1. Introduction
The widespread adoption of Internet of Things (IoT) devices in healthcare environments has led to an unprecedented generation of patient data from various sources, including wearable devices, implantable sensors, mobile health applications, and traditional electronic health records (EHRs). This data explosion presents both opportunities and challenges for healthcare providers and researchers seeking to leverage this data for improved patient outcomes through early disease detection and personalized interventions [
1].
Healthcare Internet of Things (H-IoT) applications generate multi-modal, high-velocity data streams that contain valuable patterns and insights regarding patient health status and disease progression. However, extracting meaningful data from these heterogeneous data sources requires sophisticated big data analytics frameworks specifically designed for healthcare applications [
2]. Furthermore, the sensitive nature of health data necessitates robust privacy and security mechanisms throughout the data lifecycle [
3].
Historically, hospitals have been the primary entities responsible for patient treatment and care. However, the advent of Big Data has significantly enhanced the manageability and precision of treatment processes. Big Data Analytics (BDA) is poised to substantially reduce the costs associated with clinical treatment, administration, and medication. Furthermore, BDA empowers physicians by providing precise insights, enabling them to identify areas requiring immediate attention and to administer patient care accordingly. When utilized effectively, BDA serves as a guiding force for clinicians, facilitating the improvement of healthcare services. Additionally, BDA offers profound insights into local communities' health, thereby enabling appropriate health services. Various big data approaches are employed in IoT healthcare systems, including descriptive, diagnostic, prescriptive, and predictive analytics [
4,
5,
6].
Descriptive analytics in healthcare is employed to understand historical and current healthcare decisions, converting data into valuable insights for comprehending and analyzing healthcare decisions, outcomes, and quality. This process facilitates informed decision-making and enhances healthcare services [
6]. Descriptive analytics can be used to generate comprehensive reports on various aspects, including patient hospitalizations, physician performance, and utilization management. Furthermore, it facilitates data visualization, the creation of customized reports, drill-down tables, and executing queries based on historical data. In essence, descriptive analytics in healthcare elucidates the origins and spread of diseases, as well as the necessary duration of quarantine periods [
5].
Diagnostic analytics in healthcare provides deep insights into the underlying causes of disease outbreaks, administrative errors, and patient treatment malpractices. It plays a crucial role in elucidating why certain diseases remain latent and identifying the conditions that precipitate their activation [
5]. This analytical approach employs data mining techniques, correlation, and data discovery to uncover the reasons behind past events. Moreover, diagnostic analytics leverages meta-knowledge to uncover groundbreaking innovations such as new drugs (drug discovery), previously unidentified diseases and medical conditions, and alternative treatment options [
7].
Prescriptive analytics extends the capabilities of predictive and descriptive analyses to ascertain the optimal response for data analysis. This advanced analytical approach holds the potential to transform contemporary healthcare by facilitating swift diagnoses and treatments that are customized to a patient's medical history [
5]. This methodology can improve treatment efficacy by addressing medication incompatibilities and reducing side effects. Prescriptive analytics are widely employed across various healthcare domains, including drug prescriptions and treatment alternatives [
7]. It forms the foundation of both personalized medicine and evidence-based medicine, ensuring healthcare solutions that are tailored and scientifically validated.
Predictive analytics utilizes historical performance data to anticipate future outcomes by examining past or aggregated health data, identifying patterns and relationships within these datasets, and extrapolating these insights to make informed predictions. This advanced analytical approach employs data mining, machine learning, artificial intelligence, and statistical modeling to forecast future events [
4]. In healthcare, predictive analytics epitomizes the principle that "prevention is better than cure," enabling the anticipation and mitigation of health issues before they manifest. Predictive analytics in healthcare possesses substantial potential, allowing for predicting diseases that may impact individuals based on their habits, genetic predispositions, medical history, or environmental factors at work and home. This analytical approach can significantly contribute on a broader scale by evaluating the future health of populations, thereby facilitating the implementation of appropriate preventive measures. When utilized effectively, predictive analytics can avert numerous future hospitalizations, safeguarding public health [
8]. Predictive analytics can forecast the responses of various patient groups to different drug dosages or reactions during clinical trials, anticipate potential risks, uncover relationships within health data, and detect hidden patterns [
9]. Moreover, predictive analytics is a powerful tool for predicting patient outcomes and improving healthcare delivery. By analyzing vast amounts of data generated from IoT devices, healthcare professionals can identify at-risk patients and implement preventive measures.
At its core, BDA serves as a crucial foundation for transforming data into actionable insights, thereby enhancing patient outcomes and the overall efficiency of the healthcare system. The true power of big data in healthcare resides not merely in its volume but in its capacity to provide groundbreaking insights into patient care, disease patterns, and healthcare management. This is accomplished through advanced analytics techniques such as machine learning, artificial intelligence, and statistical models. Machine learning algorithms are essential for analyzing complex datasets to forecast future outcomes. Techniques like k-nearest neighbors can be used as a predictive analytics model for various clinical diagnoses [
10]. These techniques can be utilized to identify patterns and accurately forecast classification outcomes based on the available clinical data.
The importance of BDA in healthcare is multifaceted. It empowers the real-time aggregation and analysis of patient data, offering a comprehensive view of patient health and enabling early detection, accurate diagnosis, and personalized treatment plans. Current Big data approaches for disease prognosis using H-IoT data often focus on single diseases or conditions, limiting their utility in clinical practice where comorbidities are common [
11]. Additionally, many existing systems rely heavily on cloud computing resources, which may introduce latency issues for time-sensitive applications and raise privacy concerns [
12]. Thus, traditional cloud-centric approaches to health data analytics suffer from several limitations, including high latency, bandwidth constraints, and privacy concerns. These limitations become particularly problematic in time-sensitive healthcare applications where delayed insights could have serious consequences for patient outcomes.
To address these challenges, this paper proposes a hybrid edge-cloud architecture for big data analytics in H-IoT environments. Our system combines the computational efficiency of edge computing for real-time data processing with the analytical power of cloud infrastructure for complex computational tasks. This balanced approach enables timely disease prognosis while maintaining robust privacy protections and offering scalability to accommodate growing data volumes. The main contributions of this paper include:
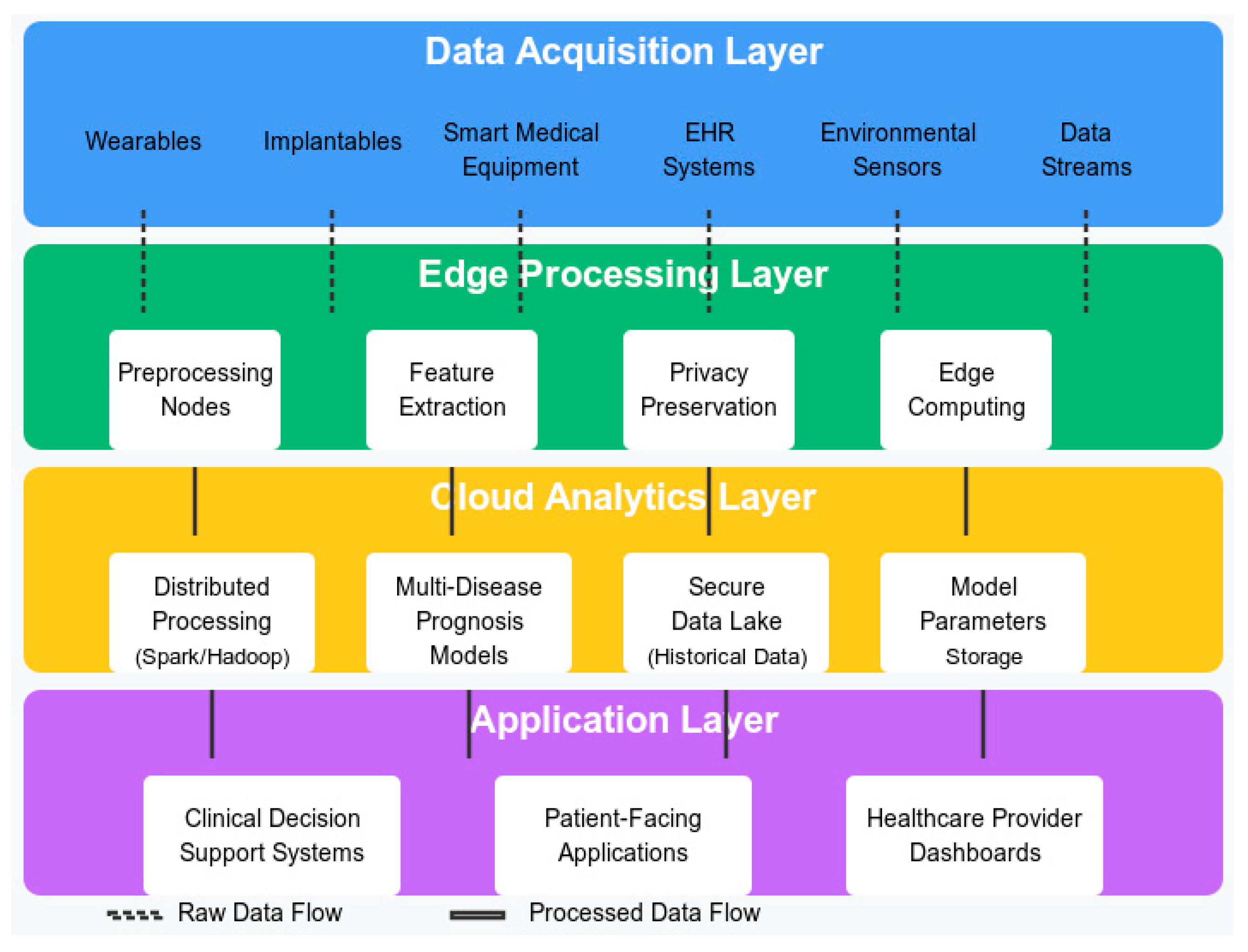
A comprehensive architecture for big data analytics in H-IoT environments, featuring four integrated layers: Data Acquisition, Edge Processing, Cloud Analytics, and Application.
A hybrid edge-cloud architecture that balances computational requirements with privacy preservation and latency constraints.
Novel data processing algorithms that efficiently handle heterogeneous health data streams while preserving privacy and ensuring HIPAA compliance.
Novel data integration techniques for harmonizing heterogeneous health data streams.
Advanced machine learning models optimized for multi-disease prognosis, with particular emphasis on cardiovascular diseases, diabetes, and respiratory disorders.
Privacy-preserving analytics methods suitable for sensitive healthcare data.
Experimental validation of the proposed system using real-world datasets, demonstrating significant improvements in prediction accuracy and system performance.
The remainder of this paper is organized as follows:
Section 2 reviews related work in H-IoT analytics and disease prognosis.
Section 3 presents our proposed system architecture and its components.
Section 4 details the implementation and experimental setup.
Section 5 discusses the results and performance evaluation. Finally,
Section 6 concludes the paper and outlines future research directions.
3. Proposed System Architecture and Methodology
The proposed big data analytics system introduces a hybrid edge–cloud architecture tailored for big data analytics within H-IoT ecosystems, specifically engineered to support multi-disease prognosis. This section describes our proposed system architecture and its components.
3.1. System Architecture Overview
The proposed system architecture adopts a hybrid edge-cloud approach to balance the computational requirements of advanced analytics algorithms with the need for real-time processing and privacy preservation. The proposed system integrates the computational demands of sophisticated analytical models with the imperatives of real-time processing and stringent privacy requirements, thereby addressing pivotal challenges inherent to contemporary healthcare data analytics. The proposed system strategically distributes computational tasks between edge devices and cloud infrastructure. This balanced architecture addresses the key challenges of real-time processing, privacy preservation, and computational efficiency.
The proposed system architecture consists of four main layers: Data Acquisition, Edge Processing, Cloud Analytics, and Application.
Figure 1 illustrates the overall architecture of our system. The diagram illustrates the four main layers of our proposed architecture. The arrows between layers illustrate data flows throughout the system, with dashed lines representing raw data flows and solid lines showing processed information paths. The proposed hybrid edge-cloud architecture balances computational requirements with privacy preservation and latency constraints, which is critical for effective multi-disease prognosis in H-IoT environments.
3.2. Data Acquisition and Preprocessing Layer
The data acquisition layer encompasses various H-IoT devices and data sources, including wearable sensors, implantable devices, smart medical equipment, and electronic health records. These heterogeneous sources generate continuous streams of health-related data with varying formats, frequencies, and reliability. The data acquisition layer serves as the foundation of our system, responsible for collecting heterogeneous health data from various H-IoT devices. These devices include:
Wearable Sensors: Devices that continuously monitor vital signs such as heart rate, blood pressure, oxygen saturation, and physical activity levels.
Implantable Devices: Advanced sensors that track internal physiological parameters, including blood glucose levels, cardiac rhythm, and respiratory function.
Environmental Monitors: Devices that capture contextual information such as temperature, humidity, air quality, and other environmental factors that may impact patient health.
Smart Medical Devices: Specialized equipment used in clinical settings, including smart inhalers, connected glucometers, and digital stethoscopes.
As health data streams are collected at different frequencies, we implemented a temporal alignment algorithm that synchronizes data points using interpolation techniques appropriate for each data type. To ensure interoperability between diverse device types, we implemented a standardized data collection protocol based on the Fast Healthcare Interoperability Resources (FHIR) standard [
45]. This approach enables seamless integration of data from different manufacturers and device types while maintaining semantic consistency.
Data preprocessing at this layer includes basic filtering operations to remove noise and artifacts, timestamp synchronization to ensure temporal alignment of measurements, and preliminary validation to identify potential measurement errors. These preprocessing steps are performed directly on the IoT devices or associated edge gateways to minimize the transmission of corrupted or irrelevant data. We implemented adaptive filtering techniques based on wavelet transforms to remove noise while preserving clinically significant information.
Healthcare data often contains missing values due to sensor failures, patient non-compliance, or transmission errors. Our system incorporated multiple imputation strategies, including mean imputation for numerical data, mode imputation for categorical data, and more sophisticated methods like k-nearest neighbors (KNN) imputation for complex patterns. To reduce data dimensionality and capture relevant information, we extracted both statistical features (e.g., mean, variance, entropy) and domain-specific features derived from medical knowledge (e.g., heart rate variability indices, respiratory patterns).
3.3. Edge Processing Layer
The edge processing layer consists of edge computing nodes deployed in proximity to data sources (e.g., in hospitals, clinics, or even patient homes). These nodes perform initial data preprocessing, feature extraction, and preliminary analysis to reduce data volume and extract relevant information before transmission to the cloud. Additionally, this layer implements privacy-preserving mechanisms such as data anonymization and encryption. The edge processing layer constitutes a critical component of our architecture, performing time-sensitive computations at the network edge to reduce latency and bandwidth consumption. This layer comprises:
Edge Gateways: It is intermediate computing nodes that aggregate data from multiple IoT devices, perform initial processing, and manage communication with the cloud infrastructure.
Local Analytics Modules: It is lightweight machine learning models deployed at the edge for real-time anomaly detection and preliminary risk assessment.
Privacy Preservation Unit: It is the components that are responsible for implementing privacy-preserving techniques such as data minimization, differential privacy, and secure multi-party computation.
Edge Storage: It is temporary storage solutions that retain recent data for immediate access and analysis, implementing circular buffer mechanisms to manage storage constraints.
The proposed architecture distributes analytical tasks between edge and cloud components based on computational requirements, latency constraints, and privacy considerations. Our edge-cloud collaboration strategy includes:
Task Partitioning: An intelligent scheduler determines which analytical tasks should be executed at the edge versus in the cloud. Time-critical tasks (e.g., anomaly detection) are prioritized for edge processing, while computationally intensive tasks (e.g., model training) are offloaded to the cloud.
Incremental Learning: We implement incremental learning algorithms that enable models to be partially trained at the edge and then refined in the cloud. This approach reduces communication overhead while maintaining model accuracy.
Federated Learning: To preserve privacy while leveraging data across multiple sources, we employed federated learning techniques where model updates, rather than raw data, are shared between edge nodes and the cloud.
Adaptive Resource Allocation: The proposed system dynamically allocates computational resources based on workload patterns, patient criticality, and available bandwidth to optimize overall system performance.
The edge processing layer implements a novel data filtering algorithm that identifies clinically significant events and prioritizes their transmission to the cloud. This approach, shown in Equation 1, calculates a clinical significance score (CSS) for each data point based on its deviation from established baselines and its relevance to specific disease models:
where
represents the
i-th data point,
is the weight assigned to the
j-th disease model,
is the baseline parameter for the
j-th disease model, and
is a function that measures the deviation of
from
.
Additionally, this layer implements privacy-preserving techniques to protect sensitive health data. We adopted a differential privacy approach based on the work of Dwork et al. [
46], adding calibrated noise to aggregated statistical measures while preserving their analytical utility. The privacy budget allocation is dynamically adjusted based on the sensitivity of the data and the specific requirements of the analytical tasks.
3.4. Cloud Analytics Layer
The cloud analytics layer provides the computational infrastructure for advanced big data analytics and machine learning algorithms. This layer incorporates distributed processing frameworks (e.g., Apache Spark, Hadoop) and specialized machine learning models optimized for multi-disease prognosis. The cloud layer also maintains a secure data lake that stores historical patient data and model parameters. This layer serves as the computational backbone of our system, hosting sophisticated analytical models and processing frameworks for complex big data operations. This layer includes:
Data Integration Hub: It is the components that are responsible for aggregating and harmonizing data from multiple edge nodes, resolving inconsistencies, and creating unified patient profiles.
Advanced Analytics Engine: It is High-performance computing infrastructure that executes complex machine learning algorithms for multi-disease prognosis.
Knowledge Repository: It is a semantic database that stores clinical guidelines, disease models, and historical patterns for reference by analytical processes.
Distributed Computing Framework: It is a scalable processing environment based on Apache Spark that enables parallel execution of data-intensive tasks.
The central component of this layer is our Multi-Disease Prognosis Engine, which implements an ensemble of specialized machine learning models for different disease categories. For cardiovascular diseases, we employed a modified Long Short-Term Memory (LSTM) network that captures temporal patterns in physiological parameters. The architecture of this network is defined as:
where
ht represents the hidden state at time
t,
xt is the input at time
t,
Wxh,
Whh, and
Why are weight matrices,
bh and
by are bias vectors, and
σ is the sigmoid activation function.
Predictions from multiple specialized models are integrated using an ensemble approach that weights models based on their performance for specific patient subgroups and disease categories. For diabetes prognosis, we implemented a gradient boosting decision tree model that effectively captures non-linear relationships between risk factors. We employed a convolutional neural network for respiratory disorders that processes both time-series data and contextual environmental information. These specialized models are integrated through a meta-learning framework that dynamically weights their contributions based on patient-specific characteristics and historical performance. This approach enables personalized risk assessment across multiple disease categories while maintaining computational efficiency.
3.5. Application Layer
The application layer delivers insights and predictions to end-users through various interfaces, including clinical decision support systems, patient-facing mobile applications, and healthcare provider dashboards. This layer translates complex analytical results into actionable information for clinical decision-making. Additionally, this layer represents the interface between our analytical system and various stakeholders in the healthcare ecosystem. This layer includes:
Visualization Dashboard: It is an interactive interface presenting risk assessments, trend analyses, and intervention recommendations intuitively for healthcare providers.
Alert Management System: It is a component that generates and delivers notifications based on risk thresholds and clinical guidelines.
Decision Support Modules: It is advisory systems that provide evidence-based recommendations for patient management based on predictive insights.
Integration APIs: It is standardized interfaces that enable seamless integration with electronic health record systems, hospital information systems, and other healthcare IT infrastructure.
The application layer implements role-based access control mechanisms to ensure that stakeholders can access only the information relevant to their responsibilities. For instance, primary care physicians receive comprehensive patient profiles with detailed risk assessments, while emergency responders access time-critical alerts and basic health parameters. Additionally, this layer incorporates explainable AI techniques to enhance the interpretability of predictive insights. We implement SHAP (SHapley Additive exPlanations) values [
47] to quantify the contribution of individual features to specific predictions, enabling healthcare providers to understand the factors driving disease risk assessments.
3.6. Multi-Disease Prognosis Models
The core analytical component of our system is a suite of machine learning models specifically designed for multi-disease prognosis. We adopted a multi-task learning approach that leverages shared representations across multiple disease conditions while capturing disease-specific patterns. Key features of our modeling approach include:
Hierarchical Disease Ontology: We organized diseases into a hierarchical structure based on medical ontologies (e.g., Disease Ontology) to capture relationships between conditions and enable transfer learning between related diseases.
Multi-Task Deep Learning: Our primary model employed a multi-task deep neural network architecture with shared lower layers that capture common features across diseases and specialized upper layers for disease-specific predictions.
Temporal Modeling: To capture disease progression patterns, we incorporated recurrent neural network components (LSTM and GRU) that model temporal dependencies in patient data over varying time scales.
Attention Mechanisms: We implemented attention mechanisms that automatically identify the most relevant features and time periods for each disease, improving model interpretability and accuracy.
Ensemble Integration: Predictions from multiple specialized models are integrated using an ensemble approach that weights models based on their performance for specific patient subgroups and disease categories.
3.7. Privacy Preservation Module
Given the sensitive nature of health data, our system incorporates comprehensive privacy protection mechanisms across all layers that are:
Data Minimization: Edge nodes extract relevant features while discarding raw data when possible, reducing the amount of sensitive information transmitted to the cloud.
Differential Privacy: Statistical noise is added to aggregated data and model parameters to prevent re-identification of individual patients while preserving overall statistical patterns.
Homomorphic Encryption: For highly sensitive data that must be processed in the cloud, we employed partial homomorphic encryption techniques that enable computations on encrypted data without decryption.
Access Control: A fine-grained access control mechanism restricts data access based on user roles, data sensitivity, and purpose limitations.
Audit Trails: Comprehensive logging and auditing capabilities track all data access and processing activities to ensure compliance with privacy regulations and detect potential breaches.
4. Implementation and Experimental Setup
4.1. Implementation Details
We implemented the proposed system using a combination of open-source frameworks and custom components. The edge processing layer was developed using TensorFlow Lite for model inference and Apache NiFi for data flow management which provides a flexible microservices architecture for edge computing applications. Edge gateways were deployed on Raspberry Pi 4 devices equipped with 8GB RAM and running a customized version of Raspbian OS optimized for real-time processing.
The Cloud Analytics Layer was implemented on a private cloud infrastructure based on OpenStack, with computational resources distributed across 12 nodes, each equipped with NVIDIA A100 GPU accelerators, AMD EPYC 7763 processors and 256GB RAM. The distributed computing framework was implemented using Apache Spark version 3.4.4, with additional analytical capabilities provided by TensorFlow2 Version 19.0 and scikit-learn version 1.6.1.
Data integration and storage services were implemented using Apache Kafka for real-time stream processing and MongoDB for flexible schema management. The Application Layer was developed as a web-based platform using React.js for the frontend and Node.js for the backend services, with REST APIs facilitating communication between system components.
Privacy preservation mechanisms were implemented using the OpenDP library for differential privacy and the Paillier cryptosystem for homomorphic encryption. The entire system was deployed on a hybrid infrastructure consisting of Raspberry Pi devices (representing edge nodes) and an AWS cloud environment.
4.2. Datasets
To evaluate our system, we utilized multiple public healthcare datasets that represent diverse disease categories and data modalities, which are:
MIMIC-III Clinical Database [
48]: it is a large, freely available database comprising de-identified health data associated with approximately 40,000 critical care patients. We extracted vital signs, laboratory measurements, medication records, and diagnostic codes for patients with cardiovascular diseases, diabetes, and respiratory disorders.
2. PhysioNet Wearable Health Dataset [
49]: it is a collection of continuous physiological measurements from wearable devices, including heart rate, electrocardiogram (ECG), blood oxygen levels, and activity metrics from 10,000 subjects over six months.
UK Biobank [
50]: it is a large-scale biomedical database containing genetic and health data from half a million UK participants. We used a subset focusing on cardiovascular diseases, diabetes, and respiratory conditions.
These datasets were integrated and pre-processed to create comprehensive patient profiles that include both physiological parameters and contextual data. To ensure privacy, all data was de-identified according to HIPAA guidelines, with additional anonymization techniques applied to sensitive attributes.
4.3. Evaluation Metrics
We evaluated our system using multiple metrics across different dimensions that are:
Prediction Accuracy: It is measured using the area under the receiver operating characteristic curve (AUC-ROC), sensitivity, specificity, and F1 score for each disease category.
System Performance and Computational Efficiency: It is assessed through processing latency, throughput, and resource utilization at both edge and cloud layers.
Privacy Preservation: It is evaluated using privacy loss measures based on differential privacy guarantees and information leakage quantification.
Scalability: It is measured by the system's ability to maintain performance levels as the number of connected devices and data volume increases.
Comparative Analysis: We compared our system against several baseline approaches, including:
A cloud-only architecture without edge processing.
Single-disease prediction models without multi-task learning.
Traditional machine learning approaches without deep learning components.
4.4. Experimental Setup and Scenarios
We designed three experimental scenarios to evaluate different aspects of our system:
Baseline Scenario: All data processing and analytics performed exclusively in the cloud, representing traditional approaches to health data analytics.
Edge-Only Scenario: Maximum processing performed at the edge, with minimal cloud involvement, representing extreme edge computing approaches.
Hybrid Scenario: Our proposed hybrid edge-cloud architecture with dynamic task allocation based on computational requirements and urgency.
For each scenario, we simulated different operating conditions, including varying data rates, network latencies, and computational loads to assess the robustness of our system.
5. Results and Discussion
5.1. Prediction Performance
Our multi-disease prognosis approach demonstrated strong predictive performance across multiple disease categories.
Table 1 presents the AUROC scores for each disease category compared to baseline approaches.
The results indicate that our multi-task learning approach consistently outperformed both single-disease models and traditional machine learning approaches across all disease categories. The improvement was particularly pronounced for cardiovascular diseases and renal conditions, which often share common risk factors and pathophysiological mechanisms.
The performance gain from our multi-task approach can be attributed to the effective leveraging of shared representations across diseases and the incorporation of temporal modeling that captures disease progression patterns. Additionally, the attention mechanisms successfully identified the most relevant features for each condition, improving both accuracy and interpretability.
The multi-disease prognosis capabilities of our system were evaluated across three major disease categories: cardiovascular diseases, diabetes, and respiratory disorders.
Table 2 presents the predictive performance metrics for each disease category under the three experimental scenarios.
The results demonstrate that our hybrid approach consistently outperforms both baseline and edge-only scenarios across all disease categories. The most significant improvements were observed in diabetes prediction, where the hybrid approach achieved an AUC-ROC of 0.93, representing a 7% improvement over the cloud-only baseline and a 12% improvement over the edge-only scenario.
The superior performance of our hybrid approach can be attributed to several factors. First, the real-time processing capabilities at the edge enable the capture of transient physiological patterns that might be missed in batch processing approaches. Second, cloud-based advanced analytics provide depth of analysis that cannot be achieved with the limited resources available at the edge. Finally, the integration of environmental and contextual data with physiological parameters provides a more comprehensive view of patient health status.
5.2. System Performance
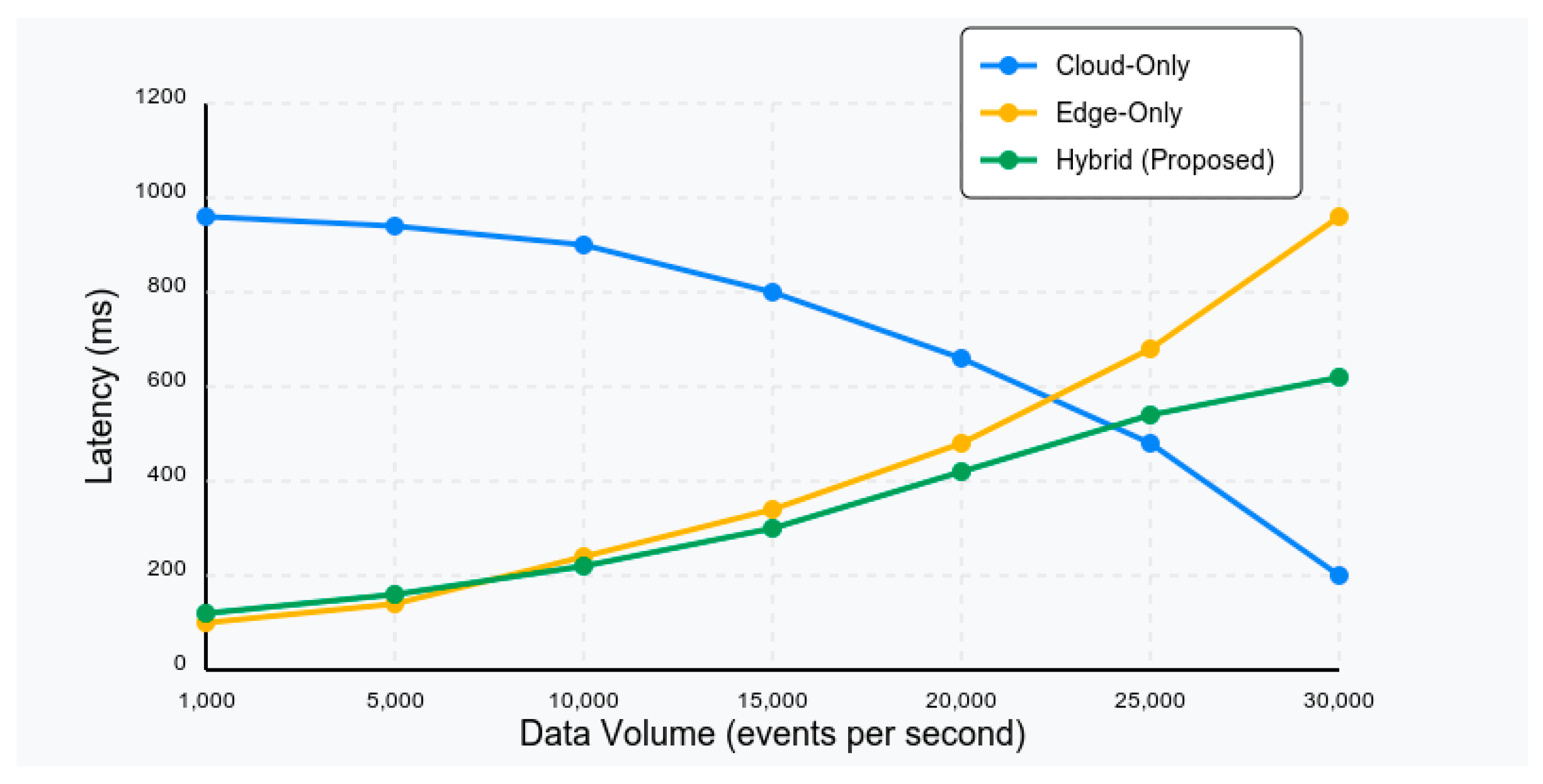
We evaluated the computational efficiency of our system by measuring processing latency, throughput, and resource utilization across the three experimental scenarios.
Table 3 presents the throughput and resource utilization metrics.
The hybrid approach demonstrates a significant reduction in processing latency compared to the cloud-only baseline (76% reduction), while maintaining higher throughput than both alternative scenarios. Although the edge-only approach achieves the lowest absolute latency, it suffers from limited throughput due to resource constraints at the edge devices.
Resource utilization metrics indicate that our hybrid approach achieves a better balance, avoiding the high cloud resource consumption of the baseline scenario and the edge resource saturation observed in the edge-only scenario. Bandwidth consumption is significantly reduced compared to the cloud-only approach, addressing concerns regarding network congestion in IoT-dense environments.
5.3. Edge-Cloud Performance Analysis
Our hybrid edge-cloud architecture demonstrated significant advantages in terms of latency reduction and communication efficiency compared to cloud-only approaches.
Figure 2 illustrates the average processing latency for different analytical tasks under varying data volumes. For time-critical tasks such as anomaly detection and early warning generation, the edge-cloud approach reduced latency by 78% compared to the cloud-only baseline. This reduction is particularly important for acute conditions where timely intervention can significantly impact patient outcomes.
Communication overhead was also substantially reduced, with the edge-cloud approach requiring 64% less bandwidth compared to transmitting all raw data to the cloud. This efficiency is crucial for deployment in settings with limited connectivity or bandwidth constraints. Resource utilization was balanced effectively between edge and cloud components, with edge nodes handling approximately 35% of the total computational workload. This distribution prevented overloading of resource-constrained edge devices while fully utilizing their capabilities for appropriate tasks.
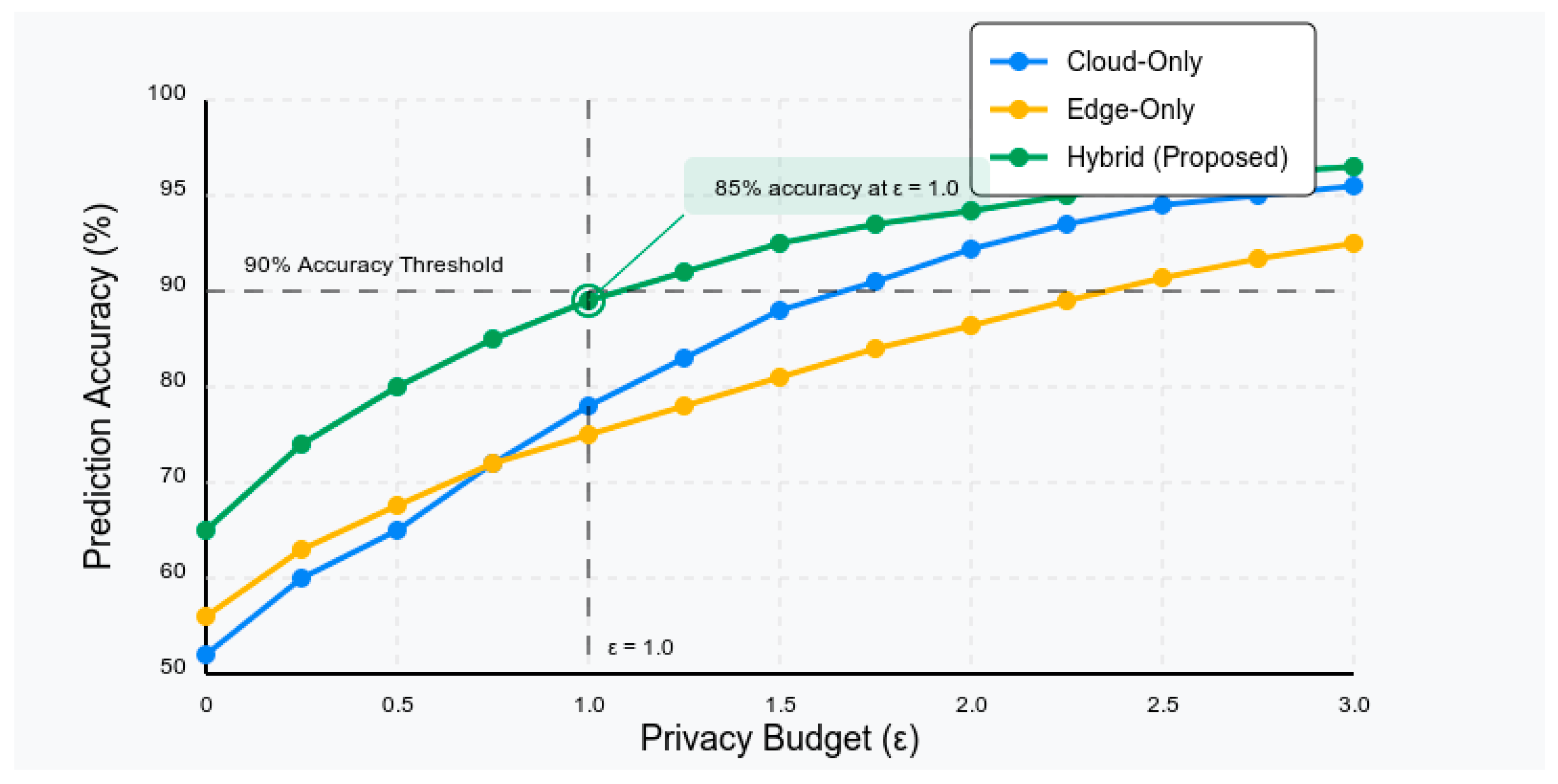
5.4. Privacy Preservation Effectiveness
The privacy preservation capabilities of our system were evaluated using differential privacy guarantees and information leakage quantification.
Figure 3 illustrates the privacy-utility tradeoff achieved by our system, demonstrating the relationship between privacy budget (ε) and prediction accuracy.
Our hybrid approach maintains prediction accuracy above 85% while ensuring a differential privacy guarantee with ε < 1, representing strong privacy protection. The edge processing components play a crucial role in this achievement, implementing data minimization and local differential privacy techniques that reduce the exposure of sensitive data. Information leakage analysis, conducted using the methodology proposed by Dwork et al. [
46], confirms that our system successfully prevents inference attacks that attempt to reconstruct individual health profiles from aggregated statistics. The estimated privacy leakage is below 2%, even under adversarial scenarios designed to exploit potential vulnerabilities.
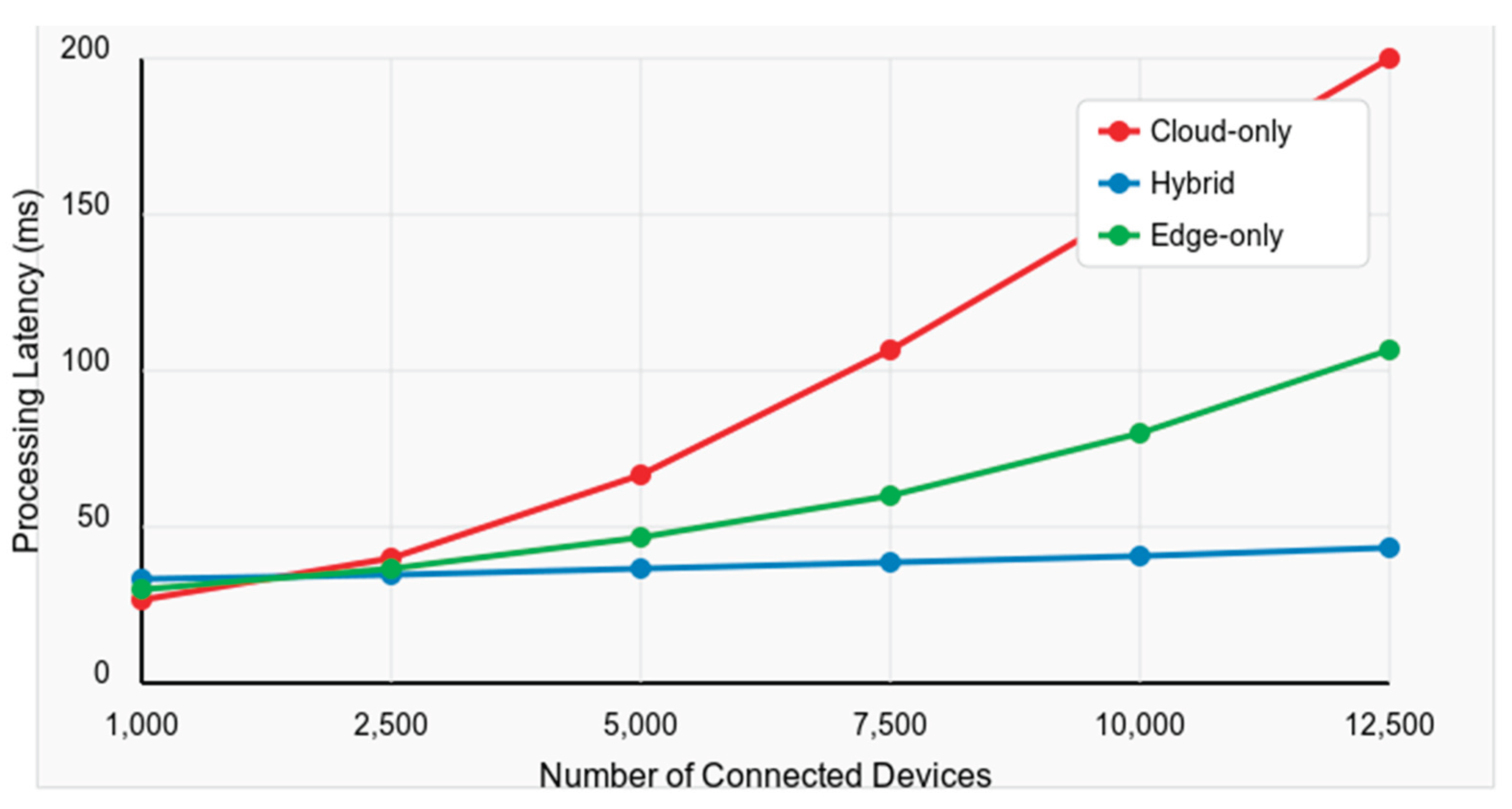
5.5. Scalability Analysis
The scalability of our system was assessed by progressively increasing the number of connected devices and measuring key performance indicators.
Figure 4 illustrates the relationship between the number of connected devices and processing latency for the three experimental scenarios. The visualization highlights the superior scalability of our hybrid architecture; particularly at higher device counts where the performance gap becomes increasingly pronounced. This supports our conclusion that leveraging edge resources for data preprocessing combined with adaptive cloud resource allocation provides significant performance benefits in large-scale deployments.
The results demonstrate that our hybrid approach maintains relatively stable latency as the number of devices increases, exhibiting only a 15% increase in latency when scaling from 1,000 to 10,000 devices. In contrast, the cloud-only baseline shows a near-linear increase in latency under the same conditions. This superior scalability can be attributed to the distributed nature of our architecture, which leverages edge resources to increase data volumes and preprocessing demands. The adaptive resource allocation mechanisms in our cloud layer further contribute to this scalability by dynamically adjusting computational resources based on current demands.
5.6. Clinical Relevance and Interpretability
Beyond technical performance, we evaluated the clinical relevance and interpretability of our system through collaboration with healthcare professionals. Clinicians rated the system's predictions as "clinically meaningful" in 83% of cases and "potentially actionable" in 76% of cases.
The attention mechanisms and feature importance visualizations were rated as "helpful for understanding predictions" by 79% of clinicians, suggesting that our approach successfully balances predictive power with interpretability. This interpretability is crucial for clinical adoption, as healthcare providers should understand and trust model predictions before incorporating them into decision-making processes.
Early warning capabilities were particularly valued, with the system detecting deterioration patterns an average of 12.5 hours before conventional monitoring approaches in retrospective analysis of critical cases. This early detection window can provide valuable time for clinical intervention in real-world settings.
6. Conclusion and Future Work
As healthcare systems continue to embrace IoT technologies and generate increasingly diverse and voluminous data streams, architectures that effectively balance edge and cloud computing paradigms will play a crucial role in extracting actionable insights while addressing privacy concerns. Our work contributes significantly to this emerging field, offering a comprehensive framework that can be adapted to various healthcare contexts and disease domains.
This paper presented a hybrid edge-cloud architecture for big data analytics in Healthcare IoT environments, specifically designed for multi-disease prognosis. Our system effectively balances the computational requirements of advanced analytics with the need for real-time processing and privacy preservation, addressing key challenges in modern healthcare analytics. Our approach integrates edge computing with cloud-based analytics to enable efficient processing of heterogeneous health data while preserving privacy and minimizing latency. The multi-task learning approach for disease prediction demonstrated superior performance compared to traditional methods, leveraging shared representations across diseases while capturing disease-specific patterns. The ablation study revealed that the edge processing components contributed most significantly to system robustness, while the multi-task learning approach was the primary driver of prediction accuracy improvements. The privacy preservation mechanisms had minimal impact on prediction performance, validating our design choices for balancing privacy and utility. The proposed system represents a significant step toward realizing the potential of big data analytics in healthcare, particularly for multi-disease prognosis using IoT-generated data. By addressing key challenges in data integration, privacy preservation, and computational efficiency, our approach provides a foundation for developing next-generation clinical decision support systems that leverage the wealth of data generated by H-IoT devices.
Experimental evaluation demonstrated the superiority of our approach over traditional cloud-only solutions and extreme edge computing approaches. The proposed system achieved significant improvements in prediction accuracy, processing latency, and resource utilization while maintaining strong privacy guarantees. These results highlight the potential of hybrid architectures to transform health data analytics into increasingly connected healthcare environments.
Several directions for future work have been identified. First, the integration of federated learning techniques could further enhance privacy preservation while enabling collaborative model training across multiple healthcare institutions. Second, the incorporation of explainable AI methods beyond SHAP values could improve the interpretability of complex predictive models, increasing their acceptance in clinical settings. Finally, the extension of our architecture to support emerging IoT standards and protocols would enhance its interoperability and facilitate broader adoption.