Submitted:
14 April 2025
Posted:
15 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Literature Selection
3. Definition and Characteristics of Delirium
4. Clinical Features of Delirium in ICU
5. Applications, Dosages, and Key Consideration in ICU Management
6. Caution and Contraindications
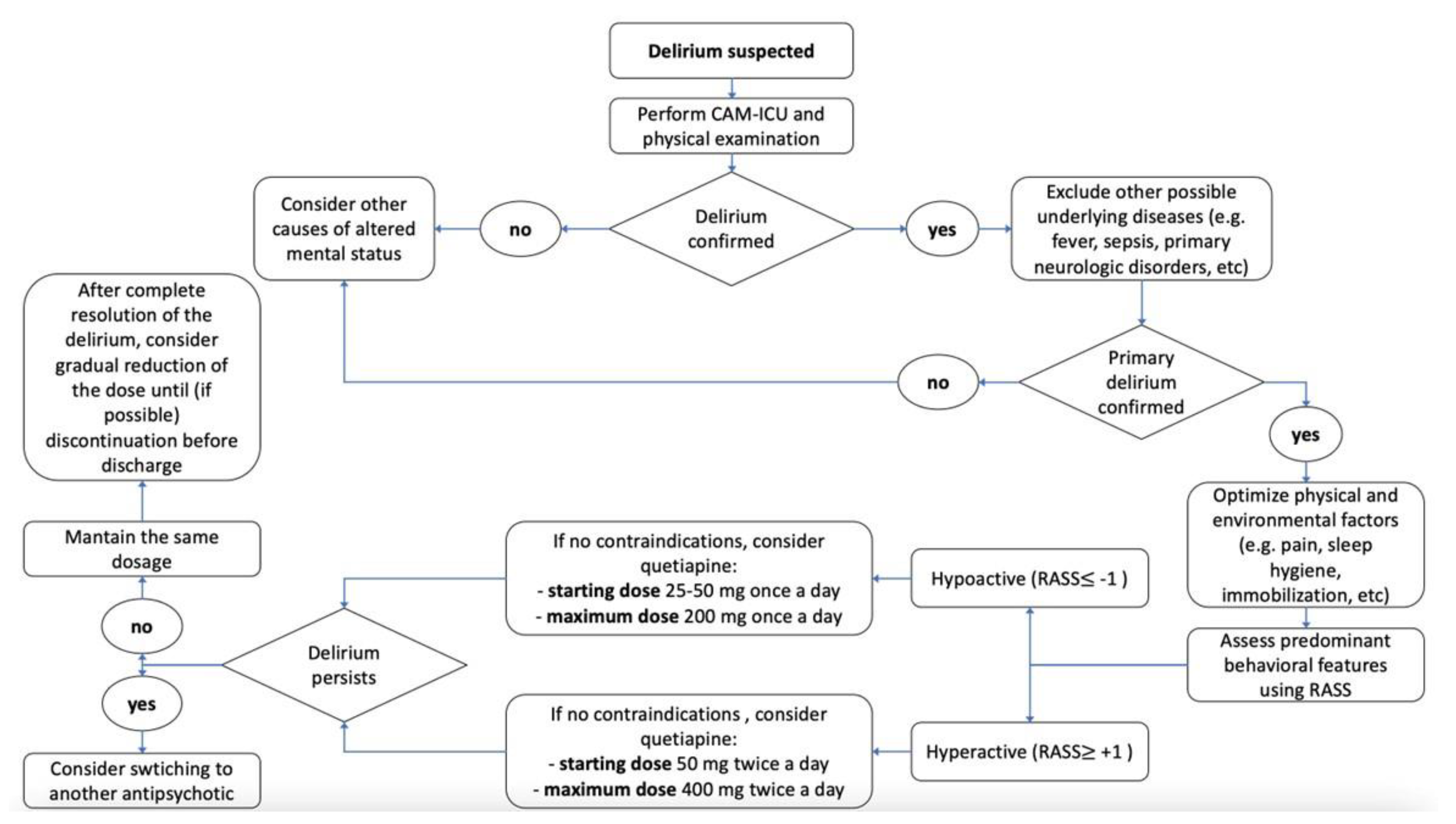
7. Clinical Practical Algorithm
8. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Martinez, F.E.; Tee, R.; Poulter, A.-L.; Jordan, L.; Bell, L.; Balogh, Z.J. Delirium Screening and Pharmacotherapy in the ICU: The Patients Are Not the Only Ones Confused. J Clin Med 2023, 12, 5671. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation-Sedation Scale: Validity and Reliability in Adult Intensive Care Unit Patients. Am J Respir Crit Care Med 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Ely, E.W.; Truman, B.; Shintani, A.; Thomason, J.W.W.; Wheeler, A.P.; Gordon, S.; Francis, J.; Speroff, T.; Gautam, S.; Margolin, R.; et al. Monitoring Sedation Status over Time in ICU Patients: Reliability and Validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003, 289, 2983–2991. [Google Scholar] [CrossRef] [PubMed]
- Miranda, F.; Gonzalez, F.; Plana, M.N.; Zamora, J.; Quinn, T.J.; Seron, P. Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) for the Diagnosis of Delirium in Adults in Critical Care Settings. Cochrane Database Syst Rev 2023, 11, CD013126. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.; Herzig, S.J.; Howell, M.D.; Le, S.H.; Mathew, C.; Kats, J.S.; Stevens, J.P. Antipsychotic Utilization in the Intensive Care Unit and in Transitions of Care. J Crit Care 2016, 33, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, N.; Dubois, M.J.; Dumont, M.; Dial, S.; Skrobik, Y. Intensive Care Delirium Screening Checklist: Evaluation of a New Screening Tool. Intensive Care Med 2001, 27, 859–864. [Google Scholar] [CrossRef]
- van den Boogaard, M.; Pickkers, P.; Slooter, A.J.C.; Kuiper, M.A.; Spronk, P.E.; van der Voort, P.H.J.; van der Hoeven, J.G.; Donders, R.; van Achterberg, T.; Schoonhoven, L. Development and Validation of PRE-DELIRIC (PREdiction of DELIRium in ICu Patients) Delirium Prediction Model for Intensive Care Patients: Observational Multicentre Study. BMJ 2012, 344, e420. [Google Scholar] [CrossRef]
- Wassenaar, A.; van den Boogaard, M.; van Achterberg, T.; Slooter, A.J.C.; Kuiper, M.A.; Hoogendoorn, M.E.; Simons, K.S.; Maseda, E.; Pinto, N.; Jones, C.; et al. Multinational Development and Validation of an Early Prediction Model for Delirium in ICU Patients. Intensive Care Med 2015, 41, 1048–1056. [Google Scholar] [CrossRef]
- Kucuk, O.; Memis, D.; Inal, M.T.; Turan, F.N.; Memis, I. Comparison of the Effectiveness of Delirium Evaluation Tools in Intensive Care Patients: Pre-Deliric Versions 1 and 2, E-Pre-Deliric and ICDSC. Eur Rev Med Pharmacol Sci 2023, 27, 10365–10374. [Google Scholar] [CrossRef]
- Alghadeer, S.; Almesned, R.S.; Alshehri, E.A.; Alwhaibi, A. Evaluation of the Efficacy and Safety of Quetiapine in the Treatment of Delirium in Adult ICU Patients: A Retrospective Comparative Study. J Clin Med 2024, 13, 802. [Google Scholar] [CrossRef]
- Wang, C.-L.; Wu, V.C.-C.; Lee, C.H.; Wu, C.-L.; Chen, H.-M.; Huang, Y.-T.; Chang, S.-H. Incidences, Risk Factors, and Clinical Correlates of Severe QT Prolongation after the Use of Quetiapine or Haloperidol. Heart Rhythm 2024, 21, 321–328. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca, A.C.C.; Matias, D.; Garcia, C.; Amaral, R.; Geraldo, L.H.; Freitas, C.; Lima, F.R.S. The Impact of Microglial Activation on Blood-Brain Barrier in Brain Diseases. Front Cell Neurosci 2014, 8, 362. [Google Scholar] [CrossRef]
- MohanKumar, S.M.J.; Murugan, A.; Palaniyappan, A.; MohanKumar, P.S. Role of Cytokines and Reactive Oxygen Species in Brain Aging. Mech Ageing Dev 2023, 214, 111855. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, N. Electrolyte Disorders and the Nervous System. Continuum (Minneap Minn) 2020, 26, 632–658. [Google Scholar] [CrossRef]
- Arora, R.C.; Cunningham, C. Losing Sleep over Delirium. Crit Care Med 2018, 46, 1036–1038. [Google Scholar] [CrossRef]
- Bani Younis, M.; Hayajneh, F.; Alshraideh, J.A. Effect of Noise and Light Levels on Sleep of Intensive Care Unit Patients. Nurs Crit Care 2021, 26, 73–78. [Google Scholar] [CrossRef] [PubMed]
- John, C.J.; Engler, M.; Zaki, H.; Crooker, A.; Cabrera, M.; Golden, C.; Whitehill, R.; Xiang, Y.; Liu, K.; Fundora, M.P. The Effect of Antipsychotic Medications on QTc and Delirium in Paediatric Cardiac Patients with ICU Delirium. Cardiol Young 2024, 1–5. [Google Scholar] [CrossRef]
- Zakhary, T.; Ahmed, I.; Luttfi, I.; Montasser, M. Quetiapine Versus Haloperidol in the Management of Hyperactive Delirium: Randomized Controlled Trial. Neurocrit Care 2024. [Google Scholar] [CrossRef]
- Hanna, M.P.; Adie, S.K.; Ketcham, S.W.; Deshmukh, A.; Gondi, K.; Abdul-Aziz, A.A.; Prescott, H.C.; Thomas, M.P.; Konerman, M.C. Atypical Antipsychotic Safety in the CICU. Am J Cardiol 2022, 163, 117–123. [Google Scholar] [CrossRef]
- Mo, Y.; Yam, F.K. Rational Use of Second-Generation Antipsychotics for the Treatment of ICU Delirium. J Pharm Pract 2017, 30, 121–129. [Google Scholar] [CrossRef]
- Lewis, K.; Balas, M.C.; Stollings, J.L.; McNett, M.; Girard, T.D.; Chanques, G.; Kho, M.E.; Pandharipande, P.P.; Weinhouse, G.L.; Brummel, N.E.; et al. A Focused Update to the Clinical Practice Guidelines for the Prevention and Management of Pain, Anxiety, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical Care Medicine 10.1097/CCM.0000000000006574. [CrossRef]
- Ali, M.; Cascella, M. ICU Delirium. In StatPearls; StatPearls Publishing: Treasure Island (FL), 2024. [Google Scholar]
- Arumugam, S.; El-Menyar, A.; Al-Hassani, A.; Strandvik, G.; Asim, M.; Mekkodithal, A.; Mudali, I.; Al-Thani, H. Delirium in the Intensive Care Unit. J Emerg Trauma Shock 2017, 10, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.K.; Needham, E. Diagnosis of Delirium: A Practical Approach. Pract Neurol 2023, 23, 192–199. [Google Scholar] [CrossRef]
- Saxena, S.; Lawley, D. Delirium in the Elderly: A Clinical Review. Postgrad Med J 2009, 85, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Stevens, R.D.; Nyquist, P.A. Coma, Delirium, and Cognitive Dysfunction in Critical Illness. Crit Care Clin 2006, 22, 787–804; abstract x. [CrossRef]
- Ormseth, C.H.; LaHue, S.C.; Oldham, M.A.; Josephson, S.A.; Whitaker, E.; Douglas, V.C. Predisposing and Precipitating Factors Associated With Delirium: A Systematic Review. JAMA Netw Open 2023, 6, e2249950. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.B. Which Medications to Avoid in People at Risk of Delirium: A Systematic Review. Age Ageing 2011, 40, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Reisinger, M.; Reininghaus, E.Z.; Biasi, J.D.; Fellendorf, F.T.; Schoberer, D. Delirium-associated Medication in People at Risk: A Systematic Update Review, Meta-analyses, and GRADE-profiles. Acta Psychiatr Scand 2023, 147, 16–42. [Google Scholar] [CrossRef]
- Fiest, K.M.; Soo, A.; Hee Lee, C.; Niven, D.J.; Ely, E.W.; Doig, C.J.; Stelfox, H.T. Long-Term Outcomes in ICU Patients with Delirium: A Population-Based Cohort Study. Am J Respir Crit Care Med 204, 412–420. [CrossRef]
- Zaal, I.J.; Devlin, J.W.; Hazelbag, M.; Klein Klouwenberg, P.M.C.; van der Kooi, A.W.; Ong, D.S.Y.; Cremer, O.L.; Groenwold, R.H.; Slooter, A.J.C. Benzodiazepine-Associated Delirium in Critically Ill Adults. Intensive Care Med 2015, 41, 2130–2137. [Google Scholar] [CrossRef]
- Alagiakrishnan, K.; Wiens, C.A. An Approach to Drug Induced Delirium in the Elderly. Postgrad Med J 2004, 80, 388–393. [Google Scholar] [CrossRef]
- Maldonado, J.R. Neuropathogenesis of Delirium: Review of Current Etiologic Theories and Common Pathways. Am J Geriatr Psychiatry 2013, 21, 1190–1222. [Google Scholar] [CrossRef]
- Flacker, J.M.; Lipsitz, L.A. Neural Mechanisms of Delirium: Current Hypotheses and Evolving Concepts. J Gerontol A Biol Sci Med Sci 1999, 54, B239-246. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Li, Y.; Li, B.; Ge, Q. Inflammatory Biomarkers and Delirium: A Mendelian Randomization Study. Front Aging Neurosci 2023, 15, 1221272. [Google Scholar] [CrossRef]
- Springer, B. Hyperactive Delirium with Severe Agitation. Emerg Med Clin North Am 2024, 42, 41–52. [Google Scholar] [CrossRef]
- Rosen, J.H.; Bieber, E.; Matta, S.E.; Sayde, G.E.; Fedotova, N.O.; deVries, J.; Rafferty, M.; Stern, T.A. Hypoactive Delirium: Differential Diagnosis, Evaluation, and Treatment. Prim Care Companion CNS Disord 2024, 26, 23f03602. [Google Scholar] [CrossRef]
- Cole, M.G.; McCusker, J.; Dendukuri, N.; Han, L. Symptoms of Delirium among Elderly Medical Inpatients with or without Dementia. J Neuropsychiatry Clin Neurosci 2002, 14, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Gunther, M.L.; Morandi, A.; Ely, E.W. Pathophysiology of Delirium in the Intensive Care Unit. Crit Care Clin 2008, 24, 45–65, viii. [CrossRef] [PubMed]
- Tokuda, R.; Nakamura, K.; Takatani, Y.; Tanaka, C.; Kondo, Y.; Ohbe, H.; Kamijo, H.; Otake, K.; Nakamura, A.; Ishikura, H.; et al. Sepsis-Associated Delirium: A Narrative Review. J Clin Med 2023, 12, 1273. [Google Scholar] [CrossRef]
- Faisal, H.; Farhat, S.; Grewal, N.K.; Masud, F.N. ICU Delirium in Cardiac Patients. Methodist DeBakey Cardiovascular Journal 2023, 19, 74. [Google Scholar] [CrossRef]
- Guidet, B.; de Lange, D.W.; Boumendil, A.; Leaver, S.; Watson, X.; Boulanger, C.; Szczeklik, W.; Artigas, A.; Morandi, A.; Andersen, F.; et al. The Contribution of Frailty, Cognition, Activity of Daily Life and Comorbidities on Outcome in Acutely Admitted Patients over 80 Years in European ICUs: The VIP2 Study. Intensive Care Med 2020, 46, 57–69. [Google Scholar] [CrossRef]
- Menges, D.; Seiler, B.; Tomonaga, Y.; Schwenkglenks, M.; Puhan, M.A.; Yebyo, H.G. Systematic Early versus Late Mobilization or Standard Early Mobilization in Mechanically Ventilated Adult ICU Patients: Systematic Review and Meta-Analysis. Crit Care 2021, 25, 16. [Google Scholar] [CrossRef]
- Goldstein, J.M. Quetiapine Fumarate (Seroquel): A New Atypical Antipsychotic. Drugs Today (Barc) 1999, 35, 193–210. [Google Scholar] [CrossRef]
- DeVane, C.L.; Nemeroff, C.B. Clinical Pharmacokinetics of Quetiapine: An Atypical Antipsychotic. Clin Pharmacokinet 2001, 40, 509–522. [Google Scholar] [CrossRef] [PubMed]
- Bakken, G.V.; Rudberg, I.; Christensen, H.; Molden, E.; Refsum, H.; Hermann, M. Metabolism of Quetiapine by CYP3A4 and CYP3A5 in Presence or Absence of Cytochrome B5. Drug Metab Dispos 2009, 37, 254–258. [Google Scholar] [CrossRef]
- Seeman, P. Atypical Antipsychotics: Mechanism of Action. Can J Psychiatry 2002, 47, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Gefvert, O.; Lundberg, T.; Wieselgren, I.M.; Bergström, M.; Långström, B.; Wiesel, F.; Lindström, L. D(2) and 5HT(2A) Receptor Occupancy of Different Doses of Quetiapine in Schizophrenia: A PET Study. Eur Neuropsychopharmacol 2001, 11, 105–110. [Google Scholar] [CrossRef]
- Ohman, K.L.; Schultheis, J.M.; Kram, S.J.; Cox, C.E.; Gilstrap, D.L.; Yang, Z.; Kram, B.L. Effectiveness of Quetiapine as a Sedative Adjunct in Mechanically Ventilated Adults Without Delirium. Ann Pharmacother 2021, 55, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Assadoon, M.S.; Kovacevic, M.P.; Dube, K.M.; Szumita, P.M.; Lupi, K.E.; DeGrado, J.R. Evaluation of Atypical Antipsychotics for the Facilitation of Weaning Sedation in Mechanically Ventilated Critically Ill Patients. J Intensive Care Med 2024, 39, 52–58. [Google Scholar] [CrossRef]
- Girard, T.D.; Pandharipande, P.P.; Carson, S.S.; Schmidt, G.A.; Wright, P.E.; Canonico, A.E.; Pun, B.T.; Thompson, J.L.; Shintani, A.K.; Meltzer, H.Y.; et al. Feasibility, Efficacy, and Safety of Antipsychotics for Intensive Care Unit Delirium: The MIND Randomized, Placebo-Controlled Trial. Crit Care Med 2010, 38, 428–437. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Riker, R.R.; Hinderleider, E.; Roberts, R.J.; Fong, J.J.; Ruthazer, R.; Hill, N.S.; Garpestad, E. Impact of Quetiapine on Resolution of Individual Delirium Symptoms in Critically Ill Patients with Delirium: A Post-Hoc Analysis of a Double-Blind, Randomized, Placebo-Controlled Study. Crit Care 2011, 15, R215. [Google Scholar] [CrossRef]
- Abraham, M.P.; Hinds, M.; Tayidi, I.; Jeffcoach, D.R.; Corder, J.M.; Hamilton, L.A.; Lawson, C.M.; Bollig, R.W.; Heidel, R.E.; Daley, B.J.; et al. Quetiapine for Delirium Prophylaxis in High-Risk Critically Ill Patients. Surgeon 2021, 19, 65–71. [Google Scholar] [CrossRef]
- Wan, R.Y.; Kasliwal, M.; McKenzie, C.A.; Barrett, N.A. Quetiapine in Refractory Hyperactive and Mixed Intensive Care Delirium: A Case Series. Critical Care 2011, 15, R159. [Google Scholar] [CrossRef] [PubMed]
- Michaud, C.J.; Bullard, H.M.; Harris, S.A.; Thomas, W.L. Impact of Quetiapine Treatment on Duration of Hypoactive Delirium in Critically Ill Adults: A Retrospective Analysis. Pharmacotherapy 2015, 35, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Devlin, J.W.; Roberts, R.J.; Fong, J.J.; Skrobik, Y.; Riker, R.R.; Hill, N.S.; Robbins, T.; Garpestad, E. Efficacy and Safety of Quetiapine in Critically Ill Patients with Delirium: A Prospective, Multicenter, Randomized, Double-Blind, Placebo-Controlled Pilot Study. Crit Care Med 2010, 38, 419–427. [Google Scholar] [CrossRef]
- Maneeton, B.; Maneeton, N.; Srisurapanont, M.; Chittawatanarat, K. Quetiapine versus Haloperidol in the Treatment of Delirium: A Double-Blind, Randomized, Controlled Trial. Drug Des Devel Ther 2013, 7, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Hasnain, M.; Vieweg, W.V.R.; Howland, R.H.; Kogut, C.; Breden Crouse, E.L.; Koneru, J.N.; Hancox, J.C.; Digby, G.C.; Baranchuk, A.; Deshmukh, A.; et al. Quetiapine, QTc Interval Prolongation, and Torsade de Pointes: A Review of Case Reports. Ther Adv Psychopharmacol 2014, 4, 130–138. [Google Scholar] [CrossRef]
- Dube, K.M.; DeGrado, J.; Hohlfelder, B.; Szumita, P.M. Evaluation of the Effects of Quetiapine on QTc Prolongation in Critically Ill Patients. J Pharm Pract 2018, 31, 292–297. [Google Scholar] [CrossRef]
- Shim, S.S. Extrapyramidal Symptoms Associated with Quetiapine. Aust N Z J Psychiatry 2003, 37, 773. [Google Scholar] [CrossRef]
- Mistraletti, G.; Mantovani, E.S.; Cadringher, P.; Cerri, B.; Corbella, D.; Umbrello, M.; Anania, S.; Andrighi, E.; Barello, S.; Di Carlo, A.; et al. Enteral vs. Intravenous ICU Sedation Management: Study Protocol for a Randomized Controlled Trial. Trials 2013, 14, 92. [Google Scholar] [CrossRef]
- Tomichek, J.E.; Stollings, J.L.; Pandharipande, P.P.; Chandrasekhar, R.; Ely, E.W.; Girard, T.D. Antipsychotic Prescribing Patterns during and after Critical Illness: A Prospective Cohort Study. Crit Care 2016, 20, 378. [Google Scholar] [CrossRef]
- Nakamura, M.; Seki, M.; Sato, Y.; Nagamine, T. Quetiapine-Induced Bradycardia and Hypotension in the Elderly—A Case Report. Innovations in Clinical Neuroscience 2016, 13, 34. [Google Scholar]
- Gunther, M.; Dopheide, J.A. Antipsychotic Safety in Liver Disease: A Narrative Review and Practical Guide for the Clinician. J Acad Consult Liaison Psychiatry 2023, 64, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Thyrum, P.T.; Wong, Y.W.; Yeh, C. Single-Dose Pharmacokinetics of Quetiapine in Subjects with Renal or Hepatic Impairment. Prog Neuropsychopharmacol Biol Psychiatry 2000, 24, 521–533. [Google Scholar] [CrossRef] [PubMed]
- Palakshappa, J.A.; Hough, C.L. How We Prevent and Treat Delirium in the ICU. Chest 2021, 160, 1326. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med 2018, 46, e825–e873. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, A.; Delgado, E.; Battle, A.; Norton, C. Quetiapine Twice Daily Versus Bedtime Dosing in the Treatment of ICU Delirium. J Pharm Pract 2023, 8971900231193545. [Google Scholar] [CrossRef]
- Mart, M.F.; Boehm, L.M.; Kiehl, A.L.; Gong, M.N.; Malhotra, A.; Owens, R.L.; Khan, B.A.; Pisani, M.A.; Schmidt, G.A.; Hite, R.D.; et al. Long-Term Outcomes after Treatment of Delirium during Critical Illness with Antipsychotics (MIND-USA): A Randomised, Placebo-Controlled, Phase 3 Trial. The Lancet Respiratory Medicine 2024, 12, 599–607. [Google Scholar] [CrossRef]
| Study | Patients | Design | Main Findings |
|---|---|---|---|
| Martinez et al. [1] | 665 ICU patients | Retrospective observational study | The screening rates for RASS and CAM-ICU were below the recommended levels. The administration of antipsychotic medications – mostly quetiapine in this cohort - occurs more frequently than the diagnosis of delirium |
| Sessler et al. [2] | 192 ICU patients | Comparative study | RASS showed high inter-rater reliability among the entire adult ICU population. Robust correlations between the investigator-assigned RASS and the visual analog scale scores validated the use of RASS across all subgroups within the ICU. The RASS scores documented by individual physicians, nurses, and pharmacists exhibited a strong correlation with the principal investigator's visual analog scale score. |
| Ely et al. [3] | 290 ICU patients | Prospective cohort study | The RASS represents the first sedation scale validated for its capacity to identify variations in sedation levels over successive days of ICU treatment, in relation to constructs such as consciousness levels and delirium, and it showed a correlation with the dosages of sedative and analgesic medications administered. This study confirmed the reliability and validity of RASS for monitoring sedation status over time. |
| Miranda et al. [4] | 2817 ICU | Cochrane review | This study evaluated CAM-ICU for diagnosing delirium in critical care settings. The test is primarily beneficial for ruling out delirium. However, it may fail to identify a subset of patients with newly developed delirium. Consequently, in scenarios where comprehensive detection of all delirium cases is essential, it may be advisable to either retest or to use the CAM-ICU in conjunction with an additional assessment. |
| Marshall et al. [5] | 164'996 ICU patients | Retrospective observational cohort study | Antipsychotic medications are prescribed to 1 in every 10 patients in the ICU, and their use is correlated with prolonged lengths of stay in both the ICU and the hospital. Patients receiving antipsychotics without any recorded diagnosis of a mental disorder exhibit longer ICU stays, extended hospitalizations, and higher mortality rates in comparison to those with a documented mental disorder. |
| Ohman et al [49] | 57 ICU mechanically ventilated | retrospective interpatient comparator study | Following quetiapine initiation, no significant differences were observed in 24-hour cumulative doses of propofol, dexmedetomidine, benzodiazepines, or opioids. However, dexmedetomidine requirements increased significantly over 48 hours (P = 0.03). There were no changes in pain or sedation scores, sedation depth, or QTc interval. |
| Assadoon et al [50] | 107 ICU patients | Retrospective | Within 48 hours of initiating atypical antipsychotics, 77.6% of patients showed ≥20% reduction in cumulative dose of a sedative/analgesic. Propofol use decreased significantly, and dexmedetomidine use increased. Sedation levels were lighter, with no change in pain scores. |
| Wan et al [54] | 70 ICU patients | retrospective | In patients previously treated with multiple agents for delirium (median RASS = 3), quetiapine was started at 25 mg/day and titrated to 50 mg/day. Initiated after a median of 15 days of persistent delirium, quetiapine was associated with reduced use of other medications and delirium resolution within a median of 4 days. Reported adverse effects included somnolence and transient hypotension. |
| Michaud et al. [55] | 113 ICU diagnosed hypoactive delirium | Prospective intervntional study | Quetiapine was associated with a shorter median duration of delirium (1.5 vs 2.0 days, p=0.04) and a trend toward faster extubation (3 vs 5 days, p=0.08). No significant differences were observed in ICU or hospital length of stay, and safety profiles were comparable between groups |
| Girard et al. [51] | 101 ICU patients mechanically ventilated | Randomized, double-blind, placebo-controlled | Neither haloperidol nor ziprasidone significantly shortened the duration of delirium when compared to placebo. Patients across the three treatment groups had a comparable number of days alive without experiencing delirium or coma. |
| Mart et al. [69] | 566 ICU patients | Randomized, double-blind, placebo-controlled | In critically ill patients experiencing delirium, neither haloperidol nor ziprasidone demonstrated a significant impact on cognitive, functional, psychological, or quality-of-life outcomes in survivors. |
| Devlin et al. [56] | 36 ICU patients with delirium | Prospective, randomized, double-blind, placebo-controlled | The inclusion of quetiapine with as-needed haloperidol is associated with a more rapid resolution of delirium, decreased levels of agitation, and a higher rate of discharge to home or rehabilitation. Patients receiving quetiapine need fewer days of as-needed haloperidol. Furthermore, the occurrence of QTc prolongation and extrapyramidal symptoms was comparable between the groups. |
| Zakhary et al. [18] | 100 ICU patients | Randomized controlled | Quetiapine has been shown to be as effective as haloperidol in alleviating the symptoms of hyperactive delirium in critically ill patients, although it does not confer any benefit in terms of mortality. |
| Maneeton et al. [57] | 52 ICU patients with delirium | Prospective, double-blind, randomized controlled | Low doses of quetiapine and haloperidol demonstrate comparable efficacy and safety for managing behavioral disturbances (efficacy, tolerability, total sleep time) in patients with delirium, particularly when combined with environmental modifications. |
| Alghadeer et al. [10] | 47 ICU patients | Retrospective comparative study | The authors found no significant differences in efficacy or adverse effects when comparing the treatment of delirium with quetiapine, haloperidol, risperidone, and olanzapine |
| Wang et al. [11] | 11173 patients, quetiapine vs haloperidol | Multicenter retrospective cohort study | The authors showed that severe QT prolongation was prevalent among patients undergoing treatment with quetiapine or haloperidol. A considerable proportion of these patients were exposed to risk factors associated with QT prolongation, including older age, heart failure, hypokalemia, and the concurrent administration of medications recognized to elevate the risk of torsades des pointes. |
| Dube et al. [59] | 103 ICU patients | Single-center, prospective cohort analysis | There were no reported occurrences of torsades de pointes. QTc prolongation was relatively rare among critically ill patients receiving quetiapine. Patients who were prescribed concomitant medications known to prolong the QTc interval may be at a heightened risk. |
| Tomichek et al. [62] | 500 ICU patients | Single-center prospective cohort study | The administration of an atypical antipsychotic markedly increased the probability of receiving an antipsychotic prescription at discharge, a practice that should be carefully evaluated during medication reconciliation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





