1. Introduction
Rapid palatal expansion (RPE) is a treatment method employed in orthodontic care for growing children when the maxillary dental arch needs to be expanded [
1]. When forces larger than those used for ordinary tooth movement are applied to expand the maxillary arch, the midpalatal suture of the maxilla separates and stabilizes over time through localized bone growth and proliferation, resulting in the expansion of the maxillary alveolar arch width [
2].
In adults, the general consensus is that RPE alone is not suitable because of the fusion of the midpalatal suture. Instead, surgical-assisted rapid palatal expansion (SARPE), which combines orthodontic devices with surgical procedures, is performed [
3,
4]. However, in recent years, miniscrew-assisted rapid palatal expansion (MARPE) has gained popularity, allowing for maxillary arch expansion in adults in the absence of surgical assistance [
5]. This device utilizes screws implanted in the hard palate to facilitate maxillary alveolar arch expansion via midpalatal suture separation in adults.
Herein, we report a case of maxillary bone fracture caused by MARPE and discuss its implications.
2. Case Report
The patient was a 32-year-old female gym instructor who was referred to our plastic surgery department by an orthodontist for orthognathic surgery. She presented with Angle Class III malocclusion, an edge-to-edge bite with crowding, and maxillary arch constriction (
Figure 1). It was predicted that maxillary alveolar arch expansion through orthodontic treatment would be necessary to address the transverse arch discrepancy that would persist even after orthognathic surgery. A treatment plan was established to perform orthognathic surgery in our facility after leveraging presurgical orthodontic treatment to optimize the transverse dimension.
The maxillary width is smaller compared to the mandibular width.
The MARPE device was placed, and orthodontic treatment was initiated.
After orthodontic treatment was initiated, the MARPE device (M.S.E., Maxillary Skeletal Expander, Forest-One Co., Japan) was placed (
Figure 2). Comprehensive blood tests, including biochemistry, complete blood count, coagulation tests, infection screening, and imaging (electrocardiogram, chest X-ray), revealed no abnormalities. There were no findings suggestive of musculoskeletal metabolic disorders.
The MARPE device was activated as follows: 0.4 mm of expansion was performed daily, divided into two sessions until a clear separation of the midpalatal suture was observed. After achieving suture separation, the expansion rate was reduced to 0.2 mm per day in a single session, aiming for a total expansion of approximately 7 mm.
Five days after the start of expansion, the patient suddenly experienced pain, and upon looking in the mirror, she noticed the widening of the midline of her dental arch. From that day, she felt severe pain requiring analgesics. On the morning of the 12th day, the patient experienced tingling sensory disturbances on the palatal side of the upper left anterior teeth, which extended to the nose and cheek later that day. By the evening of the same day, the sensation in these areas, as well as within her oral cavity, had completely disappeared. No facial swelling was observed at this time.
The patient’s orthodontist recommended discontinuing the expansion therapy.
The patient visited our plastic surgery outpatient clinic on the 20th day after starting expansion (15 days after symptom onset). Physical examination revealed that the sensation in her left upper lip had almost completely resolved. The sensation on the left side of the nose was entirely absent, while the sensation in the left cheek had slightly recovered but remained dull. The area inside the nasolabial fold and the left lower eyelid were completely anesthetic. No facial erythema or edema was observed. Based on these findings, we strongly suspected damage to the second branch of the left trigeminal nerve.
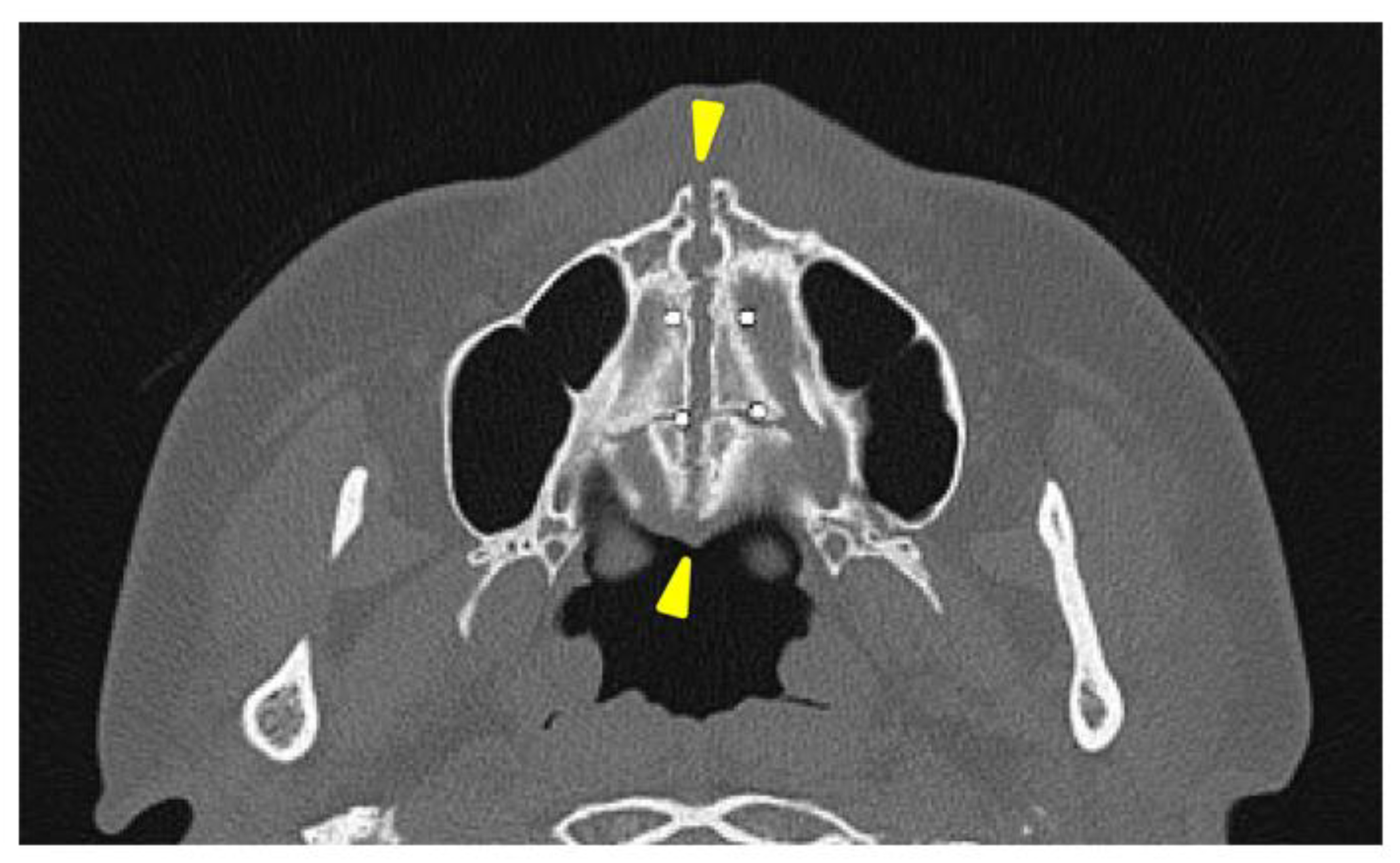
A separation of approximately 4 mm was observed in the midpalatal suture.
A head CT was performed on the same day. The axial slices revealed a 4-mm-wide separation of the midpalatal suture (
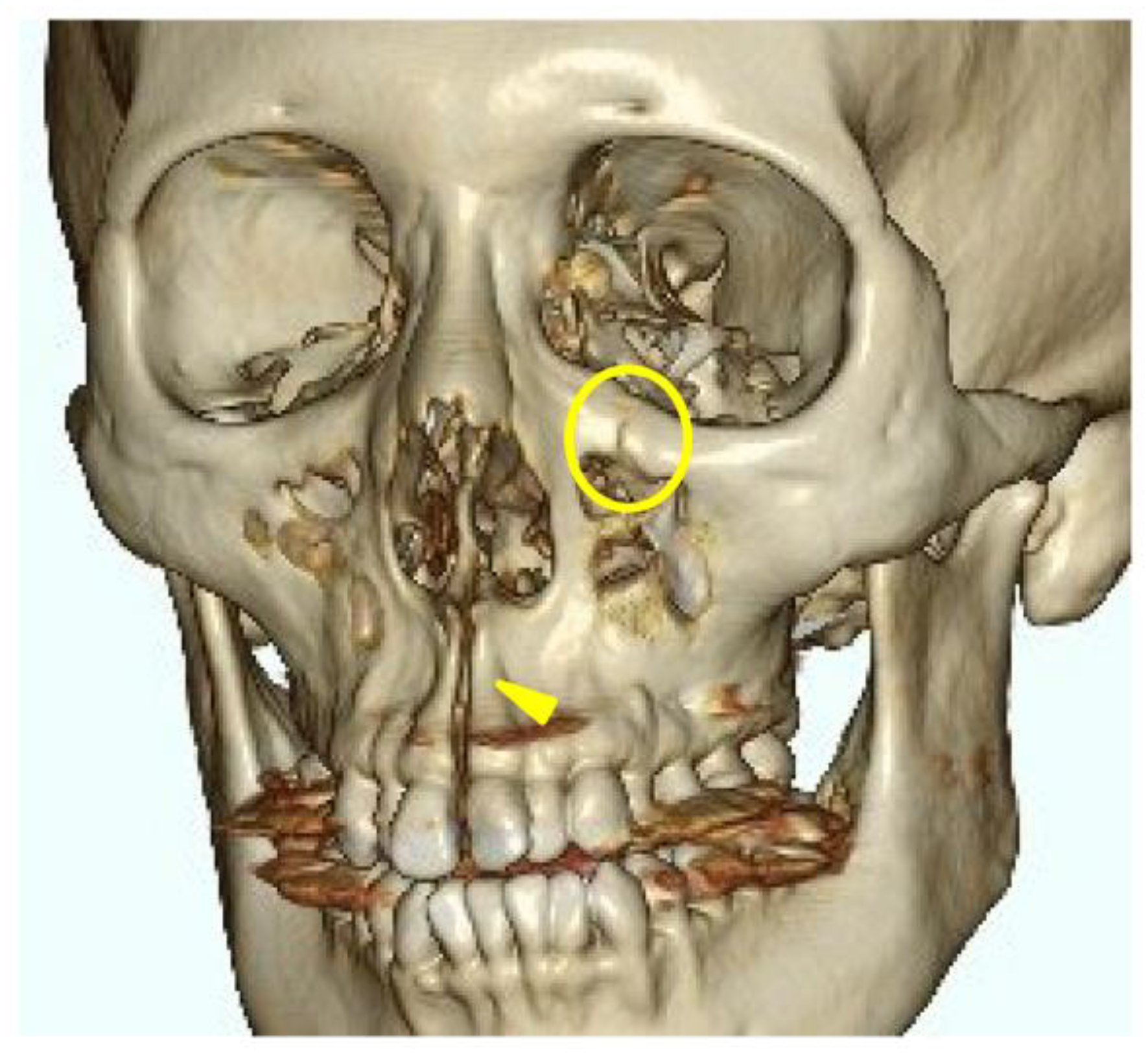
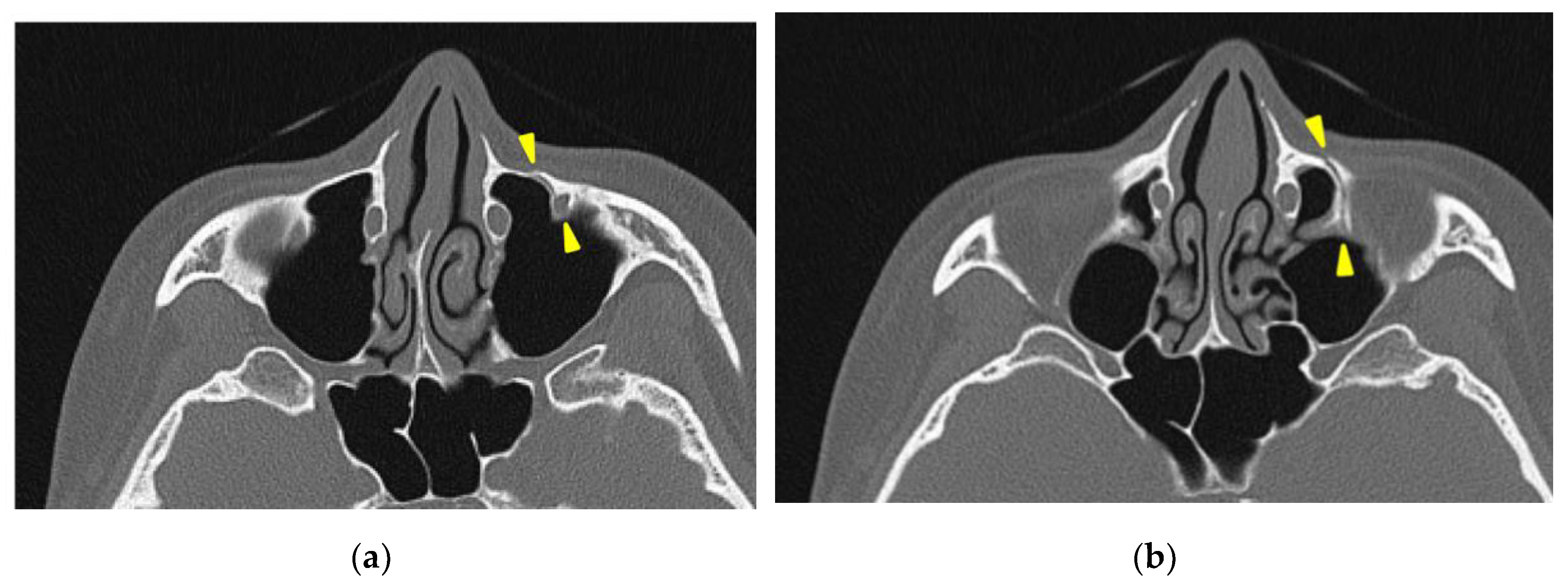
Figure 3). A fracture of the left maxilla was also observed. The line of this fracture extended from the orbital floor and the anterior surface of the maxilla (
Figure 4), starting at the medial edge of the orbital rim, passing through the entire wall of the infraorbital foramen (
Figure 5a, b), and reaching the maxilla’s alveolar process. Three-dimensional CT reconstruction revealed that the rapid expansion of the maxilla had been resisted by the surrounding bones, particularly the zygomatic bones, leading to the observed fracture.
A fracture line extending from the infraorbital rim to the infraorbital foramen (Circle mark) and a separation of the midpalatal suture (Yellow triangle marks) are observed.
The patient returned for a follow-up visit one month later, reporting improvement in symptoms despite the persistence of some sensory disturbances. At her two-month follow-up visit, there were no areas of complete anesthesia, although she continued to experience paresthesia in previously affected regions.
The sensory disturbances gradually resolved, and two years later, all symptoms had completely disappeared. However, the patient developed a phobia of the planned orthognathic surgery and ultimately canceled it, opting for orthodontic treatment alone.
3. Discussion
Reports of MARPE-induced maxillary bone fractures are unprecedented. However, fractures have been reported with SARPE. Shimming et al [
6]. described the case of an alveolar process fracture in a 38-year-old woman undergoing SARPE due to midpalatal suture ossification. Thus, factors such as age and suture ossification can increase the risk of fractures, which may be even greater in nonsurgical expansions like MARPE.
The trigeminal nerve sensory disturbances observed in this case were likely caused by a fracture within the infraorbital canal and infraorbital foramen, resulting in nerve injury. This is supported by the fact that the symptoms were limited to the region innervated by the infraorbital nerve. The preservation of maxillary molar sensation indicates that the middle superior alveolar branch, which branches off before the infraorbital canal, was not damaged.
In this case, the fracture was concentrated around the zygomatico-maxillary suture for reasons that are unclear; however, there are studies investigating the correlation between the ossification state of facial bone sutures and the effects of rapid maxillary expansion (RME) devices [
7]. Provatidis et al. [
7] analyzed the effects of RME on the craniofacial complex using finite element modeling, a computer simulation method, by applying RME to a dry human skull. Their analysis revealed that while the lacrimomaxillary, frontomaxillary, and nasomaxillary sutures had little influence on RME outcomes, the zygomatico-maxillary suture was significantly affected. These findings may have something to do with the underlying mechanisms of the fractures observed in this case. Furthermore, in trauma-induced zygomatic fractures, it is well-known that fracture lines frequently pass through the infraorbital foramen and that sensory disturbances of the second branch of the trigeminal nerve are typical symptoms of such fractures [
8,
9]. Therefore, the infraorbital foramen is inherently a site prone to fractures caused by external forces, and a MARPE-induced fracture is highly likely to involve this area.
In this case, the expansion rate did not exceed the manufacturer’s recommendations. The maxillary bone fracture is likely caused by factors predisposing patients to fractures, such as stress concentration due to bone morphology, aging-related bone elasticity reduction, and suture ossification. There is currently no established method of evaluating these risks before initiating treatment to our knowledge. However, in cases where a high-risk is suspected, even SARPE should be avoided. Instead, the expansion of the alveolar arch width through presurgical orthodontic treatment should be omitted, and a surgical approach using multiple osteotomies during Le Fort I osteotomy should be considered to achieve the desired transverse expansion.
4. Conclusions
This case report highlights a rare but clinically significant complication of MARPE, resulting in a maxillary bone fracture. The fracture, localized around the zygomatico-maxillary suture, appears to be associated with stress concentration during expansion. In adult patients undergoing rapid maxillary expansion, anatomical variations, decreased bone elasticity, and suture ossification should be recognized as potential risk factors. Careful patient selection and thorough risk assessment are essential to minimize complications. In high-risk cases, presurgical orthodontic treatment must be avoided, and a surgical approach to transverse expansion considered. Clear communication of potential risks to the patient and close observation throughout treatment are crucial for reducing complications and improving patient outcomes.
Author Contributions
Conceptualization, U.H.; investigation, U.H., H.M. and T.A.; data curation, H.M.; writing—original draft preparation, U.H.; writing—review and editing, T.A.; supervision, T.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This case report is exempt from ethical review and approval in our institute.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The deidentified patient data supporting this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank Enago (
www.enago.jp) for the English language review.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MARPE |
Miniscrew-assisted rapid palatal expansion |
| RME |
Rapid maxillary expansion |
| RPE |
Rapid palatal expansion |
| SARPE |
Surgical-assisted rapid palatal expansion |
References
- da Silva Filho, O.G.; do Prado Montes, L.A. , Torelly, L.F. Rapid maxillary expansion in the deciduous and mixed dentition evaluated through posteroanterior cephalometric analysis. Am J Orthod Dentofacial Orthop 1995, 107, 268–75. [Google Scholar] [CrossRef] [PubMed]
- Haas, A.J. Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod 1970, 57, 219–55. [Google Scholar] [CrossRef] [PubMed]
- Suri, L.; Taneja, P. Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofacial Orthop 2008, 133, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Cureton, S.L.; Cuenin, M. Surgically assisted rapid palatal expansion: orthodontic preparation for clinical success. Am J Orthod Dentofacial Orthop 1999, 116, 46–59. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, Y.C.; Park, J.Y.; Hwang, W.S. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop 2010, 137, 830–9. [Google Scholar] [CrossRef] [PubMed]
- Schimming, R.; Feller, K.U.; Herzmann, K.; Eckelt, U. Surgical and orthodontic rapid palatal expansion in adults using Glassman's technique: retrospective study. Br J Oral Maxillofac Surg 2000, 38, 66–9. [Google Scholar] [CrossRef] [PubMed]
- Provatidis, C.G.; Georgiopoulos, B.; Kotinas, A.; McDonald, J.P. Evaluation of craniofacial effects during rapid maxillary expansion through combined in vivo/in vitro and finite element studies. Eur J Orthod 2008, 30, 437–48. [Google Scholar] [CrossRef] [PubMed]
- Tajima, S. Malar bone fractures: experimental fractures on the dried skull and clinical sensory disturbances. J Maxillofac Surg 1977, 5, 150–6. [Google Scholar] [CrossRef] [PubMed]
- Jungell, P.; Lindqvist, C. Paraesthesia of the infraorbital nerve following fracture of the zygomatic complex. Int J Oral Maxillofac Surg 1987, 16, 363–7. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).