Introduction
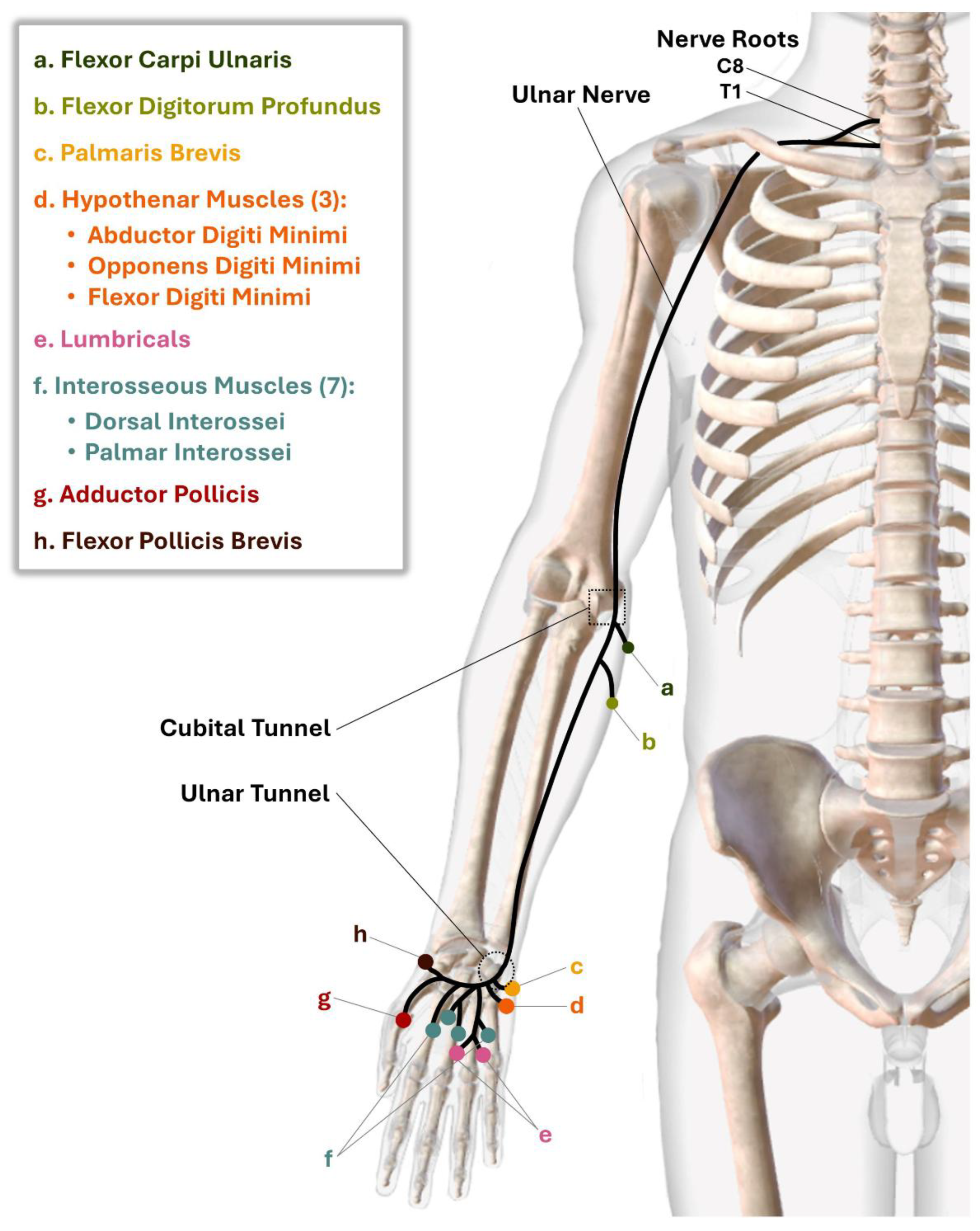
Ulnar nerve compression is a common injury of the peripheral nervous system resulting from increased force on the nerve along its pathway. This nerve is especially vulnerable in the cubital tunnel at the elbow and the ulnar tunnel (Guyon’s canal) at the wrist. If left untreated the resulting muscle denervation and soft tissue imbalance can eventually result in a visual sign known as the pathognomonic “claw hand” deformity [
1,
2,
3,
4,
5]. This visual presentation can vary from strikingly obvious to subtle, depending on factors such as lesion location, injury mechanism, severity level, and recovery phase [
6,
7]. Due to the variability of presentation, ulnar nerve compression injuries often go unrecognized or misdiagnosed. This is particularly problematic because prolonged compression can ultimately result in permanent disability or impairment, accompanied by symptoms of neuropathic pain, paresthesia, sensory loss, and muscle weakness [
3,
8]. Even if the nerve recovers and motor units reinnervate, structural and mechanical changes to the hand can persist and cortical representation remains unaltered. Thus, it is important for providers to be able to recognize early signs of ulnar nerve compression and refer these clients to a certified hand therapist (CHT) for timely, specialized treatment.
CHTs are licensed occupational or physical therapists with advanced training in the evaluation and treatment of the hand-to-shoulder region. Client access to hand therapy can correct or mitigate deformity pattern progression. Specifically, hand therapy can maximize function, reduce pain, offer sensory loss strategies, restore soft tissue imbalance, and improve quality of life [
2,
9]. Despite CHTs’ expertise in assessing complex hand conditions, clients with ulnar nerve compression rarely get referred to them. This may be due to provider misconceptions or lack of awareness regarding the scope and benefits of hand therapy, time constraints with clients, limited access to CHTs, or cost/insurance barriers. In cases in which clients with ulnar nerve compression do receive a hand therapy referral, it is common for the diagnoses to be incomplete or incorrect, encompassing terms such as “general hand weakness,” “hand changes due to aging,” “Dupuytren’s disease,” or “proximal interphalangeal joint contracture.” This might be attributed to unfamiliarity with the risk factors and deformity patterns inherent to ulnar nerve compression. Therefore, this editorial is intended to assist providers in detecting early signs of the often
camouflaged devastation to the hand that results from ulnar nerve compression and increase the likelihood of referring clients to CHTs.
Recognizing Ulnar Nerve Compression
Visual Signs
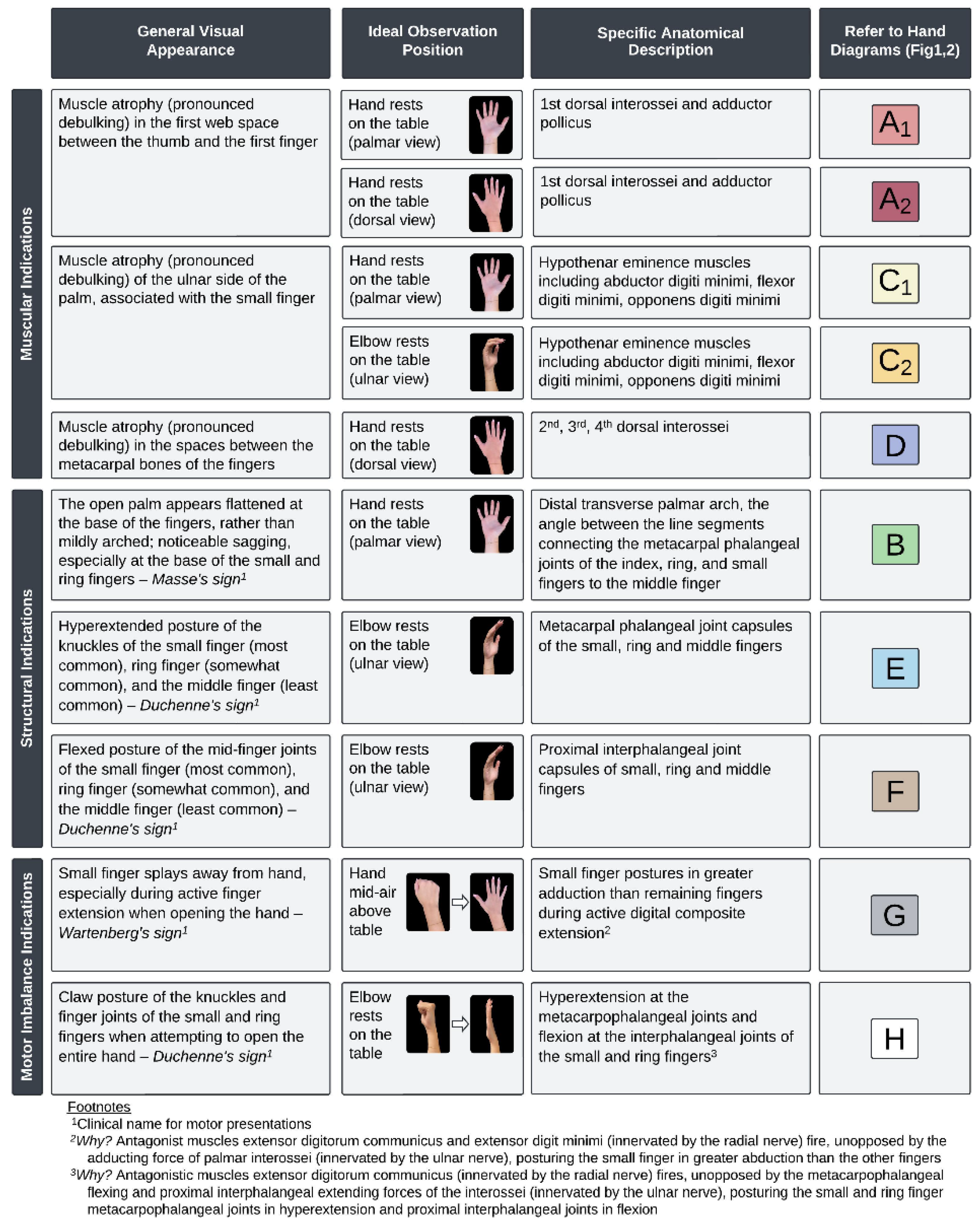
The visual presentation of the hand is itself an observable motor sign, but thinking beyond the ubiquitous “claw hand” is necessary. This term describes the appearance of a hand with
advanced injury to the ulnar nerve; when actively extending the hand, the index and middle fingers will straighten normally, but the ring and small fingers will posture in a hook. This paper offers a framework for providers to detect ulnar nerve motor weakness and soft tissue imbalance at
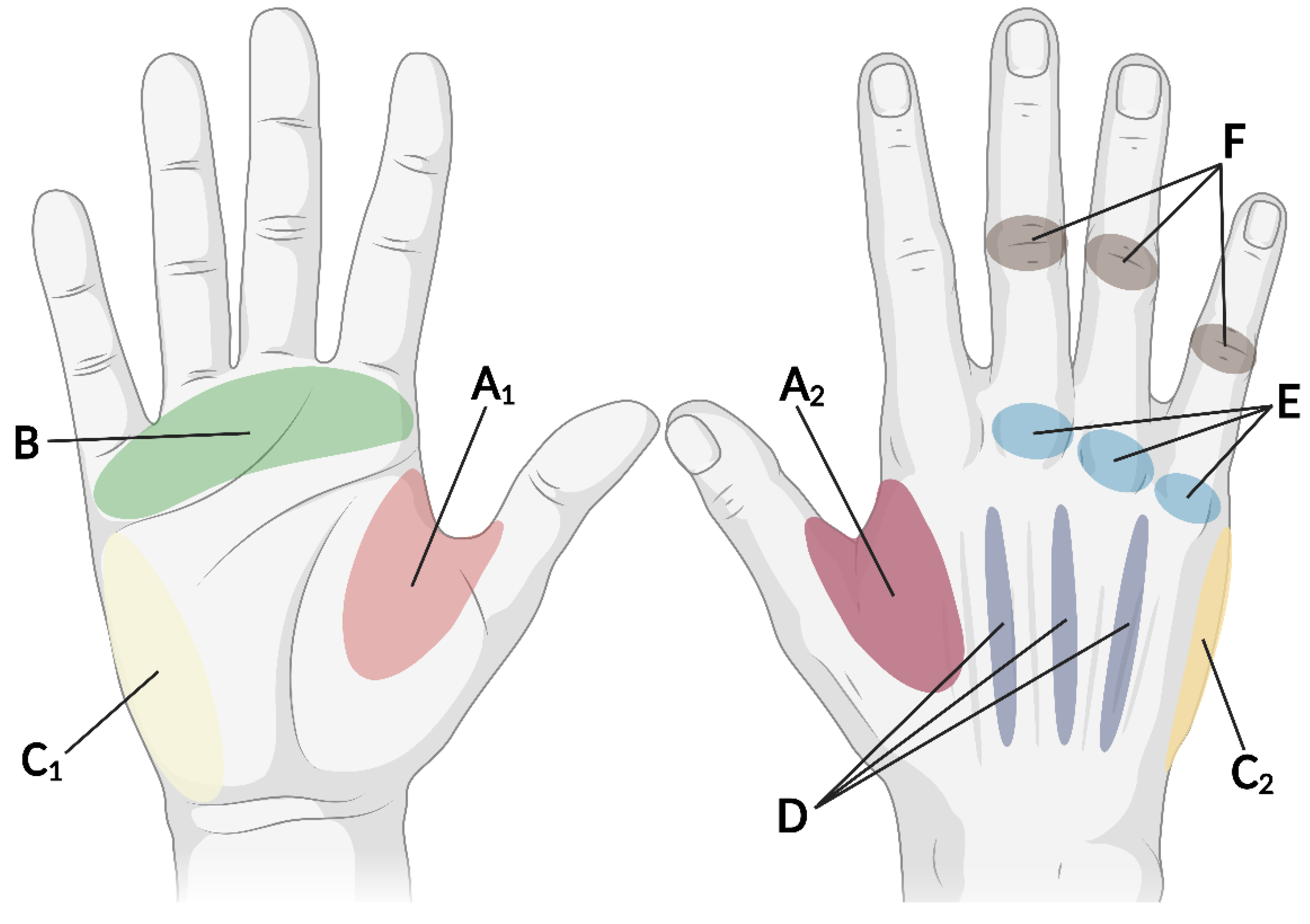
earlier stages of injury, well before the classic “claw hand” appears. The hand regions most commonly impacted throughout the course of injury are indicated in
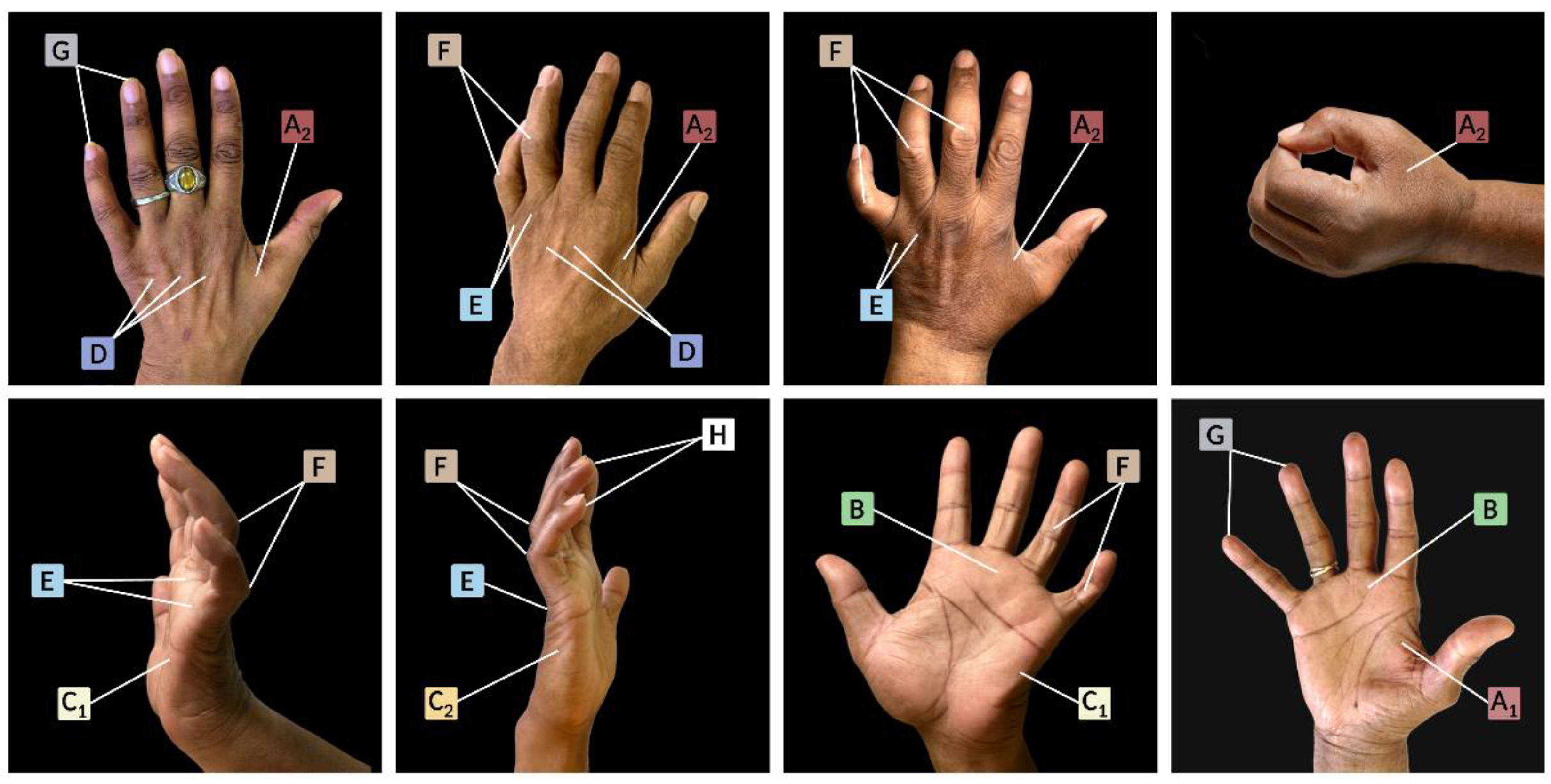
Figure 1, with real-world examples of client hands portrayed in
Figure 2. General descriptions of the various visual signs and their anatomical explanations as well as ideal observation positions are provided in
Figure 3. These visual indicators may result from muscular, structural, and/or motor imbalance that can be examined by placing a client’s hand in various postures. Combining direct assessment with a client interview is necessary for earlier detection, as speaking with the client will help reveal various risk factors and functional complaints associated with ulnar nerve compression.
Risk Factors
Primary Conditions & Trauma
While ulnar nerve compression can be an isolated injury, it often accompanies other conditions as a secondary ailment (see
Table 1A for common primary conditions). Some examples of systemic conditions that metabolically prime peripheral nerves to be more susceptible to mechanical forces and entrapment within the body include autoimmune disease [
10], diabetes mellitus [
11], hypertension [
11], and thyroid disease [
11]. Similarly, musculoskeletal conditions such as carpal tunnel syndrome can also increase the risk of ulnar nerve compression. In fact, conditions such as brachial plexus compression and cervical radiculopathy predispose upper extremity nerves to a “double crush” injury [
12], such that when a nerve is compressed at one location, it is more likely to become compressed at a 2nd or 3rd location [
13,
14,
15,
16,
17]. For example, a double crush injury of the ulnar nerve can start at the brachial plexus and later impact the elbow or wrist (secondary to proximal nerve compression). Some other conditions that can disrupt the nerve pathway include cysts and tumors, as they place increasing pressure on the nerve as they grow over time.
Recent trauma can also serve as a clue for possible ulnar nerve compression, even if trauma occurred without direct injury to the nerve. Nerves are sensitive and easily irritated by excessive stress, even from surrounding structures. Secondary nerve damage may be overlooked when there is a concurrent and less subtle primary injury. For example, soft tissue traumas such as a crush injury or high velocity stretch give rise to contusion and intra- or extra-neural edema; these biochemical responses create pressure in localized areas along the ulnar nerve pathway, resulting in secondary nerve irritation [
18,
19]. Similarly, bone fractures about the wrist, forearm, elbow, upper arm, and shoulder can generate enough force to impact surrounding nerves. Evidence of indirect nerve involvement can be supported by details of the client’s story. Discover the intensity, duration, and location of force on the body as well as the body’s position during impact when clients describe the mechanism of injury.
Inquiring about pre-existing nerve compression is also an essential part to a comprehensive history intake, as prior compression renders the nerve more vulnerable to trauma and can expedite nerve damage. Individuals with chronic nerve compression who encounter an acute force that exceeds the nerve’s capacity to adapt may experience severe neurogenic symptoms. For example, a motor vehicle accident might lead to excessive torque of an individual’s wrist and forearm if they firmly grip the steering wheel upon impact; this high velocity stretch of a pre-existing ulnar nerve irritation could result in progressed muscle atrophy. If any of the aforementioned primary or traumatic conditions are revealed as part of the client’s health history, this information can bolster suspicion of ulnar nerve compression.
Lifestyle Components
Various aspects of a client’s lifestyle may increase the risk of ulnar nerve compression. During the initial interview, look for clues revealing common intrinsic and extrinsic lifestyle factors that increase compression risk (see
Table 1B for detailed list). Some demographic examples include being over 40, pregnant, or in perimenopause/menopause [
20,
21]. Behavioral factors can also compromise ulnar nerve health, such as lacking quality sleep, consuming a nutrient-deprived diet, and being sedentary [
22,
23,
24,
25]. In addition, toxin exposures such as alcohol and tobacco use, certain medications (e.g., antibiotics, heart medicine), and cancer treatment (e.g., chemotherapy, radiation) can endanger nerves [
15,
26,
27,
28].
It is also important to consider the various postures the client may be positioned in on a regular basis due to their career, hobbies, and/or daily activities. Undue mechanical stress to the upper limb can occur during typical activities of daily living which place the axilla, elbow, wrist, and palm in prolonged positions of excessive strain. For example, regularly engaging in driving a vehicle, gaming, or using a keyboard without proper arm support can result in compression or excessive stretch of the ulnar nerve at multiple locations, particularly the cubital and ulnar tunnels. In addition, use of certain assistive devices for mobility can also damage the nerve: crutches compress at the axilla, platform walkers at the elbow, and standard walkers/manual wheelchairs at the wrist. Finally, activities that consist of high-velocity stretching [
29], repetitive motion [
29,
30], and direct force [
30] can also be problematic, such as throwing/dribbling a ball, swinging a bat/racquet, or gripping a club.
Functional Impairments
Motor deficits from ulnar nerve compression can be subtle and masked by compensatory behaviors; despite a normal appearance, function can be greatly impacted (see
Table 1C for common impairments). Normal-appearing grasp and prehension patterns are achievable, but the hand lacks the strength and power to secure, stabilize and manipulate – a focused clinical history can reveal such deficits. Functionally, clients can make a fist but struggle with generating sufficient force for a tight squeeze. For example, the power grip needed to wring water from a sponge or twist open a jar is suboptimal. Dropping objects and complaints of hand weakness are common. While various pinch positions are possible, the strength needed to stabilize a pinched object for manipulation is absent. The client may be able to clasp a key between their thumb and lateral index finger (i.e., a lateral pinch) but unable to exert the strength and force needed to insert and turn the key in the lock. In addition, the client may be able to hold a pen to paper but struggle to maintain stability when writing; holding a fork and knife may be possible, but the utensils slide from the client’s grip when pressing down to cut food. Attending to subtle deficits such as these can help in securing the correct diagnosis.
From a physical standpoint, the hand cannot fully open, as the small and ring finger proximal interphalangeal (PIP) joints remain flexed to some degree. This impedes the hand’s ability to successfully perform tasks with a flat palm. Clients often describe their fingers as “catching” and/or “tangling” when performing open-handed tasks such as reaching into pants pockets, wiping a kitchen counter, smoothing bed linens, or folding laundry. They also report difficulty with facial grooming such as poking oneself while applying makeup or lotion. Dexterous motions, such as opening/closing a resealable bag, lathering a bar of soap, buttoning clothes, and hand-sewing, are also challenging [
31]. Small objects like pills and vitamins often slip out of the ulnar side of the hand when attempting to secure them in a cupped palm. Asking clients about similar fine motor tasks will assist in determining if the ulnar nerve is compromised. In addition, in-hand-manipulation skills, such as translating and shifting objects between the palm and fingers, may also be impacted; this can be easily assessed in the clinic using the Corbett Targeted Coin Test [
32].
Case Description
This case illustrates the importance of providers’ ability to recognize early signs of ulnar nerve compression and willingness to involve a certified hand therapist (CHT) as part of the rehabilitation team. In July of 2022, a healthy active 90-year-old female fell at work onto her outstretched arm, sustaining a distal radius fracture. She was treated conservatively with a removable wrist splint under the care of a general orthopedic surgeon. 7 weeks post-injury, she experienced neurogenic symptoms so severe that she presented to the emergency department. After ruling out the central nervous system as the cause of her numbness, pain and weakness, she returned to her surgeon. Magnetic Resonance Imaging and electromyography revealed cervical stenosis as well as peripheral compressions of the median and ulnar nerves. Only two tests were completed during the in-office examination, including a Tinel’s test at the carpal tunnel (which was positive) and a gross hand strength assessment (without focus on isolated muscles). The surgeon focused treatment on the median nerve, and a carpal tunnel release was performed 14 weeks post-injury. Post-operatively, general hand weakness and PIP joint stiffness were noted; care included traditional physical therapy with a plan to return to work in 2 months. After four months of therapy, however, she continued to suffer from hand weakness, PIP joint stiffness, paresthesia, and pain, and was unable to return to work.
After 7 months of failed therapy, the client was evaluated by a CHT (occupational therapist). Findings included diminished sensory perception of all five digits and the ulnar palm as well as visible muscle atrophy of the thumb webspace and Hypothenar Eminence. Structural deficits of a flattened distal transverse palmar arch and PIP joint flexion contractures of the small and ring fingers were noted. Functional complaints consisted of hand weakness, inability to write, and difficulty unlocking her front door. Further assessment revealed inability to maintain grasp of her pen during writing and to press her needle into fabric while sewing. Based on these findings, the CHT suspected ulnar nerve compression and initiated a treatment plan accordingly; custom-designed and fabricated orthotics were used for deformity correction by reinforcing the distal transverse palmar arch, blocking the MCP joints in flexion, and redirecting motor force to the PIP joints to achieve full active motion. Use of the orthotics restored the client’s tissue balance and functional movement patterns.
The CHT recommended that the surgeon consider a diagnosis of ulnar nerve compression given the motor findings and corresponding hand presentation; however, this diagnosis was dismissed in the medical note at the client’s follow-up visit. Due to this, after 6 weeks of hand therapy, the client’s insurance denied continued coverage for hand therapy despite ongoing functional deficits preventing return to work. The client returned to traditional physical therapy under the supervision of the provider for five more months without any amelioration of symptoms, and PIP joint contractures ultimately recurred. Finally, in October 2023, her provider agreed that her symptoms (i.e., parasthesia, targeted muscle weakness, and deformity pattern) may be sequelae of ulnar nerve compression. Accordingly, an ulnar nerve trans-position was completed in November 2023, 16 months post-injury. Parasthesia improved, but weakness and structural changes persisted, likely due to a significantly delayed diagnosis. The client continued to receive physical therapy for 7 more months without change and never returned to work.
This case highlights the long-term consequences of delayed recognition and treatment of ulnar nerve compression, emphasizing the impact of missed early intervention on functional recovery and overall outcomes.
Conclusions
This paper is intended to assist providers in recognizing early signs of ulnar nerve compression and encourage them to refer impacted clients to hand therapy as soon as possible. Access to CHTs will help clients receive the advanced rehabilitation skills needed for delicate functional recovery and for deformity prevention or correction, increasing the likelihood of restored hand performance.
Acknowledgment Statement
None
Disclosures of Potential Conflicts of Interest
None
References
- Goldman, S.B.; Brininger, T.L.; Schrader, J.W.; Koceja, D.M. A review of clinical tests and signs for the assessment of ulnar neuropathy. J Hand Ther. 2009, 22, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Colditz, J. Splinting the hand with a peripheral-nerve injury. Rehabilitation of the hand and upper extremity, 2-volume set.2011:e141-e152.
- Bertelli, J.A. Prior to repair functional deficits in above- and below-elbow ulnar nerve injury. J Hand Surg Am. 2020, 45, e551–e552. [Google Scholar] [CrossRef] [PubMed]
- WebMD Editorial Contributors. What is claw hand deformity? Accessed , 2025. https://www.webmd. 3 March.
- Cleveland Clinic. Claw hand. Accessed , 2025. https://my.clevelandclinic. 3 March 2350.
- American Society for Surgery of the Hand. Cigarettes and hand conditions. Accessed 03/03/2025. https://www.assh.
- National Institutes of Neurological Disorders and Stroke. Peripheral neuropathy. Accessed , 2025. https://www.ninds.nih. 3 March.
- Davis, D.D.; Kane, S.M. Ulnar nerve entrapment. Statpearls, 2025. [Google Scholar]
- Hand Therapy Certification Commission. Definition of hand therapy and scope of practice of certified hand therapists. Accessed , 2025. https://www.htcc.org/docs/default-source/about/htcc-definition-and-sop.pdf? 3 March 8371.
- Ramdharry, G. Peripheral nerve disease. Handb Clin Neurol. 2018, 159, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Bartels, R.H.; Verbeek, A.L. Risk factors for ulnar nerve compression at the elbow: A case control study. Acta Neurochir (Wien). 2007, 149, 669–674. [Google Scholar] [CrossRef]
- Węgiel, A.; Zielinska, N.; Tubbs, R.S.; Olewnik, Ł. Possible points of compression of the ulnar nerve: Tricks and traps that await clinicians from an anatomical point of view. Clin Anat. 2022, 35, 155–173. [Google Scholar] [CrossRef]
- Shin, R.; Ring, D. The ulnar nerve in elbow trauma. J Bone Joint Surg Am. 2007, 89, 1108–1116. [Google Scholar] [CrossRef]
- Osei, D.A.; Groves, A.P.; Bommarito, K.; Ray, W.Z. Cubital tunnel syndrome: Incidence and demographics in a national administrative database. Neurosurgery. 2017, 80, 417–420. [Google Scholar] [CrossRef]
- Mendelaar NHA, Hundepool, C. A.; Hoogendam, L.; et al. Multiple compression syndromes of the same upper extremity: Prevalence, risk factors, and treatment outcomes of concomitant treatment. J Hand Surg Am. 2023, 48, 479–488. [Google Scholar] [CrossRef]
- Doughty, C.T.; Bowley, M.P. Entrapment neuropathies of the upper extremity. Med Clin North Am. 2019, 103, 357–370. [Google Scholar] [CrossRef]
- Freund, G.; Dafotakis, M.; Bahm, J.; Beier, J.P. Treatment of peripheral nerve compression syndromes of the upper extremities: A systematic review. Z Orthop Unfall. 2023, 161, 182–194. [Google Scholar] [CrossRef]
- Nyman, E.; Dahlin, L.B. The unpredictable ulnar nerve-ulnar nerve entrapment from anatomical, pathophysiological, and biopsychosocial aspects. Diagnostics (Basel). 2024, 14, 10.3390–diagnostics14050489. [Google Scholar] [CrossRef] [PubMed]
- Dy, C.J.; Mackinnon, S.E. Ulnar neuropathy: Evaluation and management. Curr Rev Musculoskelet Med. 2016, 9, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Asif, N.; Singh, P.N.; Hossain, M.M. Motor nerve conduction velocity in postmenopausal women with peripheral neuropathy. J Clin Diagn Res, c: 10, 7860. [Google Scholar]
- Massey, E.W.; Guidon, A.C. Peripheral neuropathies in pregnancy. Continuum (Minneap Minn). 2014, 20, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Elma, Ö.; Brain, K.; Dong, H.J. The importance of nutrition as a lifestyle factor in chronic pain management: A narrative review. J Clin Med. 2022, 11, 10.3390–jcm11195950. [Google Scholar] [CrossRef]
- Şah, V.; Baydar, C.; Örün, M.; Elasan, S. The relationship between entrapment level of the nerve and upper extremity function and sleep quality in ulnar neuropathy patients. Eastern Journal Of Medicine. 2024, 29, 509–517. [Google Scholar] [CrossRef]
- Brain, K.; Burrows, T.L.; Rollo, M.E.; Collins, C.E. Nutrition and chronic pain. Accessed , 2025. https://www.iasp-pain. 3 March.
- The Foundation for Peripheral Neuropathy. Nutritional and vitamin deficiency neuropathy. Accessed , 2025. https://www.foundationforpn. 3 March.
- Crosby, N.E.; Nosrati, N.N.; Merrell, G.; Hasting, H.; 2nd. Relationship between smoking and outcomes after cubital tunnel release. J Hand Microsurg. 2018, 10, 12–15. [Google Scholar] [CrossRef]
- Richardson, J.K.; Ho, S.; Wolf, J.; Spiegelberg, T. The nature of the relationship between smoking and ulnar neuropathy at the elbow. Am J Phys Med Rehabil. 2009, 88, 711–718. [Google Scholar] [CrossRef]
- Brown, T.J.; Sedhom, R.; Gupta, A. Chemotherapy-induced peripheral neuropathy. JAMA Oncol. 2019, 5, 750. [Google Scholar] [CrossRef]
- Chauhan, M.; Anand, P.; Das, J.M. Cubital tunnel syndrome. Statpearls, 2025. [Google Scholar]
- Frost, P.; Johnsen, B.; Fuglsang-Frederiksen, A.; Svendsen, S.W. Lifestyle risk factors for ulnar neuropathy and ulnar neuropathy-like symptoms. Muscle Nerve. 2013, 48, 507–515. [Google Scholar] [CrossRef]
- McCormick, C.A.; Rath, S.; Patra, P.N.; Pereira, J.; Wilkinson, M. A qualitative study of common functional problems experienced by people with complete ulnar nerve paralysis. Lepr Rev. 2008, 79, 154–161. [Google Scholar] [CrossRef]
- Grice, K.O.; Almeida, G.J. The corbett targeted coin test: Reliability, criterion related validity, and normative data. J Hand Ther. 2024, 37, 371–377. [Google Scholar] [CrossRef]
- Hagert, E. ; Hagert C-G. Manual muscle testing—a clinical examination technique for diagnosing focal neuropathies in the upper extremity. Upper extremity nerve repair - tips and techniques: A master skills publication. 2008:451-466.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).