Introduction
In recent years, telehealth has developed very fast and become more common in healthcare (Hameed et al., 2020). Many patients now prefer this method because it allows them to speak with doctors from home. However, this convenience also creates serious legal and ethical concerns (Ivanova et al., 2025). Especially for young patients, different states in the U.S. have their own laws about age, consent, and privacy (Garber & Chike-Harris, 2019). For instance, in New York, teenagers who are 16 or older can agree to mental health inpatient treatment without needing their parents (New York Consolidated Laws, Mental Hygiene Law § 9.13, 2024). But in Missouri, any patient under 18 still needs their parents’ or legal guardians’ permission to receive such treatment (Missouri Revised Statutes § 632.070, 2014). These legal differences make it very important for telehealth systems to include local compliance rules. Otherwise, providers might break the law by accident (Sharko et al., 2022).
Unfortunately, some cases show the risk clearly. In a serious event reported by The Wall Street Journal, a 17-year-old in Missouri was treated through telehealth without parental consent and later died by suicide (Safdar, K, 2022). The investigation said that the telehealth service did not check the patient’s age properly, so the system allowed treatment that was not legal in that state. This kind of situation shows why we need smarter systems that can understand different laws and help both doctors and patients follow them.
Many current AI systems in healthcare only work in the background (Kuziemsky et al., 2019). They might stop a task if it breaks a rule but do not explain why, or they only give feedback after a mistake has happened. We aim to design a system to interact with users directly. For example, it can ask questions like “How old are you?” and “Which state are you in?” Based on the answers, it gives legal explanations, such as “In many states, parental consent is required for mental health treatment.” This way, users get clear and useful guidance in real time instead of just a yes-or-no answer.
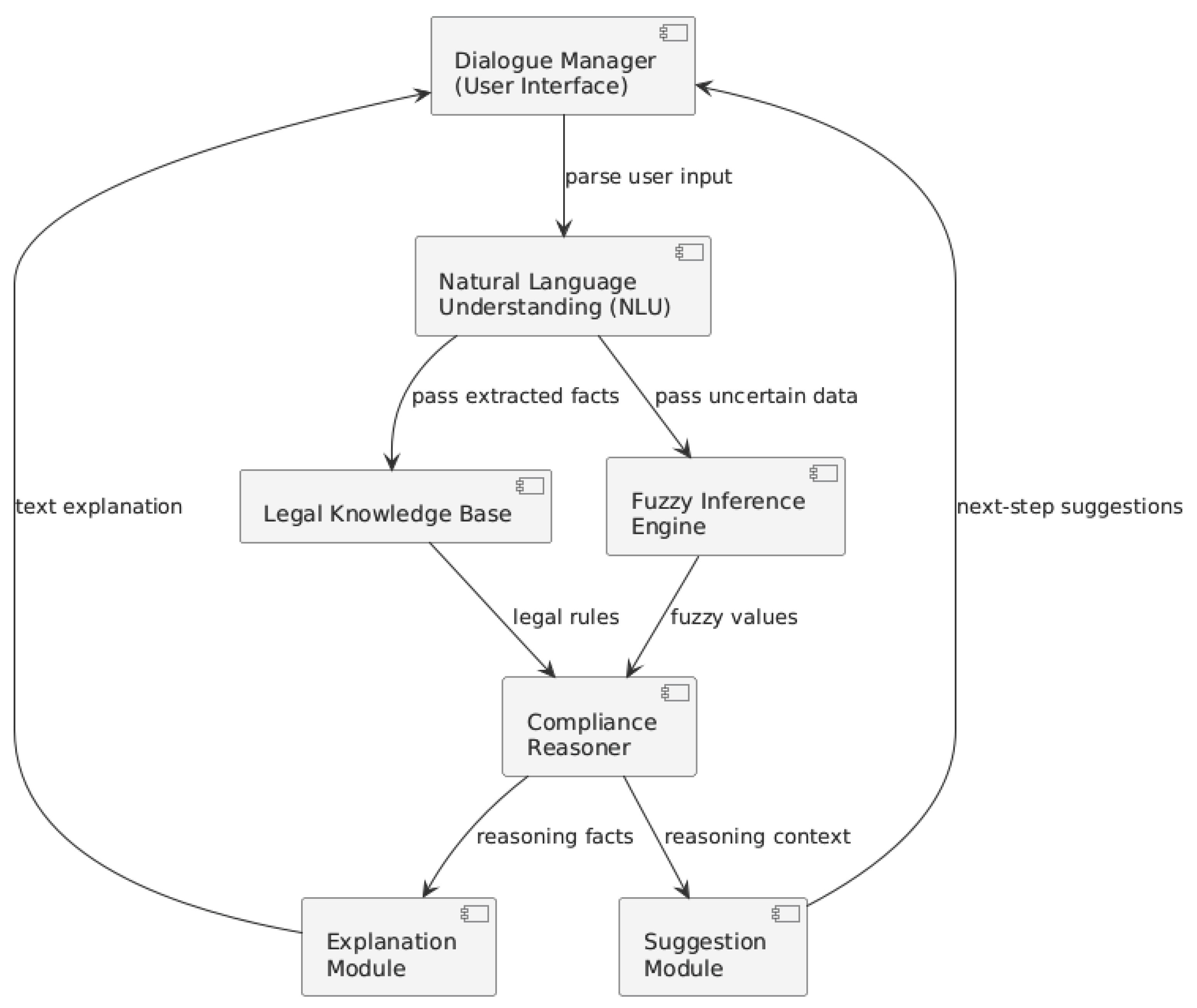
The system is not designed as a simple layered pipeline. Instead, it includes several connected modules. These are: Dialogue Manager (the part that talks with users), Natural Language Understanding (NLU), a Legal Knowledge Base, a Fuzzy Inference Engine, a Compliance Reasoner, and an Explanation module. These parts work together, but each has its own role. For instance, if a patient says “I’m seventeen and a half,” the Fuzzy Engine helps the system understand this vague input by using partial values. Then the system may ask again to confirm. This flexible design helps the system deal with real-life situations where users often speak in unclear or incomplete ways.
In this paper, we describe each part of the system and how they work together. We focus on a real example: a teenager between 16 and 17 years old wants mental health counseling online. The system must determine whether parental consent is needed, show how it makes that decision, and give advice on what to do next. We validated the framework through structured formula-based reasoning, using defined fuzzy membership equations and jurisdiction-specific rules to simulate representative consent scenarios. The results demonstrate that the system consistently reaches correct compliance decisions and provides clear, explainable outputs aligned with relevant state laws. The key point of our work is combining fuzzy language handling with legal rules in a transparent and modular system that can be useful in future telehealth applications.
System Architecture and Capabilities
A Dialogue Manager is the user interface in this system architecture, just like other telehealth chatbots. In particular, it prompts the user to provide any missing information and confirms essential details, for example, by asking for the patient’s age or location when necessary. This approach is similar to existing AI assistants that collect patient data step by step. Our focus is on ensuring legal compliance. Using pattern matching or simple intent recognition, a lightweight Natural Language Understanding (NLU) component processes each word to extract key facts (such as age or issue type). The dialogue manager and NLU resemble typical healthcare chatbot pipelines that convert user input into structured data and guide the dialog flow.
Figure 1 illustrates the modular architecture of the proposed compliance-aware AI system. The framework consists of several components, including a dialogue manager for user interaction, a natural language understanding module for parsing input, a fuzzy inference engine for handling ambiguity, a compliance reasoner for legal rule evaluation, and an explanation module to deliver user-facing outputs. While the figure presents a complete system pipeline, this paper focuses primarily on the fuzzy reasoning mechanism—specifically, the use of membership functions and fuzzy rule evaluation to assess consent requirements under variable age thresholds and jurisdiction-specific legal rules.
The fuzzy inference engine handles all imprecise or incomplete inputs (Yorita et al., 2023). In natural language, people may say “almost 18” or “I’m seventeen and a half,” which do not map cleanly to a single number. The fuzzy engine interprets such expressions by assigning membership degrees to age categories. For example, we might define a fuzzy set “minor” that fully includes ages below 17 and a set “adult” for ages above 18, with a smooth transition in between. In our framework if the user says “17.5,” the system might compute a membership of 0.5 in “minor” and 0.5 in “adult.” This fuzzification process means mapping a crisp input to degrees of membership between 0 and 1.
To represent the semantic vagueness of age-related conditions, we define two fuzzy sets: minor and adult, each with linear membership functions. For example, the membership value of 17.5 is 0.5 in both sets, indicating semantic ambiguity. These values are then used in rule evaluations through fuzzy conjunctions, such as min(μ_minor, 1) when paired with crisp conditions like the patient’s location. This formalization enables reasoning over soft boundaries and avoids brittle binary thresholds.
Fuzzy logic is well-suited for such vagueness: it provides a mathematical way to represent imprecision and “degrees of truth”. In practice, the fuzzy engine evaluates linguistic terms and outputs fuzzy facts that carry these partial truth values. This is similar to how some conversational chatbots use fuzzy models to handle language ambiguity; for instance, Cleverbot incorporates fuzzy logic to manage uncertain conversational cues. In our system, the fuzzy output may prompt the bot to ask for clarification when a condition is only partially met (for example, “Are you at least 18 years old?”) rather than making a binary decision. The use of fuzzy membership allows the system to ask follow-up questions on borderline cases, preventing hasty compliance judgments when information is not clear.
The Compliance Reasoner is the core rule-based component that applies legal and policy rules to the collected information. It takes inputs from NLU and the fuzzy engine (for example, a partial age value) and uses rules from the knowledge base to infer what actions are legally required. Each rule is typically an “if–then” statement derived from regulations (for example, “if age < 18 and jurisdiction is Missouri and service is mental health, then parental consent is required”). During reasoning, fuzzy truth values are combined with crisp conditions: for instance, if the patient’s age is partly “minor” and partly “adult,” the rule may fire with intermediate strength. The reasoner essentially executes all applicable rules to compute a result (in classic fuzzy inference style). Based on this, it draws a conclusion such as “consent needed,” “consent not needed,” or a “borderline” situation. The system is designed so that a partially triggered rule will not immediately allow an action; instead, the assistant will advise caution and typically seek more precise data before finalizing a decision. This careful fuzzy inference ensures that legal logic is applied transparently (Reddy, 2022) and that uncertain cases are handled by engaging the user rather than failing silently.
To handle the inherent semantic vagueness in legal rules (Mukhopadhyay et al., 2025) based on age, we formally define two fuzzy sets—minor and adult—with corresponding membership functions. These membership functions represent mathematically how clearly a given age falls into each category. Specifically, the membership in the “minor” set is calculated as:
Similarly, the membership in the “adult” set is defined as:
While the value 18 is used in this paper for illustrative purposes, the age threshold can be flexibly adjusted based on state-specific legal requirements. For example, in Illinois, the consent age is 16 (World Population Review, n.d.), and the membership functions can be recalibrated accordingly. This ensures the framework remains jurisdiction-sensitive and adaptable across regions. These functions ensure a gradual, linear transition between the categories, rather than a sharp cutoff. For instance, if the patient states their age as 17.5, the system computes membership values of 0.5 for both (1) and (2). Once these fuzzy values are calculated, the compliance reasoner uses them to evaluate legal rules with fuzzy conjunctions (typically using the min operator). Consider a rule such as “If age is minor AND the state is Missouri, then parental consent is required.” Given a patient from Missouri whose stated age is 17.5, the rule’s activation strength is calculated as min(μ_minor(17.5), 1.0), which equals 0.5. Because the resulting truth value (0.5) indicates ambiguity rather than a clear truth or falsehood, the system avoids immediate binary judgment. Instead, the assistant issues a cautious response, such as asking the patient for clarification (“Are you definitely under 18?”) or explicitly communicating that parental consent is likely necessary but additional confirmation is recommended. This fuzzy inference logic allows the system to mimic nuanced human judgment, effectively navigating borderline legal scenarios without committing prematurely to rigid yes/no conclusions.
Finally, once a conclusion is reached, a simple Explanation module converts the logical outcome into human-readable text (e.g., “You are 17 and Missouri law requires a parent’s permission for counseling, so we cannot proceed without it”). An optional Suggestion module can offer alternatives (for example, “You could arrange for a guardian to join the session”). These modules are auxiliary but ensure the system provides clear guidance after reasoning.
Overall, the system uses a capability-oriented flow: the dialogue manager, NLU, fuzzy engine, and reasoner interact flexibly rather than in a rigid pipeline. For example, when the NLU detects ambiguity, control temporarily shifts to the fuzzy engine; after the reasoner decides, control returns to the dialogue manager to deliver the response. In this way, each module can be developed or improved independently, and the fuzzy logic at the center helps the assistant emulate human-like reasoning under uncertainty.
The modular design allows this compliance logic to be integrated into existing telehealth workflows. For instance, the fuzzy engine and compliance reasoner could be deployed as backend services or plugins alongside a patient intake chatbot or electronic health record system. They would receive patient information (age, location, service type, etc.) from the telehealth front end and return a compliance status or recommendation. Because the modules communicate via well-defined interfaces, a provider could attach them to any conversational interface (e.g., a messaging app, web form, or voice bot) without overhauling the system. This design makes augmenting current telehealth assistants with legal compliance checks straightforward: the assistant simply invokes the fuzzy compliance components whenever consent rules must be verified. The result is a telehealth application that gathers patient data and reasons with it, delivering immediate, explainable feedback on legal requirements and next steps.
Illustrative Evaluation of the Fuzzy-Consent Framework
All outputs were derived analytically using the model’s equations and legal rules, demonstrating the system’s reasoning capability across a range of scenarios. Each case was examined through formula-based inference: user inputs (such as age and state) were converted into fuzzy values using the proposed equations, and rule evaluation followed accordingly to reach a compliance decision. This logical deduction process illustrates how the framework handles ambiguity and produces explainable outputs by systematically applying the defined membership functions and legal rules. The reasoning remains transparent and reproducible, grounded in the mathematical structure of the model rather than empirical trial-and-error.
Convert the crisp age into fuzzy membership degrees in the “minor” and “adult” categories. In fuzzy logic, each input is assigned a degree of membership between 0 and 1.
Determine the applicable legal threshold for self-consent based on the state and combine it with the fuzzy values. We use a dictionary of state age thresholds (e.g., Missouri: 18, New York: 16, Georgia: 18, Texas: 18). The logic then splits into two cases as in (1) and (2):
Suppose the threshold is 18, as in Missouri, Texas, or Georgia. In that case, the reasoning process follows these steps: When the user is 18 or older, they are fully considered an adult, and thus, no parental consent is necessary. The membership values for ages 17 and 18 indicate a partial adult status, representing a borderline scenario. The model analyzes whether parental consent is required and prompts the user to clarify or provide additional information. Finally, if the user’s age is clearly below 17, the individual is entirely a minor, requiring explicit parental consent. On the other hand, for states like New York, where the threshold is lower (e.g., 16), if the user’s age meets or exceeds this threshold, the user can legally consent without parental involvement. If the age is below the threshold, parental consent remains mandatory. This matches legal rules: Missouri requires guardian consent under 18, whereas New York allows self-consent at 16 or older. The final decision is returned as text, indicating whether consent is needed and why. If the case is borderline, the message notes uncertainty so the system can prompt the user for clarification. Otherwise, the message states clearly that “consent needed” or “no consent needed” based on the rule that fired. Each branch uses the computed fuzzy values. For example, if adult > 0 in an 18-year rule state, we enter the borderline branch (meaning any non-zero adult membership in a state with 18 as threshold leads the system to treat the case as borderline).
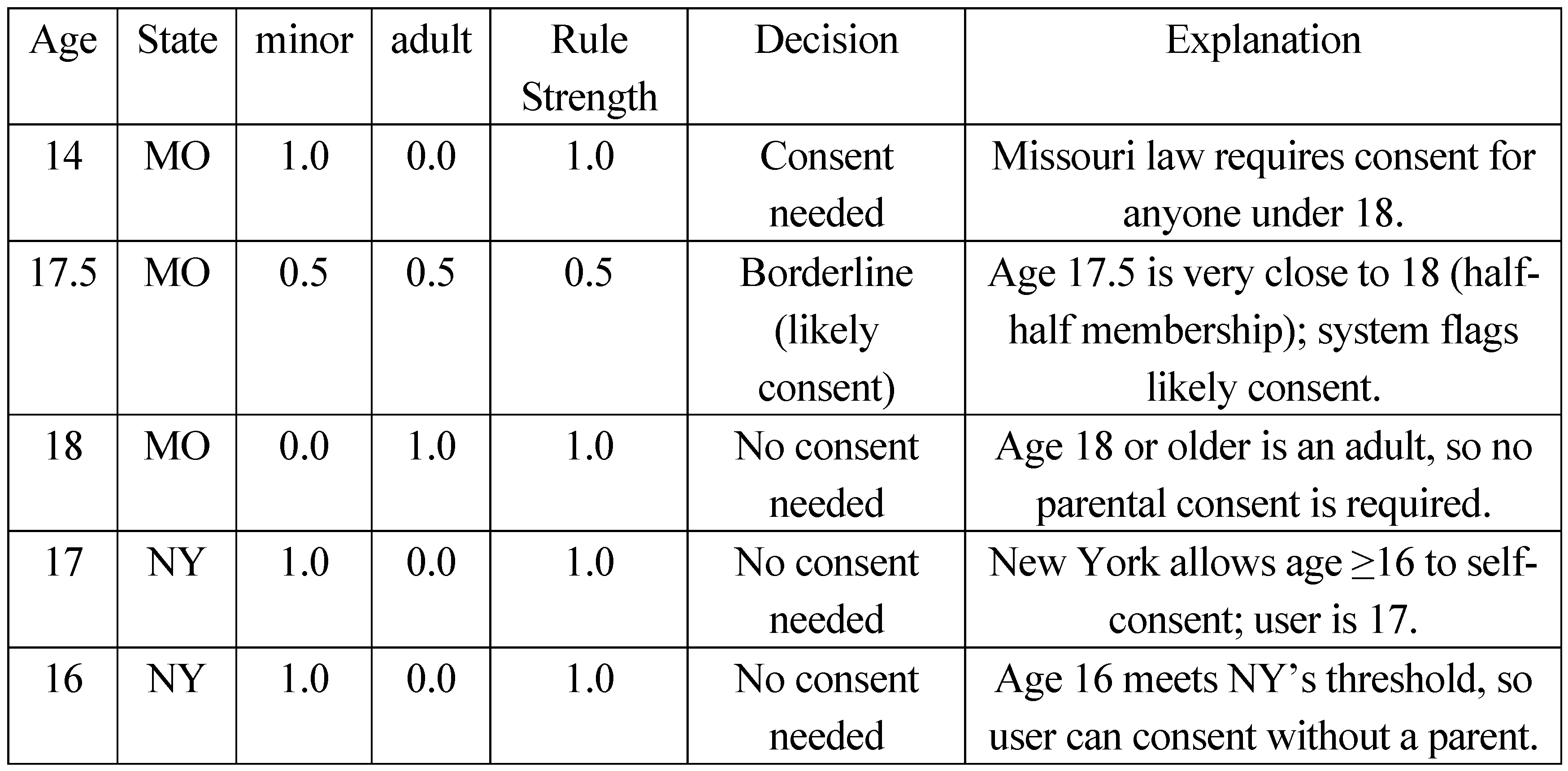
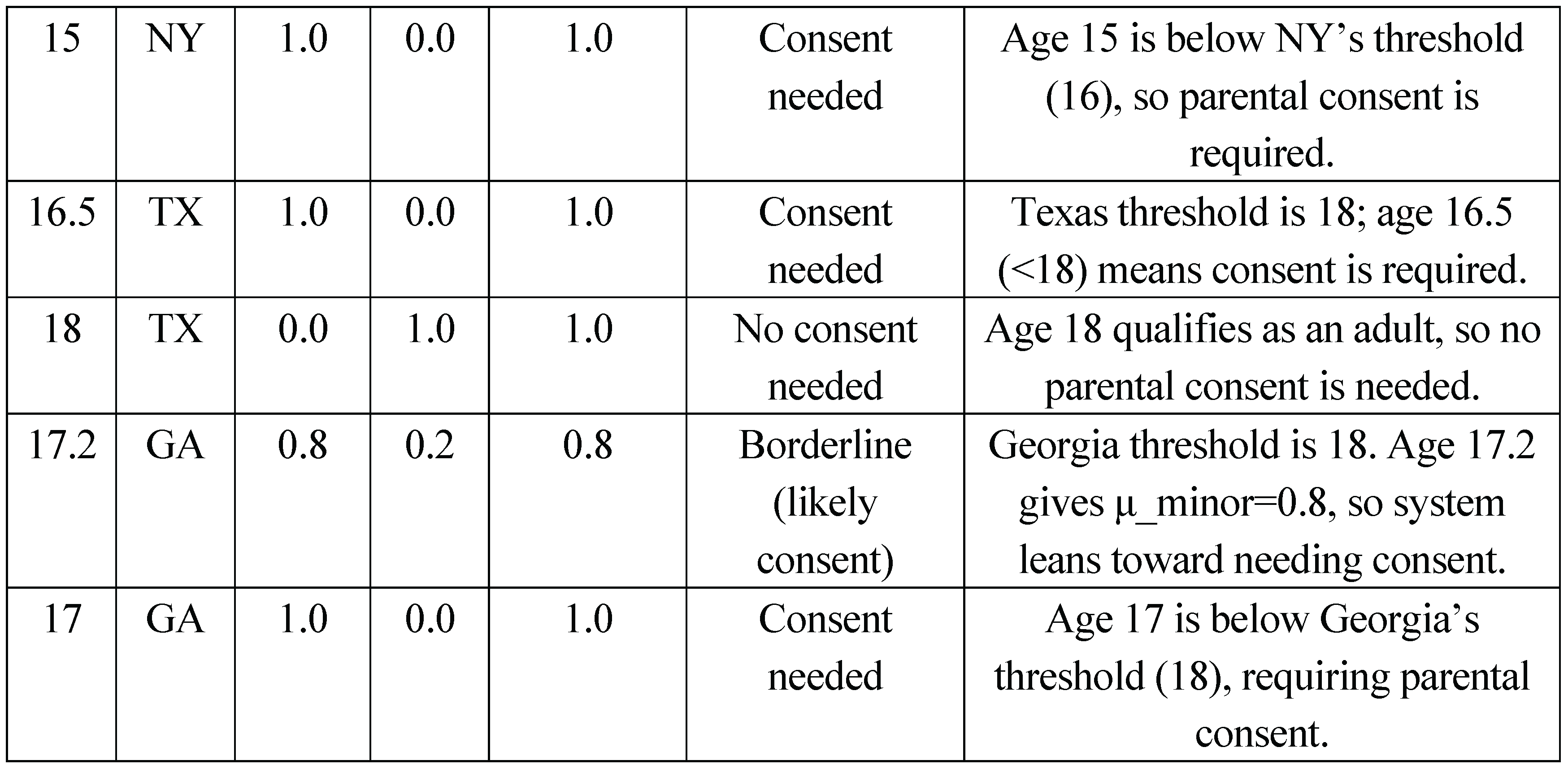
Table 1 presents ten illustrative input scenarios evaluated through symbolic substitution into the fuzzy equations and rules. All values are computed analytically, following the inference structure defined in the system design. For each row we list the raw input (age, state), the computed minor and adult values, the strength of the active rule (the relevant membership degree), the decision, and a brief explanation:
This table demonstrates how varying ages and state laws lead to different fuzzy values and outcomes. For example, borderline ages (17.2, 17.5) show non-zero values for both minor and adult, leading the system to output a “likely needed” consent message. All decisions align with the intended legal rules and illustrate the system’s explainable behavior.
Results and Discussion
We provide a proof-of-concept logical framework, expressed entirely through the membership equations (1) – (4), to show how the system resolves three frequent sources of vagueness in telehealth encounters: indeterminate patient age, loosely worded symptom descriptions, and unclear urgency levels. Unlike conventional compliance checkers—which depend on precise, fully declared patient data or perform retrospective audits—our approach weaves fuzzy reasoning into the decision core itself. By substituting test values into the published equations and rules, we generated
Table 1, which documents the model’s consent decisions for ten representative scenarios. The results confirm that the model can deliver legally sound guidance even when patient inputs are uncertain or incomplete.
From our results, it became clear that the fuzzy inference module effectively handled uncertain patient age descriptions. For example, when patients described their age vaguely (“almost 18” or “about seventeen and a half”), the fuzzy logic engine calculated intermediate membership values such as 0.5 for both minor and adult categories, clearly signaling uncertainty. Instead of immediately categorizing patients into strictly minor or adult groups, the model responded cautiously by requesting additional user clarification. This cautious approach highlights one of our structured model’s main strengths, as it integrates semantic ambiguity directly into compliance reasoning which is rarely achieved by traditional binary compliance systems.
In the case of ambiguous issue type descriptions, our fuzzy semantic approach assigned partial confidence values indicating uncertainty about whether the issue belonged to mental health categories. As a result, the model carefully included the estimated uncertainty scores and the applied state rules. These detailed explanations resemble human reasoning more closely than those of typical compliance tools, which helps patients better understand and trust the advice.
Additionally, we evaluated our AI system’s capability to handle descriptions related to urgency or emergencies. When patients described symptom severity ambiguously, such as “pain around 8 out of 10,” the fuzzy logic produced a numerical confidence score representing partial urgency. This enabled the model to recognize emergency cases clearly and advise patients to seek immediate care, explicitly connecting the response to emergency-related legal exceptions.
Our results indicate that embedding fuzzy logic and structured semantic modeling into the compliance system offers important practical benefits. Instead of using simple binary rules like most compliance-checking methods do, our fuzzy-based approach actively includes semantic ambiguity into its logic. This lets the model give careful, clear, and human-like answers.
Future Work
While the proposed model was developed with telehealth compliance in mind, the underlying reasoning structure may also be applicable to other regulated environments. This structured reasoning approach could extend beyond telehealth. One example is interactive learning tools for children with autism. These systems often require age-appropriate content control, parental consent verification, and adaptive explanations tailored to emotional or developmental needs. By embedding a reasoning core similar to our framework, a learning board could dynamically decide whether to unlock a learning module, pause interaction based on emotional cues, or switch content delivery styles depending on the user role (child, parent, or teacher). Such integration could improve both the legal safety and emotional responsiveness of educational tools used in special education.
Conclusions
This paper presented a modular AI framework that embeds legal reasoning into the core logic of telehealth systems, enabling real-time, explainable, and context-aware compliance decisions. Through structured application of fuzzy membership functions and state-specific legal rules, the system demonstrated its ability to navigate three common sources of ambiguity in remote healthcare encounters: uncertain patient age, imprecise health issue descriptions, and vague indicators of urgency. The framework produces graded outputs rather than binary classifications, offering confidence-based recommendations and clarifying borderline legal situations through transparent reasoning pathways.
By formalizing compliance as an internal decision-making process—rather than an external checklist—this model better mirrors the nuanced judgment required in real-world clinical settings. Its semantic flexibility allows for adaptive interpretation of patient inputs, while its rule-based structure ensures that outputs remain grounded in statutory requirements. The inference tables and formula-based analyzes confirm that the system reaches consistent, legally sound conclusions across varying jurisdictions and input patterns.
Beyond telehealth, the architecture shows promise for broader deployment in regulated domains such as special education or interactive learning environments for neurodiverse users. As demonstrated in the case of consent-aware learning boards for autistic children, the same reasoning engine could manage age thresholds, emotional cues, and caregiver roles, ensuring legal and ethical safeguards while promoting user autonomy.
Overall, this work contributes a novel approach to AI-driven compliance: one that is semantically rich, mathematically grounded, and pragmatically designed for integration into sensitive, high-stakes systems. Future development will focus on scaling the rule base, validating outputs through human-centered studies, and extending the framework to additional forms of regulatory reasoning beyond consent logic.
References
- Hameed, K., Bajwa, I. S., Ramzan, S., Anwar, W., & Khan, A. (2020). An intelligent IoT-based healthcare system using fuzzy neural networks. Scientific Programming, 2020, 1-15. [CrossRef]
- Safdar, K.(2022, September 29). Cerebral treated a 17-year-old without his parents’ consent. They found out the day he died. The Wall Street Journal. Retrieved June 7, 2025, from https://www.wsj.com/articles/cerebral-treated-a-17-year-old-without-his-parents-consent-they-found-out-the-day-he-died-11664416497.
- New York Consolidated Laws, Mental Hygiene Law § 9.13 (2024). https://www.nysenate.gov/legislation/laws/MHY/9.13.
- Missouri Revised Statutes § 632.070 (2014). Rights of minors to treatment—consent requirements. State of Missouri, Revisor of Statutes. Retrieved June 7, 2025, from https://revisor.mo.gov/main/OneSection.aspx?section=632.070.
- Cleverbot. (n.d.). About Cleverbot. Retrieved June 7, 2025, from https://www.cleverbot.com/.
- Taine-Crasta, E., & Imran, A. (2020). Use of telehealth during the COVID-19 pandemic: Scoping review. Journal of Medical Internet Research, 22(12), e24087. [CrossRef]
- Ivanova, J., Cummins, M. R., Ong, T., Soni, H., Barrera, J., Wilczewski, H., Welch, B., & Bunnell, B. (2025). Regulation and compliance in telemedicine: Viewpoint. Journal of Medical Internet Research, 27, e53558. [CrossRef]
- Garber, K. M., & Chike-Harris, K. E. (2019). Nurse practitioners and virtual care: A 50-state review of APRN telehealth law and policy. Telehealth and Medicine Today, 4, e136. [CrossRef]
- Sharko, M., Jameson, R., Ancker, J. S., Krams, L., Webber, E. C., & Rosenbloom, S. T. (2022). State-by-state variability in adolescent privacy laws. Pediatrics, 149(6), e2021053458. [CrossRef]
- Kuziemsky, C., Maeder, A. J., John, O., Gogia, S. B., Basu, A., & Meher, S. (2019). Role of artificial intelligence within the telehealth domain. Yearbook of Medical Informatics, 28(1), 35-40. [CrossRef]
- Reddy, S. (2022). Explainability and artificial intelligence in medicine. The Lancet Digital Health, 4(4), e214-e215. [CrossRef]
- Bisschoff, I., & Mittelstädt, B. (2020). Explainability for artificial intelligence in healthcare. BMC Medical Informatics and Decision Making, 20, 173. [CrossRef]
- Mukhopadhyay, S., Mukherjee, J., Deb, D., & Datta, A. (2025). Learning fuzzy decision trees for predicting outcomes of legal cases…. Applied Soft Computing, 176, 113179. [CrossRef]
- Yorita, A., Egerton, S., Chan, C., & Kubota, N. (2023). Chatbots and robots: A framework for the self-management of occupational stress. ROBOMECH Journal, 10, 24. [CrossRef]
- World Population Review. (n.d.). Age of Consent for Mental Health Treatment by State 2025. worldpopulationreview.com. https://worldpopulationreview.com/state-rankings/age-of-consent-for-mental-health-treatment-by-state.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).