1. Introduction
The coronavirus disease, referred to as COVID-19 by the WHO, was declared a pandemic on March 11th, 2020. It was known to first emerge in Wuhan, China and quickly spread throughout the world 1. There was noted to be a disruption in the delivery of essential health services2. Elective surgeries were canceled as a public health measure3. Hospitals were required to stop performing in-hospital elective surgeries as COVID-19 cases rose during later waves of the pandemic4.
In the United States, New York City (NYC) was disproportionately impacted by COVID-19. During the initial wave, nonessential services were ordered to close and stay-at-home orders were issued5. The multimodal impact of COVID-19 on the healthcare field was significant. Cancellations occurred across multiple fields of surgery. The pandemic impacted surgical training as well. Several surgical fields have case log minima, but the Accreditation Council for Graduate Medical Education (ACGME) posited that the pandemic would lead to the reduction of elective operations completed by residents and that it was up to the Program Director to assess residents’ competence6.
Elective surgical procedures were suspended in NYC between March 16 and June 15, 20207. Beginning April 28, 2020, hospitals were allowed to resume elective outpatient treatments under certain conditions. It was posited that if a county or hospital that had resumed elective surgeries experienced a significant increase in cases, elective surgeries would have to stop8.
Of particular interest in studies of the pandemic’s effect on healthcare is the Far Rockaway region of Queens, New York, which has an estimated population of 134,7009. Data through September 2022 suggests the area had a case rate of 32960.24 per 100,000 people and death rate of 933.35 per 100,00 people-which is greater than the overall rates for Queens and NYC10. Far Rockaway is served primarily by St. John’s Episcopal Hospital, a 257-bed facility, serving as a safety net hospital where 90% of patients have government insurance11. The racial demographics of the area must be noted; per the 2010 census the population of Far Rockaway was 44.7% African American and 24.7% Hispanic10. African American and Hispanic individuals had higher rates of COVID-19 than Caucasians12. Estimates posit that 23.8% of people in the area lived below the poverty line which was more than 1.5 times the rate in NYC13.
St. John’s Episcopal Hospital serves a large nursing home population. Studies of the pandemic’s effect on this hospital in large reflect the impact on the nursing home population. Within Far Rockaway, there are 11 nursing homes within the 11691 zip code, with 2049 beds14. Nursing homes were hard hit during the pandemic. A New York Times analysis suggested that over 172,000 residents and employees of nursing homes and long-term care facilities died due to COVID-related complications. A State Health Department report raised questions about how the state reported nursing home deaths and some sources suggested the administration undercounted them15. Letitia James, the attorney general of New York, released a report stating that the Cuomo administration had understated the number of COVID-19 deaths in nursing homes by 50%16. Such information underscores the impact that the pandemic had on nursing homes. Statewide data from 2020 suggested that there were 7177 cases of COVID in nursing homes across New York State, with 6432 deaths17. In comparison, nationwide data from the Centers for Medicare & Medicaid Services indicates that there has been a total of 1,297,914 resident COVID-19 confirmed cases and 159,126 deaths (fatality rate ~12%) 18. This impact on nursing home populations significantly impacted St. John’s Episcopal Hospital.
Several studies have been conducted on the impact of the pandemic on the various aspects of Ophthalmology. It is suggested that compared to other specialties, the field of Ophthalmology experienced one of the largest declines in patient visits as a result of the pandemic. One study suggests that average Ophthalmology case logs in the United States in 2020 were lower than the averages in 201919.
To our knowledge, no study has examined the impact of COVID-19 surgical rates in Ophthalmology among the various waves of the COVID pandemic through the years, and specifically in medically underserved areas such as Far Rockaway that are served by a single hospital. This knowledge will contribute to a broader understanding of the pandemic’s multifaceted impacts on the healthcare system in underserved regions-as well as help be prepared in case of further pandemics.
2. Methods
This study was conducted as a retrospective chart review. The research protocol was submitted to the Institutional Review Board (IRB) for approval. All appropriate institutional approvals were obtained by St. John’s Episcopal Hospital IRB number EHS-22a002. Waivers for informed consent was obtained as no patient or subject identifying data was included. This study is in full accordance with the Declaration of Helsinki20. Patient information was de-identified during analysis. Consent for collection, analysis, and storage of data was waived. The health, privacy and rights of patients were fully respected. Risks to patients and their health care information was minimized as it was treated in an anonymous matter.
Data from the St. John’s Episcopal Operating Room records was obtained, concerning completed surgical procedures by service and by month between January 2018 and February 2022.
Cases were grouped into four major time categories: pre-covid (January 2018 to February 2020), first wave (March 2020 through May 2021), delta (June 2021 through December 2021), and omicron (January 2022 onwards). This specific grouping was chosen as it reflected the pattern with which the United States as a nation was most severely affected, defined based on Centers for Disease Control and Prevention’s definitions based on national trends21.
The fields of Ear, Nose and Throat (ENT), General Surgery, Orthopedic Surgery, Pain Management, Podiatry and Ophthalmology were analyzed. An average number of procedures per surgical subspecialty per wave was calculated, and for each subspecialty, differences between the average surgical count in each wave were studied using two-tailed t-test. Similar analysis was done for each type of Ophthalmology surgery, where the average surgical counts were compared between individual waves using two-tailed t-test.
The authors report no disclosure of financial or personal relationships that could influence this work. There were no funding sources or financial support required for this project.
3. Results
Specialty Analysis
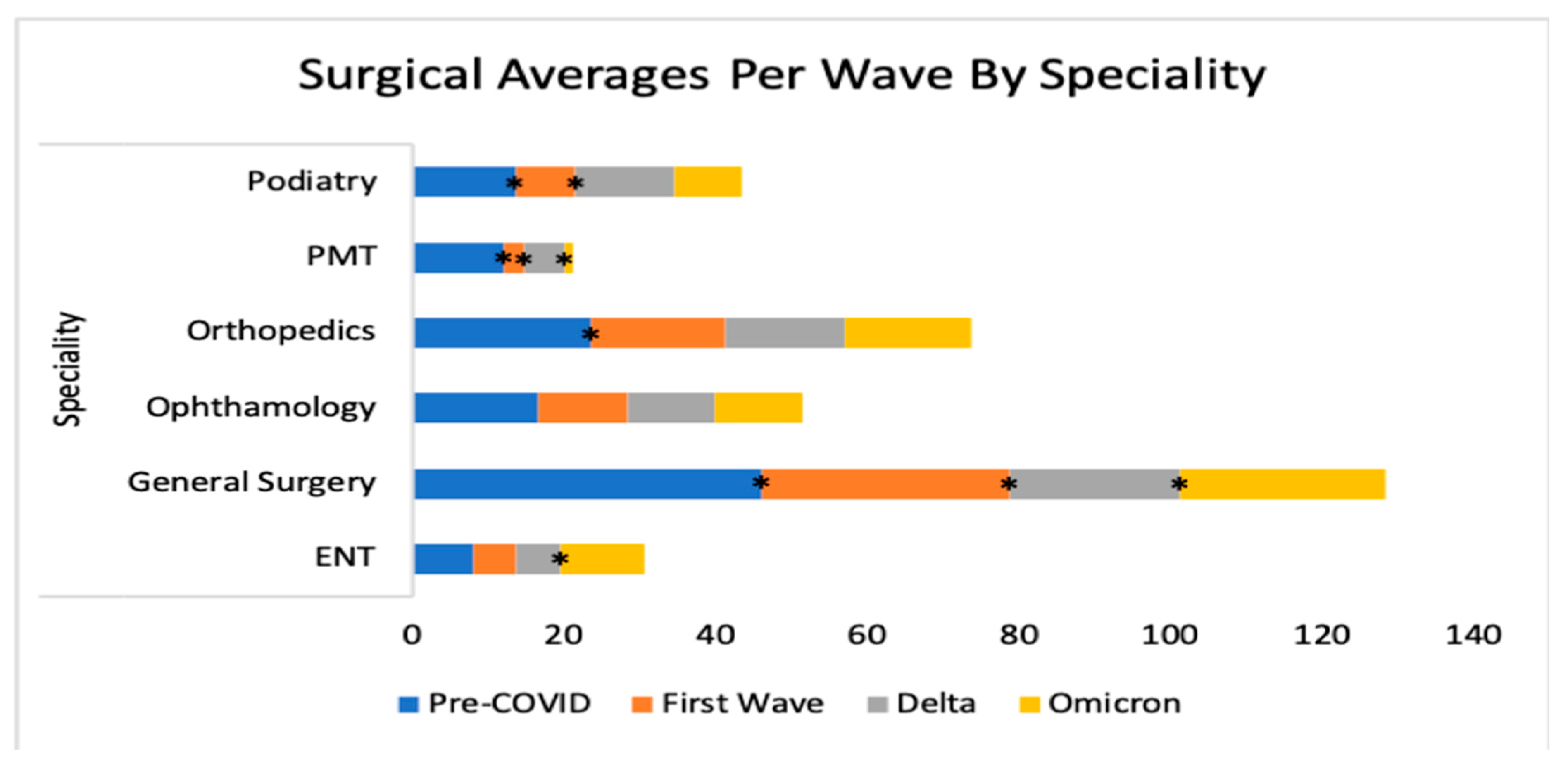
Statistically significant changes were detected when comparing pre-covid numbers to numbers during the first wave in ENT, General Surgery, Orthopedic Surgery, Pain Management, Podiatry and Ophthalmology (Table I and
Figure 1).
Table I: Surgical Numbers by COVID wave.
| ENT |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-2.48 |
-30.50 |
0.01 |
| |
pre-covid vs. delta |
-2.230 |
-28.17 |
0.04 |
| |
pre-covid vs. omicron |
2.85 |
34.91 |
0.04 |
| |
first wave vs. delta |
0.19 |
3.36 |
0.89 |
| |
first wave vs. omicron |
2.85 |
50.23 |
0.03 |
| |
delta vs. omicron |
5.14 |
87.81 |
0.05 |
| SURG |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-13.62 |
-29.51 |
0.00 |
| |
pre-covid vs. delta |
-13.62 |
-29.51 |
9.63E-06 |
| |
pre-covid vs. omicron |
-19.15 |
-41.50 |
0.02 |
| |
first wave vs. delta |
-9.82 |
-30.18 |
0.01 |
| |
first wave vs. omicron |
-19.15 |
-58.87 |
0.36 |
| |
delta vs. omicron |
4.28 |
18.87 |
0.03 |
| OPT |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-4.96 |
-29.71 |
0.00 |
| |
pre-covid vs. delta |
-5.14 |
-30.77 |
0.00 |
| |
pre-covid vs. omicron |
-5.19 |
-31.11 |
0.08 |
| |
first wave vs. delta |
-0.18 |
-1.52 |
0.95 |
| |
first wave vs. omicron |
-5.19 |
-44.25 |
0.96 |
| |
delta vs. omicron |
-0.06 |
-0.49 |
0.97 |
| ORT |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-6.130 |
-25.83 |
0.00 |
| |
pre-covid vs. delta |
-7.87 |
-33.18 |
0.00 |
| |
pre-covid vs. omicron |
-7.23 |
-30.47 |
0.06 |
| |
first wave vs. delta |
-1.74 |
-9.90 |
0.49 |
| |
first wave vs. omicron |
-1.1 |
-6.25 |
0.38 |
| |
delta vs. omicron |
0.64 |
4.05 |
0.86 |
| PMT |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-9.38 |
-77.44 |
7.00E-09 |
| |
pre-covid vs. delta |
-6.69 |
-55.19 |
0.00 |
| |
pre-covid vs. omicron |
-11.11 |
-91.75 |
0.00 |
| |
first wave vs. delta |
2.69 |
98.61 |
0.01 |
| |
first wave vs. omicron |
-1.73 |
-63.42 |
0.34 |
| |
delta vs. omicron |
-4.43 |
-81.58 |
0.01 |
| POD |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-5.68 |
-41.73 |
0.00 |
| |
pre-covid vs. delta |
-0.61 |
-4.52 |
0.75 |
| |
pre-covid vs. omicron |
-4.61 |
-0.34 |
0.15 |
| |
first wave vs. delta |
5.07 |
0.64 |
0.01 |
| |
first wave vs. omicron |
1.07 |
0.13 |
0.71 |
| |
delta vs. omicron |
-4 |
-0.31 |
0.30 |
ENT: Ear, Nose and Throat; SURG: General Surgery; OPT: Ophthalmology; ORT: Orthopedic Surgery; PMT: Pain Management; POD: Podiatry.
Several surgical numbers, including those in the field of Ophthalmology, fell between pre-covid and the first wave. Some fields experienced a rebound after the initial ban on surgeries was lifted.
In ENT and General Surgery statistically significant changes were found when comparing the pre-covid time to every subsequent wave and several such changes were found in Ophthalmology as well (Table II and
Figure 1). For example, in ENT, there was a -28.2% fall in cases between pre-covid and delta (p<.05).
Table II: Ophthalmology Surgery Analysis by COVID wave.
| Enucleation |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.07 |
0 |
0.19 |
| |
pre-covid vs. delta |
0 |
0 |
0 |
| |
pre-covid vs. omicron |
0 |
0 |
0 |
| |
first wave vs. delta |
-0.07 |
-100 |
0.50 |
| |
first wave vs. omicron |
-0.07 |
-100 |
0.73 |
| |
delta vs. omicron |
0 |
0 |
0 |
| Evisceration |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.03 |
73.33 |
0.70 |
| |
pre-covid vs. delta |
0.24 |
642.86 |
0.05 |
| |
pre-covid vs. omicron |
-0.04 |
-100 |
0.79 |
| |
first wave vs. delta |
0.2 |
328.57 |
0.18 |
| |
first wave vs. omicron |
-0.07 |
-100 |
0.73 |
| |
delta vs. omicron |
-0.29 |
-100 |
0.46 |
| Pterygium |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.05 |
15.55 |
0.81 |
| |
pre-covid vs. delta |
0.08 |
23.81 |
0.80 |
| |
pre-covid vs. omicron |
-0.3 |
-100 |
0.52 |
| |
first wave vs. delta |
0.03 |
7.14 |
0.92 |
| |
first wave vs. omicron |
-0.4 |
-100 |
0.30 |
| |
delta vs. omicron |
-0.4 |
-100 |
0.49 |
| Exc Eyelid Lesion |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.03 |
73.33 |
0.70 |
| |
pre-covid vs. delta |
0.10 |
271.43 |
0.32 |
| |
pre-covid vs. omicron |
0.46 |
1200 |
0.01 |
| |
first wave vs. delta |
0.08 |
114.29 |
0.58 |
| |
first wave vs. omicron |
0.43 |
650 |
0.08 |
| |
delta vs. omicron |
0.36 |
250 |
0.35 |
| Laser App |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.08 |
73.33 |
0.54 |
| |
pre-covid vs. delta |
0.03 |
23.81 |
0.85 |
| |
pre-covid vs. omicron |
-0.11 |
-100 |
0.14 |
| |
first wave vs. delta |
-0.06 |
-28.57 |
0.81 |
| |
first wave vs. omicron |
0.3 |
150 |
0.50 |
| |
delta vs. omicron |
0.36 |
250.00 |
0.35 |
| Laser Photocoagulation |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.47 |
0 |
0.00 |
| |
pre-covid vs. delta |
0.57 |
0 |
0.01 |
| |
pre-covid vs. omicron |
0 |
0 |
4.22E-05 |
| |
first wave vs. delta |
0.10 |
18.33 |
0.80 |
| |
first wave vs. omicron |
0.03 |
7.14 |
0.95 |
| |
delta vs. omicron |
-0.07 |
-15.31 |
0.94 |
| Repair RD |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.35 |
90.67 |
0.29 |
| |
pre-covid vs. delta |
-0.10 |
-25.71 |
0.79 |
| |
pre-covid vs. omicron |
-0.39 |
-100 |
0.39 |
| |
first wave vs. delta |
-0.45 |
-61.04 |
0.32 |
| |
first wave vs. omicron |
0.27 |
36.36 |
0.76 |
| |
delta vs. omicron |
0.71 |
250.00 |
0.24 |
| Ruptured Globe |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
-0.08 |
-100 |
0.28 |
| |
pre-covid vs. delta |
0.21 |
271.43 |
0.24 |
| |
pre-covid vs. omicron |
-0.08 |
-100 |
0.70 |
| |
first wave vs. delta |
0.28 |
0 |
0.15 |
| |
first wave vs. omicron |
0 |
0 |
0 |
| |
delta vs. omicron |
-0.28 |
-100 |
0.63 |
| Scleral Buckle |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.07 |
0 |
0.19 |
| |
pre-covid vs. delta |
0 |
0 |
0 |
| |
pre-covid vs. omicron |
0 |
0 |
0 |
| |
first wave vs. delta |
-0.07 |
-100 |
0.50 |
| |
first wave vs. omicron |
-0.07 |
-100 |
0.73 |
| |
delta vs. omicron |
0 |
0 |
0 |
| PPV and silicone air oil procedures |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. first wave |
0.82 |
52.19 |
0.30 |
| |
pre-covid vs. delta |
0.71 |
44.95 |
0.48 |
| |
pre-covid vs. omicron |
-1.58 |
-100 |
0.97 |
| |
first wave vs. delta |
-0.11 |
-4.76 |
0.09 |
| |
first wave vs. omicron |
-0.9 |
-37.5 |
0.62 |
| |
delta vs. omicron |
-0.79 |
-34.38 |
0.60 |
Cataracts fell in volume between the pre-covid era and first wave, but later rebounded. Volumes for retinal detachment repairs, scleral buckles, and globes did not differ significantly between waves.
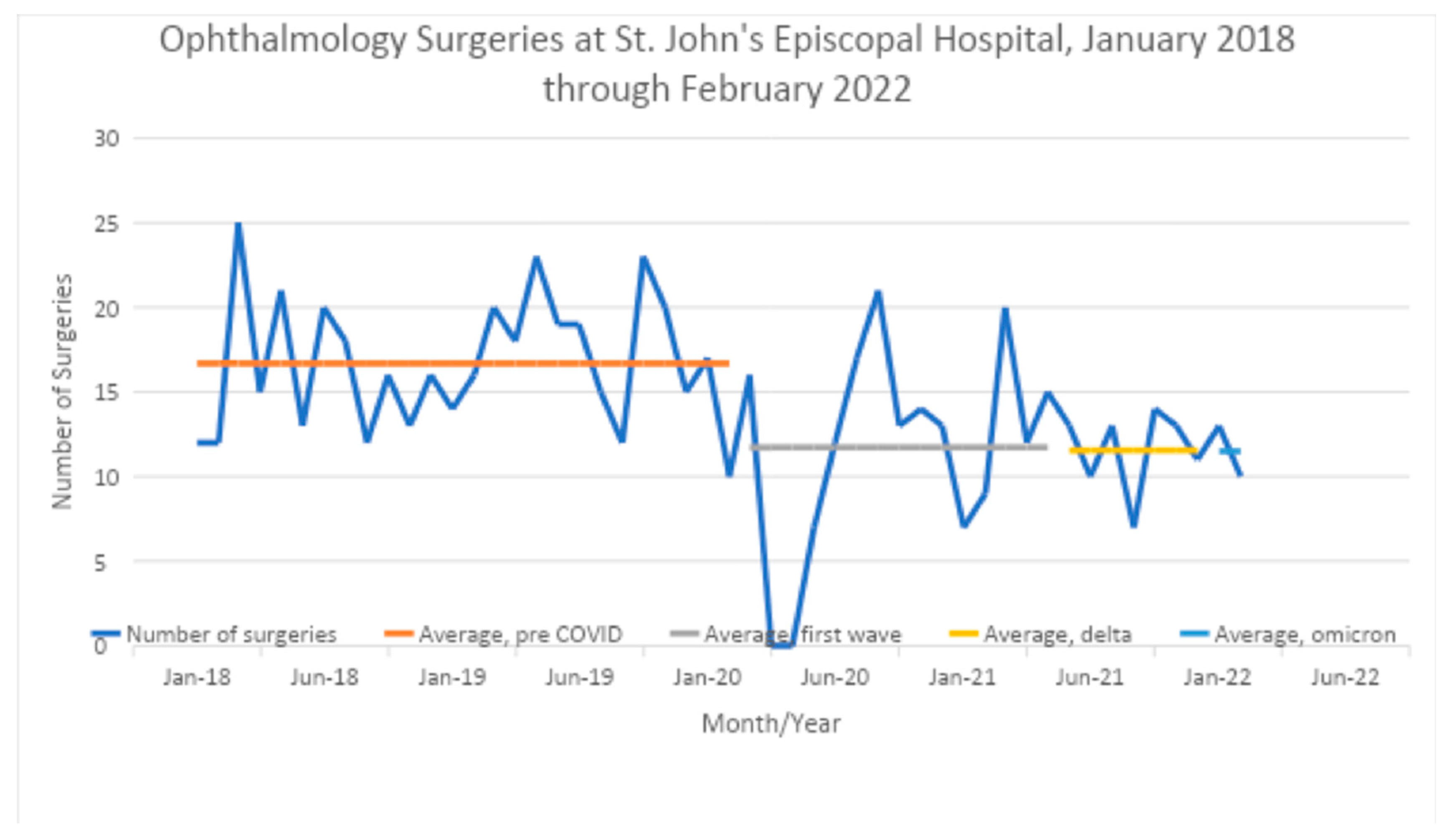
Among Ophthalmology cases (
Figure 2), the greatest significant fall in cases occurred between the pre-covid time and the delta wave (-30.7%, p<.002) (Table I) and statistically significant changes in case numbers were found when comparing pre-covid vs. the first wave, and pre-covid vs. delta. No significant changes were found when comparing the pre-covid era to omicron, the first wave to the delta or omicron waves, or when comparing the delta and omicron waves.
The large decrease between cases during the pre-covid era and the delta wave were also noted in ENT (-28.1%, p<.05), general surgery (-29.5%, p<.01), orthopedic surgery (-33.1%, p<.01), and pain management (-55.2%, p<.001)
Ophthalmology Analysis
Between pre-covid and the first wave there were small statistically significant increases in the number of cases of laser photocoagulation (p<.01) (Table II). There was also a statistically significant increase in the number of laser photocoagulation cases when comparing the pre-COVID era to the delta wave (Table II).
Retinal detachment (RD) repairs, pars plana vitrectomies/silicone removal procedures, and globe rupture repairs, showed no significant changes in volume between the waves (Table II).
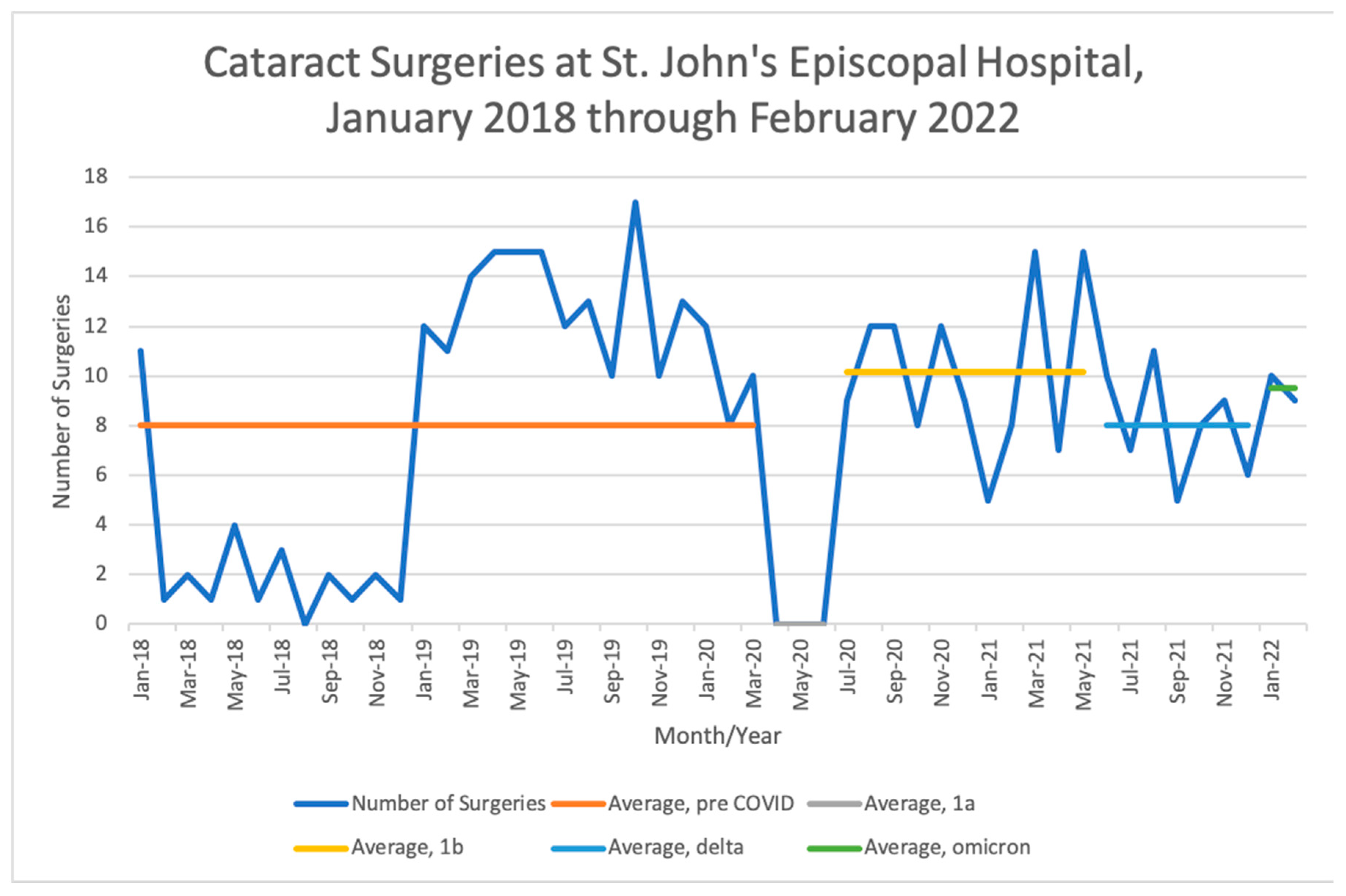
Cataract surgeries consisted the bulk of Ophthalmology surgeries performed. Elective surgeries-which included most cataract cases- were cancelled in New York between April 2020 through June 2020, however, the first wave lasted past this time period. On the premise that the ban on elective surgeries likely affected cataract volume significantly, we therefore divided the first wave into “1a” consisting of April 2020 through June 2020, and “1b” consisting of the remainder of the first wave (July 2020 through May 2021). This revealed that there was a 100% drop in cataract surgeries between the pre-covid era and the time period during which elective surgeries were cancelled (p<.05) (Table III) (
Figure 3). It also revealed that once elective surgeries were allowed to resume, there was a 127.27% increase in the number of cataract surgeries (p<.01) (Table III). Significant falls in cataract volume were found when comparing the latter half of the first wave to the delta and omicron waves (Table III,
Figure 2)
Table III: Closer Look at Cataract Surgeries.
| Cataract-Overall |
Waves |
Difference in Averages |
Percent Change |
P-Value |
| |
Pre-covid vs. 1a |
-8 |
-100 |
0.02 |
| |
pre-covid vs. 1b |
2.18 |
27.27 |
0.22 |
| |
Pre-covid vs. delta |
0 |
0 |
0 |
| |
Pre-covid vs. omicron |
1.5 |
18.75 |
0.72 |
| |
1a vs. 1b |
10.18 |
12.27 |
1.9E-186 |
| |
1a vs. delta |
8 |
N/A |
N/A |
| |
1a vs. omicron |
9.5 |
N/A |
N/A |
| |
1b vs. delta |
-2.18 |
-21.430 |
1.4E-239 |
| |
1b vs. omicron |
-0.68 |
-6.70 |
2.6E-157 |
| |
Delta vs. omicron |
1.5 |
18.75 |
0.30 |
Cataract surgeries fell in volume at the onset of the pandemic, but then rose during the first wave once the ban on surgeries was lifted-only to fall again during later waves of the pandemic.
“1a” consists of the initial wave between April 2020 through June 2020, and “1b” consists of the remainder of the first wave (July 2020 through May 2021).
4. Discussion
Data Analysis
The COVID-19 pandemic led to the disruption of hospital services and elective surgeries were reduced to preserve personal protective equipment and release beds for COVID surges. Certain surgical fields may have experienced drastic declines in volume due to their non-emergent nature. For example, the American Academy of Orthopedic Surgeons stated that elective surgeries should only be considered when the hospital had the additional staff, capacity, and resources to care for COVID patients [
22].
Our findings paralleled those of other studies- a study of sixteen general surgery programs in the US suggested that there was a 33.5% reduction in total major cases in March to June 2020 compared to 2018 and 2019. Several of the case types that declined were non-emergent, such as endoscopies and hernia surgeries, whereas trauma, liver, and pancreatic cases did not decline [
23]. Inpatient ENT case counts in June 2020 were found to be 87.9% of the level of the prior year [
24].
Ophthalmology Analysis
In March 2020, the American Academy of Ophthalmology released a statement recommending that Ophthalmologists cease treatment that is not urgent or emergent. A list of several urgent/emergent Ophthalmic surgeries was provided, including orbital biopsies for suspected malignancy, orbital decompression related to tumors, laser retinopexy for retinal detachments or tears, repair of open globe, and vitrectomy in relation to retinal detachment, ocular trauma, or vitreous hemorrhage [
25]. A delay in such procedures can lead to irreversible loss of vision, and our study found that the volumes of certain procedures such as open globe repair and retinal detachment repair did not change significantly between waves.
Our study assessed surgical volume at St. John’s Episcopal Hospital- this combined ambulatory and inpatient volumes as there is no separate ambulatory surgical site and all surgeries are done in one Operating Room. Surgical volumes at the hospital during the pandemic reflect the impact uniquely on a medically unserved community and on several nursing homes-which were an epicenter of the pandemic. There was a significant fall in cataract surgery volume at the onset of the pandemic. Elective surgeries were paused in NYC in March 2020, and there was a 100% fall in cataract surgeries between the pre-covid time period and the initial part of the first wave. Other studies also suggest that there were decreases in cataract surgeries. One retrospective cohort study using administrative claims from a nationwide health care technology clearinghouse found that cataract surgical procedures declined by 89.5% between 2019 and 2020 [
26]. Studies worldwide indicated that cataract surgeries were disrupted at the onset of the pandemic [
27,
28]. After the initial ban on elective surgeries was removed, cataract surgery volume rose. This time period still fell within the realm of the first wave of the pandemic.
There was also an increase in the number of Operating Room cases of laser photocoagulation during the first wave and delta wave as compared to the pre-COVID era. Laser photocoagulation is used for retinal conditions including diabetic retinopathy, rubeosis iridis and retinal vein occlusions. This is typically an outpatient procedure, however during the initial waves of COVID, Ophthalmology outpatient offices were closed and emergent lasers were done in the Operating Room. Those who postponed regular office follow-up due to the pandemic likely developed complications such as neovascular glaucoma, prompting laser treatment- which was done inpatient during the pandemic. In support of this claim, one Indian cross-sectional study of ophthalmic findings of 72 patients with diabetic retinopathy before and after the COVID-19 outbreak suggested that during the pandemic there was a significant progression of diabetic retinopathy and clinically significant macular edema among those with diabetes [
29]. It found an increase in the number of cases of proliferative diabetic retinopathy, vitreous hemorrhage and tractional retinal detachments during the lockdown. It is likely that the causes of progression included an inability to go to regular office appointments. The study posited that patients’ common reason for not visiting an ophthalmologist was also the fear of COVID-19 [
29]. Studies of retina practices in the Philippines suggested that during the pandemic there was a decrease in the number of clinic consults, laser procedures and intravitreal procedures done in the clinic, as only urgent cases were scheduled [
30]. Therefore, the increase in inpatient laser photocoagulation cases observed in our study was likely due to the fact that patients did not attend their routine outpatient retina appointments, due to a combination of office closures and patients’ fear of exposure to the virus. This likely worsened their conditions, prompting the need for laser treatment-which was only being done in the inpatient Operating Room setting. As elective procedures were cancelled, lasers that did take place in the Operating Room were not elective but rather deemed essential to prevent irreversible vision loss-therefore did reflect a rise in complications that led to the need for lasers in the first place.
The impact of the decrease in Ophthalmology surgical volume on residents’ training must be noted. The cancellation of these surgeries led to decreased training opportunities for residents. Ophthalmologists were deployed to other areas of need such as emergency departments, interrupting their ophthalmic training [
31].This highlights the need for virtual training and surgical simulators in the future in case of a future public health emergency [
31]. In response to the pandemic, the ACGME formulated recommendations for Competency-Based Medical Education (CBME). It recommended that residents and fellows be assessed based on competencies and that Review Committees would focus on the quality of educational programs. Per these guidelines, the program director, with input from a Clinical Competency Committee, could determine whether a trainee had achieved competence. The ACGME posited that educational experiences could be modified with alternate forms of education like virtual learning [
32].
These findings are limited as they are drawn from a retrospective study based on one specific geographical area with a unique population. It is possible that the impact of such findings may be more pronounced, or different, in other hospital settings or when multiple hospital systems are analyzed.
5. Conclusions
Our study suggests that at the onset of the COVID-19 pandemic, surgical volumes across several specialties drastically declined, and this effect was observed in subsequent COVID waves as well. This is consistent with the cancellation of elective surgeries around the world. Fields with elective surgeries were significantly affected.
The study of Ophthalmological surgical volumes during COVID is interesting as some ocular surgeries are elective, and others are emergent. The delay of an open globe repair or retinal detachment repair can lead to irreversible blindness-our study found that the rates of these surgeries were not significantly reduced.
Studies have shown that during and/or after COVID lockdown periods there have been higher rates of Ophthalmological complications such as posterior capsule rupture and cystoid macular edema [
33]. This suggests that the postponement of care and surgeries may directly correlate to an increase in complications. Our study’s noted rise on inpatient laser cases-which likely occurred due to complications from conditions like diabetic retinopathy- further cements this. This study also brings up the question of a decrease in surgical skill training for residents-it could be that interruptions in surgical training can hurt micro-surgical skills and lead to more operative complications [
33]. This further highlights the need for qualitative assessment of residents’ surgical skills over quantitative requirements during a public health emergency.
The lessons gleaned from this study are important as they may help public health authorities anticipate and plan for future surges. They also shed light on the impact of surgical cancellations on resident physicians’ training, and bring up the question of alternate forms of resident education. Several different factors, including the risk of delaying routine outpatient patient care and regular surgeries, and the risk of undertraining residents, should be taken into consideration. Currently, the avian influenza A (H5N1) viruses are considered by some to warrant planning to prevent spread and mitigate the impact of a pandemic. This virus expanded geographically in 2021 and moved around the world. These viruses have been noted to cause severe disease in mammals [
34]. Sporadic human infections have been noted as well [
35]. With the recent spread of the virus, State Health Departments are currently advised to notify the CDC about cases under investigation [
35]. This highlights that there is always a possibility of future epidemics and pandemics; knowledge of how they affect health care systems can truly help plan for future events and mitigate such effects.
This study had several limitations. It is a retrospective study, with surgical volume analysis limited to a single hospital in one unique location of New York City. St. John’s Episcopal Hospital is the only hospital in the Rockaway area, so analysis of surgical trends there may not be applicable to other areas. The study did not differentiate between inpatient surgical volumes and ambulatory surgical volumes, as at our location, all surgical procedures are performed in a single core within an inpatient environment. Far Rockaway is a geographically isolated community with an estimated population of 134,700 [
13]. Other areas may have distinct inpatient and ambulatory surgical centers, and it is possible the surgical trends during the pandemic differed between these two sites. Future studies assessing surgical volume trends amongst specialties impacted by COVID may need to consider such factors and their impact on residents’ training.
Author Contributions
Priya Sorab, MD: Conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, visualization, writing-original draft, writing-review and editing; Michael Parise, DO: Data curation, formal analysis, validation, visualization, writing-review and editing; Alexander Kaufman, BA Candidate: Data curation, formal analysis, validation, visualization, writing-review and editing; David Kirsch, MD: Data curation, methodology, project administration, supervision, validation, writing-review and editing; Norman Saffra, MD, FACS: Data curation, methodology, supervision, project administration, validation, writing-review and editing.
Funding
There were no external sources of funding. This was a retrospective data analysis.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the St. John’s Episcopal Hospital. All appropriate institutional approvals were obtained by St. John’s Episcopal Hospital IRB number EHS-22a002.
Data Availability Statement
The data is provided in tables and graphs on this manuscript. Further data can be obtained on request.
Acknowledgments
a. This study did not receive any governmental or non-governmental support
b. The authors of this study do not have any financial disclosures
c. No other acknowledgements to disclose
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ochani RK, Asad A, Yasmin F et al. COVID-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management. Infez Med. 2021;29(1):20-36.
- Schnitzler L, Janssen LMM, Evers SMAA, Jackson LJ, Paulus ATG, Roberts TE, Pokhilenko I (2021). The broader societal impacts of COVID-19 and the growing importance of capturing these in health economic analyses. Int J Technol Assess Health Care. 2021 Mar 9;37:e43. [CrossRef] [PubMed]
- Sims, B. M., Patel, A. D., Garnica, B. G., Faraj, M. T., Tang, A., Parsons, T., Hoegler, J. J., & Day, C. S. (2021). Effect of elective surgery cancellations during the COVID-19 pandemic on patients’ activity, anxiety and pain. Br J Surg, 00(O). [CrossRef]
- LaPointe J. 40 Hospitals in NY Forced to Stop Elective Surgery as COVID-19 Surges. 11 January 2022. Accessed September 07, 2022. URL: https://revcycleintelligence.com/news/40-hospitals-in-ny-forced-to-stop-elective-surgery-as-covid-19-surges.
- Hoertel N, Blachier M, Blanco C et al., Facing the COVID-19 epidemic in NYC: a stochastic agent-based model of various intervention strategies. medRxiv. Preprint. 2020 Apr 28.
- Potts III, MD, FACS, J. R. (2020). COVID-19: Special Communication to Surgical Program Directors, including Case Log Guidance. Accreditation Council for Graduate Medical Education.
- Lee SS, Ceasar D, Margolis B, Venkatesh P, Espino K, Gerber D, & Lieslie RB. The impact of the ban on elective surgery in New York City during the coronavirus outbreak on gynecologic oncology patient care. Gynecol Oncol Rep 2022;41:100997. [CrossRef]
- McGuire Woods. State Governors’ “Stay-at-Home” and Prohibition on Elective Procedures Orders. October 13, 2020. URL: https://www.mcguirewoods.com/client-resources/Alerts/2020/10/state-governors-stay-at-home-prohibition-elective-procedures-orders#NY. Accessed November 4, 2022.
- Census Reporter. NYC-Queens Community District 14-Far Rockaway, Breezy Point & Broad Channel. URL: https://censusreporter.org/profiles/79500US3604114-nyc-queens-community-district-14-far-rockaway-breezy-point-broad-channel-puma-ny/. Accessed March 17, 2023.
- NYC.gov. Neighborhood Data Profiles. URL: https://www1.nyc.gov/site/doh/covid/covid-19-data-neighborhoods.page. Accessed September 14, 2022.
- Rzewski M. St. John’s Hospital in Far Roockaway pressed by New York state to reduce services. URL https://ehs.org/about/news/new-york-safety-net-hospital-coalition-releases-policy-solutions-to-advance-health-equity-in-new-york/. Accessed July 14, 2024.
- Hill, L., & Artiga, S. (2022, August 22). COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes Over Time. KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/#:~:text=Trends%20in%20Cases&text=Early%20in%20the%20pandemic%20Hispanic.
- Census Reporter. NYC-Queens Community District 14-Far Rockaway, Breezy Point & Broad Channel. URL: https://censusreporter.org/profiles/79500US3604114-nyc-queens-community-district-14-far-rockaway-breezy-point-broad-channel-puma-ny/. Accessed March 17, 2023.
- NYS Health Profiles. URL https://profiles.health.ny.gov/nursing_home/view/150742. Accessed May 2022.
- Gold M, Shanahan E. What We Know About Cuomo’s Nursing Home Scandal. 4 August 2021. URL: https://www.nytimes.com/article/andrew-cuomo-nursing-home-deaths.html.
- The Economist. Andrew Cuomo faces a reckoning for a pandemic-related cover-up. February 20, 2021. URL: https://www.economist.com/united-states/2021/02/20/andrew-cuomo-faces-a-reckoning-for-a-pandemic-related-cover-up. Accessed November 4, 2022.
- New York State Department of Health. Factors Associated with Nursing Home Infections and Fatalities in New York State During the COVID-19 Global Health Crisis. 2021. URL: https://www.health.ny.gov/press/releases/2020/docs/nh_factors_report.pdf. Accessed November 4, 2022.
- Centers for Medicare & Medicaid Services. COVID-19 Nursing Home Data. Latest data available October 23, 2022. URL: https://data.cms.gov/covid-19/covid-19-nursing-home-data. Accessed November 4, 2022.
- Vongsachang H., Fliotsos MJ., Lorch AC et al. The impact of COVID-19 on ophthalmology resident surgical experience: a retrospective cross-sectional analysis. BMC Med Educ. 2022;22(1):142. [CrossRef]
- World Medical Association Declaration of Helsinski. Ethical principles for medical research involving human subjects. URL: https://jamanetwork.com/journals/jama/fullarticle/1760318/. Accessed March 17, 2023.
- Centers for Disease Control and Prevention. URL https://www.cdc.gov/museum/timeline/covid19.html accessed July 14, 2024.
- Lott A., Urish K.L. Recommendations regarding safety of elective surgery during COVID-19 pandemic. 2020. https://www.aaos.org/about/covid-19-information-for-our-members/guidance-for-elective-surgery/recommendations-regarding-safety-of-elective-surgery-during-covid-19/ Accessed July 14, 2024.
- Purdy, A. C., de Virgilio, C., Kaji, A. H., Shields Frey, E., Lee-Kong, S., Inaba, K., Gauvin, J. M., Neville, A. L., Donahue, T. R., Smith, B. R., Salcedo, E. S., Calhoun, K. E., Poola, V. P., Namm, J. P., Spain, D. A., Dickinson, K. J., Tanner, T., Wolfe, M., & Amersi, F. (2021, April 30). Factors Associated With General Surgery Residents’ Operative Experience During the COVID-19 Pandemic. JAMA Surgery. [CrossRef]
- Saraswathula, A., MD. (2021, April 1). National Trends in US Otolaryngology Surgical Volume During the Early COVID-19 Pandemic. Otolaryngology | JAMA Otolaryngology–Head & Neck Surgery | JAMA Network. https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2776451.
- American Academy of Ophthalmology. List of urgent and emergent ophthalmic procedures. March 27, 2020. URL https://www.aao.org/education/headline/list-of-urgent-emergent-ophthalmic-procedures accessed July 14, 2024.
- Mattingly A.S., Rose L., Eddington HS et al. Trends in US Surgical Procedures and Health Care System Response to Policies Curtailing Elective Surgical Operations During the COVID-19 Pandemic. JAMA Network Open(2021): 4(12):e2138038. [CrossRef]
- Carr F., Agarwal P., Narula H. et al. Restarting cataract surgery during the COVID-19 pandemic; a prospective study analyzing 30 day outcomes after elective cataract surgery in the United Kingdom. BMC Ophthalmology. 2021; 21:167. [CrossRef]
- Eshghi SRT, Cheema M, Damji KF. Effect of the COVID-19 pandemic on elective cataract surgery wait times. Can J Ophthalmol. 2022;S0008-4182(22)00274-5. [CrossRef]
- Prajapati V., Shah K., Shah D., Wanjari MB., Singhal D. Effect of the COVID-19 Pandemic Lockdown on the Management of Diabetic Retinopathy: A Cross-Sectional Study. Cureus. 2022;14(8):e27623. [CrossRef]
- Bromeo, AJ., Grula-Quilendrino P., Lerit SJ et al. Changes in Retina Practice Patterns During the COVID-19 Pandemic in the Philippines. Clin Ophthalmol. 2021;15:3493-3504. [CrossRef]
- Dub, N., Konopinska J., Obuchowska I, Lisowski L, Dmuchowska DA, Rekas M. The Impact of the COVID-19 Pandemic on Ophthalmology Residents: A Narrative Review. Int J Environ Res Public Health. 2021;18(21):11567. [CrossRef]
- Accreditation Council for Graduate Medical Education. Guidance Statement on Competency-Based Medical Education during COVID-10 Residency and Fellowship Disruptions. September 2020. URL: https://www.acgme.org/newsroom/2020/9/guidance-statement-on-competency-based-medical-education-during-covid-19-residency-and-fellowship-disruptions/. Accessed March 17, 2023.
- Theodoraki K., Naderi K., Lam CFJ et al. Impact of cessation of regular cataract surgery during the COVID pandemic on the rates of posterior capsular rupture and post-operative cystoid macular edema. Eye (22). [CrossRef]
- Kandel, A., Patton C., Jones JC et al. Rapid evolution of A(H5N1) influenza viruses after intercontinental spread to North America. Nat Commun. 2023;14(1):3082.
- CDC.Gov. Highly Pathogenic Avian Influenza A(H5N1) Virus in Animals: Interim Recommendations for Prevention, Monitoring, and Public Health Investigations. URL https://www.cdc.gov/flu/avianflu/hpai/hpai-interim-recommendations.html. Accessed May 28, 2024.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).