Figure 1.
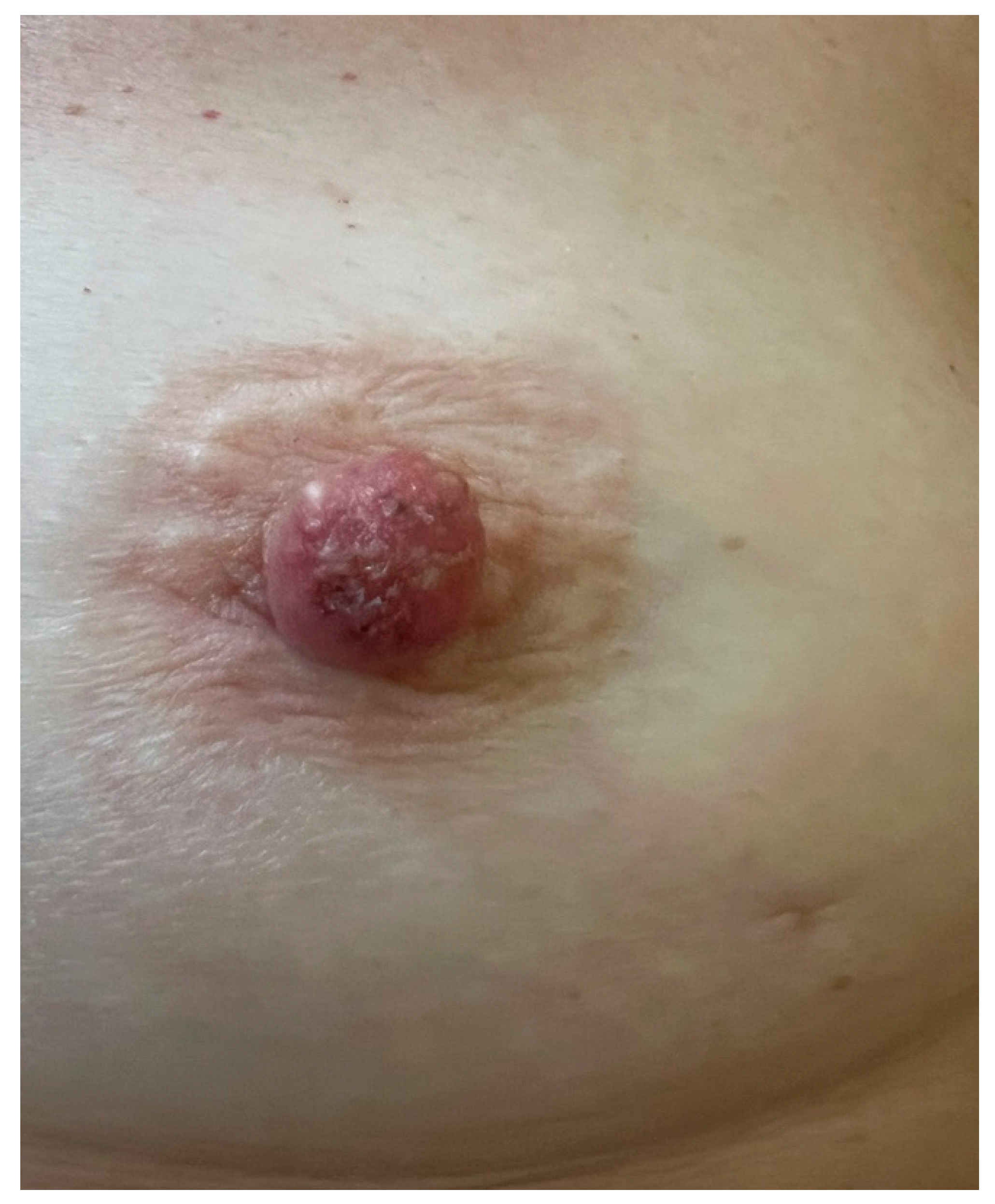
Macroscopic aspect: erythematous-crusty lesion of the left NAC with a 6-months history in a 56-year-old woman; no response to topical steroid ointment. Unilateral eczematous lesions of the NAC in postmenopausal women, especially if poorly responsive to topical treatment, should raise suspicion for malignant disease [
1,
2,
3].
Figure 1.
Macroscopic aspect: erythematous-crusty lesion of the left NAC with a 6-months history in a 56-year-old woman; no response to topical steroid ointment. Unilateral eczematous lesions of the NAC in postmenopausal women, especially if poorly responsive to topical treatment, should raise suspicion for malignant disease [
1,
2,
3].
Figure 2.
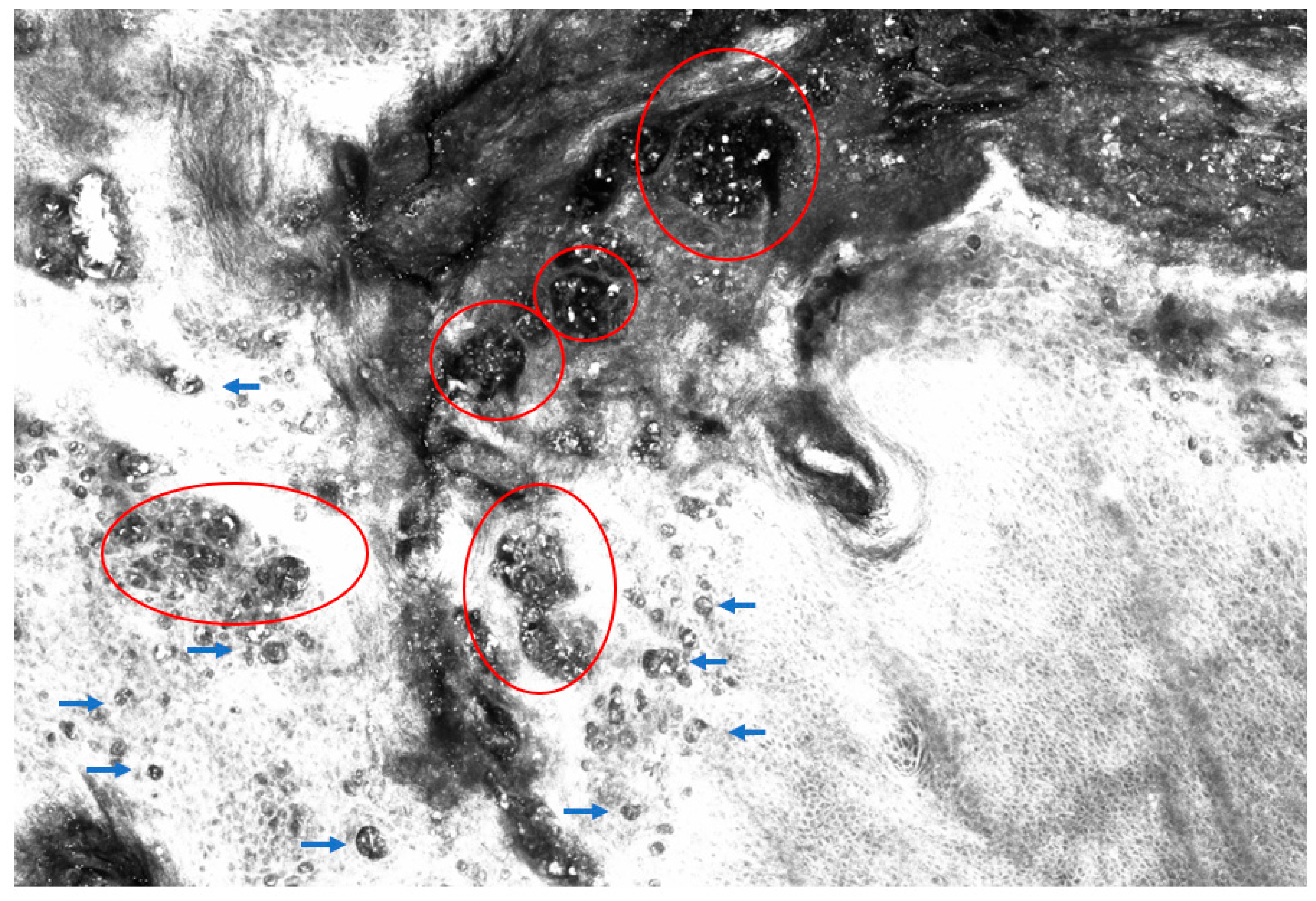
Dermoscopy showing multicolour erythematous-yellowish lesion characterized by erosions, scales, dots, blotches, pseudocysts, and multicomponent vessel pattern: these features, though not specific, are more consistent with a suspect of a malignancy rather than inflammatory disease [
4,
5,
6]. Sometimes pigmented variants, showing irregular brown pigmentation, gray dots or globules, can mimick melanoma or pigmented basal cell carcinoma, complicating differential diagnosis [
7,
8].
Figure 2.
Dermoscopy showing multicolour erythematous-yellowish lesion characterized by erosions, scales, dots, blotches, pseudocysts, and multicomponent vessel pattern: these features, though not specific, are more consistent with a suspect of a malignancy rather than inflammatory disease [
4,
5,
6]. Sometimes pigmented variants, showing irregular brown pigmentation, gray dots or globules, can mimick melanoma or pigmented basal cell carcinoma, complicating differential diagnosis [
7,
8].
Figure 3.
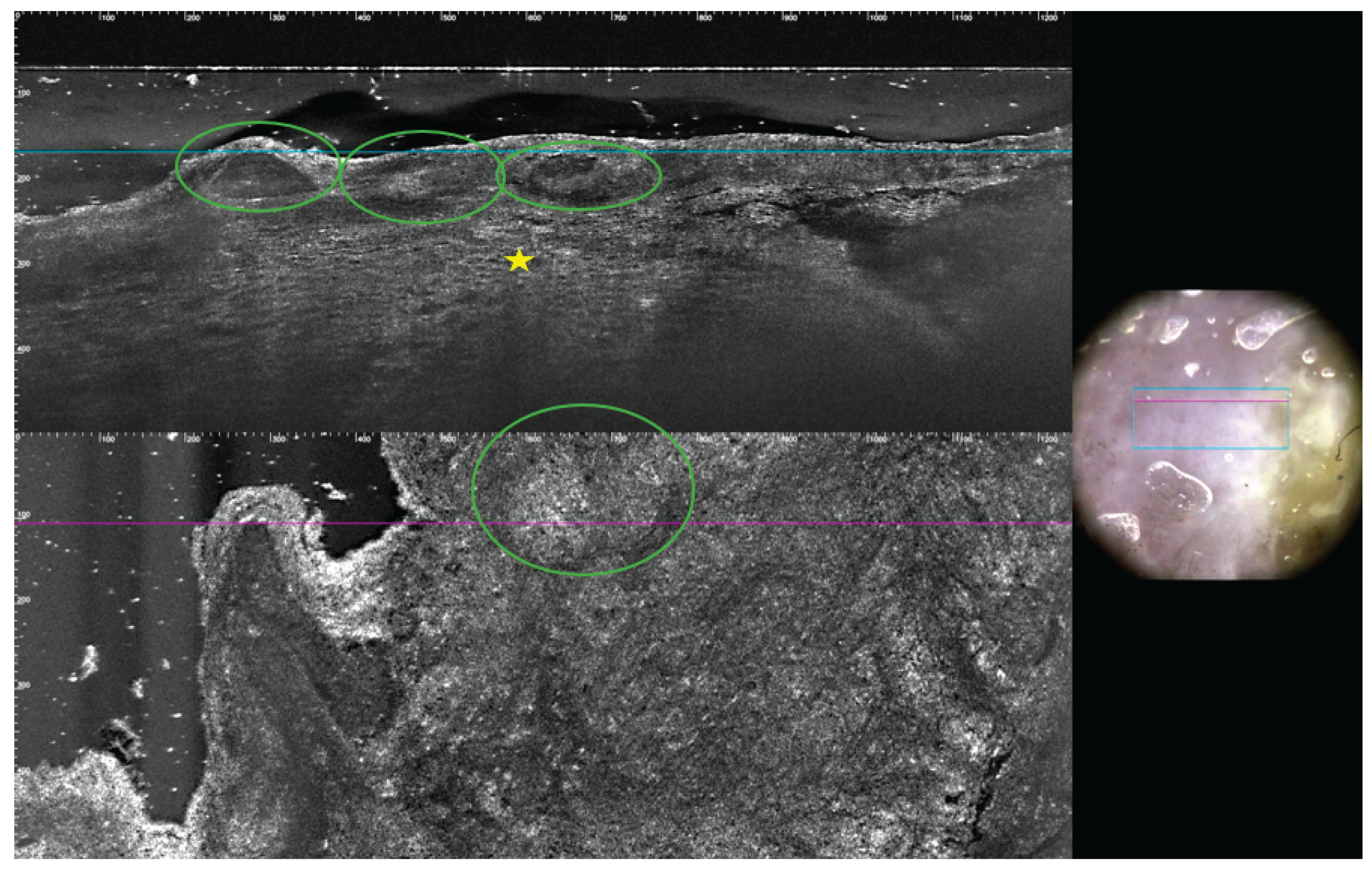
Reflectance confocal microscopy (RCM) is a non-invasive, in vivo imaging technique that enables real-time and high-resolution visualization of the epidermis and upper dermis at near-histologic resolution: by employing a near-infrared laser and detecting backscattered light, RCM allows for horizontal optical sectioning of the skin, revealing cellular and architectural details without the need for biopsy [
9,
10,
11]. In this case, normal epidermal honeycomb pattern is disrupted by the presence of big tumour nests (red circles), appearing as dark silhouettes in different size and shape; these nests are composed of hyporeflective tumour cells (Paget cells) larger than adjacent keratinocytes with abundant, pale cytoplasm and small, mildly bright nuclei (blue arrowheads).
Figure 3.
Reflectance confocal microscopy (RCM) is a non-invasive, in vivo imaging technique that enables real-time and high-resolution visualization of the epidermis and upper dermis at near-histologic resolution: by employing a near-infrared laser and detecting backscattered light, RCM allows for horizontal optical sectioning of the skin, revealing cellular and architectural details without the need for biopsy [
9,
10,
11]. In this case, normal epidermal honeycomb pattern is disrupted by the presence of big tumour nests (red circles), appearing as dark silhouettes in different size and shape; these nests are composed of hyporeflective tumour cells (Paget cells) larger than adjacent keratinocytes with abundant, pale cytoplasm and small, mildly bright nuclei (blue arrowheads).
Figure 4.
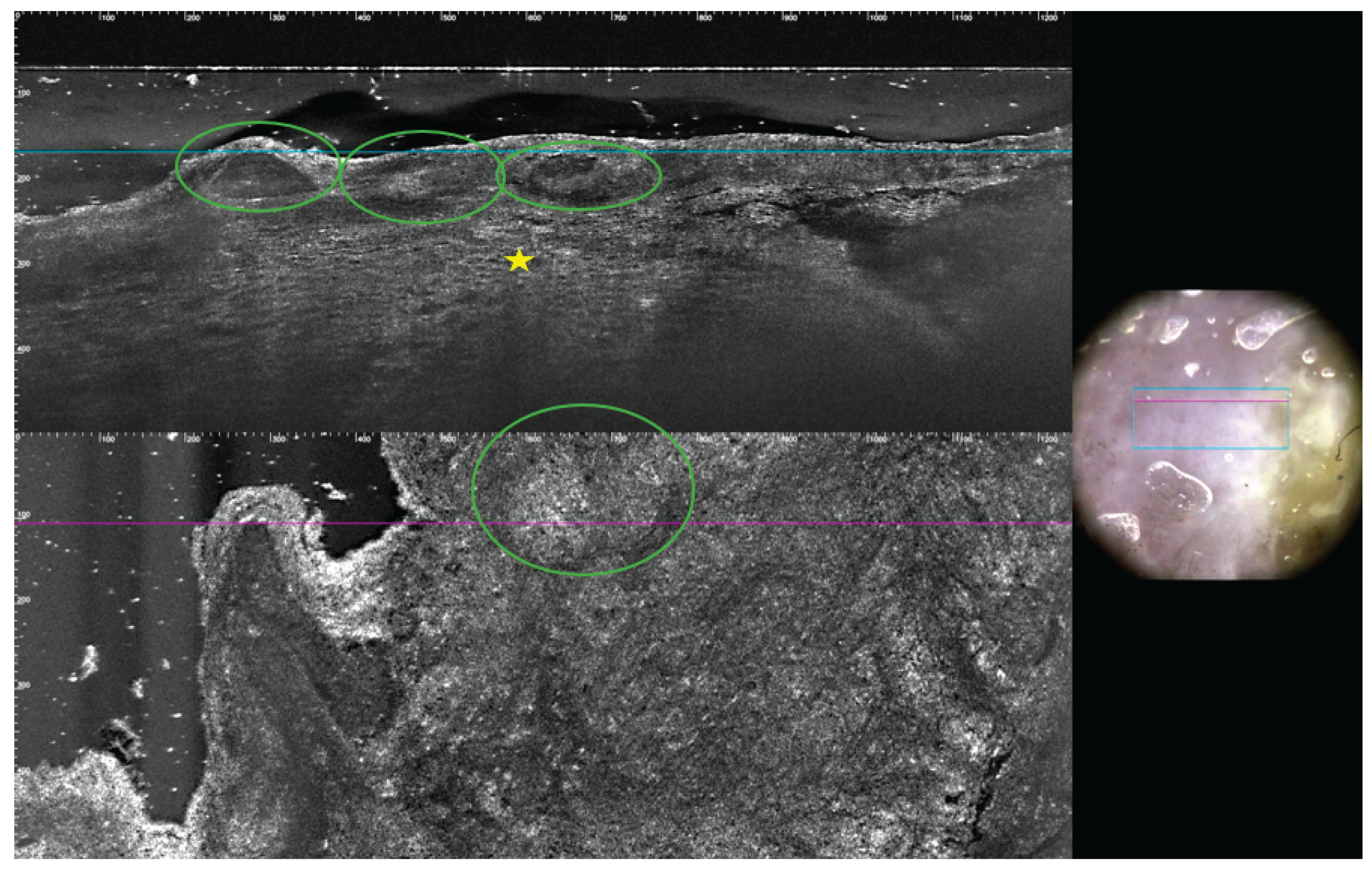
LC-OCT is a innovative non-invasive imaging technique that uses light to capture high-resolution cross-sectional images of tissues [
12]: in this patient, LC-OCT examination demonstrated the presence of pseudovescicular pattern (green circles) altering normal epidermal architecture, full of atypical cells (yellow star) with mildly bright nuclei and several atypical cell nests, even in the dermis, at transversal evaluation. After this non-invasive examination, it became evident that the patient was not affected by nipple eczema, which typically presents with intraepidermal vesicles (spongiotic pattern) filled with inflammatory cells and keratinocytes [
13,
14,
15]. Therefore, after a multidisciplinary consultation, multiple nipple biopsies were carried out: a double cluster of R4a calcifications of the left breast was discovered; one cluster was based in the retro areolar region, the other one in the lower outer quadrant (LOQ); one lymph node showing slightly thickened cortex was also noted. Both cluster of microcalcification were removed by vacuum assisted breast biopsy (VABB). Cytological examination of nipple scraping, and secretion was also performed. Nipple secretion was found to be inflammatory, nipple scraping showed isolated and loosely clustered malignant glandular cells with enlarged nuclei, prominent nucleoli and pale cytoplasm, detected among squamous cells suspicious for Paget disease. A further VABB of the LOQ was operated and a moderately differentiated invasive breast carcinoma of no special type was rule out. The lesion resulted estrogen receptor (ER) negative, progesterone receptor (PgR) negative, HER-2 positive and Ki-67 ranged 25%. Our breast multidisciplinary team chose a simple mastectomy as the treatment of choice: histological examination of this sample confirmed the presence of infiltrative carcinoma of the LOQ with adjacent ductal carcinoma in situ (DCIS) G2-G3 and the presence of DCIS G2-G3 of the large ducts behind the nipple and Paget disease of the nipple; a micro metastatic lymph node was diagnosed by molecular analysis one step nucleic acid analysis amplification (OSNA). The preliminary dermatological analysis of the NAC was very helpful to make the best therapeutic decision before confirming: these technologies provide high-resolution images of tissue architecture and cellular abnormalities, aiding in early detection and, in some cases, reducing the need for invasive procedures or accelerating need for biopsy [
14,
15]. However, histological confirmation remains essential. In our case, conventional instrumental investigations were negative, and cytology was nonspecific, so multiple targeted biopsies were required to confirm what had been immediately highlighted by high-resolution dermatological techniques.
Figure 4.
LC-OCT is a innovative non-invasive imaging technique that uses light to capture high-resolution cross-sectional images of tissues [
12]: in this patient, LC-OCT examination demonstrated the presence of pseudovescicular pattern (green circles) altering normal epidermal architecture, full of atypical cells (yellow star) with mildly bright nuclei and several atypical cell nests, even in the dermis, at transversal evaluation. After this non-invasive examination, it became evident that the patient was not affected by nipple eczema, which typically presents with intraepidermal vesicles (spongiotic pattern) filled with inflammatory cells and keratinocytes [
13,
14,
15]. Therefore, after a multidisciplinary consultation, multiple nipple biopsies were carried out: a double cluster of R4a calcifications of the left breast was discovered; one cluster was based in the retro areolar region, the other one in the lower outer quadrant (LOQ); one lymph node showing slightly thickened cortex was also noted. Both cluster of microcalcification were removed by vacuum assisted breast biopsy (VABB). Cytological examination of nipple scraping, and secretion was also performed. Nipple secretion was found to be inflammatory, nipple scraping showed isolated and loosely clustered malignant glandular cells with enlarged nuclei, prominent nucleoli and pale cytoplasm, detected among squamous cells suspicious for Paget disease. A further VABB of the LOQ was operated and a moderately differentiated invasive breast carcinoma of no special type was rule out. The lesion resulted estrogen receptor (ER) negative, progesterone receptor (PgR) negative, HER-2 positive and Ki-67 ranged 25%. Our breast multidisciplinary team chose a simple mastectomy as the treatment of choice: histological examination of this sample confirmed the presence of infiltrative carcinoma of the LOQ with adjacent ductal carcinoma in situ (DCIS) G2-G3 and the presence of DCIS G2-G3 of the large ducts behind the nipple and Paget disease of the nipple; a micro metastatic lymph node was diagnosed by molecular analysis one step nucleic acid analysis amplification (OSNA). The preliminary dermatological analysis of the NAC was very helpful to make the best therapeutic decision before confirming: these technologies provide high-resolution images of tissue architecture and cellular abnormalities, aiding in early detection and, in some cases, reducing the need for invasive procedures or accelerating need for biopsy [
14,
15]. However, histological confirmation remains essential. In our case, conventional instrumental investigations were negative, and cytology was nonspecific, so multiple targeted biopsies were required to confirm what had been immediately highlighted by high-resolution dermatological techniques.
Author Contributions
All authors have read and approved the final manuscript. All authors contributed equally to this work.
Informed Consent Statement
Written consent for the publication of patient photographs or other identifiable material was obtained by the authors and attested to at the time of article submission to the journal stating that patient gave her consent with the understanding that this information may be publicly available.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MPD |
Mammary Paget disease |
| LC-OCT |
Line-field confocal-optical coherence tomography |
| RCM |
Reflectance confocal microscopy |
| NAC |
Nipple areola complex |
| DCIS |
Ductal carcinoma in situ |
| IDC |
Invasive ductal carcinoma |
| LOQ |
Lower outer quadrant |
| VABB |
Vacuum assisted breast biopsy |
| PgR |
Progesterone Receptor |
| OSNA |
One step nucleic acid analysis amplification |
References
- Markarian, S. & Holmes, D. R. Mammary Paget’s Disease: An Update. Cancers (Basel) 14, 2422 (2022).
- Scott-Emuakpor, R. et al. Mammary Paget’s Disease Mimicking Benign and Malignant Dermatological Conditions: Clinical Challenges and Diagnostic Considerations. Cureus (2024) doi:10.7759/cureus.65378.
- Hudson-Phillips, S., Cox, K., Patel, P. & Al Sarakbi, W. Paget’s disease of the breast: diagnosis and management. Br J Hosp Med 84, 1–8 (2023). [CrossRef]
- Apalla, Z. et al. Dermoscopic features of mammary Paget’s disease: a retrospective case-control study by the International Dermoscopy Society. Journal of the European Academy of Dermatology and Venereology 33, 1892–1898 (2019).
- Errichetti, E., Avellini, C., Pegolo, E. & De Francesco, V. Dermoscopy as a Supportive Instrument in the Early Recognition of Erosive Adenomatosis of the Nipple and Mammary Paget’s Disease. Ann Dermatol 29, 365 (2017).
- Crignis, G. S. N. de, Abreu, L. de, Buçard, A. M. & Barcaui, C. B. Polarized dermoscopy of mammary Paget disease. An Bras Dermatol 88, 290–292 (2013).
- D’Erme, A. M. et al. Pigmentary Mammary Paget Disease: clinical, dermoscopical and histological challenge. Dermatol Reports (2021). [CrossRef]
- Yanagishita, T. et al. Pigmented mammary Paget disease mimicking melanoma on dermatoscopy. J Am Acad Dermatol 64, e114–e116 (2011).
- Shahriari, N., Grant-Kels, J. M., Rabinovitz, H., Oliviero, M. & Scope, A. Reflectance confocal microscopy. J Am Acad Dermatol 84, 1–14 (2021).
- Hofmann-Wellenhof, R. et al. Reflectance Confocal Microscopy—State-of-Art and Research Overview. Semin Cutan Med Surg 28, 172–179 (2009).
- Levine, A. & Markowitz, O. Introduction to reflectance confocal microscopy and its use in clinical practice. JAAD Case Rep 4, 1014–1023 (2018).
- Cinotti, E. et al. Diagnostic Accuracy of Line-Field Confocal Optical Coherence Tomography for the Diagnosis of Skin Carcinomas. Diagnostics 13, 361 (2023).
- Richtig, E., Ahlgrimm-Siess, V., Arzberger, E. & Hofmann-Wellenhof, R. Noninvasive differentiation between mamillary eczema and Paget disease by in vivo reflectance confocal microscopy on the basis of two case reports. British Journal of Dermatology 165, 440–441 (2011).
- Dubois, A. et al. Line-field confocal optical coherence tomography for high-resolution noninvasive imaging of skin tumors. J Biomed Opt 23, 1 (2018).
- Donelli, C. et al. Line-Field Confocal Optical Coherence Tomography for the Diagnosis of Skin Carcinomas: Real-Life Data over Three Years. Current Oncology 30, 8853–8864 (2023).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).