Submitted:
19 March 2025
Posted:
19 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Pulmonary Fungal Infections
- A. Pulmonary Aspergillosis
2.1. Allergic Bronchopulmonary Aspergillosis (ABPA)
2.2. Invasive Pulmonary Aspergillosis (IPA)
2.3. Chronic Pulmonary Aspergillosis (CPA):
- Aspergillus nodules,
- Simple Aspergilloma,
- Chronic Cavitary Pulmonary Aspergillosis
- Subacute Invasive Pulmonary Aspergillosis,
- Chronic Fibrosing Pulmonary Aspergillosis
2.4. Aspergillus Nodules
2.5. Aspergilloma
2.6. Chronic Cavitary Pulmonary Aspergillosis (CCPA)
2.7. Subacute Invasive Pulmonary Aspergillosis (SAIA)
2.8. Chronic Fibrosing Pulmonary Aspergillosis (CFPA)
2.9. Pulmonary Cryptococcosis
2.10. Pneumocystis Pneumonia
2.11. Pulmonary Blastomycosis
2.12. Pulmonary Coccidioidomycosis
2.13. Pulmonary Histoplasmosis
2.14. Pulmonary Candidiasis
2.15. Pulmonary Mucormycosis
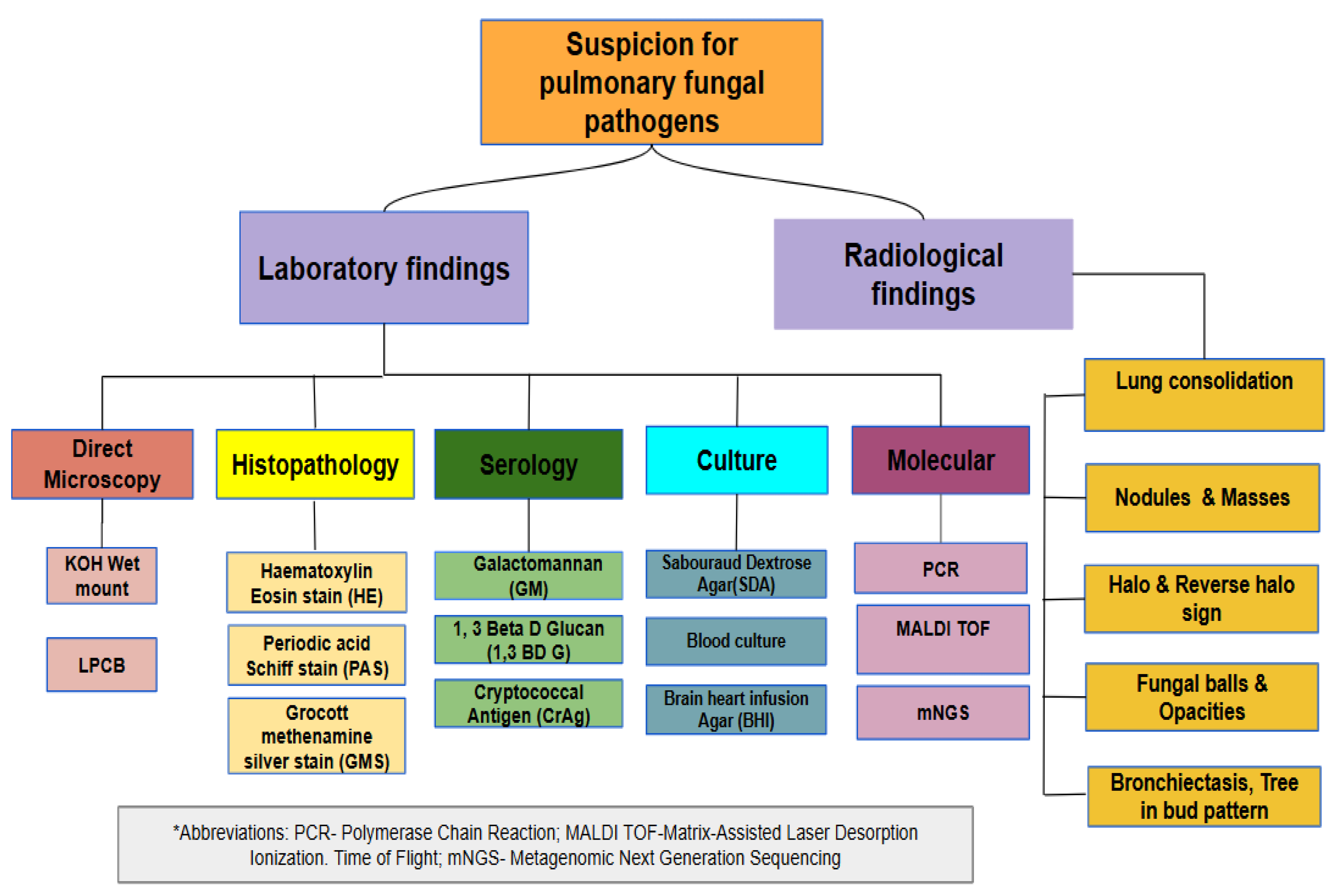
3. Diagnosis
3.1. Direct microscopy & Histopathological Examination
3.2. Radiology
3.3. Culture
3.4. Immunology
3.5. Molecular Diagnosis
3.6. Metagenomic Next Generation Sequencing (mNGS)
3.7. Matrix Assisted Laser Desorption Ionisation-Time of Flight Mass Spectrometry (MALDI TOF MS)
3.8. Antifungal Therapy
4. Conclusions
Conflicts of Interest
References
- “Global Tuberculosis Report 2023.” [Online]. Available: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023. [Accessed: 28-Aug-2024].
- J. Singh, A. Dinkar, and P. Gupta, “Uncommon manifestations in tuberculosis: An expanding clinical spectrum from North India.,” Int. J. Mycobacteriol., vol. 11, no. 1, pp. 30–37, 2022. [CrossRef]
- A. Bitew and S. Bati, “Profiling of potential pulmonary fungal pathogens and the prevalence of the association between pulmonary tuberculosis and potential fungal pathogens in presumptive tuberculosis patients referred to Saint Peter’s Specialized Tuberculosis Referral Hospital, Addis Ababa, Ethiopia.,” SAGE Open Med., vol. 9, p. 20503121211056164, Nov. 2021. [CrossRef]
- S. Muni et al., “Identification of fungal isolates in patients with pulmonary tuberculosis treated at a tertiary care hospital.,” Cureus, vol. 15, no. 4, p. e37664, Apr. 2023. [CrossRef]
- Z. Li, G. Lu, and G. Meng, “Pathogenic fungal infection in the lung.,” Front. Immunol., vol. 10, p. 1524, Jul. 2019. [CrossRef]
- B. T. Kelly, K. M. Pennington, and A. H. Limper, “Advances in the diagnosis of fungal pneumonias.,” Expert Rev. Respir. Med., vol. 14, no. 7, pp. 703–714, Jul. 2020. [CrossRef]
- X. Yan et al., “Pulmonary Fungal Diseases in Immunocompetent Hosts: A Single-Center Retrospective Analysis of 35 Subjects.,” Mycopathologia, vol. 181, no. 7–8, pp. 513–521, Aug. 2016. [CrossRef]
- A. P. Campbell et al., “Endemic mycoses in children in North America: a review of radiologic findings.,” Pediatr. Radiol., vol. 53, no. 5, pp. 984–1004, May 2023. [CrossRef]
- W. Seo, H. W. Kim, J. S. Kim, and J. Min, “Long term management of people with post-tuberculosis lung disease.,” Korean J. Intern. Med., vol. 39, no. 1, pp. 7–24, Jan. 2024. [CrossRef]
- B. E. Ekeng, A. A. Davies, I. I. Osaigbovo, A. Warris, R. O. Oladele, and D. W. Denning, “Pulmonary and extrapulmonary manifestations of fungal infections misdiagnosed as tuberculosis: the need for prompt diagnosis and management.,” J Fungi (Basel), vol. 8, no. 5, Apr. 2022. [CrossRef]
- A. Kanj, N. Abdallah, and A. O. Soubani, “The spectrum of pulmonary aspergillosis.,” Respir. Med., vol. 141, pp. 121–131, Aug. 2018. [CrossRef]
- R. Agarwal et al., “Allergic bronchopulmonary aspergillosis.,” Indian J. Med. Res., vol. 151, no. 6, pp. 529–549, Jun. 2020. [CrossRef]
- S. Ueki, A. Hebisawa, M. Kitani, K. Asano, and J. S. Neves, “Allergic Bronchopulmonary Aspergillosis-A Luminal Hypereosinophilic Disease With Extracellular Trap Cell Death.,” Front. Immunol., vol. 9, p. 2346, Oct. 2018. [CrossRef]
- P. A. Grenier, A. L. Brun, E. Longchampt, M. Lipski, F. Mellot, and E. Catherinot, “Primary immunodeficiency diseases of adults: a review of pulmonary complication imaging findings.,” Eur. Radiol., vol. 34, no. 6, pp. 4142–4154, Jun. 2024. [CrossRef]
- S. Khan et al., “Distribution of Aspergillus species and risk factors for aspergillosis in mainland China: a systematic review.,” Ther. Adv. Infect. Dis., vol. 11, p. 20499361241252536, Jun. 2024. [CrossRef]
- J. Heylen, Y. Vanbiervliet, J. Maertens, B. Rijnders, and J. Wauters, “Acute invasive pulmonary aspergillosis: clinical presentation and treatment.,” Semin. Respir. Crit. Care Med., vol. 45, no. 1, pp. 69–87, Feb. 2024. [CrossRef]
- S.-H. Kim et al., “Invasive Pulmonary Aspergillosis-mimicking Tuberculosis.,” Clin. Infect. Dis., vol. 61, no. 1, pp. 9–17, Jul. 2015. [CrossRef]
- M. H. van der Torre, H. Shen, R. Rautemaa-Richardson, M. D. Richardson, and L. Novak-Frazer, “Molecular Epidemiology of Aspergillus fumigatus in Chronic Pulmonary Aspergillosis Patients.,” J Fungi (Basel), vol. 7, no. 2, Feb. 2021. [CrossRef]
- C. Kosmidis, “Special issue: chronic pulmonary aspergillosis.,” J Fungi (Basel), vol. 8, no. 7, Jul. 2022. [CrossRef]
- D. W. Denning, D. C. Cole, and A. Ray, “New estimation of the prevalence of chronic pulmonary aspergillosis (CPA) related to pulmonary TB - a revised burden for India.,” IJID Reg., vol. 6, pp. 7–14, Mar. 2023. [CrossRef]
- A. Zarif, A. Thomas, and A. Vayro, “Chronic pulmonary aspergillosis: A brief review.,” Yale J. Biol. Med., vol. 94, no. 4, pp. 673–679, Dec. 2021.
- D. Jha et al., “Chronic pulmonary aspergillosis incidence in newly detected pulmonary tuberculosis cases during follow-up.,” Mycoses, vol. 67, no. 5, p. e13747, May 2024. [CrossRef]
- N. K. Chirumamilla et al., “Innate and adaptive immune responses in subjects with CPA secondary to post-pulmonary tuberculosis lung abnormalities.,” Mycoses, vol. 67, no. 5, p. e13746, May 2024. [CrossRef]
- R. Rajpurohit, P. Wagh, M. Heda, G. Dubey, and P. S. Gujar, “Prevalence of chronic pulmonary aspergillosis in fibrocavitary pulmonary tuberculosis patients.,” J. Family Med. Prim. Care, vol. 12, no. 1, pp. 106–110, Jan. 2023. [CrossRef]
- B. G. Bharath et al., “Diagnostic utility of chest computerized tomography in the diagnosis of recurrence among sputum scarce and sputum negative previously treated pulmonary tuberculosis suspects.,” Lung India, vol. 39, no. 2, pp. 145–151, 2022. [CrossRef]
- I. S. Sehgal et al., “Role of C-Reactive Protein and Erythrocyte Sedimentation Rate in the Diagnosis and Monitoring of Treatment Response in Treatment Naïve Subjects with Chronic Pulmonary Aspergillosis.,” Mycopathologia, vol. 188, no. 5, pp. 705–711, Oct. 2023. [CrossRef]
- R. Lahiri, I. Jhalani, A. Kumar, and A. G. Goswami, “Successful management of delayed postoperative lung collapse secondary to spillage of aspergilloma.,” BMJ Case Rep., vol. 16, no. 7, Jul. 2023. [CrossRef]
- A. Gandotra et al., “Invasive Pulmonary Aspergillosis and Tuberculosis Complicated by Hemophagocytic Lymphohistiocytosis - Sequelae of COVID-19 in a Liver Transplant Recipient.,” J. Clin. Exp. Hepatol., vol. 12, no. 3, pp. 1007–1011, 2022. [CrossRef]
- S. Chaurasia, M. Thimmappa, and S. Chowdhury, “Case Report: Chronic Cavitatory Pulmonary Aspergillosis after COVID-19.,” Am. J. Trop. Med. Hyg., vol. 106, no. 1, pp. 105–107, Nov. 2021. [CrossRef]
- S. Dong, F. Wang, H. Jin, and X. Dai, “Five cases of pulmonary Aspergillus nodules diagnosed at surgery and by pathology in immunocompetent patients, with a literature review.,” Therapeutic Advances in Rare Disease, vol. 5, p. 26330040241252450, May 2024. [CrossRef]
- H. Zhong et al., “Clinical features, diagnostic test performance, and prognosis in different subtypes of chronic pulmonary aspergillosis.,” Front Med (Lausanne), vol. 9, p. 811807, Feb. 2022. [CrossRef]
- R. K. Chakraborty, T. S. Gilotra, E. H. Tobin, and K. M. Baradhi, “Aspergilloma,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2024.
- F. Lamoth and T. Calandra, “Pulmonary aspergillosis: diagnosis and treatment.,” Eur. Respir. Rev., vol. 31, no. 166, Dec. 2022. [CrossRef]
- A. Pekçolaklar, N. Çıtak, Y. Aksoy, V. Erdoğu, and M. Metin, “Is there any change in disease presentation and surgical outcomes in patients with pulmonary aspergilloma? An evaluation of the time trend.,” Turk Gogus Kalp Damar Cerrahisi Dergisi, vol. 30, no. 2, pp. 241–249, Apr. 2022. [CrossRef]
- A. Uzair, M. Waseem, N. I. Bhatti, Z. Toor, A. Ishaq, and O. Ahmad, “Chronic cavitary pulmonary aspergillosis as a sequela of pulmonary tuberculosis: A case report from Pakistan.,” SAGE Open Med. Case Rep., vol. 12, p. 2050313X241251777, May 2024. [CrossRef]
- I. Izumikawa et al., “Pathogenesis and clinical features of chronic pulmonary aspergillosis - is it possible to distinguish CNPA and CCPA clinically?,” J. Infect. Chemother., vol. 20, no. 3, pp. 208–212, Mar. 2014. [CrossRef]
- M. Garg et al., “Imaging spectrum in chronic pulmonary aspergillosis.,” Am. J. Trop. Med. Hyg., vol. 108, no. 1, pp. 15–21, Jan. 2023. [CrossRef]
- S.-F. Huang, C.-C. Huang, K.-T. Chou, Y.-J. Chan, Y.-Y. Yang, and F.-D. Wang, “Chronic Pulmonary Aspergillosis: Disease Severity Using Image Analysis and Correlation with Systemic Proinflammation and Predictors of Clinical Outcome.,” J Fungi (Basel), vol. 7, no. 10, Oct. 2021. [CrossRef]
- T. Wang, M. Liu, and F. Zhang, “Clinical diagnosis, treatment, and laboratory detection of 50 cases of pulmonary cryptococcosis.,” Comput. Math. Methods Med., vol. 2022, p. 7981472, Jul. 2022. [CrossRef]
- S. E. Kidd, A. Abdolrasouli, and F. Hagen, “Fungal nomenclature: managing change is the name of the game.,” Open Forum Infect. Dis., vol. 10, no. 1, p. ofac559, Jan. 2023. [CrossRef]
- I. J. Kwon-Chung et al., “Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis.,” Cold Spring Harb. Perspect. Med., vol. 4, no. 7, p. a019760, Jul. 2014. [CrossRef]
- J. Qu, X. Zhang, Y. Lu, X. Liu, and X. Lv, “Clinical analysis in immunocompetent and immunocompromised patients with pulmonary cryptococcosis in western China.,” Sci. Rep., vol. 10, no. 1, p. 9387, Jun. 2020. [CrossRef]
- P. Meena et al., “Cryptococcosis masquerading as disseminated tuberculosis in a patient on chronic hemodialysis.,” Saudi J. Kidney Dis. Transpl., vol. 30, no. 5, pp. 1179–1183, Oct. 2019. [CrossRef]
- N. Adsul et al., “Thoracic cryptococcal osteomyelitis mimicking tuberculosis: A case report.,” Surg. Neurol. Int., vol. 10, p. 81, May 2019. [CrossRef]
- J. Ismail, M. Chidambaram, J. Sankar, S. Agarwal, and R. Lodha, “Disseminated cryptococcosis presenting as miliary lung shadows in an immunocompetent child.,” J. Trop. Pediatr., vol. 64, no. 5, pp. 434–437, Oct. 2018. [CrossRef]
- S. Jain, V. Mahajan, and A. Kumar, “Unusual case of coexistent pulmonary cryptococcosis and tuberculosis in an immuno-competent host.,” Indian J. Tuberc., vol. 64, no. 3, pp. 228–231, Jul. 2017. [CrossRef]
- S. Pawar et al., “Pulmonary cryptococcoma masquerading as lung cancer.,” J. Assoc. Physicians India, vol. 64, no. 5, pp. 66–68, May 2016.
- S. Sharma, P. Gupta, N. Gupta, A. Lal, D. Behera, and A. Rajwanshi, “Pulmonary infections in immunocompromised patients: the role of image-guided fine needle aspiration cytology.,” Cytopathology, vol. 28, no. 1, pp. 46–54, Feb. 2017. [CrossRef]
- P. Ranjan, M. Jana, S. Krishnan, D. Nath, and R. Sood, “Disseminated cryptococcosis with adrenal and lung involvement in an immunocompetent patient.,” J. Clin. Diagn. Res., vol. 9, no. 4, pp. OD04-5, Apr. 2015. [CrossRef]
- Z. Rafat et al., “The mycological and molecular study of Pneumocystis jiroveci pneumonia among HIV and non-HIV immunocompromised patients hospitalized in pulmonary units in Guilan, Northern Iran.,” Iran. J. Microbiol., vol. 13, no. 4, pp. 518–524, Aug. 2021. [CrossRef]
- H.-Y. Lee, C.-Y. Lu, P.-I. Lee, J.-M. Chen, L.-M. Huang, and L.-Y. Chang, “Pneumocystis jiroveci pneumonia in Taiwan from 2014 to 2017: Clinical manifestations and outcomes between pediatric and adult patients.,” J. Microbiol. Immunol. Infect., vol. 52, no. 6, pp. 983–990, Dec. 2019. [CrossRef]
- A. Apostolopoulou and J. A. Fishman, “The Pathogenesis and Diagnosis of Pneumocystis jiroveci Pneumonia.,” J Fungi (Basel), vol. 8, no. 11, Nov. 2022. [CrossRef]
- I. Bateman, R. Oladele, and J. K. Kolls, “Diagnosing Pneumocystis jirovecii pneumonia: A review of current methods and novel approaches.,” Med. Mycol., vol. 58, no. 8, pp. 1015–1028, Nov. 2020. [CrossRef]
- S. Pandey, S. Ghosh, P. Halder, D. Pal, D. C. Modak, and S. K. Guha, “Pulmonary tuberculosis and pneumocystis jirovecii concurrent pneumonia in HIV infected patients at a resource limited setting in Eastern India: A case series.,” Indian J. Tuberc., vol. 67, no. 3, pp. 378–382, Jul. 2020. [CrossRef]
- J. G, S. Narayanan, S. Kumar, M. Banjade, and M. Bairwa, “Spontaneous pneumothorax, pneumomediastinum, and pneumopericardium in an HIV patient with tuberculosis: A rare trio.,” Cureus, vol. 16, no. 4, p. e58440, Apr. 2024. [CrossRef]
- V. C. Patil and H. V. Patil, “Clinical manifestations and outcome of patients with human immunodeficiency virus infection at tertiary care teaching hospital.,” Indian J. Sex. Transm. Dis., vol. 37, no. 1, pp. 38–45, Jun. 2016. [CrossRef]
- P. Indira, P. M. Kumar, S. Shalini, and K. Vaman, “Opportunistic Infections among People Living with HIV (PLHIV) with Diabetes Mellitus (DM) Attending a Tertiary Care Hospital in Coastal City of South India.,” PLoS ONE, vol. 10, no. 8, p. e0136280, Aug. 2015. [CrossRef]
- K. Ramesh, S. Gandhi, and V. Rao, “Clinical profile of human immunodeficiency virus patients with opportunistic infections: A descriptive case series study.,” Int. J. Appl. Basic Med. Res., vol. 5, no. 2, pp. 119–123, Aug. 2015. [CrossRef]
- F. Bongomin et al., “Invasive fungal diseases in africa: A critical literature review.,” J Fungi (Basel), vol. 8, no. 12, Nov. 2022. [CrossRef]
- A. Goico, J. Henao, and K. Tejada, “Disseminated blastomycosis in a 36-year-old immunocompetent male from Chicago, IL.,” Oxf. Med. Case Reports, vol. 2018, no. 10, p. omy071, Oct. 2018. [CrossRef]
- T. G. Maphanga et al., “Human Blastomycosis in South Africa Caused by Blastomyces percursus and Blastomyces emzantsi sp. nov., 1967 to 2014.,” J. Clin. Microbiol., vol. 58, no. 3, Feb. 2020. [CrossRef]
- F. Bongomin and S. Adetona Fayemiwo, “Epidemiology of fungal diseases in Africa: A review of diagnostic drivers.,” Curr. Med. Mycol., vol. 7, no. 1, pp. 63–70, Mar. 2021. [CrossRef]
- F. C. B. Abdallah et al., “[Pulmonary blastomycosis].,” Pan Afr. Med. J., vol. 36, p. 220, Jul. 2020. [CrossRef]
- I. Wang, Z. Luo, S. Deng, and Q. Li, “A young male with chronic nonproductive cough diagnosed with blastomycosis in China: a case report.,” BMC Pulm. Med., vol. 20, no. 1, p. 189, Jul. 2020. [CrossRef]
- A. Kumar, A. Kunoor, M. Eapen, P. K. Singh, and A. Chowdhary, “Blastomycosis misdiagnosed as tuberculosis, india.,” Emerging Infect. Dis., vol. 25, no. 9, pp. 1776–1777, 2019. [CrossRef]
- R. Cordeiro, S. Moura, D. Castelo-Branco, M. F. Rocha, R. Lima-Neto, and J. J. Sidrim, “Coccidioidomycosis in brazil: historical challenges of a neglected disease.,” J Fungi (Basel), vol. 7, no. 2, Jan. 2021. [CrossRef]
- N. F. Crum, “Coccidioidomycosis: A contemporary review.,” Infect. Dis. Ther., vol. 11, no. 2, pp. 713–742, Apr. 2022. [CrossRef]
- J. W. Taylor and B. M. Barker, “The endozoan, small-mammal reservoir hypothesis and the life cycle of Coccidioides species.,” Med. Mycol., vol. 57, no. Supplement_1, pp. S16–S20, Feb. 2019. [CrossRef]
- R. H. Johnson, R. Sharma, R. Kuran, I. Fong, and A. Heidari, “Coccidioidomycosis: a review.,” J. Investig. Med., vol. 69, no. 2, pp. 316–323, Feb. 2021. [CrossRef]
- A. M. Scott et al., “Examining Miliary Disease Etiology in a Coccidioides-Endemic Center: A Retrospective Cohort Study.,” J Fungi (Basel), vol. 10, no. 1, Dec. 2023. [CrossRef]
- K. Sri, A. Vaithy, S. Kathirvelu, and S. Srinivasan, “Coccidioidomycosis lymphadenopathy: an unusual presentation.,” BMJ Case Rep., vol. 16, no. 7, Jul. 2023. [CrossRef]
- D. H. Caceres and A. Valdes, “Histoplasmosis and Tuberculosis Co-Occurrence in People with Advanced HIV.,” J Fungi (Basel), vol. 5, no. 3, Aug. 2019. [CrossRef]
- M. P. N. Kuate, B. E. Ekeng, R. Kwizera, C. Mandengue, and F. Bongomin, “Histoplasmosis overlapping with HIV and tuberculosis in sub-Saharan Africa: challenges and research priorities.,” Ther. Adv. Infect. Dis., vol. 8, p. 20499361211008676, Apr. 2021. [CrossRef]
- J. Baker, C. Kosmidis, A. Rozaliyani, R. Wahyuningsih, and D. W. Denning, “Chronic Pulmonary Histoplasmosis-A Scoping Literature Review.,” Open Forum Infect. Dis., vol. 7, no. 5, p. ofaa119, May 2020. [CrossRef]
- M. Nacher et al., “A Simple Predictive Score to Distinguish between Disseminated Histoplasmosis and Tuberculosis in Patients with HIV.,” J Fungi (Basel), vol. 8, no. 1, Dec. 2021. [CrossRef]
- A. E. Ekeng, R. O. Oladele, U. E. Emanghe, E. A. Ochang, and T. Y. Mirabeau, “Prevalence of Histoplasmosis and Molecular Characterization of Histoplasma species in Patients with Presumptive Pulmonary Tuberculosis in Calabar, Nigeria.,” Open Forum Infect. Dis., vol. 9, no. 8, p. ofac368, Aug. 2022. [CrossRef]
- M. Agarwal and B. J. Shadrach, “Acute pulmonary histoplasmosis masquerading as miliary tuberculosis in a non-endemic region.,” Adv. Respir. Med., vol. 89, no. 4, pp. 464–465, Jul. 2021. [CrossRef]
- K. Anot, S. Sharma, M. Gupta, and D. Kaur, “Disseminated histoplasmosis and tuberculosis: dual infection in a non-endemic region.,” BMJ Case Rep., vol. 13, no. 8, Aug. 2020. [CrossRef]
- V. Dutta, M. Chopra, U. B. Kovilapu, and G. P. S. Gahlot, “Solitary pulmonary nodule: An interesting clinical mimicry of pulmonary tuberculosis.,” Med. J. Armed Forces India, vol. 75, no. 1, pp. 115–118, Jan. 2019. [CrossRef]
- V. Ramesh, S. Narreddy, S. Gowrishankar, R. Barigala, and S. Nanda, “A challenging case of pyrexia of unknown origin: adrenal histoplasmosis mimicking tuberculosis in a patient with chronic hepatitis C.,” Trop. Doct., vol. 51, no. 4, pp. 621–623, Oct. 2021. [CrossRef]
- M. Astekar, P. S. Bhatiya, and G. V. Sowmya, “Prevalence and characterization of opportunistic candidal infections among patients with pulmonary tuberculosis.,” J. Oral Maxillofac. Pathol., vol. 20, no. 2, pp. 183–189, 2016. [CrossRef]
- A. Azim and A. Ahmed, “Diagnosis and management of invasive fungal diseases in non-neutropenic ICU patients, with focus on candidiasis and aspergillosis: a comprehensive review.,” Front. Cell. Infect. Microbiol., vol. 14, p. 1256158, Mar. 2024. [CrossRef]
- Y. Shweihat, J. Perry, and D. Shah, “Isolated Candida infection of the lung.,” Respir. Med. Case Rep., vol. 16, pp. 18–19, Mar. 2015. [CrossRef]
- M. Hadadi-Fishani, A. Shakerimoghaddam, and A. Khaledi, “Candida coinfection among patients with pulmonary tuberculosis in Asia and Africa; A systematic review and meta-analysis of cross-sectional studies.,” Microb. Pathog., vol. 139, p. 103898, Feb. 2020. [CrossRef]
- R. Khanduri, S. Khanduri, S. Kumar, A. Saini, and A. Kotwal, “Drug-resistant tuberculosis coexisting with invasive candidiasis in an immunocompetent 30-year-old woman: A case report.,” Indian J. Tuberc., vol. 64, no. 3, pp. 232–234, Jul. 2017. [CrossRef]
- A. Kumar, C. Agarwal, A. K. Hooda, A. Ojha, M. Dhillon, and K. V. S. Hari Kumar, “Profile of infections in renal transplant recipients from India.,” J. Family Med. Prim. Care, vol. 5, no. 3, pp. 611–614, 2016. [CrossRef]
- J. Bao et al., “Clinical Manifestations of Pulmonary Mucormycosis in Recipients of Allogeneic Hematopoietic Stem Cell Transplantation: A 21-Case Series Report and Literature Review.,” Can. Respir. J., vol. 2022, p. 1237125, Jun. 2022. [CrossRef]
- H. Prakash and A. Chakrabarti, “Global epidemiology of mucormycosis.,” J. Fungi, vol. 5, no. 1, Mar. 2019. [CrossRef]
- R. Agrawal, A. Yeldandi, H. Savas, N. D. Parekh, P. J. Lombardi, and E. M. Hart, “Pulmonary mucormycosis: risk factors, radiologic findings, and pathologic correlation.,” Radiographics, vol. 40, no. 3, pp. 656–666, Mar. 2020. [CrossRef]
- A. Aggarwal, J. Chander, A. K. Janmeja, and R. Katyal, “Pulmonary tuberculosis and mucormycosis co-infection in a diabetic patient.,” Lung India, vol. 32, no. 1, pp. 53–55, 2015. [CrossRef]
- P. Dube, R. Saroa, and S. Palta, “Coinfections in Intensive Care Unit with pulmonary tuberculosis and mucormycosis: A clinical dilemma.,” Indian J. Crit. Care Med., vol. 20, no. 3, pp. 191–193, Mar. 2016. [CrossRef]
- J. Ramesh, G. Kaur, D. Deepak, and P. Kumar, “Disseminated pulmonary mucormycosis with concomitant tuberculosis infection in a diabetic patient.,” Int. J. Mycobacteriol., vol. 9, no. 1, pp. 95–97, 2020. [CrossRef]
- L. Ramachandran, S. Dewan, V. Kumar, and B. Wankhade, “Mucormycosis causing pulmonary artery aneurysm.,” Respir. Med. Case Rep., vol. 16, pp. 71–73, Jul. 2015. [CrossRef]
- “WHO fungal priority pathogens list to guide research, development and public health action.” [Online]. Available: https://www.who.int/publications/i/item/9789240060241. [Accessed: 05-Oct-2024].
- A. Mendonça, H. Santos, R. Franco-Duarte, and P. Sampaio, “Fungal infections diagnosis - Past, present and future.,” Res. Microbiol., vol. 173, no. 3, p. 103915, 2022. [CrossRef]
- O. A. Cornely et al., “Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium.,” Lancet Infect. Dis., vol. 19, no. 12, pp. e405–e421, Dec. 2019. [CrossRef]
- S. N. Baxi, M. R. Gohil, A. J. Navadiya, M. K. Bapodra, and H. R. Patel, “Comparative evaluation of histopathological analysis, KOH wet mount and fungal culture to diagnose fungal infections in post-COVID patients.,” Indian J. Pathol. Microbiol., vol. 66, no. 3, pp. 540–544, 2023. [CrossRef]
- R. Jandial, M. Choudhary, and K. Singh, “Histomorphological spectrum of fungal infections,” Int. J. Res. Med. Sci., vol. 7, no. 11, p. 4166, Oct. 2019. [CrossRef]
- R. Seth, I. Xess, and M. Jana, “Diagnosis of invasive fungal infections in children.,” Indian Pediatr., vol. 56, no. 3, pp. 229–236, Mar. 2019. [CrossRef]
- A. Vaishnav, G. Gurukiran, O. Ighodaro, and V. Kandi, “Radiological and imaging evidence in the diagnosis and management of microbial infections: an update.,” Cureus, vol. 15, no. 11, p. e48756, Nov. 2023. [CrossRef]
- Z. Ahmad, S. Bagchi, P. Naranje, S. K. Agarwal, and C. J. Das, “Imaging spectrum of pulmonary infections in renal transplant patients.,” Indian J. Radiol. Imaging, vol. 30, no. 3, pp. 273–279, Oct. 2020. [CrossRef]
- S. B. Grover, H. Grover, N. Antil, S. Patra, M. K. Sen, and D. Nair, “Imaging approach to pulmonary infections in the immunocompromised patient.,” Indian J. Radiol. Imaging, vol. 32, no. 1, pp. 81–112, Mar. 2022. [CrossRef]
- P. Ramanan, N. L. Wengenack, and E. S. Theel, “Laboratory diagnostics for fungal infections: A review of current and future diagnostic assays.,” Clin. Chest Med., vol. 38, no. 3, pp. 535–554, May 2017. [CrossRef]
- A. K. Ghosh, A. Gupta, S. M. Rudramurthy, S. Paul, V. K. Hallur, and A. Chakrabarti, “Fungal keratitis in north india: spectrum of agents, risk factors and treatment.,” Mycopathologia, vol. 181, no. 11–12, pp. 843–850, Dec. 2016. [CrossRef]
- www.icmr.gov.in/icmrobject/custom_data/pdf/resource-guidelines/Mycology_SOP_2nd_Ed_2019.pdf.
- C. A. Hage et al., “Microbiological laboratory testing in the diagnosis of fungal infections in pulmonary and critical care practice. an official american thoracic society clinical practice guideline.,” Am. J. Respir. Crit. Care Med., vol. 200, no. 5, pp. 535–550, Sep. 2019. [CrossRef]
- A. Liu et al., “Comparison of diagnostic efficiency of detecting IgG and IgE with immunoassay method in diagnosing ABPA: a meta-analysis.,” BMC Pulm. Med., vol. 23, no. 1, p. 374, Oct. 2023. [CrossRef]
- T. Takazono and K. Izumikawa, “Recent advances in diagnosing chronic pulmonary aspergillosis.,” Front. Microbiol., vol. 9, p. 1810, Aug. 2018. [CrossRef]
- R. Gunasekaran et al., “Rapid Point-of-Care Identification of Aspergillus Species in Microbial Keratitis.,” JAMA Ophthalmol., vol. 141, no. 10, pp. 966–973, Oct. 2023. [CrossRef]
- D. H. Caceres, T. Chiller, and M. D. Lindsley, “Immunodiagnostic assays for the investigation of fungal outbreaks.,” Mycopathologia, vol. 185, no. 5, pp. 867–880, Oct. 2020. [CrossRef]
- R. Gudisa, R. Harchand, and S. M. Rudramurthy, “Nucleic-Acid-Based Molecular Fungal Diagnostics: A Way to a Better Future.,” Diagnostics (Basel), vol. 14, no. 5, Feb. 2024. [CrossRef]
- S. Srinivas, P. Kumari, and D. K. Gupta, “Utility of Panfungal PCR in the diagnosis of invasive fungal infections in febrile neutropenia.,” J. Family Med. Prim. Care, vol. 10, no. 7, pp. 2533–2540, Jul. 2021. [CrossRef]
- V. Poplin, C. Smith, D. Milsap, L. Zabel, and N. C. Bahr, “Diagnosis of pulmonary infections due to endemic fungi.,” Diagnostics (Basel), vol. 11, no. 5, May 2021. [CrossRef]
- Y. Liu, W. Wu, Y. Xiao, H. Zou, S. Hao, and Y. Jiang, “Application of metagenomic next-generation sequencing and targeted metagenomic next-generation sequencing in diagnosing pulmonary infections in immunocompetent and immunocompromised patients.,” Front. Cell. Infect. Microbiol., vol. 14, p. 1439472, Aug. 2024. [CrossRef]
- S. Naik et al., “Utilizing Next-Generation Sequencing: Advancements in the Diagnosis of Fungal Infections.,” Diagnostics (Basel), vol. 14, no. 15, Aug. 2024. [CrossRef]
- A. K. Ghosh et al., “Matrix-assisted laser desorption ionization time-of-flight mass spectrometry for the rapid identification of yeasts causing bloodstream infections.,” Clin. Microbiol. Infect., vol. 21, no. 4, pp. 372–378, Apr. 2015. [CrossRef]
- S. Paul, P. Singh, S. M. Rudramurthy, A. Chakrabarti, and A. K. Ghosh, “Matrix-assisted laser desorption/ionization-time of flight mass spectrometry: protocol standardization and database expansion for rapid identification of clinically important molds.,” Future Microbiol., vol. 12, pp. 1457–1466, Dec. 2017. [CrossRef]
- M. Roy, S. Karhana, M. Shamsuzzaman, and M. A. Khan, “Recent drug development and treatments for fungal infections.,” Braz. J. Microbiol, vol. 54, no. 3, pp. 1695–1716, Sep. 2023. [CrossRef]
- L. Guo et al., “Clinical Characteristics and the Prognostic Impact of Acute Kidney Injury in Critically Ill Patients with Invasive Pulmonary Aspergillosis in the Intensive Care Unit: A Retrospective, Single-Center Study.,” Kidney Dis (Basel), vol. 10, no. 4, pp. 262–273, Aug. 2024. [CrossRef]
- R. Agarwal et al., “Revised ISHAM-ABPA working group clinical practice guidelines for diagnosing, classifying and treating allergic bronchopulmonary aspergillosis/mycoses.,” Eur. Respir. J., vol. 63, no. 4, Apr. 2024. [CrossRef]
- M. Aruanno, E. Glampedakis, and F. Lamoth, “Echinocandins for the Treatment of Invasive Aspergillosis: from Laboratory to Bedside.,” Antimicrob. Agents Chemother., vol. 63, no. 8, Aug. 2019. [CrossRef]
- Q. Li, D. Wen, Y. Chen, L. Yang, J. Li, and S. Luo, “Early respiratory interventional therapy combined with antifungal agent for endobronchial cryptococcosis: A case report and literature review.,” Medicine (Baltimore), vol. 103, no. 12, p. e37455, Mar. 2024. [CrossRef]
- K. Przywara, R. Adamski, M. Książczyk, J. Suchodolski, and M. Cal, “3-bromopyruvate induces morphological alteration and may initiate programmed cell death in Cryptococcus neoformans cells.,” Arch. Microbiol., vol. 206, no. 4, p. 153, Mar. 2024. [CrossRef]
- T. Kitazawa et al., “Efficacies of atovaquone, pentamidine, and trimethoprim/sulfamethoxazole for the prevention of Pneumocystis jirovecii pneumonia in patients with connective tissue diseases.,” J. Infect. Chemother., vol. 25, no. 5, pp. 351–354, May 2019. [CrossRef]
- J.-A. Tabanor and S. Lakshminarayanan, “Do patients on biologic drugs for rheumatic disease need PCP prophylaxis?,” Cleve. Clin. J. Med., vol. 86, no. 7, pp. 449–453, Jul. 2019. [CrossRef]
- G. R. Thompson et al., “Global guideline for the diagnosis and management of the endemic mycoses: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology.,” Lancet Infect. Dis., vol. 21, no. 12, pp. e364–e374, Dec. 2021. [CrossRef]
| Type of Aspergillosis | Reported State & Year | Type of Study | Study population | Number of isolates | Salient Findings | Reference |
|---|---|---|---|---|---|---|
| Chronic Pulmonary Aspergillosis | New Delhi 2024 | Prospective | 255- Recruited 158- Completed follow up | 11.1% were positive at baseline, and 27.5% were positive at the end of ATT | CPA may arise after anti-tubercular treatment or be present at the time of diagnosis in patients with newly diagnosed tuberculosis. | Jha et al. [22]. |
| Chronic Pulmonary Aspergillosis | Chandigarh 2024 | Prospective | 111- Of which 53 were control | 52.25%- Proven CPA | Compared to controls, those with CPA related to PTLA exhibit reduced Th-1 response and decreased neutrophil oxidative burst. | Chirumamilla et al [23] |
| Chronic Pulmonary Aspergillosis | Maharashtra 2023 | Cross-sectional/Observational | 42 | 9.5% | Serological diagnosis is necessary for detecting CPA in patients with or without TB due to similar clinical features. | Rajpurohit et al [24] |
| Chronic Pulmonary Aspergillosis | New Delhi 2022 | Prospective-Observational | 130 | 24.2% | While a differential diagnosis is needed for CPA and TB, the mediastinal necrotic lymph node is the proper CT finding for differentiating between recurrent TB and post-TB sequelae. | Bharath et al. [25] |
| Chronic Pulmonary Aspergillosis | India 2022 |
Estimation Analysis | - | - | Comprehensive estimation of total CPA burden in pulmonary TB patients | Denning et al. [20] |
| Chronic Pulmonary Aspergillosis | Chandigarh 2023 | Retrospective | 434 subjects and 20 disease controls - | - | The significance of Erythrocyte Sedimentation rate (ESR) and C-reactive protein (CRP) in CPA diagnosis among Post Tuberculosis Lung Disease PTLD has been established by this study. | Sehgal et al [26] |
| Aspergilloma | Uttarakhand 2023 | Case Report | - | 1 | This Case was reported after a decade of undergoing ATT where, unusually, Aspergilloma was found as a mass in the intrabronchial region instead of a lung cavity. | Lahiri et al [27] [59] |
| Invasive Pulmonary Aspergillosis | Chandigarh 2022 | Case Report | - | 1 | Sequelae of COVID-19 complicated by TB and IPA | Gandotra et al. [28] |
| Chronic Cavitary Pulmonary Aspergillosis | Karnataka 2022 | Case Report | - | 1 | About 20 years ago, a patient had tuberculosis and aspergilloma. COVID-19 had reactivated latent aspergilloma, and the condition developed into CCPA, a more severe form of aspergillosis. | Chaurasia et al [29] |
| Reported State/ Year | Type of Study | Study Population | Number of isolates | Site of infection | Salient Findings | Reference |
|---|---|---|---|---|---|---|
| New Delhi 2019 | Case Report | - | 1 | Lung | Initially treated for TB due to misdiagnosis but later diagnosed as Cryptococcosis. | Meena et al. [43] |
| New Delhi 2019 | Case Report | - | 1 | Thoracic spine | Empirically treated for TB before being diagnosed with Cryptococcus Osteomyelitis and was treated with voriconazole for 8 weeks. | Adsul et al. [44] |
| New Delhi 2018 | Case Report | - | 1 | Lung and CNS | Disseminated Cryptococcosis mimicking TB- Reported in an immunocompetent child | Ismail et al [45] |
| New Delhi 2016 | Case Report | - | 1 | Lung | The co-existence of Pulmonary Cryptococcosis and tuberculosis was reported. Treated with fluconazole and anti-tubercular therapy | Jain et al [46], [47] |
| New Delhi 2016 | Case Report | - | 1 | Lung | They had a history of TB, a right lower lobe mass similar to a lung tumor, but was eventually diagnosed as Cryptococcoma through CT and histopathological examination. | Pawar et al [47] |
| Chandigarh 2017 | Retrospective | 42 | 2 | Lung | This introspects the significance of Fine Needle Aspiration Cytology(FNAC) as a rapid method of diagnosis in immunocompromised patients. | Sharma et al. [48] |
| New Delhi 2015 | Case Report | - | 1 | Lung / Adrenal gland | A 65-year-old adult male with no history of TB was reportedly diagnosed with Cryptococcosis mimicking TB. Still, CT findings indicated that the abnormality was due to the fungal pathogen Cryptococcus spp. | Ranjan et al [49] |
| Reported State/ Year | Type of Study | Study Population | Number of isolates | Site of infection | Salient Findings | Reference |
|---|---|---|---|---|---|---|
| Uttarakhand 2024 | Case Report | - | 1 | Lung | HIV, Pneumothorax, and TB- A rare coexistence of three pathogens | Jithesh et al. [55] |
| Maharashtra 2016 | Retrospective | 111- HIV Patients | 3(5.76%) | Lung | Of the respiratory manifestations in HIV seropositive subjects, TB is the most common. Pneumocystis was also recorded in 3 patients. | Patil et al. [56] |
| Karnataka 2015 | Prospective | 74 PLHIV -People living with HIV (37 with diabetes mellitus (DM) and 37 without DM) | 5% among DM and 18% among those without DM | Lung | EP-TB was diagnosed among 22% of the study population, while the study also recognized the significance of Pneumocystis infection | Indhira et al [57] |
| Karnataka 2015 | Descriptive | 164- HIV population | 16% | Lung | Among opportunistic infections, 50% were reported as TB in this study. | Ramesh et al [58] |
| Reported Year | Type of Study | Study Population | Number of isolates | Site of infection | Salient Findings | Reference |
|---|---|---|---|---|---|---|
| Rajasthan 2021 | Case Report | - | 1 | Lung | Pulmonary histoplasmosis misdiagnosed as miliary tuberculosis | Agarwal et al [77] |
| Chandigarh 2020 | Case Report | - | 1 | Skin, Lung | Disseminated TB and histoplasmosis co-infection was reported in a 50-year-old male. | Anot et al [78] |
| New Delhi 2019 | Case Report | - | 1 | Lung | A 59-year-old female with a history of cutaneous TB was presented with manifestations such as fever and dry cough. Multi Drug Resistant-TB was suspected due to substantial evidence from CT images. Eventually a PET scan was performed which revealed soft tissue nodule, histopathological examination suggested the presence of H. capsulatum. | Dutta et al [79] |
| Telangana 2018 | Case Report | - | 1 | Adrenal gland, lung | Hepatitis C confirmed, case with fever, treated for four months with ATT for suspected TB but was finally diagnosed as Histoplasmosis which mimics TB in clinical manifestations. | Ramesh et al [80] |
| Reported State/ Year | Type of Study | Study Population | Number of isolates | Site of infection | Salient Findings | Reference |
|---|---|---|---|---|---|---|
| Uttarakhand 2016 | Case Report | - | 1 | Lung | Coexistence of drug-resistant tuberculosis with invasive candidiasis | Khanduri et al [85] |
| Rajasthan2016 | Prevalence Study | 60 confirmed Pulmonary TB patients | 33 | Lung | Prevalence of candidal presence in sputum samples among pulmonary tuberculosis patients was reported using SDA and ChromAgar cultures. | Astekar et al [81] |
| Maharashtra 2016 | Prospective observational Study | 45- Renal transplant recipients (RTR) | 7 | - | Among renal transplant recipients, TB with candidiasis and CMV with TB was found in 7 patients | Kumar et al [86] |
| Karnataka2015 | Descriptive Study | 164- HIV positive patients | 80 | Lung | This study reported that TB and candidiasis were most frequently occurring opportunistic infections among HIV patients which were concreted by several other studies from India. | Ramesh et al [58] |
| State | Year | Site of infection | Salient Findings | Reference |
|---|---|---|---|---|
| Chandigarh2015 | 2015 | Lung | Coinfection of Tuberculosis and mucormycosis in a diabetic patient was reported. | Aggarwal et al [90] |
| Puducherry 2016 | 2016 | Lung | Pulmonary TB with mucormycosis co-infection was demonstrated in a diabetic patient admitted to the intensive care Unit. | Dube et al [91] |
| New Delhi2020 | 2020 | Lung | Disseminated pulmonary mucormycosis and tuberculosis co-infection in a diabetic patient was reported. | Ramesh et al [92] |
| Uttar Pradesh2015 | 2015 | Lung | Pulmonary artery aneurysm, a rare condition, and its association with pulmonary mucormycosis was reported. | Ramachandran et al [93] |
| Pulmonary Mycosis | Antifungal Agents | Biological Agents |
|---|---|---|
| Aspergillosis | Voriconazole, Amphotericin B, Caspofungin, Posaconazole [119] | Omalizumab, Mepolizumab, Benralizumab, Dupilumab, Tezepelumab [120] , Echinocandins [121] |
| Cryptococcosis | Fluconazole, Amphotericin B, Amphotericin B with flucytosine [122] | 3-Bromopyruvate - Anticancer agent with excellent fungicidal activity [123] |
| Pneumocystis pneumonia | Trimethoprim-sulfamethoxazole, pentamidine, & Atovaquone [124] | Adalimumab, Certolizumab, Etanercept, Golimumab, Infliximab- these anti-tumor necrosis factor alpha agents used for Rheumatoid arthritis patients have been involved in Pneumocystis development [125] |
| Endemic mycoses | Itraconazole, Fluconazole, Voriconazole, Posaconazole, Isavuconazole and Corticosteroids [126]. | Promising research is currently underway to develop biological agents for the treatment of endemic mycoses. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





