1. Introduction
Serum transfer experiments containing arthritogenic antibodies from the K/BxN mouse model of rheumatoid arthritis has been used extensively to examine the mechanism of amelioration of the arthritis by intravenous immunoglobulin (IVIG) [
1,
2,
3,
4,
5,
6]. These publications have used a serum-transfer approach by obtaining arthritogenic serum from severely affected mice and then transferring those sera into normal, non-arthritic mice [
1,
2,
3,
4,
5,
6]. We have previously reported on using the K/BxN mouse model to examine the effects of IVIG and recombinant IgG1 rFc-μTP-L309C hexamer on amelioration of the endogenously produced arthritis in this model [
6]. We found that either IVIG or rFc-μTP-L309C were efficacious to significantly ameliorate the arthritis in these mice with rFc-μTP-L309C 10-fold more efficacious than IVIG [
6]. We further showed that the mechanism of reversal of arthritis was, in part, due to rFc-μTP-L309C able to inhibit neutrophil infiltration into the joints as well as inhibition of IL-1β production [
7].
Our earlier work looking at the effect of rFc-μTP-L309C treatment on neutrophils provided a partial explanation as to the mechanism of action of rFc-μTP-L309C to ameliorate the arthritis in the K/BxN mouse model. However, arthritis is a multifactorial disease, and we wished to understand what role, if any, the T-cell compartment may play in the effect of rFc-μTP-L309C on ameliorating the arthritis. Thus, in this brief correspondence, we have further investigated the possible mechanism of rFc-μTP-L309C to ameliorate endogenous arthritis by examining the effects of this molecule on activated T-cells. We find that treatment with rFc-μTP-L309C causes a decrease in the population of the Th1 and Th17 phenotypes with decreases in production of IL-17 and IFN-γ, in the spleen, lymph nodes and joints. GM-CSF was, in fact, increased in the spleen but was significantly decreased in the other tissues, including the joints. Concomitant increases in FoxP3+ T regulatory (Tregs) cells and interleukin-10 (IL-10) were also found in the joint synovial fluid. Transforming growth factor-β (TGF-β), although increased, the increase was not found to be significant. The decrease in the inflammatory Th1 and Th17 cell populations and an increase in anti-inflammatory Tregs, IL-10 and, marginally, TGF-β explains, in part, the mechanism of rFc-μTP-L309C amelioration of the arthritis in these animals.
2. Materials and Methods
2.1. K/BxN Mice
KRN T-cell receptor (TCR) transgenic mice on a C57BL/6 background were obtained from the Jackson Laboratory, a kind gift from C. Benoist, Harvard University. NOD/Lt mice were purchased from The Jackson Laboratory. Arthritic mice were obtained by crossing KRN mice (F, 6 weeks old) with NOD/Lt (M, 6 weeks old) mice to produce K/BxN mice expressing both the TCR transgene KRN and the MHC class II molecule I-Ag7. Mice were kept under a natural light-dark cycle, maintained at 22 ± 4°C, and fed with standard diet and water ad libitum. All experiments were performed following our institutions’ guidelines on the care and use of laboratory animals and only after approval of the protocol by the animal care committee of the University Health Network (UHN); animal use protocol AUP 1788, and after review by the St. Michael’s Hospital Unity Health Toronto Animal Care Committee (ACC); approved protocol ACC 138.
2.2. Reagents
Recombinant Fc-µTP-L309C was provided by CSL Behring AG, Switzerland. Human serum albumin (HSA) was obtained from the Canadian Blood Services. Antibodies used included: anti-CD16/32 (BD Pharmingen, San Jose, CA), anti- CD44-PE-Cy7 (clone IM7, Biolegend, San Diego, CA), anti-CD4-APC-Alexa 750 (clone RM4-5, Thermofisher Scientific, Waltham, MA), anti-GMCSF-FITC (clone MPI-22E9, Biolegend, San Diego, CA), anti-IL-17-APC (clone eBio-17B7, Thermofisher Scientific, Waltham, MA), anti-IFN-gamma-Pacific Blue (clone XMG1.2, Biolegend, San Diego, CA), anti-CD25-APC (clone PC61, Biolegend, San Diego, CA), anti-FOXP3-FITC (clone FJK-16s, Thermofisher Scientific, Waltham, MA). A cascade yellow viability stain (Thermofisher Scientific, Waltham, MA) was used to distinguish between live and dead cells. For intracellular staining, cells were stimulated with PMA (Sigma Aldrich, St. Louis, MI) and ionomycin (Sigma Aldrich, St. Louis, MI). GolgiStop (Thermofisher Scientific, Waltham, MA) was used to enhance the detection of intracellular stains. IL-10 and TGF-β were measured by ELISA (R&D Systems).
2.3. Arthritis Scoring and Treatment
The clinical scores of the mice were monitored daily over the course of each experiment [
6,
7]. The development of arthritis was assessed daily, and the severity of arthritis was scored for each paw on a 3-point scale, in which 0 = normal appearance, 1 = localized edema/ erythema over one surface of the paw, 2 = edema/ erythema involving more than one surface of the paw, 3 = marked edema/erythema involving the whole paw. The scores of all four paws were added for a composite score, with a maximum score of 12 per mouse [
6,
7]. K/BxN mice with high clinical scores of 9 or greater were treated by subcutaneous injection (s.c) of 200 mg/kg rFc-µTP-L309C on days 1, 3, 5, 7, 9, and 11. HSA was used as a protein control.
2.4. Organs Examined
The spleens, popliteal lymph nodes, and joints from K/BxN mice that received 6 s.c. injections of 200 mg/kg of rFc-µTP-L309C were isolated and placed in RPMI 1640 + 5% FCS on ice. Mice treated with HSA were used as a control. The spleens and popliteal lymph nodes were pushed through a fine mesh strainer (70-µm cut-off) to form a single cell suspension. RBCs were lysed from the spleens. The cells were washed and resuspended in PBS + 2% FCS for cell counts. Joint washes were performed as previously described [
8]. Malleoli and surrounding soft tissue (excluding fat) were removed from both rear limbs and placed in RPMI 1640 + 5% FCS on ice for 60 min. The medium was then removed, centrifuged, and the supernatant (joint wash) stored at -20˚C until subsequent analysis. The washed malleoli and cell pellets were combined for each individual mouse and digested for 30 min at 37˚C with 1 mg/ml collagenase (CLS-1, 250 U/mg; Worthington Biochemical, Lakewood, NJ) and 0.1 mg/ml DNase I (1U/µL; Thermo Fisher). The digests were strained (70-µm cut-off), washed, and resuspended in PBS + 2% FCS for cell counts. Tregs were enriched using the EasySep mouse Treg cell enrichment kit (Stemcell Technologies). Single-cell suspensions of spleens, popliteal lymph nodes and joint digests were resuspended in PBS containing 2% FCS. Cells were incubated with anti-CD16/32) as FcγR blocking agent and stained for CD4, CD25 and/or CD44. Intracellular staining was used for GM-CSF, IL-17, IFN-γ, and/or FOXP3. For intracellular staining, cells were stimulated with PMA (Sigma Aldrich, St. Louis, MI) and ionomycin (Sigma Aldrich, St. Louis, MI). GolgiStop (Thermofisher Scientific, Waltham, MA) was used to enhance the detection of the intracellular stains. Cells were permeabilized with a FOXP3 permeabilization kit (Thermofisher Scientific). Cells were fixed with 4% PFA and staining was analyzed by flow cytometry on a BD LSRFortessa (BD Biosciences, San Jose, CA), and the data was analyzed by using FlowJo software (Ashland, OR). Measurement of IL-10 and TGF-β used ELISA kits (R&D Systems) according to manufacturer’s protocols. Mice treated with HSA at a similar dose as for rFc-µTP-L309C were used as a control.
2.5. Statistical Analysis
Statistical tests were performed using GraphPad Prism 8 for Windows software. Analyses of differences between sample groups were performed using the statistical tests indicated in the figure legends. Data shown are mean ± standard deviation (SD), unless otherwise stated. P < 0.05 was considered statistically significant.
3. Results
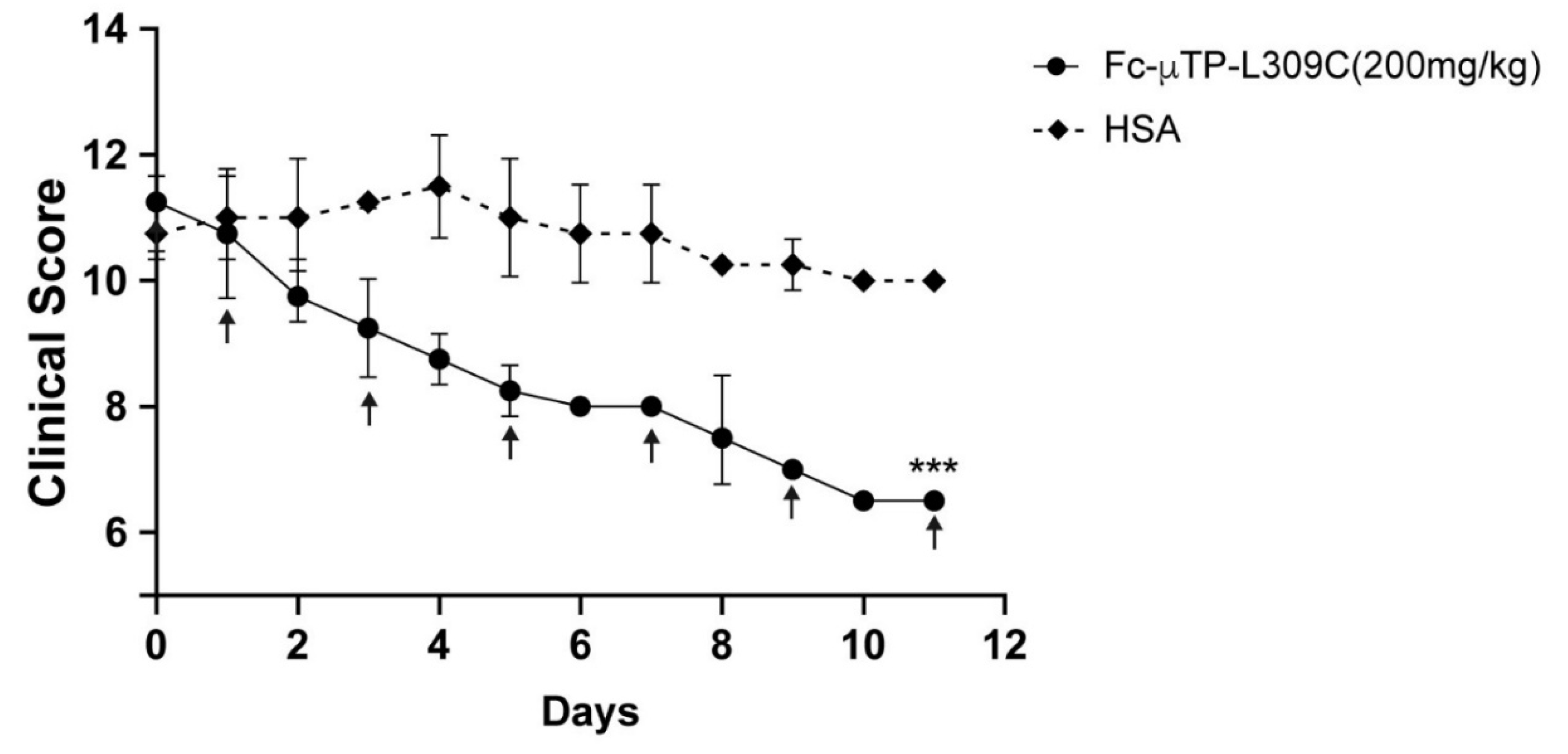
3.1. rFc-µTP-L309C Ameliorates Endogenous Arthritis in K/BxN Mice
Figure 1 shows the efficacy of rFc-µTP-L309C to ameliorate the spontaneous arthritis in K/BxN mice. Mice were allowed to develop severe arthritis, clinical score of ~10 (day 0), then administered 200 mg/kg rFc-µTP-L309C or HSA as a control over 11 days, given on days 0, 1, 3, 5, 7, 9,and 11. Control mice, treated with HSA, reached a clinical score of ~12 while the clinical score of the rFc-µTP-L309C-treated mice had dropped to 3 (p<00001).
3.2. Th1 and Th17 T-Cells Are Decreased in the Spleen, Lymph Nodes and Joints of K/BxN Mice After rFc-µTP-L309C Treatment
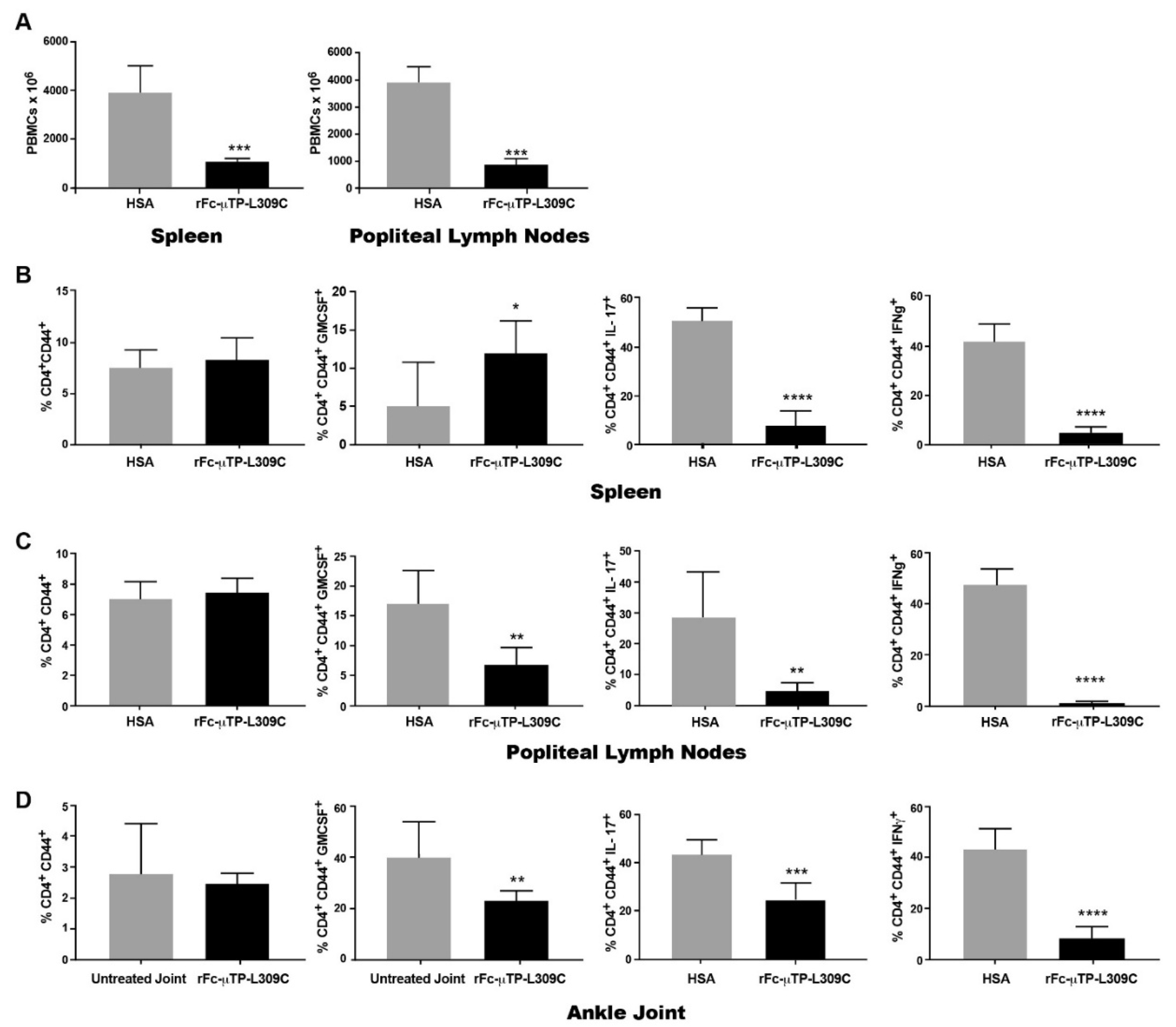
K/BxN mice that were at high clinical scores of 9-12, were given 6 s.c. injections on days 1, 3, 5, 7, 9, and 11 of 200 mg/kg of rFc-µTP-L309C, and HSA (200 mg/kg given s.c.) treated mice were used as controls. The spleen, popliteal lymph nodes and ankle joint fluid were collected (after dissection), on day 12 and cellular content analyzed. Knee joint synovial fluid was also collected for an ELISA to measure IL-10 and TGFβ levels.
We found that the total number of mononuclear cells in the spleen and lymph nodes was significantly decreased in the rFc-µTP-L309C-treated group vs. the HSA-treated control group (
Figure 2A). Similar numbers of activated T-cells (CD4
+CD44
+) in the spleen (
Figure 2B), popliteal lymph nodes (
Figure 2C) and ankle joints (
Figure 2D). Using intracellular staining we show that IL-17 (marker for Th17 T-cells) is significantly decreased in the spleen, popliteal lymph nodes and ankle joints. Although GM-CSF was significantly increased only in the spleen, GM-CSF and IFN-γ (markers for Th1 T-cells) were all significantly decreased in mice treated with rFc-µTP-L309C compared to HSA treated mice (
Figure 2B–D).
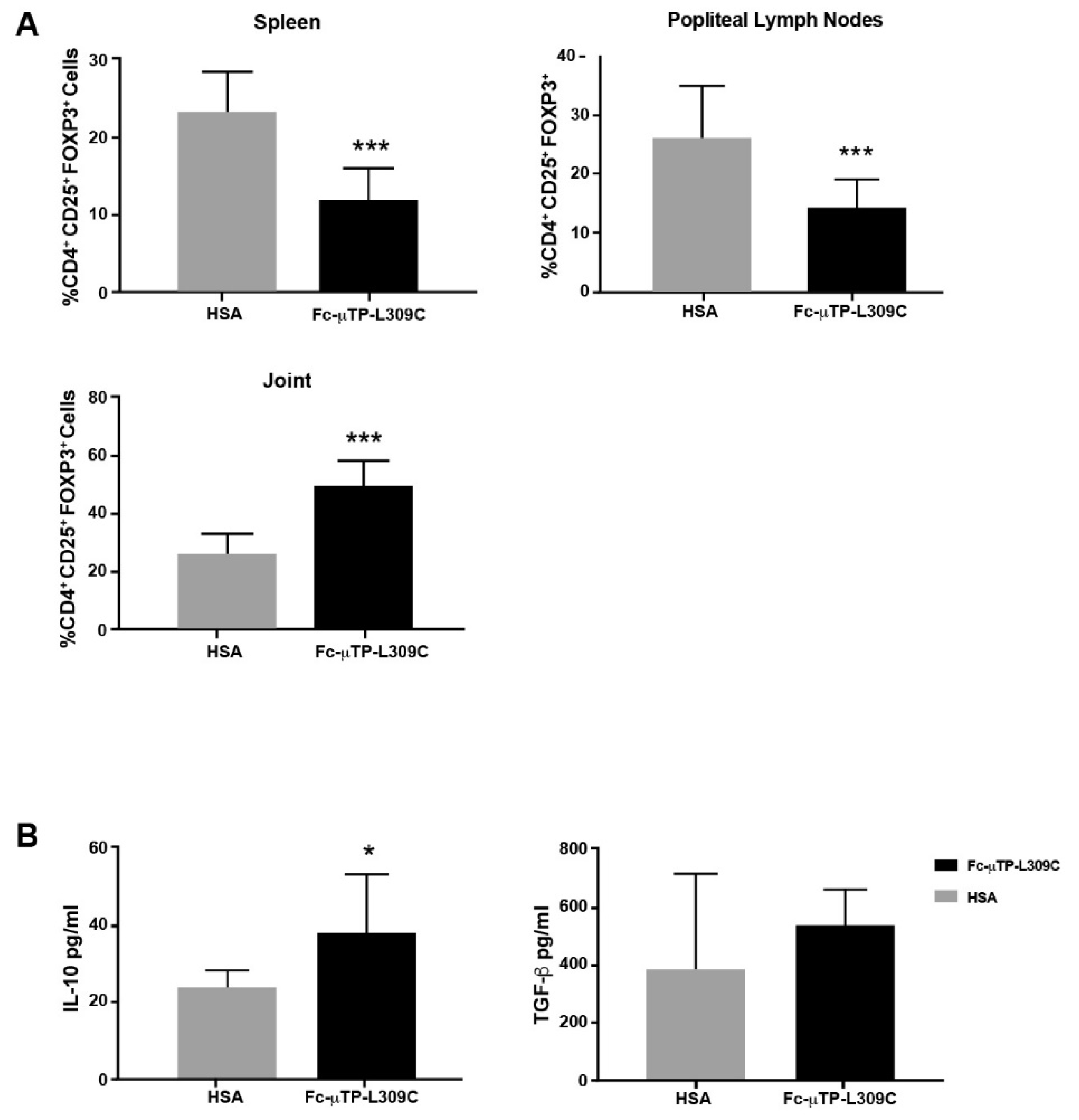
3.3. Tregs and IL-10 Are Increased in the Spleen, Lymph Nodes
We found that the number of CD4
+CD25+FOXP3
+ Tregs were significantly decreased in the spleen and popliteal lymph nodes but, in contrast, significantly increased in the joint [
Figure 3A). Possibly, these Tregs from the spleens and popliteal lymph nodes were being recruited to the joints in response to rFc-µTP-L309C administration. In line with these results, we also found that the levels of IL-10 in the synovial fluid of these mice also increased upon repeated administration of rFc-µTP-L309C, presumably because of the increase in Tregs [
Figure 3B). Although TGF-β showed an increase, mean ~500 pg/ml compared to ~400 pg/ml for HSA, this moderate trend increase was not significant (
Figure 3B).
4. Discussion
We have previously shown that the arthritis produced endogenously by K/BxN mice can be ameliorated by either IVIG or rFc-µTP-L309C, a recombinant human IgG1 Fc-hexamer [
7]. Although rFc-µTP-L309C was shown to inhibit neutrophil infiltration into the joint as well as IL-1β, and this effect was undoubtedly responsible, at least in part, for the amelioration of the severe arthritis in these mice, it didn’t provide a complete understanding of possible mechanisms for the therapeutic response of the molecule. In the study herein, we have further examined in the K/BxN arthritis model, the effect of rFc-µTP-L309C on the expression of T-cell subsets, including Th1, Th17 and T-regulatory cells (Tregs) in the spleens, lymph nodes and joints, as well as production of anti-inflammatory molecules, IL-10 and TGF-β, in the joint synovial fluid. We have determined that treatment with rFc-µTP-L309C results in a significant decrease in Th1 and Th17 cells in the joints and a concomitant increase in Tregs and production of IL-10. Interestingly, the increase of Tregs is seen only in the joints; indeed, in contrast, Tregs are found to be decreased in the spleen and lymph nodes. Perhaps, this apparent dichotomy indicates that Tregs, as previously suggested [
9], are migrating from the spleen and lymph nodes into the joints to protect the joint?
Tregs play a major role in mediating the humoral response through the suppression of autoantibody production by B cells and production of anti-inflammatory mediators such as IL-10 and TGFβ [
10,
11,
12]. Nguyen et al. [
9] reported a role for Tregs in Ab-induced arthritis at several levels. First, they showed that a Treg deficiency in K/BxN mice led to more accelerated aggressive arthritis with significantly earlier auto-Ab production. They also showed that Tregs accumulated in the inflamed joints of K/BxN serum-transferred C57BL/6 mice, which suggested that Tregs actively migrate to the site of Ab-induced inflammation and control the local inflammatory process. The main ways in which these Tregs control the local inflammatory response is through the secretion of IL-10 and TGF-β [
11]. IL-10 has inhibitory effects on cells of the innate immune system through suppressing pro-inflammatory cytokine and chemokine production by activated monocytes/macrophages and neutrophils [
12], whereas TGF-β is more known for its effects on B cells such as its ability to suppress B cell survival, proliferation, differentiation into plasmablasts, and antibody secretion. Although there is some evidence to suggest that IL-10 can indirectly affect Ab secretion by B cells by modulating B cell metabolite [13], more studies are needed to determine whether this is true. In our study, rFc-µTP-L309C was able to increase the Tregs in the joints as well as IL-10. Although TGFβ was increased, this increase was not significant. Nonetheless, taken together our results support previous published work that Tregs, IL-10 and TGF-β play a significant role in the arthritis and our findings, along with decreased numbers of inflammatory Th1 and Th17 cells, can explain, at least in part, the amelioration of the endogenous arthritis by rFc-µTP-L309C in our K/BxN mouse model. How human rFc-hexamer can reduce the impact of the T-cell phenotype is uncertain; however, it may be by engaging FcγR myeloid cells to secret factors, i.e., cytokines, which impact the T-cell phenotype?
In conclusion, rFc-µTP-L309C ameliorates chronic arthritis in the K/BxN mouse model by multiple mechanisms, including affects on neutrophil infiltration into the joints and inhibition of IL-1β as previously described [
7]. In the work herein, we describe another mechanism that rFc-µTP-L309C affects, the T-cell compartment. rFc-µTP-L309C decreases inflammatory cytokines by inhibiting Th1 and Th17 cells and increases T regulatory cells and anti-inflammatory IL-10.
Funding
This study was partially funded by a research contract with CSL Behring AG. B.J.B.L. was the recipient of a Canadian Blood Services’ Graduate Fellowship Program (GFP) award. R.J.A. was a recipient of a Canadian Blood Services’ Postdoctoral Fellowship award.
Author contributions
Conceptualization, B.J.B.L., S.C., R.S., F.K. and D.R.B.; Methodology, B.J.B.L., S.C., R.J.A., and D.R.B.; Validation, B.J.B.L., S.C., and R.J.A.; Formal Analysis, B.J.B.L., R.J.A., B.B. and D.R.B.; Investigation, B.J.B.L. and R.J.A.; Resources, R.S., F.K. and D.R.B.; Data Curation, B.J.B.L. and R.J.A.; Writing – Original Draft Preparation, B.J.B.L and R.J.A.; Writing – Review and Editing, B.J.B.L., S.C., R.J.A., B.B., R.S., F.K. and D.R.B.; Visualization, B.J.B.L., R.J.A. and B.B.; Supervision, D.R.B.; Project Administration, D.R.B.; Funding Acquisition, D.R.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted following our institutions’ guidelines on the care and use of laboratory animals and only after approval of the protocol by the animal care committee of the University Health Network (UHN); animal use protocol AUP 1788, and after review by the St. Michael’s Hospital Unity Health Toronto Animal Care Committee (ACC); approved protocol ACC 138.
Data availability
The datasets used and/or analyzed during the current study are available form the corresponding author. All data generated or analyzed during this study are included in this publication.
Acknowledgements
We thank CSL Behring AG for their in-kind provision of the rFc-µTP-L309C used in these studies. We are also grateful to Dr. C. Benoist for the generous gift of KRN mice allowing us to breed these mice and make the K/BxN mouse model.
References
- Anthony, R.M.; Nimmerjahn, F.; Ashline, D.J.; Reinhold, V.N.; Paulson, J.C.; Ravetch, JV. Recapitulation of IVIG anti-inflammatory activity with a recombinant IgG Fc. Science 2008, 320, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Anthony, R.M.; Wermeling, F.; Karlsson, M.C.; Ravetch, J.V. Identification of a receptor required for the anti-inflammatory activity of IVIG. Proc. Nat. Acad. Sci. USA 2008, 105, 19571–19578. [Google Scholar] [CrossRef] [PubMed]
- Anthony, R.M.; Kobayashi, T.; Wermeling, F.; Ravetch, J.V. (2011). Intravenous gammaglobulin suppresses inflammation through a novel TH2 pathway. Nature 2011, 475, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.K.; Miescher, S.; Branch, D.R.; Mott, P.J.; Lazarus, A.H.; Han, D.; Maraskovsky, E.; Zuercher, A.W.; Neschadim, A.; Leontyev, D.; McKenzie, B.S. Therapeutic effect of IVIG on inflammatory arthritis in mice is dependent on the Fc portion and independent of sialylation or basophils. J. Immunol. 2014, 192, 5031–5038. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, Y.; Nimmerjahn, F.; Ravetch, J. V. Anti-inflammatory activity of immunoglobulin G resulting from Fc sialylation. Science 2006, 313, 670–673. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.J.B.; Ville, J.; Blacquiere, M.; Cen., S.; Spirig, R.; Zuercher, A.W.; Fasermann, F.; Branch, D.R. Using the K/BxN mouse model of endogenous, chronic, rheumatoid arthritis for the evaluation of potential immunoglobulin-based therapeutic agents, including IVIg and Fc-μTP-L309C, a recombinant IgG1 Fc hexamer. BMC Immunol. 2019, 20, 44. [Google Scholar] [CrossRef] [PubMed]
- Almizraq, R.J.; Frias Boligan, K.; Lewis, B.J.B.; Cen, S.; Whetstone, H.; Spirig, R.; Kasermann, F.; Campbell, I.K.; von Gunten, S.; Branch, D.R. Modulation of neutrophil function by recombinant human IgG1 Fc hexamer in the endogenous K/BxN mouse model of rheumatoid arthritis. Pharmacol. 2023, 108, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.K.; Leong, D.; Edwards, K.M.; Rayzman, V.; Ng, M.; Goldberg, G.L.; et al. Therapeutic targeting of the G-CSF receptor reduces neutrophil trafficking and joint inflammation in antibody-mediated inflammatory arthritis. J. Immunol. 2016, 197, 4392–4402. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.T.; Jacobs, J.; Mathis, D.; Benoist, C. Where FoxP3-edpendent regulatory T cells impinge on the development of inflammatory arthritis. Arthritis & Rheum. 2007, 56, 509–520. [Google Scholar]
- Fujio, K.; Okamura, T.; Sumitomo, S.; Yamamoto, K. Regulatory T cell-mediated control of autoantibody-induced inflammation. Front. Immunol. 2012, 3, 28. [Google Scholar] [CrossRef] [PubMed]
- Maloy, K.J.; Salaun, L.; Cahill, R.; Dougan, G.; Saunders, N.J.; Powrie, F. CD4+ CD25+ TR cells suppress innate immune pathology through cytokine-dependent mechanisms. J. Exp. Med. 2003, 197, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.W.; de Waal Malefyt, R.; Coffman, R.L.; O’Garra, A. Interleukin-10 and the interleukin-10 receptor. Ann. Rev. Immunol. 2001, 19, 683–765. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).