Submitted:
25 October 2024
Posted:
28 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
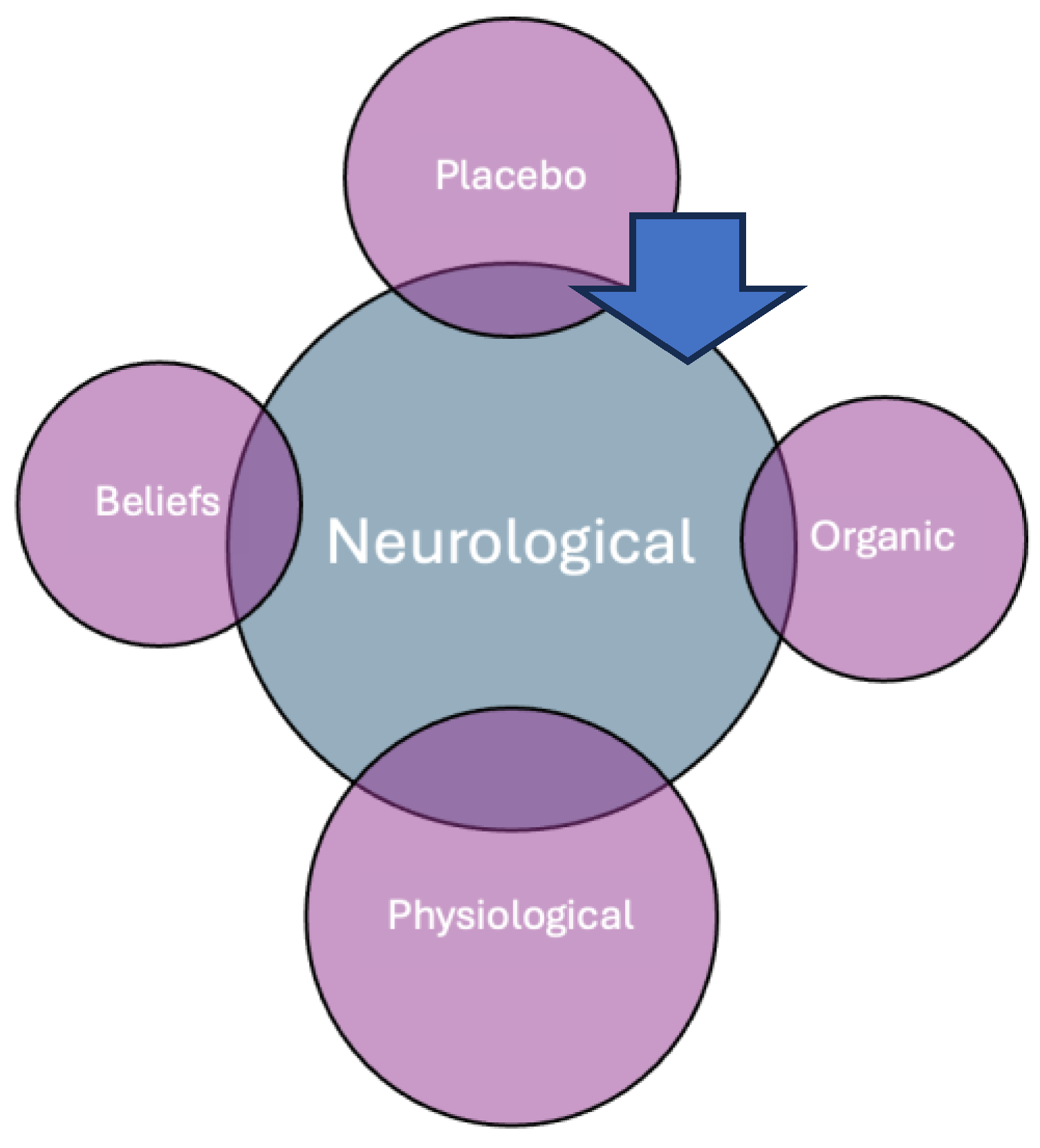
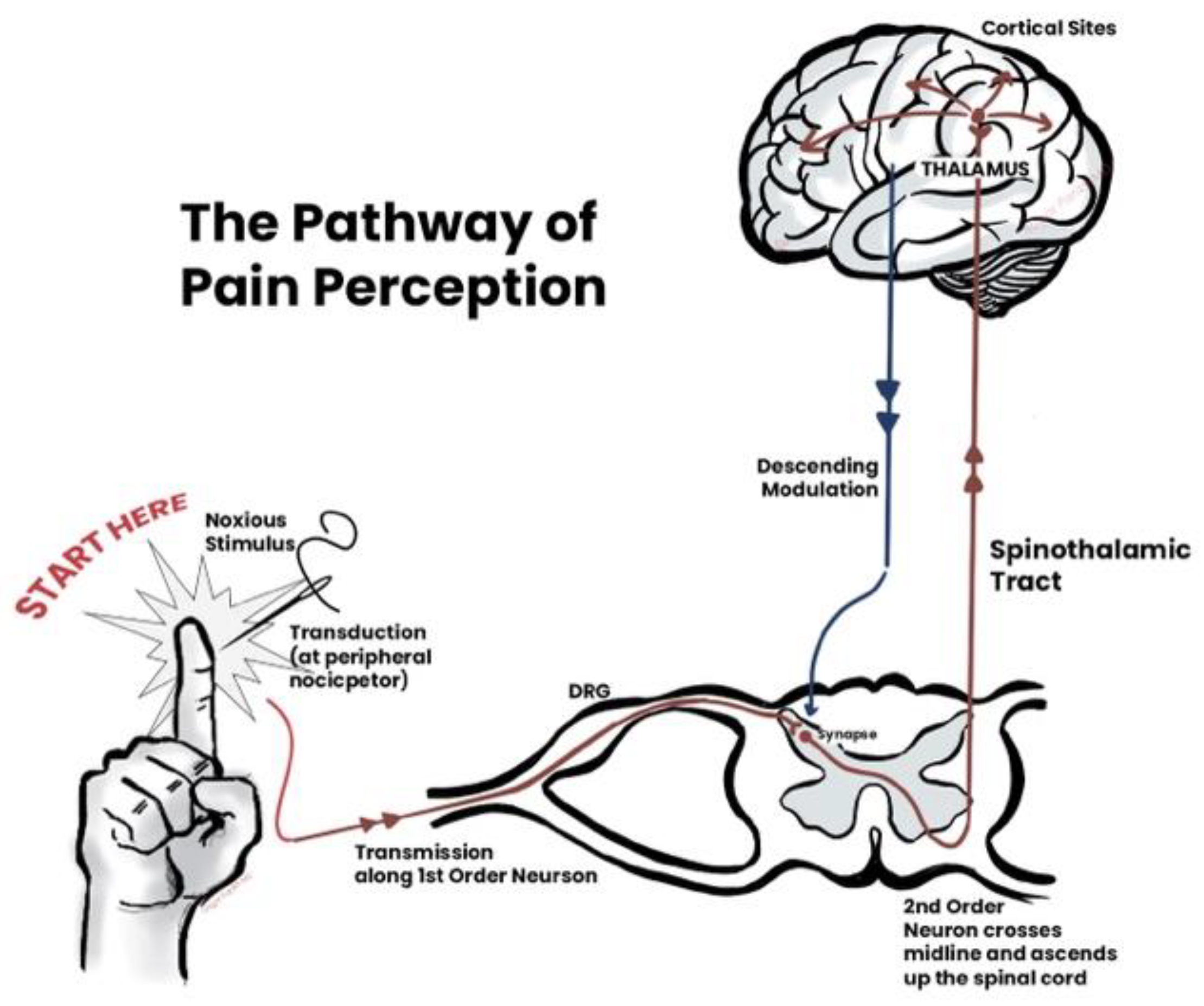
2. Understanding Placebo Effects
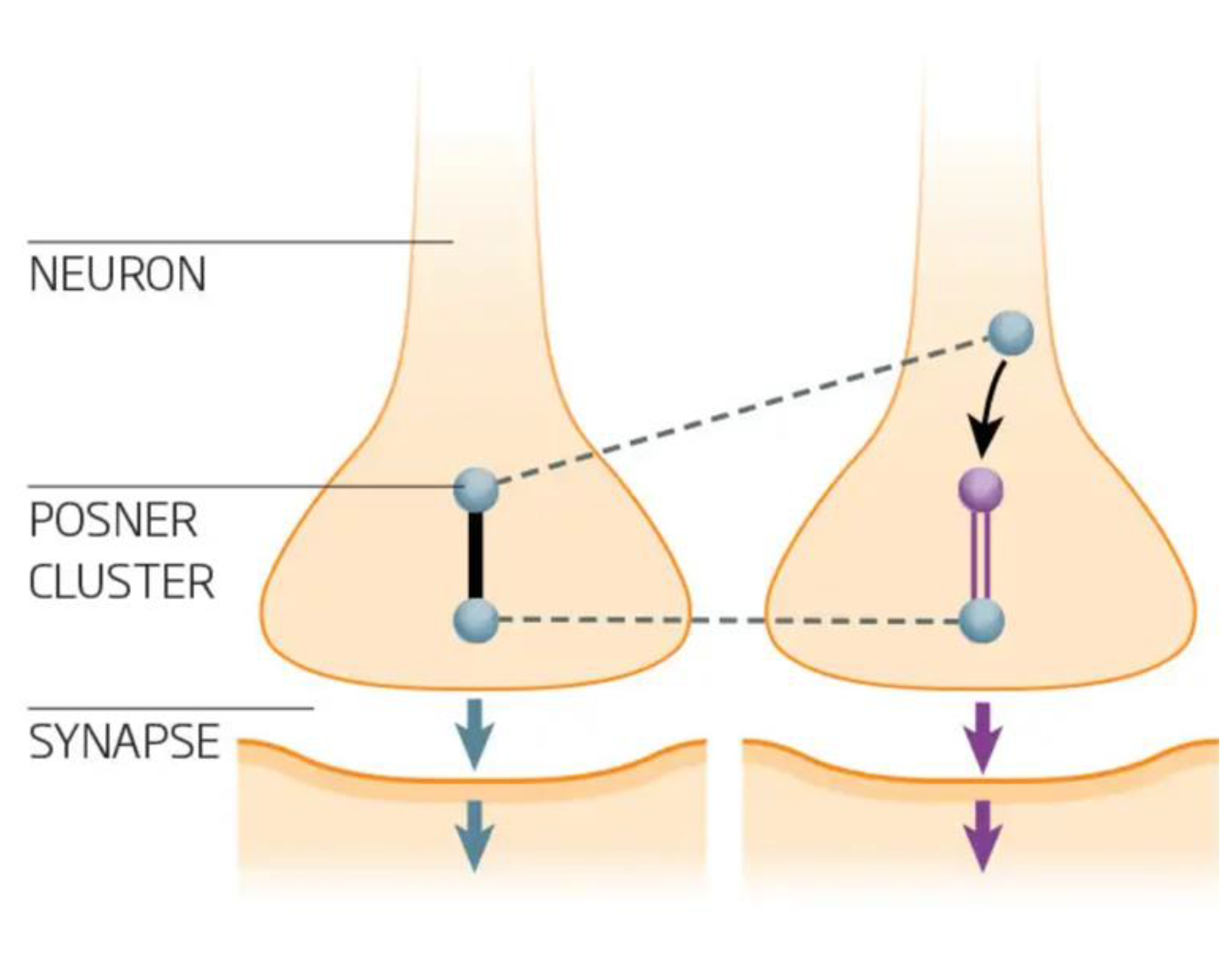
2.1. Quantum Effects
3. Physiological Responses
4. Organic Responses
4.1. Homeopathy
4.2. Meditation
4.3. Simulator Therapies
5. Beliefs
5.1. Religion
5.2. Ideologies
5.3. Discrimination
6. Placebo Prospective Analysis
6.1. Clinical Applications
6.2. Clinica Efficacy Testing
6.2.1. Statistics
6.2.2. Ethics
7. Conclusions
Funding
Conflicts of Interest
References
- Beecher, HK. The powerful placebo. J Am Med Assoc. 1955, 159, 1602–1606. [Google Scholar] [CrossRef] [PubMed]
- Haygarth, Dr John, of the Imagination as a Cause and Cure of Disorders of the Body, Exemplified by Fictitious Tractors. Ann Med (Edinb). 1800, 5, 133–145.
- Kam-Hansen S, Jakubowski M, Kelley JM, Kirsch I, Hoaglin DC, Kaptchuk TJ, et al. Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Sci Transl Med. 2014, 6, 218ra5. [Google Scholar]
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019, 21, 84–90. [Google Scholar] [CrossRef]
- Gupta U, Verma M. Placebo in clinical trials. Perspect Clin Res. 2013, 4, 49–52. [Google Scholar] [CrossRef]
- Miller FG, Colloca L, Kaptchuk TJ. The placebo effect: illness and interpersonal healing. Perspect Biol Med. 2009, 52, 518–539. [Google Scholar] [CrossRef]
- Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005, 16, 1893–1897. [Google Scholar] [CrossRef]
- Chen C, Niehaus JK, Dinc F, Huang KL, Barnette AL, Tassou A, et al. Neural circuit basis of placebo pain relief. Neural circuit basis of placebo pain relief. Nature. 2024. [Google Scholar]
- Eippert F, Bingel U, Schoell ED, Yacubian J, Klinger R, Lorenz J, et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron. 2009, 63, 533–543. [Google Scholar] [CrossRef]
- Lozano AM, Lipsman N, Bergman H, Brown P, Chabardes S, Chang JW, et al. Deep brain stimulation: current challenges and future directions. Nat Rev Neurol. 2019, 15, 148–160. [Google Scholar] [CrossRef]
- Petrovic P, Kalso E, Petersson K.M., Ingvar M. Placebo and opioid analgesia-- imaging a shared neuronal network. Science. 2002, 295, 1737–1740. [Google Scholar] [CrossRef] [PubMed]
- Kaptchuk TJ, Friedlander E, Kelley JM, Sanchez MN, Kokkotou E, Singer JP, et al. Placebos without deception: a randomized controlled trial in irritable bowel syndrome. PLoS One. 2010, 5, e15591. [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. Jama. 2010, 303, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Oken, BS. Placebo effects: clinical aspects and neurobiology. Brain. 2008, 131, 2812–2823. [Google Scholar] [CrossRef]
- Kaptchuk TJ, Goldman P, Stone DA, Stason WB. Do medical devices have enhanced placebo effects? J Clin Epidemiol. 2000, 53, 786–792. [Google Scholar] [CrossRef]
- Liberman, R. An analysis of the placebo phenomenon. Journal of Chronic Diseases. 1962, 15, 761–783. [Google Scholar] [CrossRef]
- Chaput de Saintonge DM, Herxheimer A. Harnessing placebo effects in health care. The Lancet. 1994, 344, 995–998. [Google Scholar] [CrossRef]
- Kaptchuk, TJ. Powerful placebo: the dark side of the randomised controlled trial. The Lancet. 1998, 351, 1722–1725. [Google Scholar] [CrossRef]
- Roberts AH, Kewman DG, Mercier L, Hovell M. The power of nonspecific effects in healing: Implications for psychosocial and biological treatments. Clinical Psychology Review. 1993, 13, 375–391. [Google Scholar] [CrossRef]
- Vickers, AJ. Bibliometric analysis of randomized trials in complementary medicine. Complementary Therapies in Medicine. 1998, 6, 185–189. [Google Scholar] [CrossRef]
- Taub HA, Mitchell JN, Stuber FE, Eisenberg L, Beard MC, McCormack RK. Analgesia for operative dentistry: A comparison of acupuncture and placebo. Oral Surgery, Oral Medicine, Oral Pathology 1979, 48, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Hashish I, Ho Kee H, Harvey W, Feinmann C, Harris M. Reduction of postoperative pain and swelling by ultrasound treatment: a placebo effect. Pain. 1988, 33, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Koes BW, Scholten RJPM, Mens JMA, Bouter LM. Efficacy of epidural steroid injections for low-back pain and sciatica: a systematic review of randomized clinical trials. Pain. 1995, 63, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Johnson, AG. Surgery as a placebo. The Lancet. 1994, 344, 1140–1142. [Google Scholar] [CrossRef]
- Ortega Á, Salazar J, Galban N, Rojas M, Ariza D, Chávez-Castillo M, et al. Psycho-Neuro-Endocrine-Immunological Basis of the Placebo Effect: Potential Applications beyond Pain Therapy. International Journal of Molecular Sciences. 2022, 23, 4196. [Google Scholar] [CrossRef]
- Hartmann H, Rütgen M, Riva F, Lamm C. Another's pain in my brain: No evidence that placebo analgesia affects the sensory-discriminative component in empathy for pain. Neuroimage. 2021, 224, 117397. [Google Scholar] [CrossRef]
- Singer T, Seymour B, O'Doherty J, Kaube H, Dolan RJ, Frith CD. Empathy for pain involves the affective but not sensory components of pain. Science. 2004, 303, 1157–1162. [Google Scholar] [CrossRef]
- Rizzolatti G, Craighero L. The mirror-neuron system. Annu Rev Neurosci. 2004, 27, 169–192. [Google Scholar] [CrossRef]
- Keysers C, Gazzola V. Expanding the mirror: vicarious activity for actions, emotions, and sensations. Curr Opin Neurobiol. 2009, 19, 666–671. [Google Scholar] [CrossRef]
- Weingarten CP, Doraiswamy PM, Fisher MP. A New Spin on Neural Processing: Quantum Cognition. Front Hum Neurosci. 2016, 10, 541. [Google Scholar]
- Lambert N, Chen Y-N, Cheng Y-C, Li C-M, Chen G-Y, Nori F. Quantum biology. Nature Physics. 2013, 9, 10–18. [Google Scholar] [CrossRef]
- Scheiblich H, Eikens F, Wischhof L, Opitz S, Jüngling K, Cserép C, et al. Microglia rescue neurons from aggregate-induced neuronal dysfunction and death through tunneling nanotubes. Neuron. 2024.
- Frömer R, Nassar MR, Ehinger BV, Shenhav A. Common neural choice signals can emerge artefactually amid multiple distinct value signals. Common neural choice signals can emerge artefactually amid multiple distinct value signals. Nat Hum Behav. 2024. [Google Scholar]
- Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. 2015, 16, 403–418. [Google Scholar] [CrossRef]
- Hameroff S, Penrose R. Consciousness in the universe: a review of the 'Orch OR' theory. Phys Life Rev. 2014, 11, 39–78. [Google Scholar] [CrossRef]
- Fisher MPA. Quantum cognition: The possibility of processing with nuclear spins in the brain. Annals of Physics. 2015, 362, 593–602. [Google Scholar] [CrossRef]
- Tegmark, M. Importance of quantum decoherence in brain processes. Physical review E. 2000, 61, 4194. [Google Scholar] [CrossRef]
- Greenberg, SJ. On the history of New York Medical College. N Y Med Q. 1986, 6, 116–119. [Google Scholar]
- Shang A, Huwiler-Müntener K, Nartey L, Jüni P, Dörig S, Sterne JA, et al. Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy. Lancet. 2005, 366, 726–732. [Google Scholar] [CrossRef]
- Cucherat M, Haugh MC, Gooch M, Boissel JP. Evidence of clinical efficacy of homeopathy. A meta-analysis of clinical trials. HMRAG. Homeopathic Medicines Research Advisory Group. Eur J Clin Pharmacol. 2000, 56, 27–33. [Google Scholar]
- Commons UHo. Science and Technology Committee - Fourth Report Evidence Check 2: Homeopathy. Available online: https://publications.parliament.uk/pa/cm200910/cmselect/cmsctech/45/4502.htm2010.
- Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013, 29, 450–460. [Google Scholar] [CrossRef] [PubMed]
- India NCoH. Homeopathy. Available online: https://www.nch.org.in/2024.
- Varanasi R, Srivastava A, Kumar Rt S, Bala R. Practice, prescription habits, experience and perception of Indian homeopathic practitioners in treatment of diabetes mellitus: An online observational study. J Ayurveda Integr Med. 2023, 14, 100787. [Google Scholar] [CrossRef] [PubMed]
- Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, et al. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012, 5, 750–758. [Google Scholar] [CrossRef]
- Piske M, Thomson T, Krebs E, Hongdilokkul N, Bruneau J, Greenland S, et al. Comparative effectiveness of buprenorphine-naloxone versus methadone for treatment of opioid use disorder: a population-based observational study protocol in British Columbia, Canada. BMJ Open. 2020, 10, e036102. [Google Scholar] [CrossRef]
- Maria Carmen B-G, Sandra M-R, Marta R-A. Present and Future Pharmacological Treatments for Opioid Addiction. In: Pilar Almela R, editor. Opioids. Rijeka: IntechOpen; 2019. p. Ch. 6.
- Noble F, Marie N. Management of Opioid Addiction With Opioid Substitution Treatments: Beyond Methadone and Buprenorphine. Frontiers in Psychiatry. 2019, 9.
- Tai MDS, Gamiz-Arco G, Martinez A. Dopamine synthesis and transport: current and novel therapeutics for parkinsonisms. Biochemical Society Transactions. 2024, 52, 1275–1291. [Google Scholar] [CrossRef]
- Siegel JS, Subramanian S, Perry D, Kay BP, Gordon EM, Laumann TO, et al. Psilocybin desynchronizes the human brain. Nature. 2024, 632, 131–138. [Google Scholar] [CrossRef]
- Faresjö R, Lindberg H, Ståhl S, Löfblom J, Syvänen S, Sehlin D. Transferrin Receptor Binding BBB-Shuttle Facilitates Brain Delivery of Anti-Aβ-Affibodies. Pharm Res. 2022, 39, 1509–1521. [Google Scholar] [CrossRef]
- Kakinen A, Jiang Y, Davis TP, Teesalu T, Saarma M. Brain Targeting Nanomedicines: Pitfalls and Promise. Int J Nanomedicine. 2024, 19, 4857–4875. [Google Scholar] [CrossRef]
- The Lancet Regional Health – E. Psychedelic-assisted psychotherapy: hope and dilemma. The Lancet Regional Health – Europe. 2023, 32.
- D'Onofrio V, Manzo N, Guerra A, Landi A, Baro V, Määttä S, et al. Combining Transcranial Magnetic Stimulation and Deep Brain Stimulation: Current Knowledge, Relevance and Future Perspectives. Brain Sci. 2023, 13.
- Tosti B, Corrado S, Mancone S, Di Libero T, Rodio A, Andrade A, et al. Integrated use of biofeedback and neurofeedback techniques in treating pathological conditions and improving performance: a narrative review. Front Neurosci. 2024, 18, 1358481. [Google Scholar] [CrossRef]
- Triana-Del Rio R, Ranade S, Guardado J, LeDoux J, Klann E, Shrestha P. The modulation of emotional and social behaviors by oxytocin signaling in limbic network. Frontiers in Molecular Neuroscience. 2022, 15. [Google Scholar]
- De Gregorio D, Aguilar-Valles A, Preller KH, Heifets BD, Hibicke M, Mitchell J, et al. Hallucinogens in Mental Health: Preclinical and Clinical Studies on LSD, Psilocybin, MDMA, and Ketamine. The Journal of Neuroscience. 2021, 41, 891–900. [Google Scholar] [CrossRef]
- Pearce MJ, Koenig HG, Robins CJ, Nelson B, Shaw SF, Cohen HJ, et al. Religiously integrated cognitive behavioral therapy: a new method of treatment for major depression in patients with chronic medical illness. Psychotherapy (Chic). 2015, 52, 56–66. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama. 2013, 310, 2191–2194. [CrossRef]
- FDA. Real-World Data: Assessing Electronic Health Records and Medical Claims Data To Support Regulatory Decision-Making for Drug and Biological Products. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/real-world-data-assessing-electronic-health-records-and-medical-claims-data-support-regulatory2024.
- Eapen ZJ, Lauer MS, Temple RJ. The imperative of overcoming barriers to the conduct of large, simple trials. Jama. 2014, 311, 1397–1398. [Google Scholar] [CrossRef]
- Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021, 397, 1637–1645.
- Millum J, Grady C. The ethics of placebo-controlled trials: methodological justifications. Contemp Clin Trials. 2013, 36, 510–514. [Google Scholar] [CrossRef]
- Niazi, S. Scientific Rationale for Waiving Clinical Efficacy Testing of Biosimilars. Drug Des Devel Ther. 2022, 16, 2803–2815. [Google Scholar] [CrossRef]
- Niazi, SK. Support for Removing Pharmacodynamic and Clinical Efficacy Testing of Biosimilars: A Critical Analysis. Clin Pharmacol Drug Dev. 2023. [Google Scholar] [CrossRef] [PubMed]
- Koog YH, We SR, Min BI. Three-armed trials including placebo and no-treatment groups may be subject to publication bias: systematic review. PLoS One. 2011, 6, e20679. [Google Scholar]
- Stridh A, Pontén M, Arver S, Kirsch I, Abé C, Jensen KB. Placebo Responses Among Men With Erectile Dysfunction Enrolled in Phosphodiesterase 5 Inhibitor Trials: A Systematic Review and Meta-analysis. JAMA Network Open. 2020, 3, e201423. [Google Scholar] [CrossRef] [PubMed]
- Howick J, Friedemann C, Tsakok M, Watson R, Tsakok T, Thomas J, et al. Are treatments more effective than placebos? A systematic review and meta-analysis. PLoS One. 2013, 8, e62599. [Google Scholar]
- FDA. Conducting Clinical Trials With Decentralized Elements Guidance for Industry, Investigators, and Other Interested Parties. Available online: https://www.fda.gov/media/167696/download2024.
- FDA. Good Clinical Practice. Available online: https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/regulations-good-clinical-practice-and-clinical-trials2024.
- FDA. Clinical Trials and Human Subject Protection. Available online: https://www.fda.gov/science-research/science-and-research-special-topics/clinical-trials-and-human-subject-protection2024.
- FDA. FDA Issues Draft Guidance on Conducting Multiregional Clinical Trials in Oncology. Available online: https://www.fda.gov/news-events/press-announcements/fda-issues-draft-guidance-conducting-multiregional-clinical-trials-oncology2024.
- FDA. Conducting Clinical Trials With Decentralized Elements. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/conducting-clinical-trials-decentralized-elements2024.
- Tannenholz L, Jimenez JC, Kheirbek MA. Local and regional heterogeneity underlying hippocampal modulation of cognition and mood. Frontiers in Behavioral Neuroscience. 2014, 8. [Google Scholar]
- van Prooijen JW, van Vugt M. Conspiracy Theories: Evolved Functions and Psychological Mechanisms. Perspect Psychol Sci. 2018, 13, 770–788. [Google Scholar] [CrossRef]
- van Elk M, Aleman A. Brain mechanisms in religion and spirituality: An integrative predictive processing framework. Neurosci Biobehav Rev. 2017, 73, 359–378. [Google Scholar] [CrossRef]
- Peciña M, Zubieta J-K. Molecular Mechanisms of Placebo Responses In Humans. Molecular psychiatry. 2014, 20, 416–23. [Google Scholar]
- Scheffer M, Borsboom D, Nieuwenhuis S, Westley F. Belief traps: Tackling the inertia of harmful beliefs. Proceedings of the National Academy of Sciences. 2022, 119, e2203149119. [Google Scholar] [CrossRef]
- Kapogiannis D, Barbey AK, Su M, Zamboni G, Krueger F, Grafman J. Cognitive and neural foundations of religious belief. Proc Natl Acad Sci U S A. 2009, 106, 4876–4881. [Google Scholar] [CrossRef]
- Kaplan JT, Gimbel SI, Harris S. Neural correlates of maintaining one's political beliefs in the face of counterevidence. Sci Rep. 2016, 6, 39589. [Google Scholar] [CrossRef] [PubMed]
- Wiech K, Farias M, Kahane G, Shackel N, Tiede W, Tracey I. An fMRI study measuring analgesia enhanced by religion as a belief system. PAIN. 2008, 139, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Geoffrey, A.; Flagellation. Encyclopedia Britannica. Available online: https://www.britannica.com/topic/flagellation (accessed on 25 March 2023).
- Timmann D, Drepper J, Frings M, Maschke M, Richter S, Gerwig M, et al. The human cerebellum contributes to motor, emotional and cognitive associative learning. A review. Cortex. 2010, 46, 845–857. [Google Scholar] [CrossRef] [PubMed]
- Asp E, Ramchandran K, Tranel D. Authoritarianism, religious fundamentalism, and the human prefrontal cortex. Neuropsychology. 2012, 26, 414–421. [Google Scholar] [CrossRef]
- Jost JT, Baldassarri DS, Druckman JN. Cognitive–motivational mechanisms of political polarization in social-communicative contexts. Nature Reviews Psychology. 2022, 1, 560–576. [Google Scholar] [CrossRef]
- Nickerson, RS. Confirmation Bias: A Ubiquitous Phenomenon in Many Guises. Review of General Psychology. 1998, 2, 175–220. [Google Scholar] [CrossRef]
- Amodio DM, Jost JT, Master SL, Yee CM. Neurocognitive correlates of liberalism and conservatism. Nat Neurosci. 2007, 10, 1246–1247. [Google Scholar] [CrossRef]
- Izuma K, Matsumoto M, Murayama K, Samejima K, Sadato N, Matsumoto K. Neural correlates of cognitive dissonance and choice-induced preference change. Proc Natl Acad Sci U S A. 2010, 107, 22014–22019. [Google Scholar] [CrossRef]
- Bellavite P, Conforti A, Piasere V, Ortolani R. Immunology and homeopathy. 1. Historical background. Evid Based Complement Alternat Med. 2005, 2, 441–452. [Google Scholar] [CrossRef]
- Nations, U. Universal Declaration of Human Rights. Available online: https://www.un.org/en/about-us/universal-declaration-of-human-rights1948.
- United States. Congress. House. A Bill to establish a Biotechnology Science Coordinating Committee to address scientific problems caused by genetically-engineered organisms and a Biotechnology Science Research Program to support research and regulation of the biotechnology sciences; to regulate the release of genetically-engineered organisms into the environment and the use of such organisms in manufacturing and agricultural activities; and for other purposes. 39 p. p.
- Matarèse BFE, Rusin A, Seymour C, Mothersill C. Quantum Biology and the Potential Role of Entanglement and Tunneling in Non-Targeted Effects of Ionizing Radiation: A Review and Proposed Model. International Journal of Molecular Sciences. 2023, 24, 16464. [Google Scholar] [CrossRef]
- Chvetzoff Gl, Tannock IF. Placebo Effects in Oncology. JNCI: Journal of the National Cancer Institute. 2003, 95, 19–29. [Google Scholar] [CrossRef]
- Fleming G, Scholes G, Cheng Y-C. Quantum effects in biology. Procedia Chemistry. 2011, 3, 38–57. [Google Scholar] [CrossRef]
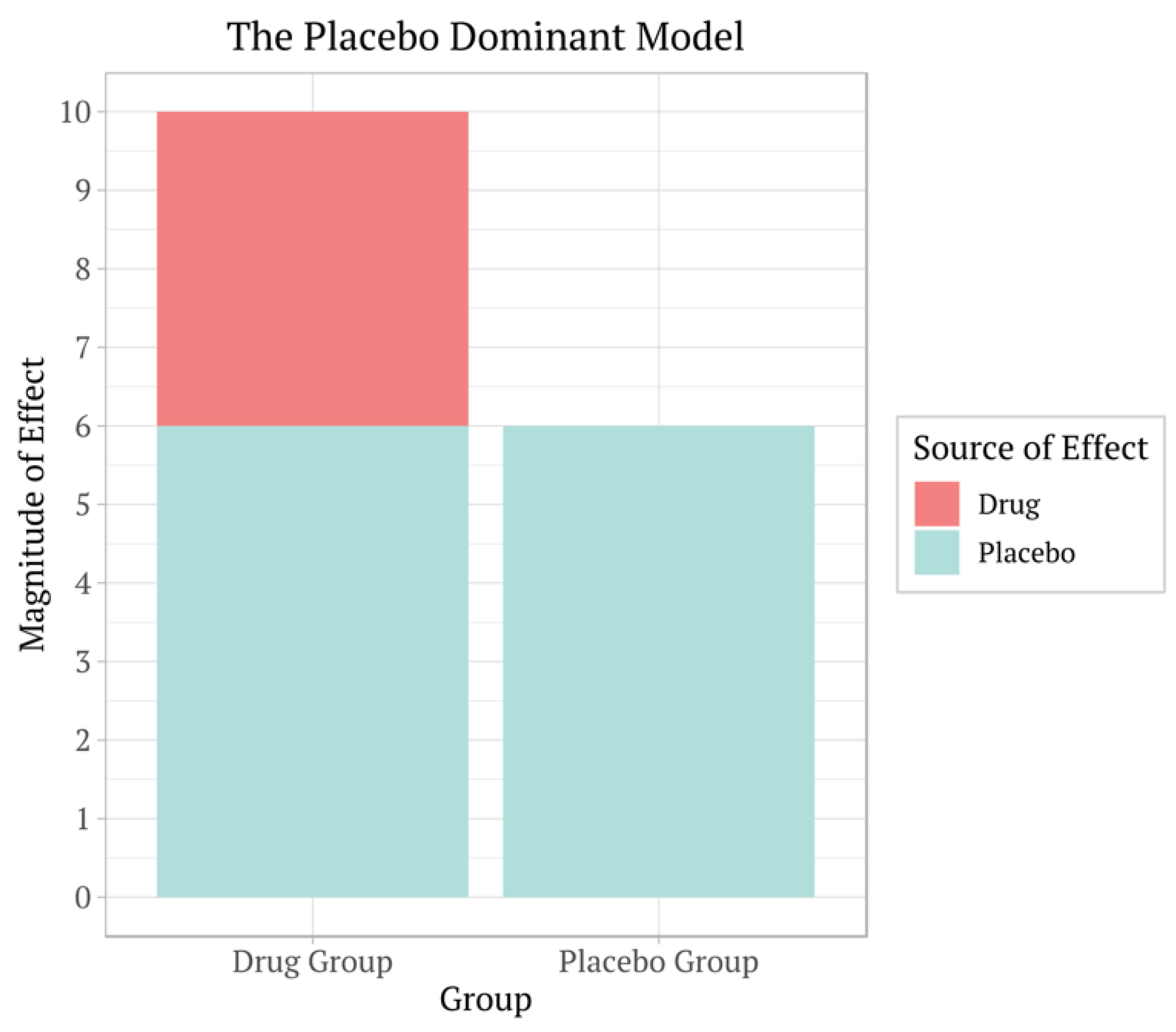
| Efficacy of Drug | Efficacy of Placebo | Statistics | Resolution |
| +++, ++, + | +++, ++, + | Non-significant | Reject. Only homeopathy has addressed this; no Agency will approve such drugs, |
| 0 | 0 | Non-significant | Rejected |
| +++ | ++ | Significant | Approved based on difference as a response. |
| + | ++ | Significant | Rejected based on additional effects of the drug. |
| +++, ++, + | Placebo arm removed | Significant | A much smaller study size reduced unnecessary exposure to humans. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




