1. Introduction
The introduction of the highly transmissible Omicron COVID-19 SARS-CoV-2 variant B.1.1.529 into Australia in December 2021 brought about a hurried need for the population to receive a booster dose of the COVID-19 vaccine [
1]. Although Australia had more than 91.4 per cent of its eligible population age 16 and above double vaccinated against COVID-19 [
2], there was an impending need for COVID-19 vaccination uptake (either as a second, subsequent booster or young children’s primary dose) to increase the immunity protection potential for the Australian community. End-of-year celebrations in mid-December invited gatherings of large groups of family and friends into homes, facilitating the transmission of the SARS-CoV-2 virus within households and communities. Together with New Year celebrations, Victoria’s COVID-19 daily cases peaked at their highest at 51,144 on 7 January 2022 [
2].
Vaccination delivery models in Victoria are a mixture of state-run vaccination centres, pharmacies and general practices [
3]. In addition, temporary mini community pop-up ‘mini pops’ vaccination sites and outreach services were used to ensure COVID-19 vaccine equity for rural, remote and at-risk community members [
4]. General practices have successfully delivered critical public health care, including administering pneumococcal and influenza vaccinations to medically vulnerable populations at no cost via the National Immunisation Program [
5]. As a significant provider of essential primary medical care, general practices were invited to become COVID-19 mass vaccination providers on 22 March 2021. Since then, up to 4,000 general practices around Australia have provided COVID-19 vaccinations to Australians in every state and jurisdiction [
6]. Additionally, children aged five to 11 years could receive their first primary dose of the COVID-19 vaccination from 10 January 2022 [
7].
To reduce the impacts of rising COVID-19 infections during the festive season and school holidays, the Victorian Government have committed AU
$31.6 million to support Australia’s vaccination booster program, especially in local government areas where there is a lower density of primary care vaccination providers [
8]. In this paper, we describe how a small general practice in suburban Victoria developed and enhanced its COVID-19 vaccination service capacity via iterative workflow redesign and social innovation.
2. Methods and Results
Over a five-week period between January 4 2022 to February 7 2022, Eden Rise Family Clinic developed an innovative program that resulted in a highly effective and efficient vaccination service. This report starts by describing the overall key goals achieved while undertaking this vaccination campaign. It then goes on to further describe the individual key components and stages undertaken to improve vaccination delivery outcomes.
As of 7 February 2022, we doubled our vaccination booking availabilities, introduced unlimited walk-ins and reutilised the clinic’s indoor physical spaces to increase the accessibility of COVID-19 vaccinations to our local community and the wider public. With the support system of the Victorian Government Department of Health, our modified clinical and administrative workflow allowed us to immunise an average of 39 patients per hour. From entering to leaving the clinic, patients would stay no longer than 25 minutes, which includes a mandatory 15-minute observation period. The clinic’s success was built on a supportive on-the-ground clinical and administrative team, rapid response to workflow process improvement, local community partnerships, utilising new digital health technologies, and possessing an efficient leadership direction.
Here, we narratively describe in detail how our efforts began and the iterative updates to improving each component of the vaccination program strategy.
2.1. Assembling a Team
The task of administering large quantities of COVID-19 vaccines in addition to regular patient consults requires a reallocation of team members’ duties and changes in current workflow processes. Considering the limited indoor space and available private rooms, team members must become familiar with managing potential patient influx into the clinic yet adhere to local social distancing measures. Our team included three general practitioners, one medical registrar, one registered nurse, one enrolled nurse, three medical receptionists, one clinical pharmacist and a practice manager. We began work on onsite readiness on 1 January 2022 and executed our first day of the vaccination campaign on 4 January 2022.
2.2. Location
Situated at a major roundabout, Eden Rise Family Clinic’s elevated topographical position provided a towering presence, bringing about increased foot and car traffic. With a total land area of approximately 747 m2, 260 m2 of indoor space, 375 m2 of onsite parking and a small roadside strip parking, the clinic was large enough to accommodate roughly 10 staff and 20 patients.
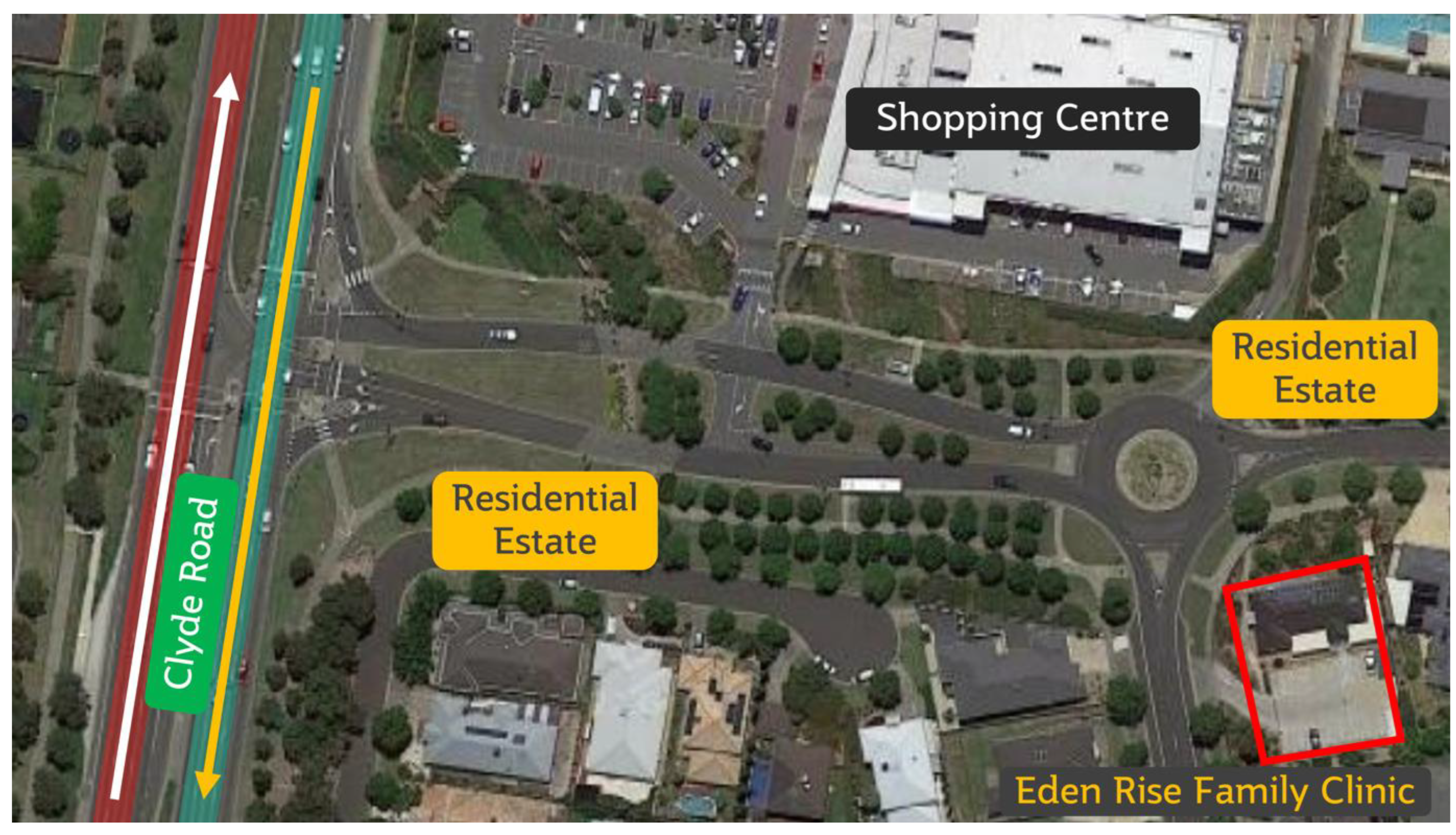
Located directly opposite a mid-sized shopping complex tenanting two major supermarket brands, Eden Rise Family Clinic was familiar to the residents within the Eden Rise residential estate (
Figure 1). With a major road (Clyde Road) in proximity, the clinic was highly accessible to new and existing community members residing in Berwick, Narre Warren South and Clyde North.
Despite these advantages, some physical constraints of the on-site parking area threatened the ability to streamline patient flow. The clinic was designed to facilitate a maximum of 20 patients, both parked drivers and those on foot. At any time, the site will have patients consulting with one of the five medical practitioners: a physiotherapist, a nurse, a pharmacist and a phlebotomist. A pilot one-day event noted that the narrow two-lane wide roadway for both ingress and egress from the two-way residential street brought difficulties in maximising the clinic’s throughput. To accommodate more patients into the clinic without causing traffic backup onto the residential street (or worse, at the roundabout), patients were encouraged to complete patient information and COVID-19 vaccination consent forms before their appointment. We subsequently reworked the parking lot traffic flow by involving administration team members to observe traffic flow. If car parking spots were fully occupied, medical receptionists would direct these patients to alternative residential parking spaces or the shopping complex. Regardless, it was essential that we provided two parking lots for the disabled, medically vulnerable, pregnant women and those with big households in the car.
2.3. Maximising Space – Maximising Workflow
Eden Rise Family Clinic has, in the past, conducted influenza vaccinations within the compound’s parking lots during the early part of the COVID-19 pandemic in 2020. However, offering such services as a standard suite of vaccination delivery options was not viable during this five-week booster dose campaign. With the new rollout of children’s COVID-19 vaccinations, young patients needed to be close to clinical team members for post-vaccination observation and care. Thus, we proposed efficiently maximising the clinic’s indoor space capacity limits to increase patient throughput and improve patient safety.
With an indoor area of approximately 260 m
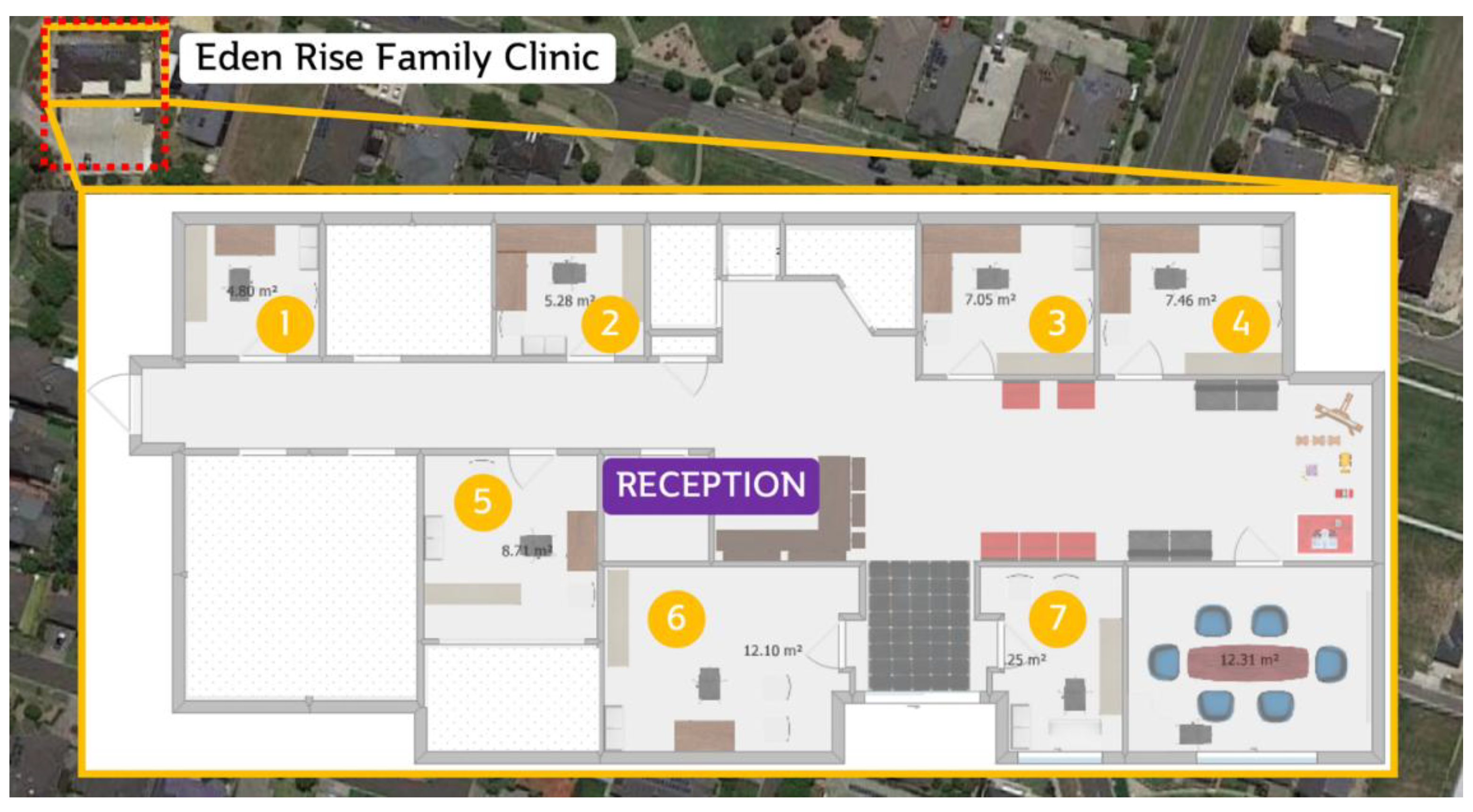
2, seven vaccinations could occur at any time within the seven consultation rooms (
Figure 2 and
Figure 3). Although this could significantly increase patient output, our pilot event noted that all general practitioners’ consultations were filled up with COVID-19 vaccinations, which led to urgent primary care and regular patients not being attended to promptly. We subsequently reshuffled the roles of each licensed vaccinator and limited COVID-19 vaccination bookings to one registered nurse, one pharmacist immuniser and two medical doctors. This freed up other general practitioners to attend to regular and urgent primary care patients, thus ensuring the continuity of primary care concurrent with this public health initiative.
We evaluated each vaccinator’s steps to complete one COVID-19 vaccination and noted the inefficiencies. To better utilise staffing resources, each vaccinator was given a specific task instead of multiple tasks during the vaccination process. For example, each vaccinator was allocated to a particular task, such as vaccine preparation, or vaccination, or patient counselling, or data collection. Repeating a singular work task reduces the lag time between moving from one task to another (i.e., walking from one room to another) and spending unnecessary time along the way. Additionally, reducing the need to perform transitional activities (i.e., getting vaccines from the fridge, inputting patient information and updating immunisation records) ensures that the speed of vaccinating one patient will be efficient and patient flow optimised. This mimics the patient journey process used in major vaccination hubs, though on a much smaller scale.
2.4. Repurposing Clinical Spaces
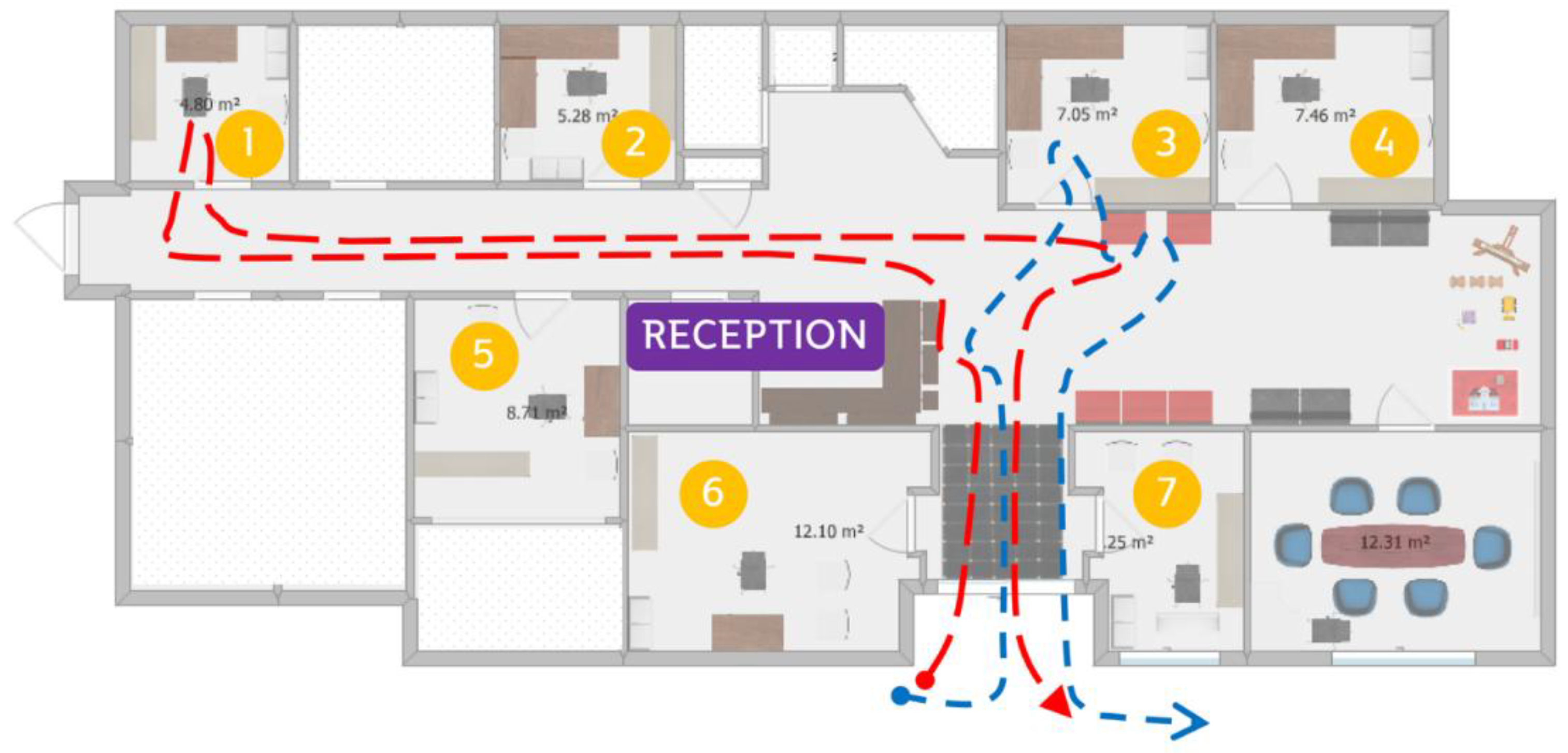
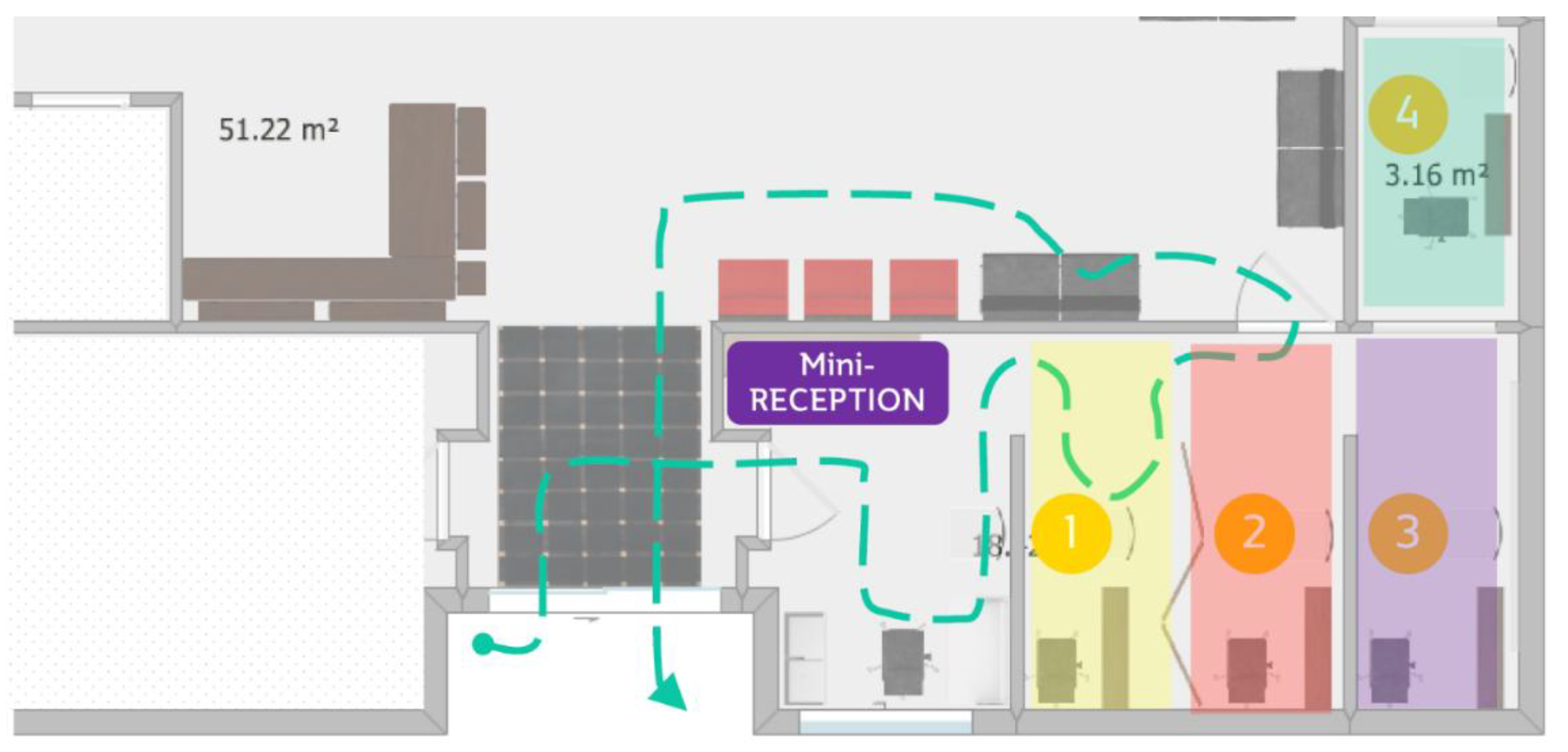
Considering the patient’s journey within the clinic, we proposed a rethink of our current workflow processes with COVID-19 vaccinations (
Figure 4). We identified a less frequently used conference room and remodelled the surrounding area to accommodate more patients and clinical activities. First, a doorway was built into the adjacent wall connecting one consultation room and a conference room, allowing for dedicated entrance and exit doors for patients post-vaccination. Second, the large conference room was subdivided into two by adding a partition wall. As one-half of the conference room was subdivided marginally bigger, we used privacy screens to create two individual work areas. The clinic also has a children’s play area that has been cordoned off and unused since COVID-19. Due to it being adjacent to the conference room, we removed the play area and built a room with a doorway connecting to it. This room also had its exit door to the main post-vaccination observation waiting area. Altogether, one mini reception and four vaccination stations were set up. Each room was provided adequate ventilation via a split system air conditioner, standing fans or open windows.
This new floorplan allows patients enter the clinic immediately through a mini reception (
Figure 5). They are greeted by a medical receptionist and asked to fill up their personal particulars and consent forms. Once completed, patients will be directed to one of four available vaccination stations. Each station is equipped with all necessary vaccination and anaphylaxis equipment. Each patient will be directed to a vaccination chair, and a vaccinator will administer the COVID-19 vaccine. The vaccinator provides important written post-vaccination information and then escorts the patient to the main waiting room for a mandatory 15-minute observation. During that time, the clinic’s main receptionist will oversee the observation of every patient in the waiting room. Once their observation time is up, the patient is allowed to leave. Each day, one medical doctor will be rostered to oversee patient care post-vaccination.
This remodelled COVID-19 vaccination area greatly enhances the patient’s experience with vaccination and reduces the many pain points observed in the original workflow. This resulted in dedicated footpaths for patients and minimised unwanted social contact with other patients inside the practice, thus reducing the spread of COVID-19. In this design, patients are not required to walk long distances between rooms, reducing the need for vaccinators to walk back and forth from their consulting rooms to call out for each patient. Instead, waiting room patients are within seeing distance of vaccinators and can be called into the vaccination stations without vaccinators leaving their stations. The change in the workflow vaccination process through remodelling and staff redistribution is reflected by vaccination acceleration by approximately two minutes per patient.
Allocating a group of vaccinators to a well-connected and dedicated vaccination area allows the clinic to maintain business-as-usual for the delivery of essential primary care and acute and chronic disease management. It was also crucial that the role of vaccinating patients was rotated between all vaccinators so that primary care patients could consult with their regular general practitioner when needed. This allowed for fairness in job task allocation and patients’ preferences for a particular doctor.
2.5. Contingency Measures
A vaccine refrigerator failure event could threaten our ability to provide COVID-19 vaccinations, and this seemed possible, given that these refrigerators are subject to sudden electricity outages and general wear and tear. Considering the highly temperature-sensitive nature of COVID-19 vaccines and strict temperature reporting requirements, additional steps were undertaken to safeguard the viability of our vaccination program. We procured an extra vaccine refrigerator and collaborated with nearby pharmacies and general practices to transfer vaccines if a refrigerator breakdown occurred. This collaborative relationship between neighbouring primary healthcare sites ensures that patients can be redirected easily to other vaccination sites if required (i.e., vaccine out of stock) to provide a continuity of vaccination service and greater efficiency in mass vaccination campaigns within the local primary healthcare network.
The 2021 year-end holiday season saw an uptick in COVID-19 infections in Victoria in January 2022. To meet the increasing demand for COVID-19 vaccinations, we increased full-time equivalent staffing hours by 20% to account for sick days, holiday leaves and staff COVID-19 infections and found it to be an ideal human resource practice.
During our mass vaccination days, we noted that patients booked between 9 am to 11 am tend to arrive 20 minutes ahead of their appointments. As the clinic doors opened for a 9 am scheduled start, we had vehicles and patients overflowing the car parks and into the clinic. As this trend continued, our team pivoted to an earlier vaccination start time while keeping first bookings at 9 am. With an additional immuniser rostered in the early mornings, we could accommodate the surge of early morning arrivals and remove the backlog of patients and vehicles by 9.30 am (i.e., 9.30 am bookings were attended to on time). At the end of each vaccination day, administration and clinical leads held debriefs to discuss lessons learned, issues of concern and ways of improving for the next vaccination event.
2.6. Community Outreach
As we settled into the new COVID-19 vaccination workflow, ensuring awareness of this service became a priority. Utilising the prominent corner block position of a roundabout, we created two large 3 m × 2 m outdoor banners and displayed them on the fences around the perimeter of the clinic (
Figure 6). We created banners emphasising the availability of children’s COVID-19 vaccination as we were in close proximity to two major primary and secondary schools. This was useful as the roundabout prompted parents to slow down and examine the banners while driving their children to school. We also adopted an online social media presence within local community groups by providing valuable public health information about children and adult COVID-19 vaccines and the availability of receiving such services at the clinic. In addition to parent outreach, we collaborated with two local school principals and parent group representatives to disseminate information about new availabilities and timings for COVID-19 vaccinations. Local schoolteachers were also given priority to receive their vaccinations during their lunch break or after work. As part of our efforts to increase COVID-19 vaccine uptake, our newly improved workflow processes allowed us to offer walk-in vaccination appointments to the larger Berwick, Clyde and Narre Warren communities. More importantly, we opened up weekend bookings, allowing day-shift working adults and parents to bring their children in on the weekends. We also prioritised vaccinations for medical and nursing colleagues and their families.
As part of medical outreach, patients’ database was used to identify at-risk populations who were not yet vaccinated against COVID-19. We noted that medically vulnerable populations, such as the elderly and those with a disability, were unintentionally displaced in receiving a COVID-19 vaccination and/or a booster dose. Using the medical recall search system within clinical software, we performed an automated patient eligibility search and identified patients who were due for a booster dose. Teamwork within the clinic ensured these patients were contacted and followed up, and vaccination bookings were made accordingly.
To assist in reaching out to at-risk populations, it was clear that an outreach service would be essential in maximising COVID-19 vaccination coverage. Our administration team partnered with DMS IT to provide additional mobile workstations through remote desktop connectivity. For every outreach vaccination, vehicles are equipped with one laptop computer with remote access capability, an iPad for electronic patient registration and consent, and a 4G pocket Wi-Fi. Collaboration between underserved populations and clinical staff was vital to the type of outreach vaccination service provided. In some instances. Some members of large households may be homebound and benefit from a family home vaccination service. Data showed that COVID-19 had a higher negative impact on communities from lower socioeconomic backgrounds and religious faith [
9], thus was a focus of outreach in the program. It was essential to understand the difficulties these close-knitted multigenerational households faced in transporting large groups of family members to the clinic and also to be able to receive culturally appropriate vaccination services. Home vaccination outreach services can take considerable time, so we conducted outreach services once a week outside working hours to ensure day-to-day operations were not negatively impacted. With each home vaccination service, one doctor and one pharmacist were allocated to each vehicle to provide adequate medical and pharmaceutical support. In times of medical emergency, a second doctor based in the clinic was within reach for additional medical support.
3. Discussion
Operating a COVID-19 booster and children’s mass vaccination clinic amid rising COVID-19 infections exposes vulnerabilities to our original operational workflow processes. While re-rostering staffing levels to meet the community’s demands, we were not immune to the labour shortage caused by staff contracting COVID-19 during their day-to-day clinical activities [
10,
11]. Additionally, booking appointments did not guarantee on-time arrivals or prevent non-attendance, which led to the need for real-time executive decision-making to maintain optimal workflow processes. Commencing vaccine preparation at least 30 minutes before the first scheduled appointment allowed morning team members to ease into their routine and reduce work stress and potential long-term burnout.
A clear communication strategy was also important for discussing the pain points experienced by each unit during the vaccination day. Despite operating with a small team, clear and concise reporting and handover are imperative to executing such mass vaccination projects and delivering our main role as a primary care general practice clinic.
As this program included the administration of first-dose children’s COVID-19 vaccinations, we noted the extended consultation time required with parents before vaccine administration. However, this consultation time was reduced significantly by the time the second dose was administered. We suspected that process familiarity played a significant role in expediting second-dose children’s COVID-19 vaccinations. However, we learned that reducing the wait times for children’s first doses was important in reducing children’s anxiety. With this observation, we substantially changed how we executed the registration and vaccination process for children receiving their COVID-19 vaccination. Upon arrival, all children’s vaccinations were attended to immediately, regardless of their appointment time, to reduce waiting-time anxiety and to improve the overall vaccination experience.
By 7 February 2022, we achieved our target of doubling our COVID-19 vaccination rates through various methods. These include redesigning the workflow process, reconfiguring unused space, using digital technologies, adopting traditional and contemporary health marketing strategies, and performing outreach services to underserved communities in the local area. The cost of running the five-week vaccination campaign was approximately A
$20,000; however, complimentary clinical supplies and equipment from local government-funded public health networks heavily reduced this amount. Evidence has shown that government incentives play a vital role in the ground-level execution of a country’s COVID-19 vaccination efforts [
12]. Additional equipment purchases and building infrastructure changes to the clinic could be repurposed to serve other healthcare needs once the demand for COVID-19 vaccination drops in the future. In the meantime, we continue to identify more efficient models for running a mass vaccination site – with the aim of high patient throughput and lower running cost. We anticipate a variable demand for COVID-19 booster doses in the future despite potentially rising infection numbers typically observed during colder seasons. However, we continue to maintain our infrastructure and staff capacities to be ready when another demand for general practices to undertake an urgent mass vaccination campaign is required.
4. Conclusions
Primary care sites such as general practice clinics and their team of allied health professionals have demonstrated to be able to adapt current workflow practices to suit the demands of a COVID-19 vaccination service in suburban Australia. Our success shows that general practice clinics should be used as vital clinical partners in the broader federal government’s vaccination strategy and a key strategic partner in future public health emergencies. This case study presented how a multidisciplinary team within one general practice fosters individual and team intrapreneurship by having its members take on active roles in public health through primary care innovation and health program execution.
Author Contributions
Conceptualization, Z.S.; methodology, Z.S..; formal analysis, Z.S.; investigation, Z.S.; writing—original draft preparation, Z.S.; writing—review and editing, Z.S.; visualisation, Z.S.; project administration, Z.S.; funding acquisition, Z.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no funding.
Acknowledgments
We thank all the team members of Eden Rise Family Clinic for their work and support during this vaccination program. We are grateful to our clinicians for their helpful discussions and advice, specifically Dr Shaheen Akhter, Dr Hossain Islam, and Dr Mahmud Ali. We want to thank Lariza Sta Ana for her dedicated administrative support. We also want to thank the Victorian Government for supporting the project and making it a worthy public health project.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Department of Health and Aged Care, ATAGI statement on Omicron variant. 2021, Department of Health and Aged Care.
- State Government of Victoria, Victorian COVID-19 data. 2021, State Government of Victoria,.
- State Government of Victoria. Where to get vaccinated. 2021 [cited 2022; Available from: https://www.coronavirus.vic.gov.au/vaccination-centres.
- State Government of Victoria. Local Vax Pop-Ups Coming To Streets And Shops Across City. 2021 13/10/2021 [cited 2022; Available from: https://www.premier.vic.gov.au/local-vax-pop-ups-coming-streets-and-shops-across-city.
- Department of Health and Aged Care. National Immunisation Program Schedule. 2021; Available from: https://www.health.gov.au/health-topics/immunisation/when-to-get-vaccinated/national-immunisation-program-schedule#national-immunisation-program-schedule-from-1-july-2020.
- Hunt, G., Phase 1B COVID-19 vaccination rollout begins. 2021, Department of Health and Aged Care.
- Department of Health and Aged Care, Australia vaccinating children against COVID-19 from early next year. 2021, Department of Health and Aged Care.
- State Government of Victoria. Boosting Victorians’ Safety Over The Festive Season. 2021 23/12/2021; Available from: https://www.premier.vic.gov.au/boosting-victorians-safety-over-festive-season.
- Pierce, M., et al., Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 2020. 7(10): p. 883-892.
- Harrington, C., et al., Nurse Staffing and Coronavirus Infections in California Nursing Homes. Policy Polit Nurs Pract, 2020. 21(3): p. 174-186.
- Xu, H., O. Intrator, and J.R. Bowblis, Shortages of Staff in Nursing Homes During the COVID-19 Pandemic: What are the Driving Factors? Journal of the American Medical Directors Association, 2020. 21(10): p. 1371-1377. [CrossRef]
- Chiyaka, E.T., et al., Prevention and Control of Infectious Diseases: Lessons from COVID-19 Pandemic Response in Zimbabwe. COVID, 2022. 2(5): p. 642-648. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).