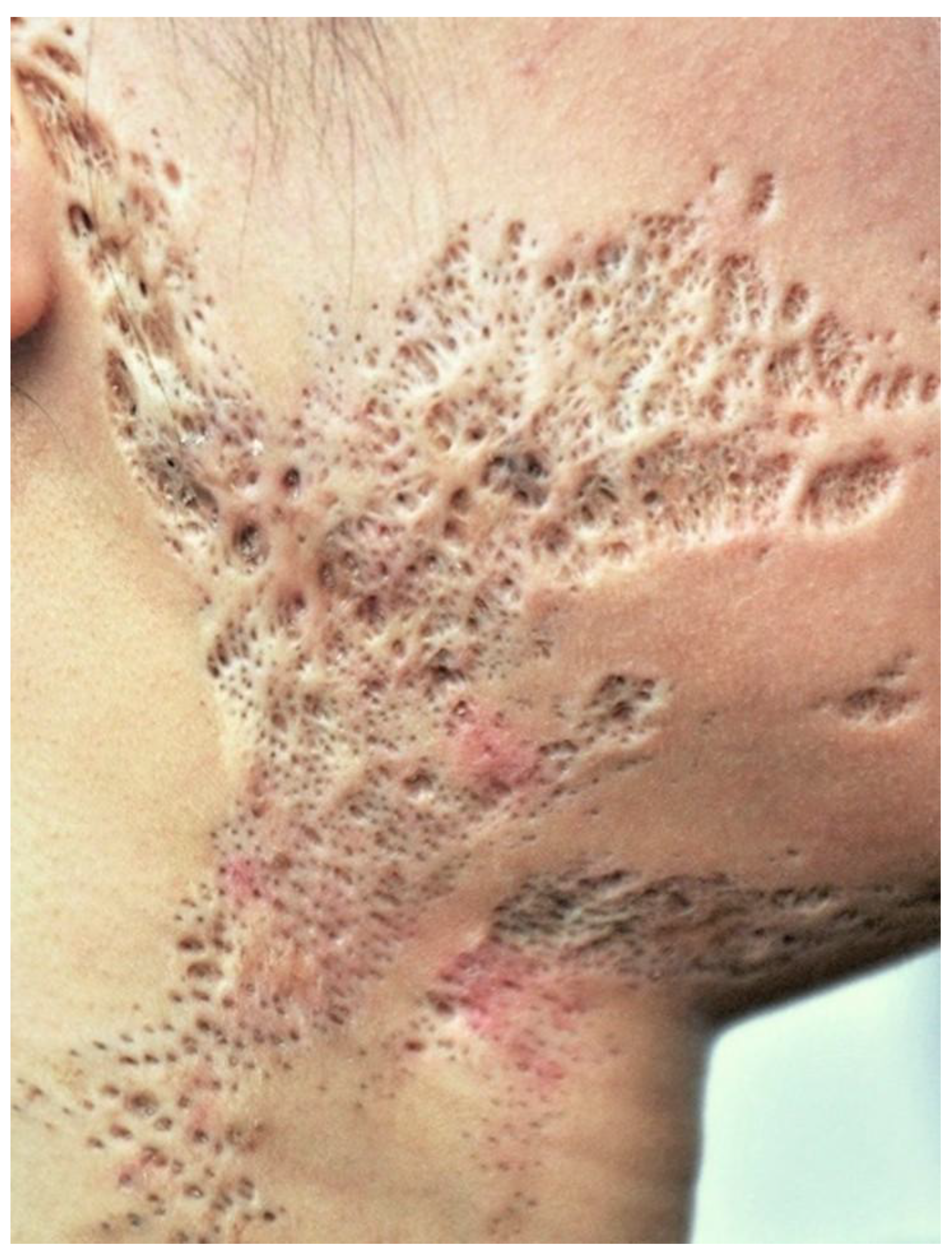
Figure 3 shows evidence of significant surface remodeling, with reduced pigmentation and improved textural uniformity.
Figure 3 demonstrates the skin condition after two full sessions
, spaced two months apart. The overall number and prominence of follicular openings—a hallmark of severe nevus comedonicus—have markedly decreased. The lesions are visibly shallower and more flattened, and the treated area exhibits a smoother texture with reduced comedonal congestion and discoloration. These changes are indicative of early remodeling, confirming that even after two sessions, the Pinholxell Therapy can reverse deep structural abnormalities in treatment-resistant nevus comedonicus.
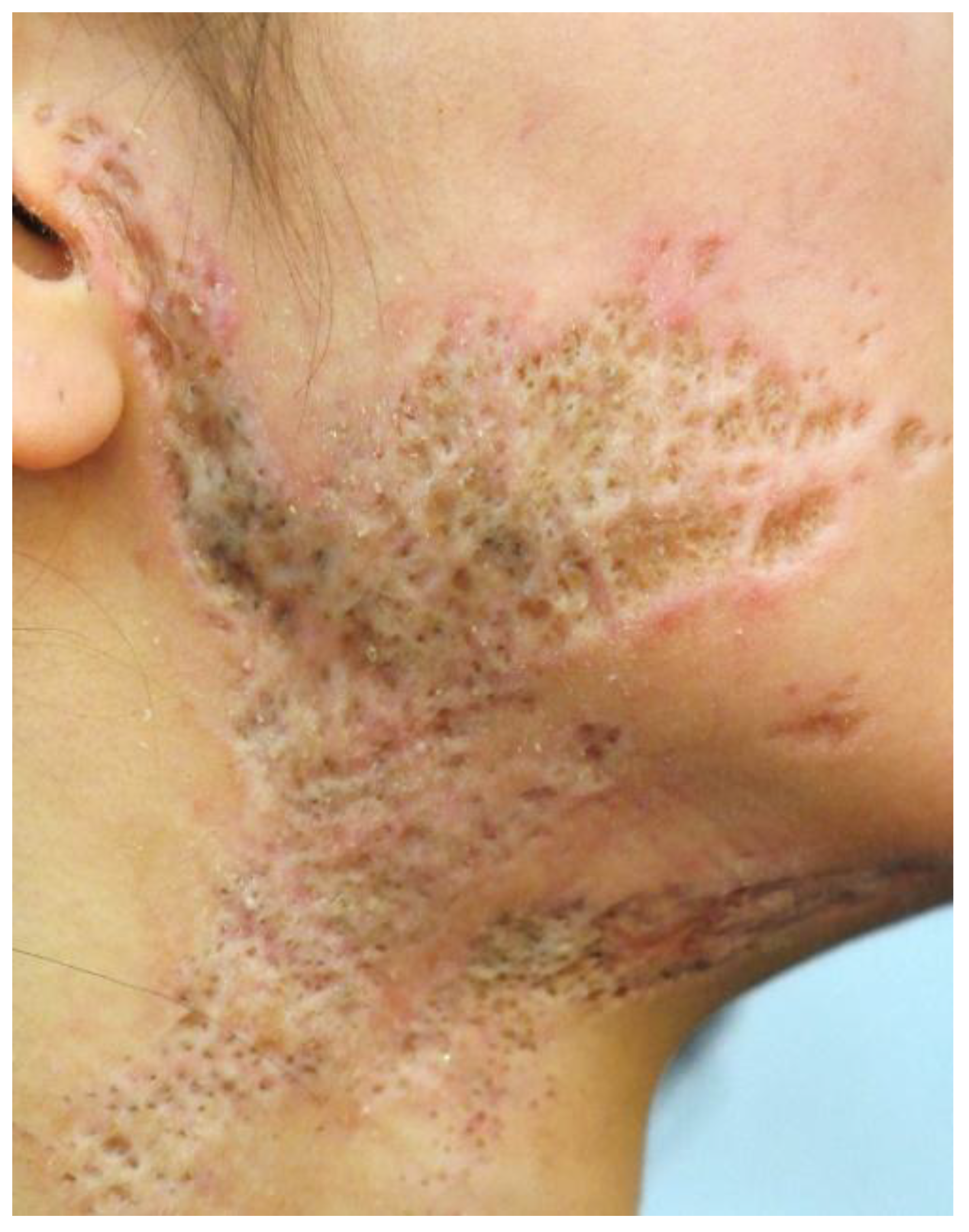
Figure 4 shows marked structural and aesthetic improvement in severe nevus comedonicus following serial Pinholxell Therapy. Compared to earlier stages (
Figure 2 and
Figure 3), follicular openings are further reduced, and the skin surface appears smoother and more compact. Dermal thickness is more uniform, with deep craters flattened or replaced by regenerating tissue. Pigmentation has normalized in several areas, and erythema and post-inflammatory discoloration are notably diminished. These changes indicate ongoing collagen remodeling and epidermal regeneration. The findings highlight the cumulative effect of repeated Pinholxell sessions in transforming deep, treatment-resistant lesions into more normalized tissue, demonstrating its strong long-term regenerative potential.
By the 22nd Pinholxell session, a key clinical milestone was achieved:
Figure 5 shows only minimally visible follicular openings, while
Figure 5 reveals the first signs of early epithelialization. At this advanced stage, the once-pronounced, keratin-filled pits have largely resolved and been replaced by a smooth, re-epithelialized surface. Skin texture is markedly refined, with improved dermal thickness, uniform contours, and significant flattening of the initial crater-like architecture. Although focal hyperpigmentation persists, it is substantially less pronounced than in earlier stages—underscoring the extensive dermal remodeling and epidermal regeneration made possible by prolonged, repeated Pinholxell Therapy.
In
Figure 6, epithelialization has further advanced, with more than half of the scar area now re-epithelialized. Although subtle textural irregularities and residual scarring persist, the treated region appears nearly normal due to extensive epithelial coverage and significantly smoother, evenly pigmented skin. This reflects the substantial regenerative capacity and aesthetic improvements achieved with ongoing Pinholxell Therapy.
Significant clinical improvement is evident, with the treated skin now closely resembling normal, healthy skin. Key improvements include:
Reduction of follicular openings: Previously enlarged, deeply plugged follicular openings are significantly reduced, resulting in noticeably smoother skin texture.
Flattening and epithelialization of scar tissue: Skin topography is substantially improved, demonstrating extensive epithelialization with decreased surface irregularities and a more even contour.
Improvement in pigmentation: Hyperpigmentation and dark keratinous plugs are notably diminished, indicating effective resolution of accumulated keratinous material.
Enhanced aesthetic outcome: The overall cosmetic appearance is significantly enhanced, positively impacting patient satisfaction and psychological well-being.
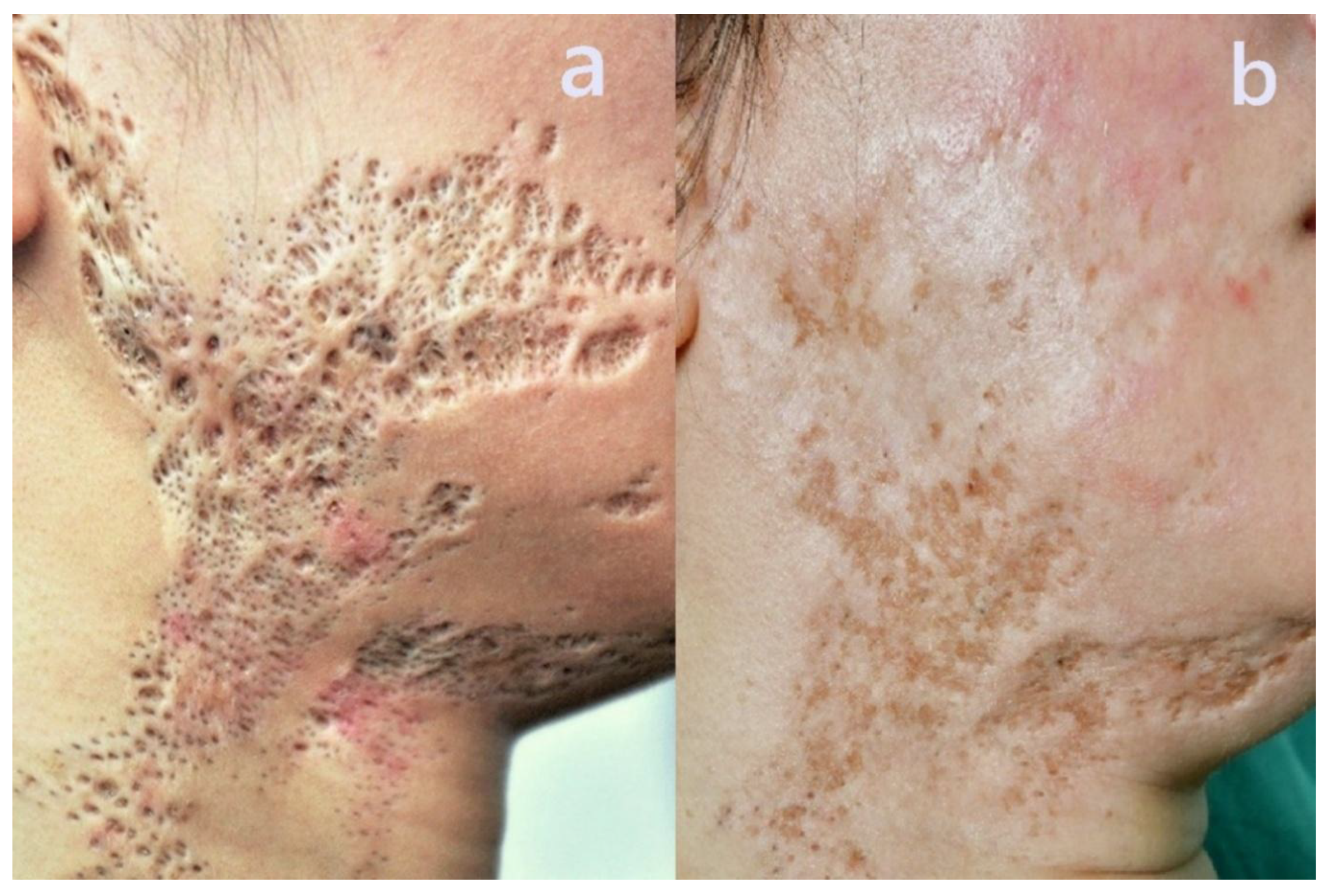
Long-term clinical outcomes were assessed by comparing baseline and final treatment conditions. As demonstrated in
Figure 8, the baseline condition (a) shows extensive, deeply plugged follicular openings and severe surface irregularities characteristic of severe nevus comedonicus. The post-treatment image (b), taken after 55 sessions, reveals remarkable skin remodeling, with significantly diminished follicular openings, smoother texture, and improved pigmentation closely resembling normal skin. This visual comparison clearly highlights the transformative potential and durable long-term efficacy of Pinholxell Therapy.
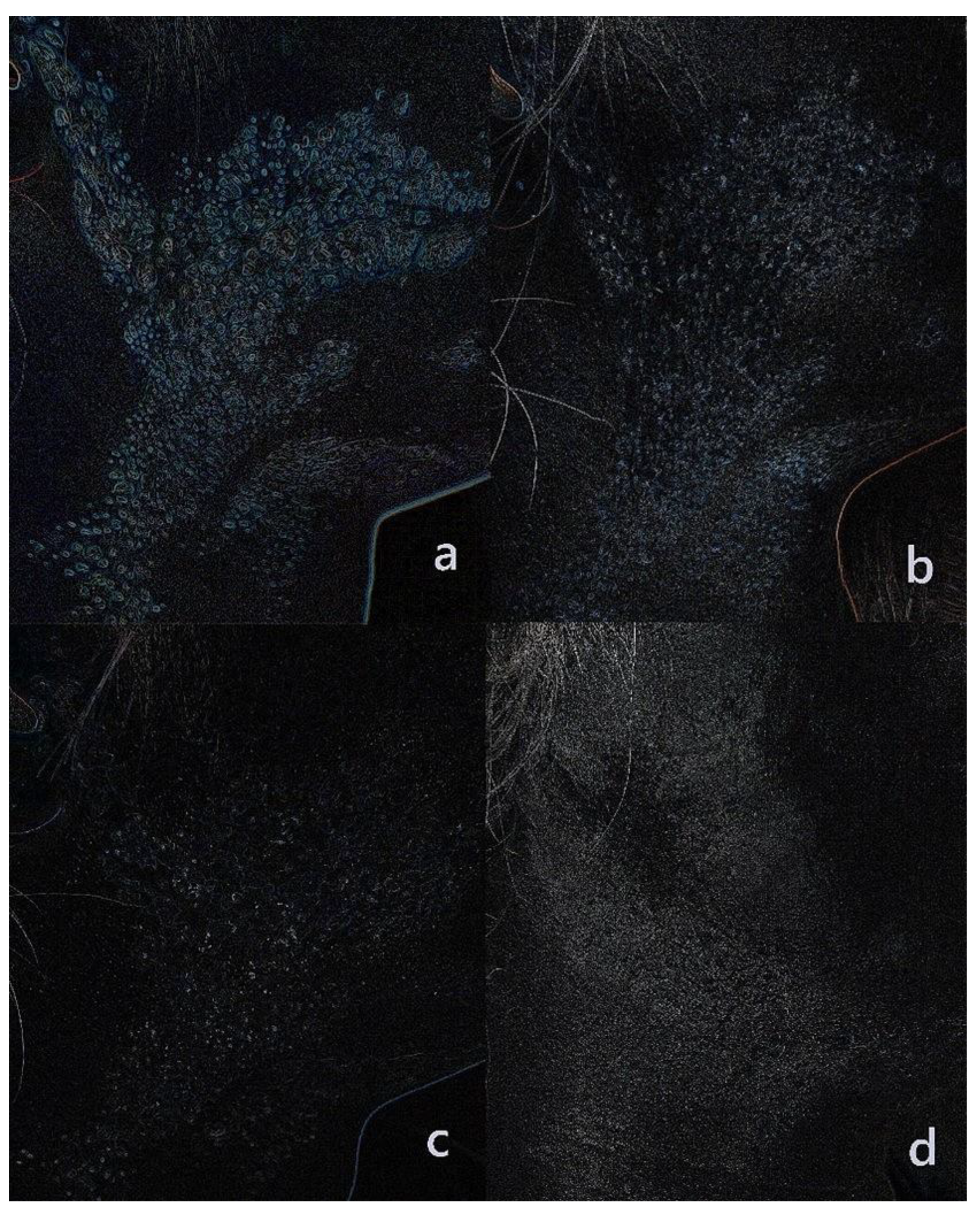
To quantitatively illustrate progressive structural improvement, edge detection analysis was conducted at multiple treatment intervals (
Figure 9). Blue highlights indicate follicular openings. At baseline (a), numerous prominent follicular openings were evident. After 8 sessions (b), a marked reduction in follicular openings occurred. By 22 sessions (c), there was a further decrease in follicular prominence along with improved skin smoothness. Finally, after 55 sessions (d), minimal follicular structures remained, and the skin texture closely resembled that of normal skin. This sequential analysis underscores the consistent and profound dermal remodeling achieved by repeated Pinholxell treatments.
This sequential follicular opening analysis clearly demonstrates the consistent and significant dermal remodeling achieved by repeated Pinholxell treatments. The skin surface now appears smooth and homogeneous, pigmentation irregularities are substantially reduced, and only minor residual hyperpigmentation remains—underscoring the extensive dermal remodeling attained through prolonged and repeated therapy. As demonstrated in
Table 1, the patient exhibited progressive reductions in lesion depth, follicular openings, and pigmentation, along with substantial improvements in overall skin texture across 55 sessions of Pinholxell Therapy.
These long-term follow-up results strongly support the capability of Pinholxell Therapy—a dual-mode approach combining deep pinhole columns ablation and fractional CO₂ laser resurfacing—to effectively remodel severe nevus comedonicus lesions. Therefore, this approach represents a highly promising therapeutic option, even for cases traditionally considered refractory or resistant to conventional treatment modalities.
Discussion
Conventional management strategies for NC, such as topical agents and surgical excision, have historically demonstrated limited efficacy due to their superficial mode of action, which inadequately addresses the deeper follicular pathology inherent in NC [
4,
5]. A recent systematic review underscored that surgical excision and conventional laser treatments frequently fail to completely eradicate lesions, contributing to high recurrence rates and patient dissatisfaction due to significant cosmetic impairment [
3,
4]. Furthermore, traditional laser modalities often lack the necessary precision to target deeply situated follicular keratin plugs, thus increasing the risk of post-procedural complications, including persistent erythema, scarring, and pigmentary disorders [
1,
2].
Recent literature strongly advocates novel treatment methods capable of delivering deep dermal remodeling combined with selective epidermal resurfacing [
5,
6]. The limitations of existing therapies highlight the necessity of an advanced treatment paradigm such as Pinholxell Therapy. This innovative approach, which combines focused pinhole-column creation via CO₂ laser with fractional CO₂ laser resurfacing, allows for precise targeting of deep-seated follicular structures while concurrently promoting epidermal regeneration and dermal remodeling. By harnessing synergistic mechanisms—precise follicular ablation, regenerative cytokine induction, and rapid epidermal healing—Pinholxell Therapy comprehensively addresses NC lesions, potentially overcoming the established inadequacies of traditional treatment modalities [
8].
In conclusion, given the well-documented limitations of conventional therapies and the growing consensus on the urgent need for new treatment strategies, further research and clinical validation of advanced laser-based modalities such as Pinholxell Therapy are essential. This approach holds significant promise for establishing a definitive therapeutic standard for Nevus Comedonicus.
Conclusions
This case study demonstrates the long-term efficacy of Pinholxell Therapy, a dual-mode CO₂ laser approach, in treating severe nevus comedonicus. Over 15 years and 55 sessions, the patient showed marked reductions in lesion depth, follicular plugging, and surface irregularities, accompanied by improvements in skin texture and pigmentation, with minimal scarring or adverse effects. These findings strongly support the “cytokine hypothesis,” wherein controlled macro-injuries from combined pinhole and fractional laser treatments stimulate dermal remodeling and epidermal regeneration. Pinholxell therapy thus offers a promising, effective non-surgical option for managing refractory or inoperable NC. Further prospective clinical studies are warranted to standardize treatment protocols and validate its effectiveness across broader patient populations.
Institutional Review Board Statement
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki. The patient provided written informed consent for the publication of all clinical data and photographs. Identifiable details have been omitted or anonymized. The signed consent form is securely archived and available upon request by the editorial office of Lasers in Surgery and Medicine. This case report did not require formal Institutional Review Board (IRB) approval, as it documents a retrospective single-patient therapeutic course without experimental intervention.
Conflicts of Interest
The author declares that there is no conflict of interest regarding the publication of this article.
References
- Kirtak N, Inaloz HS, Karakok M, Ozgoztasi O. Extensive inflammatory nevus comedonicus: treatment with topical retinoids and antibiotics. J Eur Acad Dermatol Venereol. 2003;17(2):220-222.
- Tchernev G, Ananiev J, Semkova K, Dourmishev LA, Schönlebe J, Wollina U. Nevus comedonicus: an updated review. Dermatol Ther (Heidelb). 2013;3(1):33-40. [CrossRef]
- Guldbakke KK, Khachemoune A. Nevus comedonicus: a review of management and treatment options. Dermatol Ther. 2007;20(3):160-163.
- Ferrari B, Taliercio V, Restrepo P, Luna PC, Abad ME, Larralde M. Surgical outcomes and patient satisfaction in nevus comedonicus treatment: a systematic review. Dermatol Surg. 2022;48(5):497-502.
- Liu Y, Ma J, Wang T, Zhang J, Liu J. Long-term efficacy of fractional CO₂ laser for nevus comedonicus: a systematic review and meta-analysis. J Dermatolog Treat. 2023;34(1):214-219.
- Wang Y, Zhao X, Liu Y, et al. Emerging therapeutic strategies for nevus comedonicus: a narrative review. Dermatol Ther (Heidelb). 2023;13(2):401-409.
- Lee SJ, Kang JS, Kim JK. Combination therapies involving fractional CO₂ laser and regenerative techniques: novel pathways for treating resistant nevus comedonicus. Lasers Surg Med. 2024;56(4):388-395.
- Seo, J. K. Five Cases of Skin Graft Scar Treatment Using the Pinholxell Method: A Dual-Mode 10,600-nm CO2 Laser Approach. Preprints 2025, 2025060087. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).