Submitted:
15 October 2024
Posted:
16 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
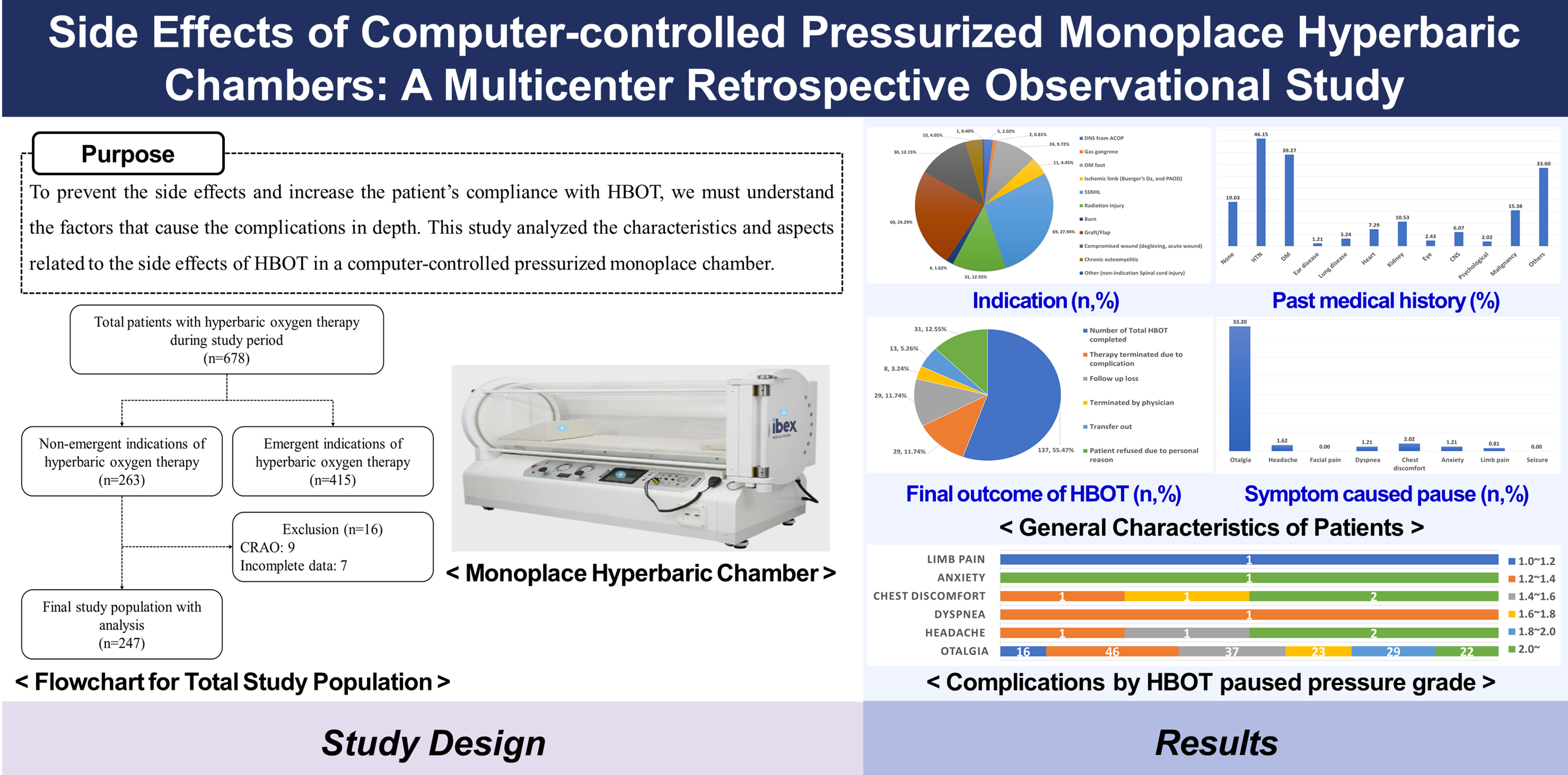
3.1. Characteristics of Study Subjects
3.2. Demographic & Clinical Differences Between Groups by HBOT Pressure Grade
3.3. Demographic & Clinical Differences Between Groups by HBOT Termination Pressure Grade
3.4. Complications by HBOT Pressure Grade
3.5. Demographic & Clinical Differences in the Otalgia Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jain, K.K.; Baydin, S.A. Textbook of hyperbaric medicine, 6th ed.; Springer; 2017.
- Mathieu, D.; Marroni, A.; Kot, J. Tenth European Consensus Conference on Hyperbaric Medicine: recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment. Diving Hyperb Med, 2017, 47(1), 24-32.
- Moon, R.E.; Bakker, D.; Barnes, R.; Bennett, M.; Camporesi, E.; Cianci, P. Hyperbaric oxygen therapy indications. 14th ed.; North Palm Beach: Best Publishing Company, FL, USA, 2017.
- Lee, S.M.; Heo, T.; Kim, K.W.; Kim, H. Current status and development direction of hyperbaric medicine in Korea. J Korean Med Assoc, 2022, 65(4), 232-238. [CrossRef]
- Weaver, L.K.; Hopkins, R.O.; Chan, K.J.; Churchill, S.; Elliott, C.G.; Clemmer, T.P.; Orme, J.F.Jr.; Thomas, F.O.; Morris, A.H. Hyperbaric oxygen for acute carbon monoxide poisoning. New Engl J Med, 2002, 347(14), 1057-1067. [CrossRef]
- Hart, G.B. Indications and contraindications for hyperbaric-oxygen therapy. J Am Med Assoc, 1976, 236(16), 1892-1892.
- Klingmann, C.; Gonnermann, A.; Dreyhaupt, J.; Vent, J.; Praetorius, M.; Plinkert, P.K. Decompression illness reported in a survey of 429 recreational divers. Aviat Space Environ Med, 2008, 79(2), 123-128. [CrossRef]
- Tibbles, P.M.; Edelsberg, J.S. Hyperbaric-oxygen therapy. New Engl J Med, 1996, 334(25), 1642-1648.
- Vahidova, D.; Sen, P.; Papesch, M.; Zein-Sanchez, M.P.; Mueller, P.H.J. Does the slow compression technique of hyperbaric oxygen therapy decrease the incidence of middle-ear barotrauma?. J Laryngol Otol, 2006, 120(6), 446-449. [CrossRef]
- Miyazawa, T.; Ueda, H.; Yanagita, N. Eustachian tube function and middle ear barotrauma associated with extremes in atmospheric pressure. Ann Otol Rhinol Laryngol Suppl, 1996, 105(11), 887-892. [CrossRef]
- Yamamoto, Y.; Noguchi, Y.; Enomoto, M.; Yagishita, K.; Kitamura, K. Otological complications associated with hyperbaric oxygen therapy. Eur Arch Otorhinolaryngol Suppl, 2016, 273, 2487-2493. [CrossRef]
- Becker, G.D.; Parell, G.J. Barotrauma of the ears and sinuses after scuba diving. Eur Arch Otorhinolaryngol Suppl, 2001, 258, 159-163. [CrossRef]
- O'Neill, O.J.; Weitzner, E.D. The O'Neill grading system for evaluation of the tympanic membrane: A practical approach for clinical hyperbaric patients. Undersea Hyperb Med, 2015, 42(3).
- Skeik, N.; Porten, B.R.; Isaacson, E.; Seong, J.; Klosterman, D.L.; Garberich, R.F.; Alexander, J.Q.; Rizvi, A.; Manunga J.M.Jr.; Cragg, A.; Graber, J.; Alden, P., Sullivan, T. Hyperbaric oxygen treatment outcome for different indications from a single center. Ann Vasc Surg, 2015, 29(2), 206-214. [CrossRef]
- Hadanny, A.; Meir, O.; Bechor, Y.; Fishlev, G.; Bergan, J.; Efrati, S. Seizures during hyperbaric oxygen therapy: retrospective analysis of 62,614 treatment sessions. Undersea Hyperb Med, 2016, 43(1).
- Zhang, Y.; Zhou, Y.; Jia, Y.; Wang, T.; Meng, D. Adverse effects of hyperbaric oxygen therapy: a systematic review and meta-analysis. Front Med, 2023, 10, 1160774. [CrossRef]
- Mathieu, D. (Ed.). Handbook on hyperbaric medicine. Springer, Dordrecht, The Netherlands, Springer, 2006; p. 812.
- Stachler, R.J.; Chandrasekhar, S.S.; Archer, S.M.; Rosenfeld, R.M.; Schwartz, S.R.; Barrs, D.M.; Brown, S.R.; Fife, T.D.; Ford, P., Ganiats, T.G.; Hollingsworth, D.B.; Lewandowski, C.A., Montano, J.J.; Saunders, J.E.; Tucci, D.L.; Valente, M.; Warren, B.E.; Yarechuk, K.L.; Robertson, P.J. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg, 2012, 146(3_suppl), S1-S35.
- Chandrasekhar, S.S.; Tsai Do, B.S.; Schwartz, S.R.; Bontempo, L.J.; Faucett, E.A.; Finestone, S.A.; Hollingsworth, D.B.; Kelly, D.M.; Kmucha, S.T.; Moonis, G.; Poling, G.L.; Roberts, J.K.; Stachler, R.J.; Zeiter, D.M.; Corrigan, M.D., Nnacheta, L.C.; Satterfield, L. Clinical practice guideline: sudden hearing loss (update). Otolaryngol Head Neck Surg, 2019, 161(1_suppl), S1-S45.
- Skevas, T.; Baumann, I.; Bruckner, T.; Clifton, N.; Plinkert, P.K.; Klingmann, C. Medical and surgical treatment in divers with chronic rhinosinusitis and paranasal sinus barotrauma. Eur Arch Otorhinolaryngol Suppl, 2012, 269, 853-860. [CrossRef]
- Heyboer 3rd, M.; Jennings, S.; Grant, W.D.; Ojevwe, C.; Byrne, J.; Wojcik, S.M. Seizure incidence by treatment pressure in patients undergoing hyperbaric oxygen therapy. Undersea Hyperb Med, 2014, 41(5), 379-385.
- Gill, A.Á.; Bell, C.N. Hyperbaric oxygen: its uses, mechanisms of action and outcomes. QJM, 2004, 97(7), 385-395. [CrossRef]
- Hadanny, A.; Abbott, S.; Suzin, G.; Bechor, Y.; Efrati, S. Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post-traumatic brain injury patients: retrospective analysis. BMJ open, 2018, 8(9), e023387. [CrossRef]
- Rozbicki, P.; Usowski, J.; Krzywdzińska, S.; Jurkiewicz, D.; Siewiera, J. Assessing the Effectiveness of Different Hyperbaric Oxygen Treatment Methods in Patients with Sudden Sensorineural Hearing Loss. Audiol Res, 2024, 14(2), 333-341. [CrossRef]
- Hwang, L.; Song, M.; Lee, Y.; Shin, T.M. Methods for preventing middle ear barotrauma in computer-controlled pressurization of monoplace hyperbaric chambers. Undersea Hyperb Med, 2019, 46(2). [CrossRef]
- Miller, R.S.; Weaver, L.K.; Bahraini, N.; Churchill, S.; Price, R.C.; Skiba, V.; Caviness, J.; Mooney, S.; Hetzell, B.; Liu, J.; Deru, K.; Ricciardi, R.; Francisco, S.; Close, N.C.; Surrett, G.W.; Bartos, C.; Margaret, R.; Brenner, L.A.; HOPPS Trial Team. Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms: a randomized clinical trial. JAMA Intern Med, 2015, 175(1), 43-52.

| Variables | Total patients (n=247) |
|---|---|
| Age, yr (M±S.D) | 59.35±15.05 |
| Male, n(%) | 157 (63.56) |
| Indication | |
| DNS from ACOP | 5 (2.02) |
| Gas gangrene | 2 (0.81) |
| DM foot | 24 (9.72) |
| Ischemic limb (Buerger’s Dz, and PAOD) | 11 (4.45) |
| SSNHL | 69 (27.94) |
| Radiation injury | 31 (12.55) |
| Burn | 4 (1.62) |
| Graft/Flap | 60 (24.29) |
| Compromised wound (degloving, acute wound) | 30 (12.15) |
| Chronic osteomyelitis | 10 (4.05) |
| Other (non-indication Spinal cord injury) | 1 (0.40) |
| Past Medical Hx., n(%) | |
| None | 47 (19.03) |
| HTN | 114 (46.15) |
| DM | 97 (39.27) |
| Ear disease | 3 (1.21) |
| Lung (asthma, COPD, Pneumothorax) | 8 (3.24) |
| Heart | 18 (7.29) |
| Kidney | 26 (10.53) |
| Eye | 6 (2.43) |
| CNS | 15 (6.07) |
| Psychological | 5 (2.02) |
| Malignancy | 38 (15.38) |
| Others | 83 (33.20) |
| Mental Status, n(%) | |
| Alert | 242 (97.98) |
| Verbal | 5 (2.02) |
| Final outcome of completed HBOT session, n(%) | |
| Number of Total HBOT completed | 137 (55.47) |
| Therapy terminated due to complication | 29 (11.74) |
| Follow up loss | 29 (11.74) |
| Terminated by physician | 8 (3.24) |
| Transfer out | 13 (5.26) |
| Patient refused due to personal reason | 31 (12.55) |
| Symptom caused treatment pause | |
| Otalgia | 82 (33.20) |
| Headache | 4 (1.62) |
| Facial pain | - |
| Dyspnea | 3 (1.21) |
| Chest discomfort | 5 (2.02) |
| Anxiety | 3 (1.21) |
| Limb pain | 2 (0.81) |
| Seizure | - |
| HBOT outcome at initial treatment | |
| Completed without pause | 162 (65.59) |
| Completed with pause | 35 (14.17) |
| Treatment terminated | 50 (20.24) |
| Pressure (kPa) |
Frequency (n, %) |
Delayed treatment time (minute) | |||
|---|---|---|---|---|---|
| Minimum | Maximum | Median [IQR] | |||
| Treatment paused pressure (n=180) |
1.0~1.2 | 17 (9.44) | 1 | 8 | 2 [1-3] |
| 1.2~1.4 | 48 (26.67) | 1 | 15 | 3 [2-5] | |
| 1.4~1.6 | 38 (21.11) | 1 | 13 | 2 [1-4] | |
| 1.6~1.8 | 23 (12.78) | 1 | 14 | 1 [1-2] | |
| 1.8~2.0 | 29 (16.11) | 1 | 7 | 2 [1-2] | |
| 2.0~ | 25 (13.89) | 1 | 10 | 3 [2-5] | |
| Treatment terminated pressure (n=50) |
1.0~1.2 | 1 (2.00) | 1 | 1 | 1 [1-1] |
| 1.2~1.4 | 9 (18.00) | 1 | 9 | 2 [1-4] | |
| 1.4~1.6 | 10 (20.00) | 1 | 4 | 1 [1-1] | |
| 1.6~1.8 | 5 (10.00) | 1 | 1 | 2 [1-2] | |
| 1.8~2.0 | 10 (20.00) | 1 | 4 | 3 [2-7] | |
| 2.0~ | 15 (30.00) | 1 | 9 | 1 [1-1] | |
| Variables | Pressure grade | p-value | |||
|---|---|---|---|---|---|
| No terminated (n=197) |
1.0~1.2 (n=1) |
1.2~2.0 (n=34) |
2.0~ (n=15) |
||
| Age, yr [IQR] | 60 [47-70] | 64 [64-64] | 61.5 [54-72] | 61 [53-69] | 0.868 |
| Male, n(%) | 129 (65.48) | 0 | 20(58.82) | 8 (53.33) | 0.345 |
| Indication, n(%) | |||||
| DNS from ACOP | 4 (2.03) | 0 | 1 (2.94) | 0 | 0.681 |
| Gas gangrene | 2 (1.02) | 0 | 0 | 0 | 1.000 |
| DM foot | 21 (10.66) | 0 | 3 (8.82) | 0 | 0.629 |
| Ischemic limb | 10 (5.08) | 0 | 1 (2.94) | 0 | 1.000 |
| SSNHL | 51 (25.89) | 1(100.00) | 9 (26.47) | 8 (53.33) | 0.047* |
| Radiation injury | 27 (13.71) | 0 | 3 (8.82) | 1 (6.67) | 0.738 |
| Burn | 3 (1.52) | 0 | 0 | 1 (6.67) | 0.316 |
| Graft/Flap | 47 (22.22) | 0 | 9 (26.47) | 4 (26.67) | 0.911 |
| Compromised wound | 24 (12.18) | 0 | 6 (17.65) | 0 | 0.337 |
| Chronic osteomyelitis | 8 (4.06) | 0 | 1 (2.94) | 1 (6.67) | 0.679 |
| Other | 0 | 0 | 1 (2.94) | 0 | 0.202 |
| Past Medical Hx., n(%) | |||||
| None | 38 (19.29) | 0 | 5 (14.71) | 4 (26.67) | 0.680 |
| HTN | 91 (46.19) | 1 (100.00) | 18 (52.94) | 4 (26.67) | 0.462 |
| DM | 83 (42.13) | 0 | 11 (32.35) | 3 (20.00) | 0.203 |
| Ear disease | 2 (1.02) | 0 | 1 (2.94) | 0 | 0.494 |
| Lung | 6 (3.05) | 0 | 2 (5.88) | 0 | 0.613 |
| Heart | 14 (7.11) | 0 | 3 (8.82) | 1 (6.67) | 0.900 |
| Kidney | 22 (11.17) | 0 | 3 (8.82) | 1 (6.67) | 1.000 |
| Eye | 6 (3.05) | 0 | 0 | 0 | 0.731 |
| Brain | 10 (5.08) | 0 | 5 (14.71) | 0 | 0.161 |
| Psychological | 4 (2.03) | 0 | 1 (2.94) | 0 | 0.681 |
| Maignancy | 34 (17.26) | 0 | 3 (8.82) | 1 (6.67) | 0.476 |
| Others | 62 (31.47) | 0 | 14 (41.18) | 6 (40.00) | 0.568 |
| Complication, n(%) | |||||
| Otalgia | 32 (16.24) | 1 (100.00) | 33 (97.06) | 15 (100.0) | <0.001*** |
| Headache | 3 (1.52) | 0 | 1 (2.94) | 0 | 0.598 |
| Dyspnea | 3 (1.52) | 0 | 0 | 0 | 1.000 |
| Chest discomfort | 3 (1.52) | 0 | 0 | 0 | 1.000 |
| Anxiety | 3 (1.52) | 0 | 0 | 0 | 1.000 |
| Limb pain | 2 (1.02) | 0 | 0 | 0 | 1.000 |
| Symptom caused treatment pause | Treatment paused pressure (kPa) | ||||||
|---|---|---|---|---|---|---|---|
| 1.0~1.2 | 1.2~1.4 | 1.4~1.6 | 1.6~1.8 | 1.8~2.0 | 2.0~ | ||
| Otalgia (n=82) |
n,% | 16 (19.51) | 46 (56.10) | 37 (45.12) | 23 (28.05) | 29 (35.37) | 22 (26.83) |
| p-value | <0.001*** | <0.001*** | <0.001*** | <0.001*** | <0.001*** | <0.001*** | |
| Headache (n=4) |
n,% | 0 | 1 (25.00) | 1 (25.00) | 0 | 0 | 2 (50.00) |
| p-value | 1.000 | 0.581 | 0.490 | 1.000 | 1.000 | 0.052 | |
| Dyspnea (n=3) |
n,% | 0 | 1 (33.33) | 0 | 0 | 0 | 0 |
| p-value | 1.000 | 0.479 | 1.000 | 1.000 | 1.000 | 1.000 | |
| Chest discomfort (n=5) |
n,% | 0 | 1 (20.00) | 0 | 1 (20.00) | 0 | 2 (40.00) |
| p-value | 1.000 | 1.000 | 1.000 | 0.389 | 1.000 | 0.081 | |
| Anxiety (n=3) |
n,% | 0 | 0 | 0 | 0 | 0 | 1 (33.33) |
| p-value | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 0.275 | |
| Limb pain (n=2) |
n,% | 1 (50.00) | 0 | 0 | 0 | 0 | 0 |
| p-value | 0.133 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |
| Variables | Pressure grade | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| No terminated (n=32) |
1.0~1.2 (n=1) |
1.2~1.4 (n=9) |
1.4~1.6 (n=10) |
1.6~1.8 (n=5) |
1.8~2.0 (n=10) |
2.0~ (n=10) |
||
| Age, yr [IQR] | 59.5 [56.5~71.5] |
64 [64-64] |
57 [48~76] |
59 [53~62] |
63 [62~68] |
64 [56~73] |
61 [53~69] |
0.861 |
| Male, n(%) | 17 (53.13) | 0 | 5(55.56) | 7 (70.00) | 3 (60.00) | 5 (50.00) | 8 (53.33) | 0.943 |
| Indication, n(%) | ||||||||
| DNS from ACOP | 3 (9.38) | 0 | 0 | 0 | 0 | 1(10) | 0 | 0.804 |
| Gas gangrene | 0 | 0 | 0 | 0 | - | |||
| DM foot | 6 (18.75) | 0 | 0 | 0 | 1 (20.00) | 2((20) | 0 | 0.219 |
| Ischemic limb | 1 (3.13) | 0 | 0 | 1 | 0 | 0 | 0 | 0.706 |
| SSNHL | 7 (21.88) | 1 (100.00) | 2 (22.22) | 3 (30.00) | 1 (20.00) | 3(30) | 8(53.33) | 0.288 |
| Radiation injury | 3 (9.38) | 0 | 0 | 2 (20.00) | 0 | 1(10) | 1(15) | 0.853 |
| Burn | 0 | 0 | 0 | 0 | 0 | 0 | 1(6.67) | 0.610 |
| Graft/Flap | 10 (31.25) | 0 | 5 (55.56) | 2 (20.00) | 0 | 2(20) | 4(26.67) | 0.445 |
| Compromised wound | 2 (6.25) | 0 | 1 | 2 (20.00) | 3 (60.00) | 0 | 0 | 0.013* |
| Chronic osteomyelitis | 0 | 0 | 1 (11.11) | 0 | 0 | 0 | 1(6.67) | 0.288 |
| Other | 0 | 0 | 0 | 0 | 0 | 1(10) | 0 | 0.427 |
| Past Medical Hx., n(%) | ||||||||
| None | 3 (9.38) | 0 | 1 (11.11) | 2 (20.00) | 1 (20.00) | 1(10) | 4(26.67) | 0.684 |
| HTN | 19 (59.38) | 1 (100.00) | 6 (66.67) | 4 (40.00) | 3 (60.00) | 5(50) | 4(26.67) | 0.313 |
| DM | 19 (59.38) | 0 | 2 (22.22) | 2 (20.00) | 3 (60.00) | 4(40) | 3(20) | 0.055 |
| Ear disease | 0 | 0 | 0 | 0 | 0 | 1(10) | 0 | 0.427 |
| Lung | 0 | 0 | 1 (11.11) | 1 (10.00) | 0 | 0 | 0 | 0.186 |
| Heart | 5 (15.63) | 0 | 0 | 1 (10.00) | 2 (40.00) | 0 | 1(6.67) | 0.307 |
| Kidney | 7 (21.88) | 0 | 0 | 1 (10.00) | 2 (40.00) | 0 | 1(6.67) | 0.213 |
| Eye | 2 (6.25) | 0 | 0 | 0 | 0 | 0 | 0 | 1.000 |
| Brain | 0 | 0 | 1 (11.11) | 2 (20.00) | 2 (40.00) | 0 | 0 | 0.006** |
| Psychological | 0 | 0 | 0 | 0 | 0 | 1(10) | 0 | 0.427 |
| Maignancy | 5 (15.63) | 0 | 0 | 2 (20.00) | 0 | 1(10) | 1(6.67) | 0.822 |
| Others | 13 (40.63) | 0 | 3 (33.33) | 5 (50.00) | 2 (40.00) | 4(40) | 6(40) | 0.995 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





