1. Racial Discrimination as a Traumatic Bedrock of Healthcare Avoidance: A Pathway Through Healthcare Institutional Betrayal and Mistrust
Racial discrimination within the healthcare system has an ongoing influence on the quality of healthcare services for Black, Indigenous and People of Color (BIPOC) (Mohottige et al., 2023; Yearby, 2018). Prenatal care (Alhusen et al., 2016), chronic illness outcomes (Doshi et al., 2016), and emergency room outcomes (Agarwal et al., 2024) are only a few of the many places where racial disparities have been documented. Racial discrimination has also been associated with ongoing trauma symptoms, leading scholars to consider racial discrimination as a potentially traumatic event, or PTE (Hall et al., 2021). Consistent with this, experiences of racial discrimination are frequently accompanied by an increased risk of depressive (Polanco-Roman et al., 2021) and dissociative symptoms (Polanco-Roman, 2016), higher likelihood of PTSD, and overall pervasive and chronic reductions in economic, physical, and mental health (Cenat, 2022). A recent literature review of 28 studies found that racial discrimination was consistently shown to be a predictor of future traumatic symptoms for Black, Asian, and other BIPOC individuals, especially among veteran populations (Kirkinis et al., 2021). Additionally, the negative trauma-associated effects of racial discrimination have been shown to hold across age, gender, and/or education level and medical conditions (Bergeron et al., 2020; Carter et al., 2019; Cave et al., 2020; Thomas et al., 2019; Villarose, 2022). Given the above, it should come as no surprise that racial discrimination has been associated with increased healthcare avoidance behavior (Holder-Dixson et al., 2021; Zhang et al., 2022), delayed medical diagnosis (Powell et al., 2018), and increased mortality rates among BIPOC patients (Benjamins & Whitman, 2013; Pereira et al., 2022). Moreover, since avoidance behavior is described as a core feature of traumatic disorders (American Psychological Association [APA], 2022), and that racial discrimination has been shown to be a potentially traumatic experience, understanding the connection between both could lead to more comprehensive understanding of a significant issue within the healthcare system. Despite this, potential mechanisms underlying how racial discrimination from healthcare influences avoidance behavior, particularly in relation to medical mistrust and other PTE’s like healthcare institutional betrayal (HIB) have yet to be fully investigated. This is the primary purpose of the current study.
1.1. Anticipated Healthcare Avoidance as an Outcome to Prevent
Avoidance behavior is a common concern in the aftermath of a variety of traumatic or potentially traumatic events (APA, 2022). Healthcare avoidance behavior in particular, defined as delaying or outright refraining from needed medical services (Rastegar & Langhinrichsen-Rohling, 2024) can lead to a host of negative outcomes, including delayed diagnoses, higher mortality risk, and increased health disparities in populations with higher avoidance levels (Kannan et al., 2014; Smith et al., 2015). Given the logistical issues that can emerge when tracking patient behavior over time, along with the structure of most measures designed for healthcare avoidance behavior, anticipated healthcare avoidance has become the primary proxy measure for healthcare avoidance behavior. External causes of anticipated healthcare avoidance can include discomfort with screening procedures, lack of available health services, and the significant financial burden associated with available services (Kannan et al., 2014). Additionally, past negative patient-provider interactions and anticipated discrimination have also consistently been associated with healthcare avoidance across multiple demographic groups, including people classified as obese (McGuigan & Wilkinson, 2015), racial and ethnic minorities (D’Anna et al., 2018; Zhang et al., 2022), transgender and gender nonconforming individuals (Kcomt et al., 2020) and rural populations (Spleen et al., 2013). Systemic inequity plays a considerable role in how racial discrimination influences avoidance behavior, and therefore anticipated healthcare avoidance. However, understanding the specific traumatic impact and mechanisms appearing in the context of systemic inequality can provide more potential intervention targets and may aid efforts to prevent problematic avoidance behavior. The goal of this study is to investigate these connections using a trauma-informed, healthcare provider-generated framework: the BITTEN healthcare trauma impact model (Lewis et al., 2019).
1.2. The BITTEN Model
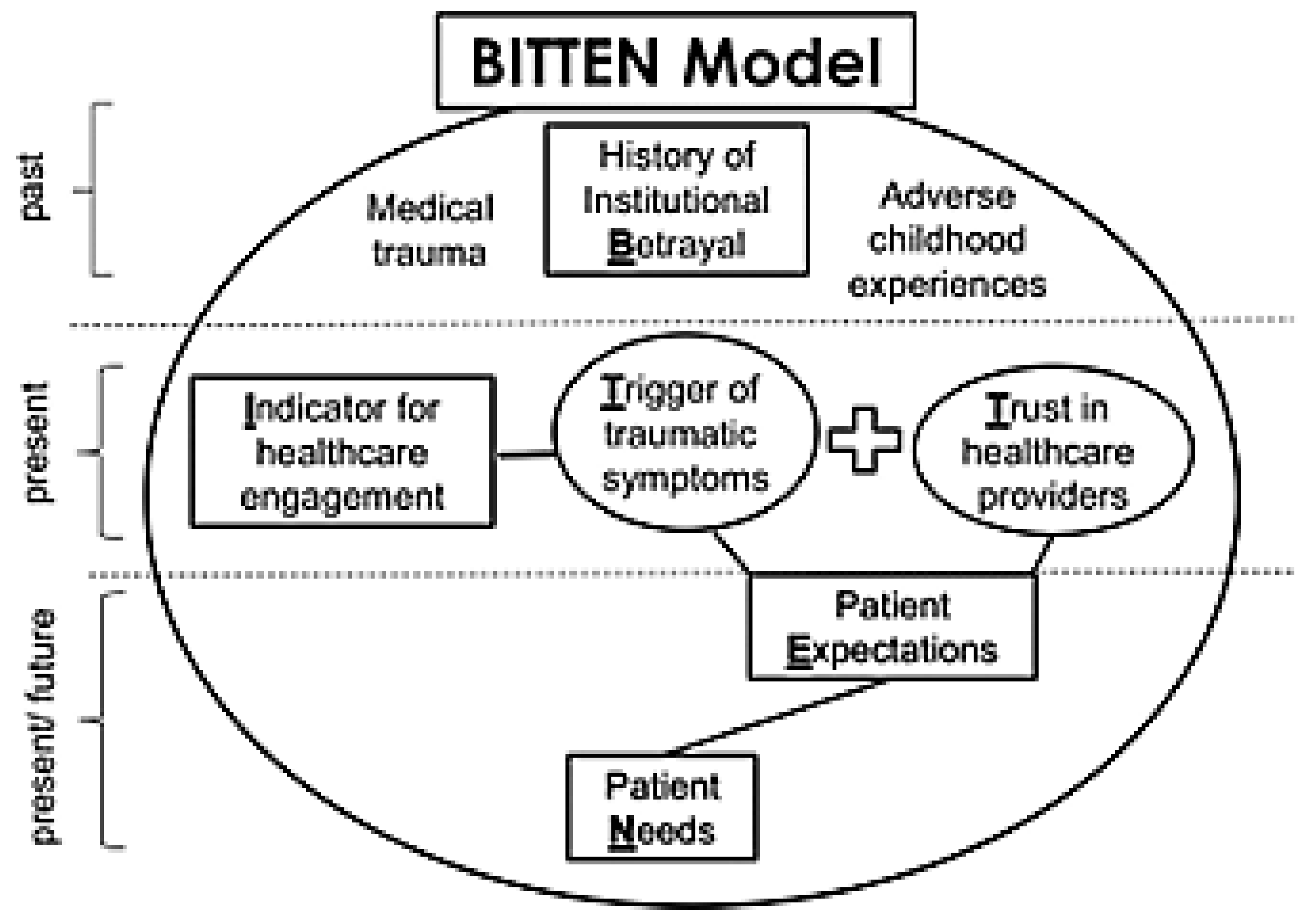
Recently advanced by Lewis and Langhinrichsen-Rohling, the BITTEN trauma impact framework (
Betrayal or trauma history,
Indicator of current problem,
Trauma symptoms and
Trust reduction activated in the current encounter, resulting in future
Expectation changes, and
Needs changes) describes the pathway by which traumatic past healthcare experiences can impact current healthcare encounters and generate future healthcare avoidance (Lewis et al., 2019). The authors posit that experiences of healthcare institutional betrayal, or HIB, can activate trauma symptoms during the current encounter, which can, in turn, negatively influence patient-provider trust, future care expectations, and needs in ways that can lead to anticipated healthcare avoidance (Lewis et al., 2019). Past traumatic experiences are brought with the patient when they seek treatment for their presenting concern (i.e., the ‘indicator’ in the framework, as seen in
Figure 1). Additionally, depending on the characteristics of the indicator, activation of trauma history also increases the risk of healthcare institutional betrayal by increasing mistrust, leading to a potential positive feedback loop of HIB sustained over time. While this model was initially generated to highlight the need for providers to assess for, prevent, and repair patients’ experiences of HIB, the framework notes that other PTE’s, such as healthcare-related racial discrimination, could also be activated, thereby increasing likelihood of medical mistrust and anticipated healthcare avoidance in a similar manner. To date, however, no published studies have considered how racial discrimination might function as an initial activating trauma or PTE in the BITTEN model. Specifically, no existing literature has considered how this pervasive and systemic type of potentially traumatic experience could be related to healthcare avoidance through the experiences of greater healthcare institutional betrayal and reduced healthcare trust in a problematic healthcare encounter. This is the purpose of the current study.
Figure 1.
The BITTEN Trauma Impact Model depicts the impact of past traumatic experiences on present healthcare behaviors and perceptions of care. Notably, racial discrimination is not listed with other PTE’s (medical trauma, HIB, ACE’s) in the original model despite being a PTE experienced by many BIPOC populations within the healthcare system.
Figure 1.
The BITTEN Trauma Impact Model depicts the impact of past traumatic experiences on present healthcare behaviors and perceptions of care. Notably, racial discrimination is not listed with other PTE’s (medical trauma, HIB, ACE’s) in the original model despite being a PTE experienced by many BIPOC populations within the healthcare system.
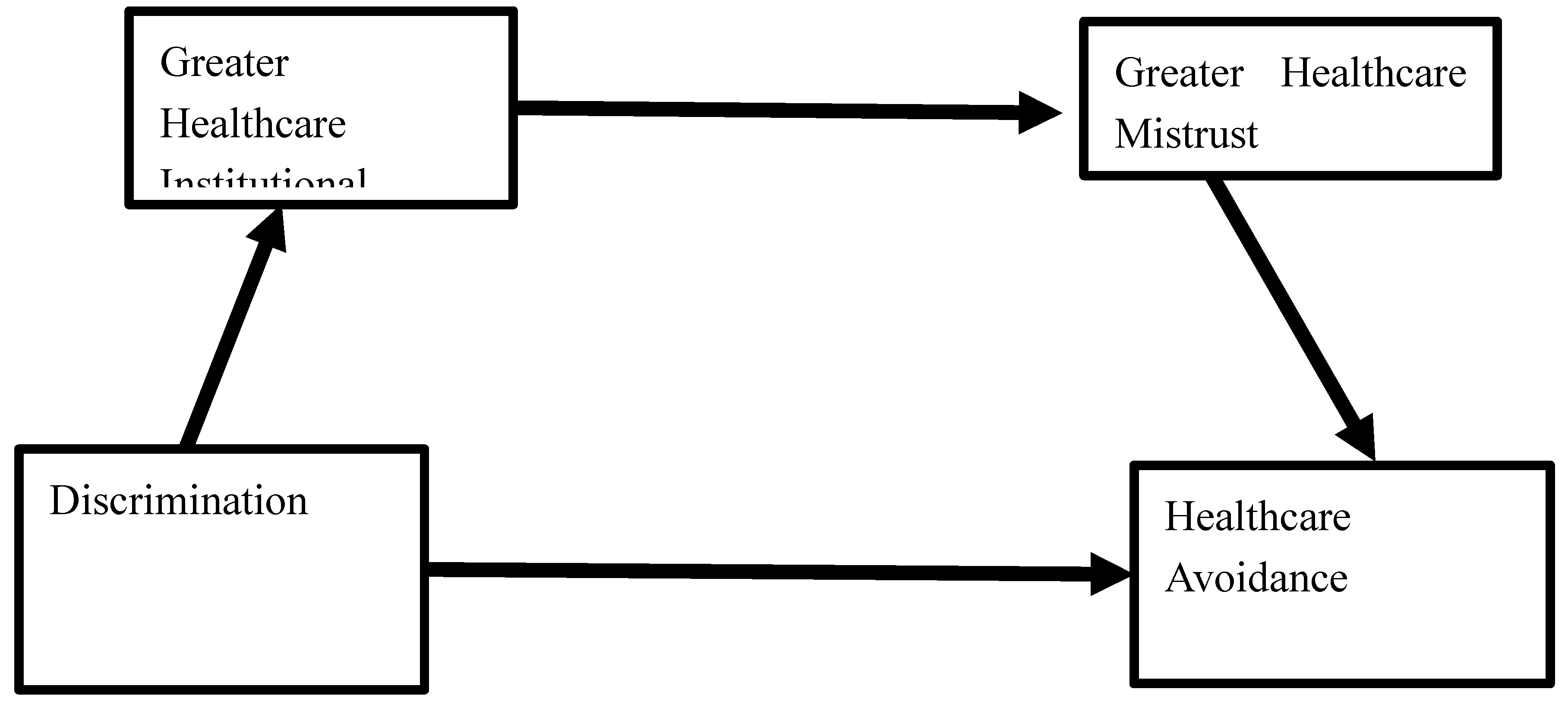
Figure 2.
Conceptual Model of Healthcare-Related Racial Discrimination, a potentially traumatic event, predicting Anticipated Healthcare Avoidance sequentially through the greater experience of Healthcare Institutional Betrayal and Mistrust in Healthcare during and after BIPOC college students’ worst or most frightening previous healthcare experience.
Figure 2.
Conceptual Model of Healthcare-Related Racial Discrimination, a potentially traumatic event, predicting Anticipated Healthcare Avoidance sequentially through the greater experience of Healthcare Institutional Betrayal and Mistrust in Healthcare during and after BIPOC college students’ worst or most frightening previous healthcare experience.
1.3. Healthcare Institutional Betrayal (HIB) as a Mediator
HIB is a type of betrayal trauma that occurs in the context of insufficiently protective or actively detrimental care provided by a healthcare system, including a hospital, health insurance company, an individual provider, or any other health-affiliated institution or service. Specifically, it is defined as an act (commission) or refusal to act (omission) perpetrated by a healthcare institution that can reasonably be expected to care for and protect the patients it serves (Smith & Freyd, 2013). HIB can include actions by the healthcare institution that run counter to best practice expectations (e.g. dismissing patient symptoms, gaslighting, careless misdiagnosis, lack of communication about cost or wait times), or negative systemic reactions to a patient reporting mistreatment or poor care (e.g., dismissing negative patient experiences or reports of injustice; poor response to whistleblowing). HIB experiences are distinct from medical trauma, in that broken trust between the institution (the healthcare system) and the patient is the primary source of distress; the act of betrayal by the system is considered damaging regardless of the severity of the event itself (Smith & Freyd, 2013). In contrast, medical trauma can include experiences of pain or poor outcomes, regardless of the healthcare system’s intention or behavior. In line with understanding HIB as a betrayal trauma, experiences of HIB have been associated with higher risk for PTSD and depressive symptoms (Tamaian & Klest., 2017) and increased healthcare avoidance, particularly if accompanied by early maladaptive schema generated from other historical traumatic experiences (Rastegar & Langhinrichsen-Rohling, 2024).
HIB may play a mediating role in the relationship between racial discrimination in the healthcare setting and healthcare avoidance, as membership of an ethnic or racial minority group increases likelihood of sustaining discrimination, which in turn increases likelihood of betrayal. For instance, a prior study found that among a group of Black and Hispanic women and non-binary people, those who endorsed higher levels of racism reported experiencing more institutional betrayal (IB) in the legal system (Porter et al., 2024), and another study found that among minoritized racial and ethnic survivors of sexual violence, 92% reported experiencing some form of institutional betrayal when reporting said violence (Gómez, 2022). Strong associations between experiences of discrimination and institutional betrayal have also been observed in general (Tamaian et al., 2024). However, since experiencing HIB requires a patient to have inherent trust in the healthcare system, it is theoretically possible that the influence of HIB on anticipated healthcare avoidance may differ for populations who have historically experienced discrimination from the healthcare system, since racial discrimination is associated with lowered perceived trust in healthcare at the outset (Hall et al., 2021). Unfortunately, little research has explored the relationship between racial discrimination and institutional betrayal within the healthcare system. As such, the role HIB plays in the healthcare avoidance behavior of BIPOC populations would benefit from further investigation.
1.4. Reduced Trust as a Mediator
In addition to HIB, medical mistrust may also play a mediating role in the relationship between discrimination and anticipated healthcare avoidance. Medical mistrust is another well-documented cause of healthcare avoidance behavior (Pellowski et al., 2017; Simon et al., 2024; Wang et al., 2023), especially for marginalized populations (e.g., BIPOC populations, LGBTQIA+, people of low SES). Multiple factors have been associated with increased mistrust levels, including previous negative healthcare experiences (Wang et al., 2023), poor insurance status (Kannan et al., 2014), and anticipated or prior experiences with racial discrimination (Slaughter-Acey et al., 2019; Zhang et al., 2022). In addition, previous negative experiences with healthcare systems and race/ethnicity can significantly influence an individual’s ‘subsequent healthcare-seeking behaviors’ (Schwei et al., 2017). As such, understanding the relationship between medical mistrust and healthcare avoidance behavior is also critical to reducing the negative public health impacts associated with avoidance of care.
It is important to note, however, that no identified research has examined the relationships among racial discrimination, HIB, and healthcare mistrust, and therefore it is unclear whether the reason mistrust is associated with avoidance behavior is due to racial discrimination itself, or an increased likelihood of sustaining HIB due to systemic racism within healthcare. Theoretically, we posit that discrimination shapes experiences of HIB and research indicates that both discrimination and HIB contribute to higher endorsement of medical mistrust (Selwyn et al., 2021, Slaughter-Acey et al., 2019; Zhang et al., 2022). Consequently, we hypothesize a sequential mediating role such that discrimination in the healthcare setting will predict higher levels of HIB which in turn will predict greater levels of healthcare mistrust and ultimately will lead to higher healthcare avoidance. Understanding the direct and indirect pathways to healthcare avoidance is a necessary next step.
Therefore, the purpose of this study is to examine the proposed relationships between racial discrimination, HIB, subsequent medical mistrust occurring in a worst or most frightening healthcare event, and overall healthcare avoidance behavior within a trauma-centered framework for healthcare experiences (i.e., BITTEN). Based on the BITTEN model and previous literature regarding the impacts of other PTE’s, we hypothesized that greater self-reported discrimination from the healthcare system would be directly associated with increased intention for healthcare avoidance among BIPOC college students. Furthermore, we expected that this relationship would be sequentially mediated by greater experiences of HIB during BIPOC participants’ self-reported worst past healthcare experience and their reports of decreased trust in healthcare in the aftermath of HIB. It is also anticipated that the addition of HIB and mistrust to the sequential model will increase the variance the model accounts for in comparison to a direct model from racial discrimination in healthcare to anticipated healthcare avoidance.
2. Methods
Participants and Procedures
Data from this study were drawn from an existing database containing responses from 956 college student participants. Participants were originally recruited to describe the impact of their previous negative healthcare experiences on their COVID-19 pandemically related healthcare behavior. For this study, we focused exclusively on participants who self-identified with at least one minoritized racial or ethnic identity. All college student participants who self-identified with a BIPOC identity were retained for analysis, including individuals who reported White and another racial identity, as well as those identifying as White and reporting Hispanic/Latino for their ethnicity.
In total, 472 total university student responses (Mage = 19.74 years, SD = 3.96) were included in this study, with ages falling between 18 to 62. Full demographic details of this sample can be found in
Table 1. The participant population was diverse with many identifying with more than one racial identity: 17.8% White, 36.7% Black/African American/Afro-Caribbean, 13.6% South Asian, 6.7% multiracial, 10.6% East Asian, 5.3% Middle Eastern/Arab, 2.5% Native American, and 1.3% Pacific Islander. In terms of ethnic identity, 14.5% of the sample identified as Hispanic/Latino. This group constitutes the BIPOC sample (i.e., Black, Indigenous, People of Color). Lastly, regarding gender identity, 32% identified as men, 63% as women; and 4% as gender minority.
All participants were undergraduate students enrolled at a large public university located in the Southeastern portion of the US. Each consented to complete a Qualtrics survey in partial fulfillment of a research requirement for an introductory psychology course; the studies were conducted as part of a SONA participant pool. IRB approval for this study was obtained and ethical procedures were followed throughout.
Participants who completed the survey in an inordinately quick fashion (less than 3 minutes), or who completed 3% of the survey or less, or who either did not answer or incorrectly answered the third attention check question which was embedded at the end of the survey were also excluded from the analysis sample. Contents of the on-line survey included demographic items, a self-report measure of their experiences with racial discrimination when receiving healthcare, written responses describing participants’ worst healthcare experience, and then the degree to which this worst experience contained acts of healthcare institutional betrayal, subsequent healthcare mistrust, and led to anticipated healthcare avoidance. Participants were compensated with course credit following completion of the on-line survey. Other options to obtain course credit were readily available and participants were able to choose not to answer any question presented to them. Thus, n’s vary slightly across analyses.
3. Measures
3.1. Demographics
Participants self-reported their race by choosing one of the following: White, Black/African American/Afro-Caribbean, American Indian/Alaskan Native/First Nations, East Asian/ East Asian American, South Asian/South Asian American, Middle Eastern/Arab/North African, Native Hawaiian or other Pacific Islander, Identity not listed (please specify). Participants were allowed to select more than one option or choose multiracial. Regarding gender identity, participants self-reported their gender from a list of seven options with the opportunity to write in an option not listed. Participants also reported on their sexual orientation by being provided a list of nine options that presented sexuality on spectrum; they were also given the opportunity to self-describe an option not listed. Lastly, participants self-reported their current age and their year in school.
3.2. Racial Discrimination in the Healthcare Setting
Racial discrimination in the healthcare setting was measured through three items that were drawn from the Everyday Discrimination Scale (Williams et al., 1997) for healthcare environments from a prior study (Hausmann et al., 2010). Participants were asked the extent to which they have: been discriminated against or made to feel inferior while receiving healthcare; were treated with less respect; or received poorer service than other people while receiving healthcare because of their race. Response options captured the frequency of occurrence on a scale from never (1) to four or more times (4). Items were summed to compute an overall racial discrimination in healthcare score, with higher values indicating more frequent experiences of healthcare discrimination. This 3-item measure had excellent internal consistency in the current study (α = 0.91).
3.3. Worst Healthcare Experience
Participants were presented with the following: “Now, think about your WORST/MOST FRIGHTENING healthcare experience when answering the following questions. Describe why you sought healthcare in the first place when you had your WORST healthcare experience.” Participants were then given a free response text box to answer why they sought healthcare during this experience. Participants were then told to continue to reflect on their worst healthcare experience as they assessed if this included acts of HIB, enhanced mistrust in their healthcare team, or led to anticipated healthcare avoidance through the use of the following measures.
3.4. Healthcare Institutional Betrayal
HIB was assessed using the Institutional Betrayal Questionnaire-Health (IBQ-H; Smith, 2017) which is a 12-item dichotomous response measure. Participants endorsed either “yes” or “no” to questions about if the healthcare system behaved in a variety of ways during their worst healthcare experience (e.g., did they mishandle your protected personal information, give you incorrect or inadequate information or advice that was not feasible for you to follow). Items were summed to compute an overall HIB score, with higher scores indicating higher endorsement of acts of HIB during one’s worst healthcare experience. The measure had good internal consistency in the current sample (α = 0.83).
3.5. Mistrust in the Healthcare System
Mistrust in the healthcare system was measured through an adaptation of the Wake Forest Physician Trust Scale (Hall et al., 2002). Questions were modified to ask about trust in the entire healthcare team, rather than the physician, after their worst healthcare experience. Item responses ranged from strongly agree (1) to strongly disagree (5) with higher scores indicating higher levels of mistrust. The measure had excellent internal consistency in this study (α = 0.91).
3.6. Anticipated Healthcare Avoidance (HAV)
Anticipated healthcare avoidance was measured via three items that were previously used to assess intention to avoid healthcare. These items had good properties in a study investigating the relationship between indicators of childhood trauma, HIB, and healthcare avoidance (Rastegar & Langhinrichsen-Rohling, 2024). The items assessed the extent to which participants avoided or delayed seeking healthcare, were fearful of seeking healthcare, or had changed their approach to seeking healthcare (e.g., now they only go to the doctor if symptoms are severe) since their worst healthcare experience. Participants rated their frequency of each type of healthcare avoidance on a scale from not at all (1) to very much (4). The items were summed to compute an overall healthcare avoidance score, with higher values indicating greater levels of anticipated avoidance. The measure had good internal consistency in this study (α = 0.81).
4. Preliminary Analyses
All data was analyzed using SPSS Version 28. Descriptive statistics were computed to ensure measures were normally distributed and had acceptable variance. Pearson’s correlations were conducted to explore relationships among variables. Gender identity and sexual orientation were used as covariates in the analysis models to control for important identities that may also be associated with focal variables. Gender identity was categorized into three groups: woman, man, and gender minority due to low response rates on various gender minority categories. Sexual orientation was also dichotomized (0 = straight/heterosexual, 1= sexual minority). Demographics for these variables are also depicted in
Table 1.
5. Primary Analyses
To test our hypotheses, we utilized Process Macro Model 6 in SPSS Version 28. Bootstrapping was used to compute confidence intervals. Gender and sexual minority were used as covariates with women and straight/heterosexual as the reference groups. To detect mediation, we first explored a direct relationship between racial discrimination in healthcare, our covariates, and healthcare institutional betrayal (HIB). Next, we determined if racial discrimination in healthcare and HIB predicted healthcare mistrust. Finally, we tested if racial discrimination within the healthcare system, HIB, and healthcare mistrust all predicted anticipated healthcare avoidance. We specifically considered if there was an indirect relationship through both of our two proposed mediators. Serial mediation was detected if the confidence interval of the indirect effect of racial discrimination in healthcare, through both HIB and healthcare mistrust, did not include zero (Hays, 2018). Descriptives for our primary measures are depicted in
Table 2.
6. Results
6.1. Associations Among the Racial Discrimination, HIB, Healthcare Mistrust, and Anticipated Healthcare Avoidance
As expected and shown in
Table 3, anticipated healthcare avoidance was significantly correlated with all focal variables including higher levels of experienced racial discrimination in healthcare (
r = 0.32,
p < .001), greater HIB (
r = 0.48,
p < .001), and healthcare mistrust (
r = 0.45,
p < .001) with small to moderate effects. Furthermore, racial discrimination in healthcare was positively associated with greater reports of HIB during one’s worst and most traumatic healthcare experience (
r = 0.40,
p < .001) and healthcare mistrust (
r = 0.33,
p < .001). HIB was moderately correlated with higher levels of healthcare mistrust (
r = 0.58,
p < .001). Lastly, sexual minority status was associated with higher reported levels of HIB, healthcare mistrust, and anticipated healthcare avoidance (
r’s = 0.13 to 0.21,
p’s < .01). The strength of these relationships was small.
6.2. Testing the BITTEN Model to Predicting Anticipated Healthcare Avoidance
Full details of the results are reported in
Table 4. First, our model predicting HIB was significant (
R2 = 0.18,
p = .000) and explained 18% of the variance. Greater healthcare-related racial discrimination predicted higher levels of HIB (β =0.38,
p = .000). Participants who identified as a sexual minority also reported higher levels of HIB (β =0.17,
p = .000). Gender identity was not associated with HIB.
Next, our model predicting healthcare mistrust was significant (R2 = 0.37, p = .000), explaining 37% of the healthcare mistrust variance. Experiences of racial discrimination in healthcare (β =0.13, p = .002) and HIB during one’s worst or most frightening healthcare experience (β =0.51, p = .000) both significantly predicted higher levels of healthcare mistrust. Participants who identified as a sexual minority also reported higher levels of healthcare mistrust (β =0.08, p = .048). Again, gender identity was not associated with healthcare mistrust.
Finally, our full model predicting anticipated healthcare avoidance was significant (R2 = 0.31, p = .000) and explained 31% of the variance. Racial discrimination within healthcare (β =0.11, p = .010), HIB (β =0.30, p = .000), and healthcare mistrust (β =0.24, p = .000) all predicted higher levels of anticipated healthcare avoidance. While men’s reports of healthcare avoidance did not significantly differ from women’s, participants who identified as a gender minority reported significantly higher levels of healthcare avoidance (β =0.11 p = .008). Sexual identity did not predict healthcare avoidance.
Lastly, as predicted via the BITTEN model, there was a significant indirect effect of racial discrimination in healthcare (β =0.05) on anticipated healthcare avoidance through HIB and healthcare mistrust based on the obtained nonzero confidence intervals. These results indicate partial mediation as the effects of racial discrimination contributed to anticipated healthcare avoidance both directly and indirectly through HIB and healthcare mistrust.
7. Discussion
Experiences of racial discrimination constitute potentially traumatic events (PTEs) that have been associated with known trauma symptoms and deleterious health-related outcomes including avoidance (Hall et al., 2021). Relatedly, experiencing racism has also been related to greater experiences of institutional betrayal in the criminal justice system (Porter et al., 2024). Understanding health-related outcomes associated with this kind of PTE is an important health directive. The current study extends the health-trauma literature by focusing on racial discrimination that has occurred within the healthcare system, with the hypothesis that these experiences will leave BIPOC college students at risk for anticipated healthcare avoidance. This study also advances the field through the use of the BITTEN trauma-impact framework, which describes how historical experiences of trauma, both from within and outside of the healthcare system, can affect both the current patient-provider encounter as well as patients’ future needs and expectations for care within the healthcare system.
One outcome that is important to predict is healthcare avoidance, as it has been associated with multiple deleterious effects including delayed diagnosis and increased mortality (Kannan et al., 2014; Smith et al., 2015). Health-related prevention efforts generally require engagement (i.e., annual physicals, routine dental care); these efforts are likely to be weakened in the face of anticipated healthcare avoidance. In the current study, racial discrimination experiences that occurred while seeking past healthcare functioned as the bedrock for anticipated healthcare avoidance among BIPOC college students, maintaining a direct effect even in analyses that contained significant mediating variables. These findings suggest that continued health disparities can be expected if we cannot eradicate BIPOC individuals’ experiences of racial discrimination from the healthcare system. The need for anti-racist healthcare is supported. These findings also support the growing literature that recognizes racial discrimination as a potentially traumatic event.
This study was theoretically grounded in the BITTEN trauma-informed model of healthcare delivery. According to BITTEN, past experiences of trauma, such as those potentially associated with experiences of healthcare racial discrimination, function as a risk factor for healthcare institutional betrayal and healthcare mistrust in current patient-provider interactions (Lewis et al., 2019). Once activated in a problematic patient encounter, these three variables can then be expected to predict anticipated healthcare avoidance in BIPOC college students. Importantly, this model was supported in the current study, accounting for 31% of the variance in anticipated healthcare avoidance. Furthermore, both proposed mediators were retained as significant predictors in the final model.
There are multiple implications to these findings. First, there is a continued need to conceptualize patient interactions with systems of care through the lens of institutional betrayal, which in turn is rooted in Betrayal Trauma Theory (Birwell & Freyd, 2008). Betrayal Trauma Theory, drawn from sexual assault survivors’ experiences of secondary trauma at the hands of the criminal justice system, postulates that there is inherent betrayal when a patient relies on an healthcare institution to provide care and that implicit trust bond is broken, either through direct action (commission of harm) or through unexpected inaction (omission of care) (Birwell & Freyd, 2008). Theoretically, however, Betrayal Trauma Theory has been silent about how systemic harm or betrayal might occur in those less likely to imbue the healthcare system with implicit trust, particularly patients with a minoritized identity and those with a greater likelihood of experiencing past discrimination within the healthcare system. Thus, further elucidation on the nuances of institutional betrayal compared to other forms of betrayal trauma is needed.
Nonetheless, findings from this study fill a gap in the literature by utilizing the BITTEN trauma-impact framework to conceptualize how discrimination experienced within healthcare can function as the bedrock of anticipated healthcare avoidance, both directly, and through increasing the likelihood of experiencing healthcare institutional betrayal and resultant medical mistrust during one’s worst/most frightening previous healthcare experience. This study adds to the growing body of literature highlighting the health toll enacted by systemic racism within the healthcare system (Bergeron et al., 2020; Carter et al., 2019; Cave et al., 2020; Thomas et al., 2019; Villarose, 2022).
Limitations to this study should be noted. First, all data were collected via self-report which is subject to memory errors and shared method variance. Second, the design was cross-sectional, precluding a true understanding of the causal relationships among these variables as well as a clear picture of how these experiences unfold across time. Other unmeasured variables, such as the level of actual avoidance compared to anticipated avoidance and primary presenting concerns of persons seeking healthcare during their worst experience, may also have important impacts on these relationships. Fortunately, the included variables in this study were grounded in theory and were designed to form a timeline from historical experiences of racial discrimination in healthcare, to a potential traumatic/worst healthcare experience that might include acts of healthcare institutional betrayal and resultant medical mistrust, to anticipated or future healthcare avoidance. Nonetheless, longitudinal work in this area will be critical.
Additionally, ‘race’ and ‘ethnicity’ are sometimes used interchangeably in the literature (Benner et al., 2018; Hackett et al 2020). However, recent scientific standards have called for treating race and ethnicity as separate constructs (Flanagin et al., 2021). In keeping with these recommendations, our study participants separately reported their race and ethnicity; however, both constructs were utilized when selecting individuals into the analysis sample of BIPOC participants. Furthermore, the discrimination measure used in the current study asked for experiences based on either race or ethnicity; future studies will need to disentangle effects based on race versus those based on ethnicity. Similarly, while a strength of this study was the inclusion of gender identity and sexual orientation status as covariates in our model, a direct focus on the potentially traumatic healthcare experiences of these individuals, using the BITTEN model, is warranted. Finally, this work was done utilizing college students as participants. While the strength of the predictive model was robust, and identifying early risk for a lifetime of healthcare avoidance is important, care should be taken if generalizing these findings to other populations or individuals located in other geographical areas.
There are many directions for advancement from this work. First, the literature focused on understanding healthcare-related trauma is nascent, even though theory in this area has advanced. Second, there is an ongoing need to consider the effects of intersectionality (e.g., veteran status, gender, age, disability, sexual orientation) on the association between racial discrimination and trauma symptoms and outcomes. Third, prevention and intervention efforts will need to explicate various ongoing forms of healthcare-related racial discrimination. For example, provider bias is a form of social discrimination in which providers withhold certain treatment options from certain populations based on the belief that these populations will not adhere to treatment (Cipollina & Sanchez, 2023). Different types of traumatic lived experiences are likely to have different impacts. Further investigation into other types of discrimination may also be warranted to determine whether this mediation relationship is unique to racial discrimination, or potentially due to the wider PTE of long-term discrimination with similar impacts. For example, recent IB research on the impact of moral injury after institutional betrayal following experiences of sexual & gender related violence has found similar traumatic symptom outcomes (anxiety, depression) along with increased chronic pain, disconnection from others, and mistrust (Kondrath et al., 2024) for cisgender women and SGM populations - a population that has historically had a higher risk of experiencing discrimination and sexual harassment.
In conclusion, racial discrimination within healthcare has already taken place for some BIPOC college students. Our findings suggest that this discrimination may be associated with healthcare avoidance both directly, and through increased institutional betrayal during a problematic healthcare experience and resultant mistrust in healthcare. Due to the crucial role HIB may play in discrimination outcomes, there is a need to reduce experiences of HIB and repair breaches of trust that have occurred during the frightening or problematic healthcare encounters of at-risk populations. A pathway forward may be to promote trauma-informed and patient-centered care rather than systems-centered care or treatment as usual (Campbell, 2024). Further investigation into the role of institutional repair strategies (Richie, 2023) along with institutional willingness to seek truth and acknowledge wrongdoing, otherwise known as institutional courage (Freyd & Smidt, 2019) could provide more information on the long-term benefits of trauma-informed care and awareness within the healthcare system; similar mitigation of institutional betrayal’s effect on trauma symptom levels in sexual assault survivors has emerged, with institutional courage lowering risk of trauma symptoms at high levels (Adams-Clark et al., 2024). Finally, investigation into the role of institutional courage in the context of healthcare with other types of traumatic experiences would provide more information on the potential cross-cutting nature of HIB and institutional betrayal at large as an intervention target for anticipated healthcare avoidance across populations.
References
- Adams-Clark, A. A., Barnes, M. L., Lind, M. N., Smidt, A., & Freyd, J. J. (2024). Institutional courage attenuates the association between institutional betrayal and trauma symptoms among campus sexual assault survivors. Psychological Trauma: Theory, Research, Practice and Policy. [CrossRef]
- American Psychiatric Association. (2022). Trauma-and Stressor-Related Disorders. In Diagnostic and statistical manual of mental disorders (5th ed., text rev.) . [CrossRef]
- Agarwal, A. K., Gonzales, R. E., Sagan, C., Nijim, S., Asch, D. A., Merchant, R. M., & South, E. C. (2024). Perspectives of Black patients on racism within emergency care. JAMA Health Forum, 5(3), e240046. [CrossRef]
- Alhusen, J. L., Bower, K. M., Epstein, E., & Sharps, P. (2016). Racial discrimination and adverse birth outcomes: An integrative review. Journal of Midwifery & Women’s Health, 61(6), 707–720. [CrossRef]
- Benner, A. D., Wang, Y., Shen, Y., Boyle, A. E., Polk, R., & Cheng, Y.-P. (2018). Racial/ethnic discrimination and well-being during adolescence: A meta-analytic review. The American Psychologist, 73(7), 855–883. [CrossRef]
- Bergeron, G., Lundy De La Cruz, N., Gould, L. H., Liu, S. Y., & Levanon Seligson, A. (2020). Association between racial discrimination and health-related quality of life and the impact of social relationships. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 29(10), 2793–2805. [CrossRef]
- Birrell, P. J., & Freyd, J. J. (2008). Betrayal trauma: Relational models of harm and healing. Journal of Trauma Practice, 5(1), 49–63. [CrossRef]
- Campbell, R. (2024). Systems-centered care versus survivor-centered care: Reimagining help and healing for sexual assault survivors. Psychology of Violence, 14(6), 379-385. [CrossRef]
- Carter, S. E., Ong, M. L., Simons, R. L., Gibbons, F. X., Lei, M. K., & Beach, S. R. H. (2019). The effect of early discrimination on accelerated aging among African Americans. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 38(11), 1010–1013. [CrossRef]
- Cave, L., Cooper, M. N., Zubrick, S. R., & Shepherd, C. C. J. (2020). Racial discrimination and child and adolescent health in longitudinal studies: A systematic review. Social Science & Medicine (1982), 250, 112864. [CrossRef]
- Cénat, J. M. (2023). Complex racial trauma: Evidence, theory, assessment, and treatment. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 18(3), 675–687. [CrossRef]
- Cipollina, R., & Sanchez, D. T. (2023). Racial identity safety cues and healthcare provider expectations. Stigma and Health, 8(2), 159–169. [CrossRef]
- D’Anna, L. H., Hansen, M., Mull, B., Canjura, C., Lee, E., & Sumstine, S. (2018). Social discrimination and health care: A multidimensional framework of experiences among a low-income multiethnic sample. Social Work in Public Health, 33(3), 187–201. [CrossRef]
- Doshi, R. P., Aseltine, R. H., Sabina, A. B., & Graham, G. N. (2017). Racial and ethnic disparities in preventable hospitalizations for chronic disease: Prevalence and risk factors. Journal of Racial and Ethnic Health Disparities, 4(6), 1100–1106. [CrossRef]
- Flanagin, A., Frey, T., Christiansen, S. L., & AMA Manual of Style Committee. (2021). Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA, 326(7), 621–627. [CrossRef]
- Freyd, J. J., & Smidt, A. M. (2019). So you want to address sexual harassment and assault in your organization? Training is not enough; Education is necessary. Journal of Trauma & Dissociation, 20(5), 489–494. [CrossRef]
- Gómez, J. M. (2022). Gender, campus sexual violence, cultural betrayal, institutional betrayal, and institutional support in US ethnic minority college students: A descriptive study. Violence Against Women, 28(1), 93-106. [CrossRef]
- Hackett, R. A., Ronaldson, A., Bhui, K., Steptoe, A., & Jackson, S. E. (2020). Racial discrimination and health: A prospective study of ethnic minorities in the United Kingdom. BMC Public Health, 20(1), 1652. [CrossRef]
- Hall, O. T., Jordan, A., Teater, J., Dixon-Shambley, K., McKiever, M. E., Baek, M., Garcia, S., Rood, K. M., & Fielin, D. A. (2022). Experiences of racial discrimination in the medical setting and associations with medical mistrust and expectations of care among Black patients seeking addiction treatment. Journal of Substance Abuse Treatment, 133, 108551. [CrossRef]
- Hausmann, L. R., Kressin, N. R., Hanusa, B. H., & Ibrahim, S. A. (2010). Perceived racial discrimination in health care and its association with patients’ healthcare experiences. Ethnicity & disease, 20(1), 40-47. https://www.jstor.org/stable/48668251.
- Holder-Dixon, A. R., Adams, O. R., Cobb, T. L., Goldberg, A. J., Fikslin, R. A., Reinka, M. A., Gesselman, A. N., & Price, D. M. (2022). Medical avoidance among marginalized groups: The impact of the COVID-19 pandemic. Journal of Behavioral Medicine, 45(5), 760–770. [CrossRef]
- Kannan, V. D., & Veazie, P. J. (2014). Predictors of avoiding medical care and reasons for avoidance behavior. Medical Care, 52(4), 336–345. [CrossRef]
- Kcomt, L., Gorey, K. M., Barrett, B. J., & McCabe, S. E. (2020). Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM - Population Health, 11, 100608. [CrossRef]
- Kirkinis, K., Pieterse, A. L., Martin, C., Agiliga, A., & Brownell, A. (2021). Racism, racial discrimination, and trauma: A systematic review of the social science literature. Ethnicity & Health, 26(3), 392–412. [CrossRef]
- Kondrath, S. R., Brandt, E. A. B., Campbell, K., Chamberlin, E. S., Dordal, P., East, R., Fantus, S., Frankfurt, S. B., Golden, K. B., Griffin, B. J., Harris, J. I., Hiltner, R. K., Holman, C. S., McGuire, A., & Usset, T. J. (2024). Moral injury and institutional betrayal among cis women and sexual and gender minorities. Current Treatment Options in Psychiatry, 11(4), 265–278. [CrossRef]
- McGuigan, R. D., & Wilkinson, J. M. (2015). Obesity and healthcare avoidance: A systematic review. AIMS Public Health, 2(1), 56. [CrossRef]
- Mohottige, D., Davenport, C. A., Bhavsar, N., Schappe, T., Lyn, M. J., Maxson, P., Johnson, F., Planey, A. M., McElroy, L. M., Wang, V., Cabacungan, A. N., Ephraim, P., Lantos, P., Peskoe, S., Lunyera, J., Bentley-Edwards, K., Diamantidis, C. J., Reich, B., & Boulware, L. E. (2023). Residential structural racism and prevalence of chronic health conditions. JAMA Network Open, 6(12), e2348914. [CrossRef]
- Pellowski, J. A., Price, D. M., Allen, A. M., Eaton, L. A., & Kalichman, S. C. (2017). The differences between medical trust and mistrust and their respective influences on medication beliefs and ART adherence among African Americans living with HIV. Psychology & Health, 32(9), 1127–1139. [CrossRef]
- Porter, E. F., Mendoza, M. P., Deng, M., Horwitz, S. D., Soltys, M. A., & Hattery, A. J. (2024). Institutional betrayal and race in the civil legal system: A latent class analysis with survivors of intimate partner violence. Race and Justice, 1-24. [CrossRef]
- Rastegar, P. J., & Langhinrichsen-Rohling, J. (2024). Understanding college students’ healthcare avoidance: From early maladaptive schemas, through healthcare institutional betrayal and betrayal trauma appraisal of worst healthcare experiences. Healthcare, 12(11), 1126. [CrossRef]
- Richie, F. J. (2023). Repair Following Healthcare Institutional Betrayal (Doctoral dissertation, The University of North Carolina at Charlotte).
- Schwei, R. J., Johnson, T., Matthews, A. K., & Jacobs, E. A. (2017). Perceptions of negative health care experiences and self-reported health behavior change in three racial and ethnic groups. Ethnicity & Health, 22(2), 156–168. [CrossRef]
- Selwyn, C. N., Lathan, E. C., Richie, F., Gigler, M. E., & Langhinrichsen-Rohling, J. (2021). Bitten by the system that cared for them: Towards a trauma-informed understanding of patients’ healthcare engagement. Journal of Trauma & Dissociation, 22(5), 636-652. [CrossRef]
- Simon, K. A., Driver, R., Rathus, T., Cole, A., Kalinowski, J., Watson, R. J., & Eaton, L. A. (2024). HIV information avoidance, HIV stigma, and medical mistrust among Black sexual minority men in the Southern United States: Associations with HIV testing. AIDS and Behavior, 28(1), 12–18. [CrossRef]
- Slaughter-Acey, J. C., Sneed, D., Parker, L., Keith, V. M., Lee, N. L., & Misra, D. P. (2019). Skin tone matters: Racial microaggressions and delayed prenatal care. American Journal of Preventive Medicine, 57(3), 321–329. [CrossRef]
- Smith, C. P., & Freyd, J. J. (2013). Dangerous safe havens: Institutional betrayal exacerbates sexual trauma. Journal of Traumatic Stress, 26(1), 119–124. [CrossRef]
- Smith, K. T., Monti, D., Mir, N., Peters, E., Tipirneni, R., & Politi, M. C. (2018). Access is necessary but not sufficient: Factors influencing delay and avoidance of health care services. MDM Policy & Practice, 3(1), 2381468318760298. [CrossRef]
- Spleen, A. M., Lengerich, E. J., Camacho, F. T., & Vanderpool, R. C. (2014). Health care avoidance among rural populations: Results from a nationally representative survey. The Journal of Rural Health, 30(1), 79–88. [CrossRef]
- Tamaian, A., Anstey, H., Kokokyi, S., & Klest, B. (2024). The impact of discrimination and institutional Betrayal on Canadian University Students’ Mental Health. Journal of Trauma & Dissociation, 25(2), 185-201. [CrossRef]
- Tamaian, A., & Klest, B. (2017). Institutional betrayal in the Canadian medical system: Reliability and validity of a self-report questionnaire. Journal of Aggression, Maltreatment & Trauma, 27(7), 703–719. [CrossRef]
- Thomas, M. D., Michaels, E. K., Reeves, A. N., Okoye, U., Price, M. M., Hasson, R. E., Chae, D. H., & Allen, A. M. (2019). Differential associations between everyday versus institution-specific racial discrimination, self-reported health, and allostatic load among Black women: Implications for clinical assessment and epidemiologic studies. Annals of Epidemiology, 35, 20-28.e3. [CrossRef]
- Villarose, L. (2022). Under the skin: The hidden toll of racism on American lives and on the health of our nation. New York: Doubleday. ISBN: 9780385544887.
- Wang, J. C., Dalke, K. B., Nachnani, R., Baratz, A. B., & Flatt, J. D. (2023). Medical mistrust mediates the relationship between nonconsensual intersex surgery and healthcare avoidance among intersex adults. Annals of Behavioral Medicine, 57(12), 1024–1031. [CrossRef]
- Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress, and discrimination. Journal of health psychology, 2(3), 335-351. [CrossRef]
- Yearby, R. (2018). Racial disparities in health status and access to healthcare: The continuation of inequality in the United States due to structural racism. The American Journal of Economics and Sociology, 77(3–4), 1113–1152. [CrossRef]
- Zhang, D., Li, G., Shi, L., Martin, E., Chen, Z., Li, J., Chen, L., Li, Y., Wen, M., Chen, B., Li, H., Su, D., & Han, X. (2022). Association between racial discrimination and delayed or forgone care amid the COVID-19 pandemic. Preventive Medicine, 162, 107153. [CrossRef]
Table 1.
Demographic Characteristics of the Analysis Sample.
Table 1.
Demographic Characteristics of the Analysis Sample.
| |
N |
% |
| |
472 |
|
| Race* |
|
|
| White |
84 |
17.8 |
| Black/AA/Afro-Caribbean |
173 |
36.7 |
| East Asian |
50 |
10.6 |
| South Asian |
64 |
13.6 |
| American Indian/Alaskan Native |
12 |
2.5 |
| Native Hawaiian/Pacific Islander |
6 |
1.3 |
| Middle Eastern/Arab/N. African |
25 |
5.3 |
| Multiracial |
64 |
13.6 |
| Identity Not listed (Other) |
46 |
9.7 |
| Prefer not to answer |
18 |
3.8 |
| Ethnicity |
|
|
| Hispanic/Latino |
139 |
29.4 |
| Not Hispanic/Latino |
322 |
68.2 |
| Prefer not to answer |
11 |
2.3 |
| Gender Identity |
|
|
| Woman |
308 |
65.3 |
| Man |
145 |
30.7 |
| Gender Minority |
16 |
3.4 |
| Prefer not to say |
3 |
0.6 |
| Sexual Orientation |
|
|
| Straight/Heterosexual |
352 |
74.6 |
| Sexual Minority |
108 |
22.9 |
| Prefer not to answer |
12 |
2.5 |
| Year in College |
|
|
| Freshmen |
212 |
44.9 |
| Sophomore |
153 |
32.4 |
| Junior |
70 |
14.8 |
| Senior |
34 |
7.2 |
| Graduate Student |
1 |
0.2 |
| Other |
2 |
0.4 |
Table 2.
Means and Standard Deviations for Racial Discrimination in Healthcare, HIB, Mistrust, and Healthcare Avoidance Measures.
Table 2.
Means and Standard Deviations for Racial Discrimination in Healthcare, HIB, Mistrust, and Healthcare Avoidance Measures.
| |
N |
Min-Max |
M (SD) |
| Racial Discrimination in Healthcare |
462 |
1.0 - 12.0 |
4.20 (2.18) |
| Healthcare Institutional Betrayal (HIB) |
458 |
0.0 - 12.0 |
2.94 (2.90) |
| Healthcare Mistrust Appraisal |
469 |
6.0 - 51.0 |
31.63 (9.40) |
| Anticipated Healthcare Avoidance |
463 |
2.0 - 15.0 |
7.56 (3.21) |
| Age in years |
455 |
18.0 - 62.0 |
19.74 (3.96) |
Table 3.
Bivariate Correlations Among Discrimination, Healthcare Institutional Betrayal, Healthcare Mistrust, Anticipated Healthcare Avoidance, and reported Sexual Minority Identity.
Table 3.
Bivariate Correlations Among Discrimination, Healthcare Institutional Betrayal, Healthcare Mistrust, Anticipated Healthcare Avoidance, and reported Sexual Minority Identity.
| |
|
1 |
2 |
3 |
4 |
5 |
| 1. |
Healthcare Avoidance |
|
|
|
|
|
| 2. |
Racial Discrimination |
0.32*** |
- |
|
|
|
| 3. |
Healthcare Inst. Betrayal |
0.48*** |
0.40*** |
- |
|
|
| 4. |
Healthcare Mistrust |
0.45*** |
0.33*** |
0.58*** |
- |
|
| 5. |
Sexual Minority Status |
0.13** |
0.09 |
0.18*** |
0.21*** |
- |
Table 4.
Regression Coefficients, Standard Errors, and Model Summary Information for Racial Discrimination predicting Healthcare Avoidance via Serial Multiple Mediators.
Table 4.
Regression Coefficients, Standard Errors, and Model Summary Information for Racial Discrimination predicting Healthcare Avoidance via Serial Multiple Mediators.
| |
Step 1 |
Step 2 |
Final Model |
| |
|
M1 (HIB) |
M2 (Mistrust) |
Y(HAV) |
|
| Antecedent |
b |
SE |
p |
b |
SE |
p |
b |
SE |
p |
| X (Discrimination) |
.53 |
.06 |
.00 |
.58 |
.19 |
.00 |
.17 |
.07 |
.01 |
| M1 (HIB) |
? |
? |
? |
1.69 |
0.14 |
.00 |
.33 |
.57 |
.00 |
| M2 (Mistrust) |
? |
? |
? |
? |
? |
? |
.08 |
.02 |
.00 |
| Men |
-.06 |
.28 |
.83 |
-1.46 |
.82 |
.75 |
-.47 |
.29 |
.10 |
| Gender Minority |
-1.48 |
.81 |
.07 |
1.19 |
2.35 |
.61 |
2.19 |
.82 |
.01 |
| Sexual Minority |
1.15 |
.32 |
.00 |
1.85 |
.93 |
.05 |
-.18 |
.33 |
.58 |
| Constant |
.53 |
.31 |
.09 |
24.18 |
.91 |
.00 |
3.59 |
.52 |
.00 |
| |
R2 |
R2 |
R2 |
| |
.18 |
.37 |
.31 |
| |
F (4,432) = 23.96
p = .00 |
F (5,431) = 50.95
p = .00 |
F (6,430) = 32.04
p = .00 |
| |
F (4,432) = 23.96
p = .00 |
F (5,431) = 50.95
p = .00 |
|
| |
F (4,432) = 23.96
p = .00 |
F (5,431) = 50.95
p = .00 |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).