Submitted:
19 December 2024
Posted:
20 December 2024
You are already at the latest version
Abstract
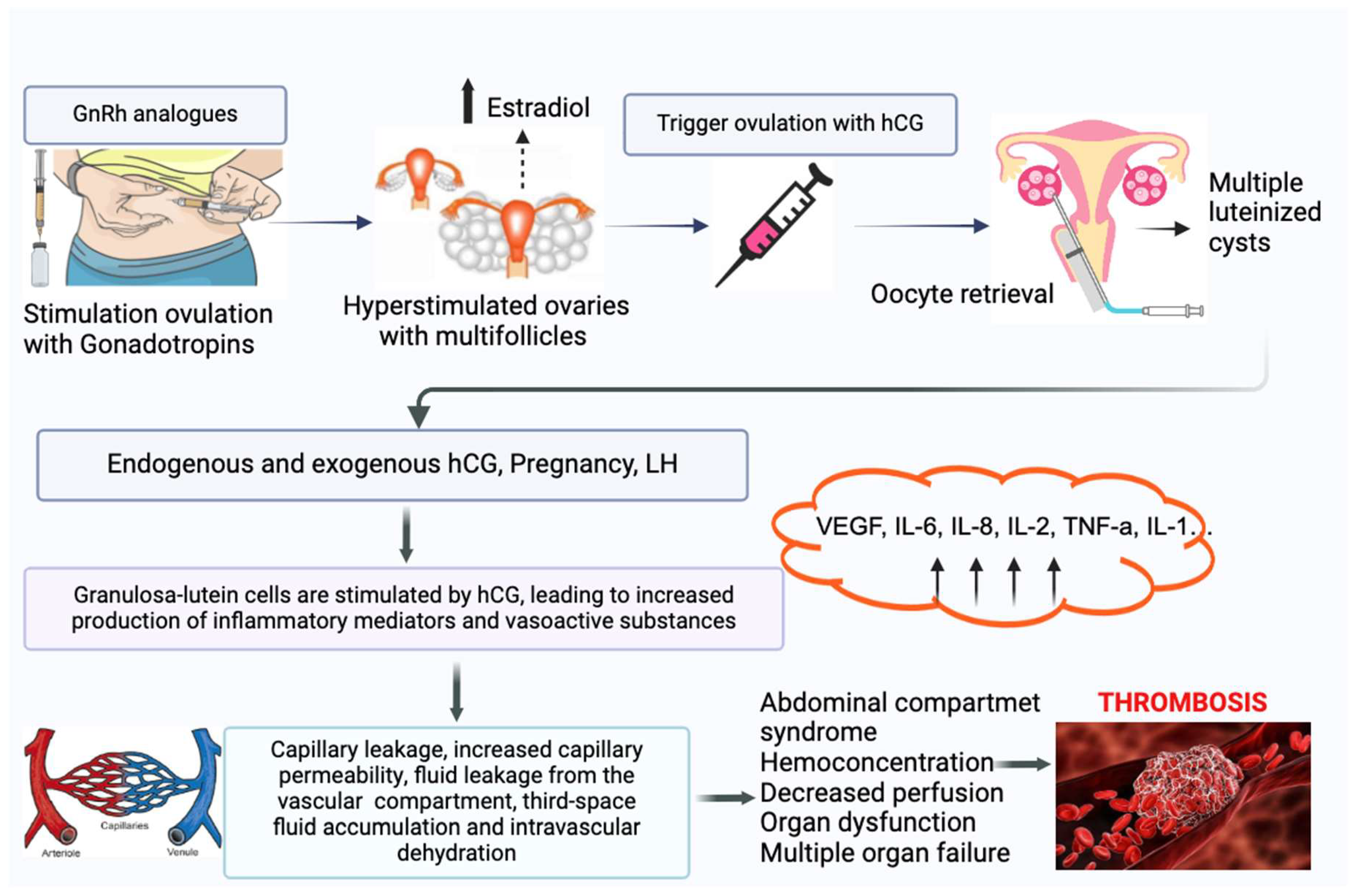
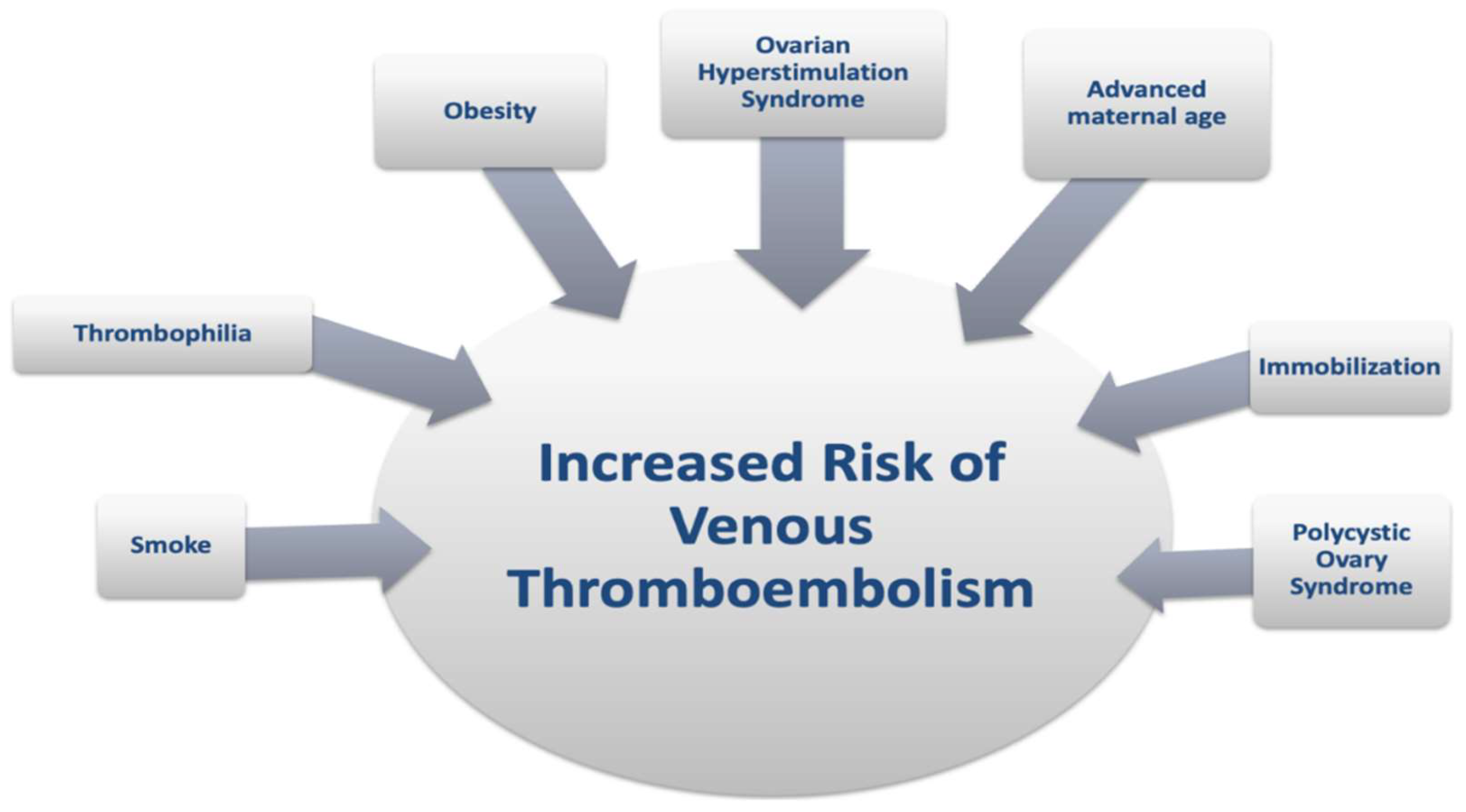
This review summarizes the available literature on the association between IVF treatments and thrombosis, focusing on epidemiology and pathophysiology. Thrombosis is a rare IVF-related complication, with an incidence of approximately 0.2%, dramatically increased by ovarian hyperstimulation syndrome (OHSS). Arterial thrombosis, primarily associated with OHSS, is a rare and early event, while venous thrombosis, although more common, remains a rare complication of IVF. Venous thrombosis often affects the upper body. The thrombotic risk is higher during the first trimester of pregnancy obtained through IVF. This review discusses the impact of risk factors such as OHSS, thrombophilia, obesity, smoking, advanced maternal age, and polycystic ovarian syndrome, which predispose women to thromboembolic events during and after IVF stimulation.
Keywords:
1. Introduction
2. Thrombosis in IVF
2.1. OHSS and Thrombotic Risk
2.2. Arterial Thrombosis in IVF Cycles
2.3. Venous Thrombosis in IVF Cycles
2.4. Anatomical Localization
| Ref | Author | Study design | IVF population(n) | Cycles (n) | ATE (n) | Incidence AT per cycle (n) | ATE localization | Timing of ATE (mean days after hCG) | VTE (n) | Incidence VTE per cycle (n) | VTE localization |
Timing of VTE (mean days after hCG) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1993 | [30] | Delvigne A | Case-control | 384 | na | 0 | 0% | na | na | 1 | 0,01% | brain | na |
| 1995 | [29] | Kodama H | Case-series | 23 | 1316 | 0 | 0% | na | na | 1 | 0,08% | brain | 11 |
| 1998 | [34] | Abramov Y | Case-control | 163 | 163 | 0 | 0% | na | na | 4 | 2,50% | lung | na |
| 1998 | [14] | Serour GI | Case-control | 2924 | 3500 | 2 | 0,05% | brain | na | 4 | 0,12% | upper extremity | na |
| 1998 | [28] | Aboulghar MA | Case reports | 2 | 2 | 0 | 0% | na | na | 2 | 100% | brain | 5 |
| 2002 | [31] | Dulitzky M | Cohort | 61 | na | 1 | na | brain | na | 2 | na | lung | na |
| 2004 | [9] | Grandone E | Case-control | 305 | 747 | 3 | 0,40% | brain, upper extremity | na | 2 | 0,30% | brain; gut | na |
| 2006 | [44] | Yinon Y | Cohort | 24 | 73 | 0 | 0% | na | na | 0 | 0% | na | na |
| 2006 | [25] | Chan WS | Review case series | 37 | 2500 | 0 | 0% | na | na | 37 | 1,48% | upper extremity; neck | 28 |
| 2007 | [15] | Girolami A | Review case series | 34 | na | 34 | na | brain, neck, heart, extremities | 13,7 | 0 | 0% | na | na |
| 2009 | [27] | Salomon O | Case-series | 5 | na | 0 | 0% | na | na | 5 | na | upper extremity; neck | 16 |
| 2009 | [16] | Chan WS | Review case series | 96 | na | 35 | na | brain, neck, heart, extremities | 10.7 | 61 | na | upper extremity; neck | 26.6 |
| 2011 | [38] | Ricci G | Cohort | 480 | 1105 | 0 | 0% | na | na | 0 | 0% | na | na |
| 2012 | [11] | Rova K | Cohort | 19194 | na | 0 | 0% | na | na | 32 | na | na | 45 |
| 2012 | [13] | Hansen AT | Cohort | 30884 | 75141 | 2 | 0,003% | na | na | 7 | 0,009% | na | na |
| 2012 | [26] | Fleming T | Case-series | 2 | 2 | 0 | 0% | na | na | 2 | 100% | neck | 39.5 |
| 2013 | [10] | Henriksson P | Cohort | 23498 | na | 0 | 0% | na | na | 99 | na | lung; other not specified sites | na |
| 2014 | [40] | Hansen AT | Cohort | 18787 | na | 0 | 0% | na | na | 36 | na | lung; other not specified sites | na |
| 2015 | [41] | Villani M | Cohort | 234 | 684 | 0 | 0% | na | na | 6 | 0,88% | lung; lower extremity | na |
| 2017 | [17] | Yang S | Case-series | 38 | na | 29 | na | brain, neck | 8 | 9 | na | brain | 8.33 |
| 2018 | [20] | Villani M | Cohort | 661 | 1836 | 0 | 0% | na | na | 5 | 0,27% | lung; lower extremity | na |
| 2018 | [32] | Grandone E | Cohort | 41 | ns | 0 | 0% | na | na | 41 | na | lung; lower and upper extremity | na |
| 2019 | [18] | Filipovic-Pierrucci A | Cohort | 277913 | 788007 | 78 | 0,01% | na | na | 282 | 0,04% | lung; lower extremity | na |
| 2020 | [33] | Olausson N | Cohort | 30328 | na | 0 | 0% | na | na | 161 | na | lower extremity, gut | na |
2.5. Thrombophilia
2.6. Other Maternal Risk Factors
2.6. Risk of VTE in Pregnancy after IVF
4. Conclusions
Author Contributions
Conflicts of Interest
Acknowledgments
References
- Calhaz-Jorge, C.; De Geyter, C.H.; Kupka, M.S.; Wyns, C.; Mocanu, E.; Motrenko, T.; Scaravelli, G.; Smeenk, J.; Vidakovic, S.; Goossens, V. Survey on ART and IUI: legislation, regulation, funding and registries in European countries: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod Open. 2020, 6, 1–15. [Google Scholar]
- European IVF Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE); Smeenk, J; Wyns, C.; De Geyter, C.; Kupka, M.; Bergh, C.; Cuevas Saiz, I.; De Neubourg, D.; Rezabek, K.; Tandler-Schneider, A.; Rugescu, I.; Goossens, V. ART in Europe, 2019: results generated from European registries by ESHRE. Hum Reprod. 2023, 38, 2321–2338. [Google Scholar]
- Farquhar, C.; Marjoribanks, J.; Brown, J.; Fauser, B.C.J.M.; Lethaby, A.; Mourad, S.; Rebar, R.; Showell, M.; van der Poel, S. Management of ovarian stimulation for IVF: narrative review of evidence provided for World Health Organization guidance. Reprod Biomed Online. 2017, 35, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.M. Venous thrombosis during assisted reproduction: novel risk reduction strategies. Thromb Res. 2013, 131 Suppl 1, S1–S3. [Google Scholar] [CrossRef]
- Grandone, E.; Villani, M. Assisted reproductive technologies and thrombosis. Thromb Res. 2015, 135 (Suppl, 1), S44–S45. [Google Scholar] [CrossRef] [PubMed]
- Kupka, M.S.; Ferraretti, A.P.; de Mouzon, J.; Erb, K.; D'Hooghe, T.; Castilla, J.A.; Calhaz-Jorge, C.; De Geyter, C.; Goossens, V.; European IVF-Monitoring Consortium, for the European Society of Human Reproduction and Embryology. Assisted reproductive technology in Europe, 2010: results generated from European registers by ESHRE†. Hum Reprod. 2014, 29, 2099–2113. [Google Scholar] [PubMed]
- Sennström, M.; Rova, K.; Hellgren, M.; Hjertberg, R.; Nord, E.; Thurn, L.; Lindqvist, P.G. Thromboembolism and in vitro fertilization - a systematic review. Acta Obstet Gynecol Scand. 2017, 96, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Practice Committee of American Society for Reproductive Medicine. Ovarian hyperstimulation syndrome. Fertil Steril. 2008, 90, S188–S193. [Google Scholar] [CrossRef]
- Grandone, E.; Colaizzo, D.; Vergura, P.; Cappucci, F.; Vecchione, G.; Lo Bue, A.; Cittadini, E.; Margaglione, M. Age and homocysteine plasma levels are risk factors for thrombotic complications after ovarian stimulation. Hum Reprod. 2004, 19, 1796–1799. [Google Scholar] [CrossRef] [PubMed]
- Henriksson, P.; Westerlund, E.; Wallén, H.; Brandt, L.; Hovatta, O.; Ekbom, A. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: cross sectional study. BMJ. 2013, 346, 1–11. [Google Scholar] [CrossRef]
- Rova, K.; Passmark, H.; Lindqvist, P.G. Venous thromboembolism in relation to in vitro fertilization: an approach to determining the incidence and increase in risk in successful cycles. Fertil Steril. 2012, 97, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.M. Prophylaxis of VTE in women - during assisted reproductive techniques. Thromb Res. 2009, 123 (Suppl 3), S8–S15. [Google Scholar] [CrossRef]
- Hansen, A.T.; Kesmodel, U.S.; Juul, S.; Hvas, A.M. No evidence that assisted reproduction increases the risk of thrombosis: a Danish national cohort study. Hum Reprod. 2012, 27, 1499–1503. [Google Scholar] [CrossRef] [PubMed]
- Serour, G.I.; Aboulghar, M.; Mansour, R.; Sattar, M.A.; Amin, Y.; Aboulghar, H. Complications of medically assisted conception in 3,500 cycles. Fertil Steril. 1998, 70, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Girolami, A.; Scandellari, R.; Tezza, F.; Paternoster, D.; Girolami, B. Arterial thrombosis in young women after ovarian stimulation: case report and review of the literature. J Thromb Thrombolysis. 2007, 24, 169–174. [Google Scholar] [CrossRef]
- Chan, W.S. The 'ART' of thrombosis: a review of arterial and venous thrombosis in assisted reproductive technology. Curr Opin Obstet Gynecol. 2009, 21, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Yuan, J.; Qin, W.; Li, Y.; Yang, L.; Hu, W. The Clinical Characteristics of Acute Cerebrovascular Accidents Resulting from Ovarian Hyperstimulation Syndrome. Eur Neurol. 2017, 77, 221–230. [Google Scholar] [CrossRef]
- Filipovic-Pierucci, A.; Gabet, A.; Deneux-Tharaux, C.; Plu-Bureau, G.; Olié, V. Arterial and venous complications after fertility treatment: A French nationwide cohort study. Eur J Obstet Gynecol Reprod Biol. 2019, 237, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.S.; Dixon, M.E. The "ART" of thromboembolism: a review of assisted reproductive technology and thromboembolic complications. Thromb Res. 2008, 121, 713–726. [Google Scholar] [CrossRef] [PubMed]
- Villani, M.; Favuzzi, G.; Totaro, P.; Chinni, E.; Vecchione, G.; Vergura, P.; Fischetti, L.; Margaglione, M.; Grandone, E. Venous thromboembolism in assisted reproductive technologies: comparison between unsuccessful versus successful cycles in an Italian cohort. J Thromb Thrombolysis. 2018, 45, 234–239. [Google Scholar] [CrossRef]
- Mozes, M.; Bogokowsky, H.; Antebi, E.; Lunenfeld, B.; Rabau, E.; Serr, D.M.; David, A.; Salomy, M. Thromboembolic phenomena after ovarian stimulation with human gonadotrophins. Lancet. 1965, 2, 1213–1215. [Google Scholar] [CrossRef]
- Kermode, A.G.; Churchyard, A.; Carroll, W.M. Stroke complicating severe ovarian hyperstimulation syndrome. Aust N Z J Med. 1993, 23, 219–220. [Google Scholar] [CrossRef] [PubMed]
- Inbar, O.J.; Levran, D.; Mashiach, S.; Dor, J. Ischemic stroke due to induction of ovulation with clomiphene citrate and menotropins without evidence of ovarian hyperstimulation syndrome. Fertil Steril. 1994, 62, 1075–1076. [Google Scholar] [CrossRef] [PubMed]
- Cluroe, A.D.; Synek, B.J. A fatal case of ovarian hyperstimulation syndrome with cerebral infarction. Pathology. 1995, 27, 344–346. [Google Scholar] [CrossRef]
- Chan, W.S.; Ginsberg, J.S. A review of upper extremity deep vein thrombosis in pregnancy: unmasking the 'ART' behind the clot. J Thromb Haemost. 2006, 4, 1673–1677. [Google Scholar] [CrossRef] [PubMed]
- Fleming, T.; Sacks, G.; Nasser, J. Internal jugular vein thrombosis following ovarian hyperstimulation syndrome. Aust N Z J Obstet Gynaecol. 2012, 52, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Salomon, O.; Schiby, G.; Heiman, Z.; Avivi, K.; Sigal, C.; Levran, D.; Dor, J.; Itzchak, Y. Combined jugular and subclavian vein thrombosis following assisted reproductive technology--new observation. Fertil Steril. 2009, 92, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Aboulghar, M.A.; Mansour, R.T.; Serour, G.I.; Amin, Y.M. Moderate ovarian hyperstimulation syndrome complicated by deep cerebrovascular thrombosis. Hum Reprod. 1998, 13, 2088–2091. [Google Scholar] [CrossRef] [PubMed]
- Kodama, H.; Fukuda, J.; Karube, H.; Matsui, T.; Shimizu, Y.; Tanaka, T. Characteristics of blood hemostatic markers in a patient with ovarian hyperstimulation syndrome who actually developed thromboembolism. Fertil Steril. 1995, 64, 1207–1209. [Google Scholar] [CrossRef] [PubMed]
- Delvigne, A.; Demoulin, A.; Smitz, J.; Donnez, J.; Koninckx, P.; Dhont, M.; Englert, Y.; Delbeke, L.; Darcis, L.; Gordts, S.; et al. The ovarian hyperstimulation syndrome in in-vitro fertilization: a Belgian multicentric study, I. Clinical and biological features. Hum Reprod. 1993, 8, 1353–1360. [Google Scholar] [CrossRef]
- Dulitzky, M.; Cohen, S.B.; Inbal, A.; Seidman, D.S.; Soriano, D.; Lidor, A.; Mashiach, S.; Rabinovici, J. Increased prevalence of thrombophilia among women with severe ovarian hyperstimulation syndrome. Fertil Steril. 2002, 77, 463–467. [Google Scholar] [CrossRef]
- Grandone, E.; Di Micco, P.P.; Villani, M.; Colaizzo, D.; Fernández-Capitán, C.; Del Toro, J.; Rosa, V.; Bura-Riviere, A.; Quere, I.; Blanco-Molina, Á.; Margaglione, M.; Monreal, M.; RIETE Investigators. Venous Thromboembolism in Women Undergoing Assisted Reproductive Technologies: Data from the RIETE Registry. Thromb Haemost. 2018, 118, 1962–1968. [Google Scholar] [CrossRef] [PubMed]
- Olausson, N.; Discacciati, A.; Nyman, A.I.; Lundberg, F.; Hovatta, O.; Westerlund, E.; Wallén, H.N.; Mobarrez, F.; Bottai, M.; Ekbom, A.; Henriksson, P. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilization with fresh respectively frozen-thawed embryo transfer: Nationwide cohort study. J Thromb Haemost. 2020, 18, 1965–1973. [Google Scholar] [CrossRef]
- Abramov, Y.; Elchalal, U.; Schenker, J.G. Obstetric outcome of in vitro fertilized pregnancies complicated by severe ovarian hyperstimulation syndrome: a multicenter study. Fertil Steril. 1998, 70, 1070–1076. [Google Scholar] [CrossRef]
- Bauersachs, R.M.; Manolopoulos, K.; Hoppe, I.; Arin, M.J.; Schleussner, E. More on: the 'ART' behind the clot: solving the mystery. J Thromb Haemost. 2007, 5, 438–439. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.A.; Berg, D.T.; Calnek, D.S.; Ciaccia, A.V.; Joyce, D.E.; Grinnell, B.W. 17beta-estradiol, but not raloxifene, decreases thrombomodulin in the antithrombotic protein C pathway. Endocrinology. 2000, 141, 3908–3911. [Google Scholar] [CrossRef] [PubMed]
- Rogolino, A.; Coccia, M.E.; Fedi, S.; Gori, A.M.; Cellai, A.P.; Scarselli, G.F.; Prisco, D.; Abbate, R. Hypercoagulability, high tissue factor and low tissue factor pathway inhibitor levels in severe ovarian hyperstimulation syndrome: possible association with clinical outcome. Blood Coagul Fibrinolysis. 2003, 14, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Ricci, G.; Bogatti, P.; Fischer-Tamaro, L.; Giolo, E.; Luppi, S.; Montico, M.; Ronfani, L.; Morgutti, M. Factor V Leiden and prothrombin gene G20210A mutation and in vitro fertilization: prospective cohort study. Hum Reprod. 2011, 26, 3068–3077. [Google Scholar] [CrossRef]
- Goualou, M.; Noumegni, S.; de Moreuil, C.; Le Guillou, M.; De Coninck, G.; Hoffmann, C.; Robin, S.; Morcel, K.; Le Moigne, E.; Tremouilhac, C.; Merviel, P.; Le Mao, R.; Leroyer, C.; Bouée, S.; Couturaud, F.; Tromeur, C. Venous Thromboembolism Associated with Assisted Reproductive Technology: A Systematic Review and Meta-analysis. Thromb Haemost. 2023, 123, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.T.; Kesmodel, U.S.; Juul, S.; Hvas, A.M. Increased venous thrombosis incidence in pregnancies after in vitro fertilization. Hum Reprod. 2014, 29, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Villani, M.; Dentali, F.; Colaizzo, D.; Tiscia, G.L.; Vergura, P.; Petruccelli, T.; Petruzzelli, F.; Ageno, W.; Margaglione, M.; Grandone, E. Pregnancy-related venous thrombosis: comparison between spontaneous and ART conception in an Italian cohort. BMJ Open. 2015, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rosendaal, F.R. Risk factors for venous thrombotic disease. Thromb Haemost. 1999, 82, 610–619. [Google Scholar] [CrossRef]
- Grandone, E.; Ageno, W. The Legacy of Edwards and Steptoe and the Windy Roads of Assisted Reproduction: Where Do We Stand with Venous Thromboembolism? Thromb Haemost. 2023, 123, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Yinon, Y.; Pauzner, R.; Dulitzky, M.; Elizur, S.E.; Dor, J.; Shulman, A. Safety of IVF under anticoagulant therapy in patients at risk for thrombo-embolic events. Reprod Biomed Online. 2006, 12, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Bates, S.M.; Greer, I.A.; Middeldorp, S.; Veenstra, D.L.; Prabulos, A.M.; Vandvik, P.O. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012, 141, e691S–e736S. [Google Scholar] [CrossRef] [PubMed]
- Grandone, E.; Piazza, G. Thrombophilia, Inflammation, and Recurrent Pregnancy Loss: A Case-Based Review. Semin Reprod Med. 2021, 39, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Sticchi, E.; Romagnuolo, I.; Cellai, A.P.; Lami, D.; Fedi, S.; Prisco, D.; Noci, I.; Abbate, R.; Fatini, C. Fibrinolysis alterations in infertile women during controlled ovarian stimulation: influence of BMI and genetic components. Thromb Res. 2012, 130, 919–924. [Google Scholar] [CrossRef] [PubMed]
- Gurunath, S.; Vinekar, S.; Biliangady, R. Assisted Reproductive Techniques in a Patient with History of Venous Thromboembolism: A Case Report and Review of Literature. J Hum Reprod Sci. 2018, 11, 193–197. [Google Scholar] [CrossRef]
- Westerlund, E.; Antovic, A.; Hovatta, O.; Eberg, K.P.; Blombäck, M.; Wallén, H.; Henriksson, P. Changes in von Willebrand factor and ADAMTS13 during IVF. Blood Coagul Fibrinolysis. 2011, 22, 127–131. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





