1. Introduction
VEXAS syndrome (Vacuoles, E1 enzyme, X-linked, Auto-inflammatory and Somatic), first described in 2020, is a monogenic disease resulting from a mutation in the UBA1 gene. This condition is characterized by a unique combination of systemic inflammatory and auto-immune disease (SIAD), along with hematological disorders, predominantly myelodysplastic syndromes (MDS) [
1]. Apart from VEXAS syndrome, around 10 to 30% of patients with a MDS present with SIAD features, compared to only 5% in the general population [
2]. In this review article, we will explore the mechanisms underlying the pro-inflammatory state in myelodysplastic syndromes with a particular focus on VEXAS syndrome.
2. Pro-Inflammatory State in Myelodysplastic Syndrome
MDS are blood disorders arising from clonal changes in hematopoietic stem cells (HSC). These alterations lead to ineffective hematopoiesis, characterized by dysplastic changes that result in cytopenias. Most individuals with MDS exhibit gene mutations affecting various gene classes, including epigenetic regulators (e.g. TET2, ASXL1), spliceosome genes (e.g. SF3B1, SRSF2), transcription factors (e.g. TP53, RUNX1), genes associated with signaling pathways (e.g. KRAS, JAK2), and components of the cohesin complex [
3]. The accumulation of these mutations provides the host cells proliferation advantage, resulting in cytopenias and associated disease manifestation, including hemorrhages, infections, and asthenia, as well as an increased risk of transformation into Acute Myeloid Leukemia (AML) [
4].
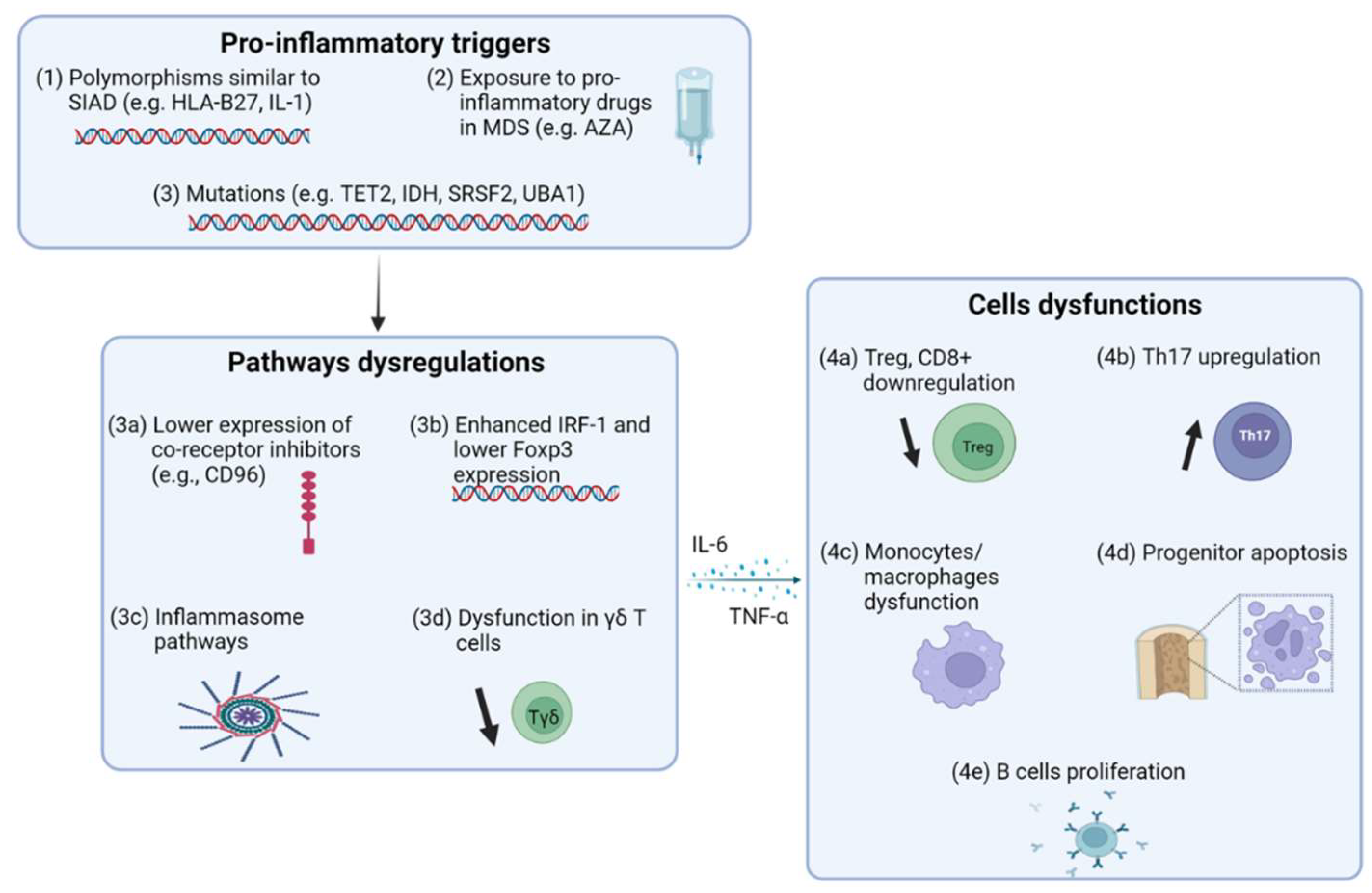
MDS are often associated with SIAD. Epidemiological data reveal that between 10% and 30% of individuals diagnosed with MDS have SIAD phenotypes, suggesting a possible link between inflammation and the pathogenesis of certain hematological disorders [
5]. The genetic immune landscape of SIAD and MDS reveals polymorphisms that link these conditions. Notably, HLA-B27, a MHC class I molecule essential for presenting peptides to T lymphocytes, is strongly associated with both spondyloarthropathies and hematological malignancies [
6]. Additionally, polymorphisms in genes involved in cytokines signaling pathways can influence the immune function, potentially leading to autoimmunity and hematological malignancies. These variations can affect the production, release, or response to cytokines, thereby disrupting the balance of pro- and anti-inflammatory signals. For example, variations in the gene encoding the IL1-receptor antagonist have been identified as risk factors for SIAD such as systemic lupus erythematous or myasthenia gravis, as well as for hematological malignancies [
7,
8,
9,
10].
In MDS, the cytokine profile indicates an upregulation of pro-inflammatory pathways, including a significant reduction in regulatory T cells (Tregs), which are essential for maintaining self-tolerance. Kordasti et al. observed this reduction in Tregs, along with an increase in Th17 cells, in patients with low-risk MDS [
11,
12]. This dysregulation is further exacerbated by an increase in the production of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which may have a pro-apoptotic effect on hematopoietic stem cells, contributing to the quantitative and functional impairment of Tregs and the expansion of Th17 cells [
12,
13,
14,
15,
16]. Moreover, Ten-eleven translocation-2 (TET2) is crucial in maintaining immune balance by actively suppressing the transcription of IL-6 during the resolution of inflammation in innate myeloid cells, such as dendritic cells and macrophages. When this regulatory function is compromised, it can lead to the persistence of an activated pro-inflammatory state, a key feature in the pathophysiology of certain hematological disorders, including MDS-associated SIAD [
17,
18,
19].
To further understand the upregulation of pro-inflammatory pathways in MDS, a French team examined the T cell phenotype in MDS patients with and without SIAD, observing a decreased Tregs count and reduced cell surface expression of immune checkpoint inhibitors (ICR), both of which are crucial for maintaining self-tolerance in patients with SIAD. Genotypic analysis revealed that these SIAD patients had higher expression of TET2, Isocitrate dehydrogenase 1 gene (IDH), Serine/arginine-rich splicing factor 2 (SRSF2) and co-occurring TET2/IDH mutations. To explore the relationship between genotype and phenotype, they compared SIAD patients with and without these mutations. In patients with mutation in the gene, was associated with a decrease in the central memory Treg (TCM) subset. Patients with TET2/IDH mutations exhibited a lower number of Tregs, central memory Tregs subset, CD8+ stem cell memory, and transitional memory cells. Moreover, the TET2/IDH mutation was linked to decreased expression of CD96, a co-inhibitory cell surface receptor, which is highly expressed by central memory T cells. Additionally, TET2 is important for the stabilization of Foxp3 expression, the canonical transcription factor for Treg function. Mutations of TET2 can lead to the downregulation of Foxp3, resulting in impaired Treg function and the development of autoimmunity. Interestingly, deficit in TET2 activity and the resulting downregulation of Foxp3 can be restored with vitamin C supplementation, offering a potential therapeutic approach [
20,
21]. Decreased Treg function in MDS patients with SIAD may also be linked to elevated levels of IRF-1 (interferon regulatory factor-1), a transcriptional regulator that inhibits Foxp3 expression. Higher IRF-1 levels have been observed in MDS patients with SIAD, further contributing to the dysfunction of Tregs in this context [
18].
γδ T cells are non-conventional T lymphocytes that play a critical role in recognizing and eliminating stressed or transformed cells, including auto-reactive cells. When γδ T cells become dysfunctional or impaired—whether due to a decrease in their numbers or reduced functional capacity—they may fail to control these auto-reactive cells effectively. This breakdown in immune surveillance can significantly contribute to the loss of self-tolerance observed in patients with MDS-associated SIAD, potentially exacerbating the inflammatory and autoimmune manifestations of the disease (
Figure 1) [
22,
23]. Some studies also associate inflammation among MDS patients with NLRP3 inflammasome activation. This suggests potential targets for anti-IL-1 therapies [
24].
3. Pro-Myelodysplastic State in Inflammation
Conversely, certain aspects of inflammation process could contribute to the development of MDS. Some SIAD appear many years before the onset of MDS, suggesting that they may represent a risk factor for the disease. A study based on the US Surveillance Epidemiology and End Results (SEER) database found a higher risk of developing acute myeloid leukemia (AML) (OR 1.29) and MDS (OR 1.50) among patients with auto-immune diseases. Specifically, AML was associated with rheumatoid arthritis (OR 1.28), systemic lupus erythematosus (OR 1.92), polymyalgia rheumatica (OR 1.73), autoimmune hemolytic anemia (OR 3.74), systemic vasculitis (OR 6.23), ulcerative colitis (OR 1.72) and pernicious anemia (OR 1.57). Myelodysplastic syndrome was associated with rheumatoid arthritis (OR1.52) and pernicious anemia (OR 2.38) [
25]. Inflammation, even caused by infection, may be a risk factor for developing MDS (
Table 1) [
26].
4. Comparison between MDS with and without SIAD
In terms of peripheral blood characteristics, patients with SIAD tend to exhibit a higher absolute neutrophil count in univariate analysis (OR 1.06, 95% CI [1.01; 1.12]) [
27]. Interestingly, autoantibodies were detected in 50% of MDS patients without SIAD, possibly due to the inherent tendency of MDS to present with auto-inflammatory features, which primarily drive by dysfunction of innate immunity rather than adaptative immunity [
28,
29]. Recent studies have highlighted significant molecular and clinical differences between MDS patients with and without SIAD. Lower-risk MDS, a subset of MDS characterized by a better prognosis, slower progression, fewer blast cells in the bone marrow, and milder cytopenias, is more frequently associated with SIAD patients. These lower-risk cases have a reduced likelihood of transforming into acute myeloid leukemia (AML) compared to higher-risk MDS. In multivariate analysis, SIAD MDS also presented with fewer blasts (OR 0.86, 95% CI [0.78; 0.93], p < 0.01). Even though caryotype seem similar in MDS with or without SIAD, MDS associated with pseudo-Behçet syndrome have been described with trisomy 8 [
30]. Furthermore, TET2 mutations are more prevalent among SIAD MDS patients (46% vs 34%, p = 0.04), although in the variant allele frequency (VAF) does not differ significantly between the groups [
27]. This finding is supported by another study that showed TET2-mutated MDS patients have a higher incidence of autoimmune features (31.3% vs. 5.3%, p = 0.001) [
31]. Additionally, IDH1/2 mutations are more frequent in the SIAD MDS cohort (14% vs. 4%, p < 0.01), with a higher VAF observed in SIAD patients (38% vs. 26%, p = 0.04). SRSF2 mutations are more common in SIAD MSD patients (31% vs. 15%, p < 0.01). These molecular markers, particularly TET2/IDH (OR 1.87, 95% CI [1.08; 3.2], p = 0.02) and SRSF2 (OR 2.21, 95% CI [1.14; 4.28], p = 0.02), underscore the unique genetic landscape of SIAD MDS and may contribute to their distinct clinical presentation and prognosis [
27].
Data on overall survival (OS) in MDS patients with and without SIAD are inconclusive. While some studies suggest that OS is lower in SIAD MSD patients, other report no significant difference. A review of multiple studies presents mixed results, likely due to the retrospective nature of most studies, which introduces potential bias (
Table 2). Furthermore, the heterogeneity of SIAD manifestations further complicates the interpretation of outcomes. Over the last decade, significant advancements in the treatment of both SIAD and MDS have added another layer of complexity to comparing survival outcomes across different patient cohorts.
3. VEXAS Syndrome
VEXAS syndrome belongs to a group of diseases known as proteasomopathies, which are characterized by abnormalities in the function or regulation of the proteasome, a cellular structure responsible for degrading proteins that have been tagged with ubiquitin. Ubiquitylation, a reversible post-translational modification, is crucial for regulating cellular responses to immune signals [
32]. VEXAS syndrome is caused by mutations in the UBA1 gene, leading to dysfunction of ubiquitin-like modifier activating E1 enzyme, the most important enzyme in the ubiquitylation cascade [
1]. UBA1's function cannot be compensated by another enzyme, and its impairment results in the accumulation of proteins. This protein aggregation triggers the unfolded protein response (UPR) and activates several inflammatory pathways such as NF-κB and interferon pathways, resulting in a pro-inflammatory state [
32]. Clinically, VEXAS syndrome primarily affects men and is marked by systemic inflammatory and autoimmune diseases (SIAD), with symptoms including systemic inflammation, hematologic abnormalities (including macrocytic anemia, thrombocytopenia, and vacuoles in myeloid and erythroid precursor cells), recurrent skin rashes, pulmonary manifestations, chondritis and arthritis (
Table 3) [
32].
3.1. Is the MDS Homeostasis in VEXAS Similar to Other MDS?
A French cohort study on VEXAS syndrome found that 24% of the 75 MDS had additional somatic mutations, predominantly in DNMT3A and TET2. Similarly, a study by the NIH/Mayo clinic reported clonal hematopoiesis in 80 VEXAS patients with or without MDS. Among them, 35% had one non-UBA1 clonal hematopoiesis mutation, and 25% had two or more. These findings confirmed the results from the French cohort, with most mutations affecting DNMT3A and TET2 genes [
33]. In the bone marrow, VEXAS patients typically present with vacuoles (also sometimes observed in peripheral blood), hypercellularity, granulocytic hyperplasia, mild dyspoiesis, usually a normal karyotype, and fewer blasts. MDS associated with VEXAS syndrome often has a lower risk profile and tends to involve fewer mutations compared to MDS without VEXAS [
34].
The precise relationship between the UBA1 clone and the development of MDS remains uncertain. It is unclear whether the UBA1 clone directly initiates the events that lead to MDS, or if the myeloid neoplasm develops because of the inflammatory microenvironment driving clonal selection. It is worth noting that various diseases characterized by high levels of inflammation, such as Giant Cell Arteritis, Periarteritis Nodosa, Behçet and others, may exhibit a lower tendency to induce MDS than VEXAS [
35].
The overall risk profile of MDS, estimated by the IPSS (International Prognostic Scoring System) or R-IPSS (Revised International Prognostic Scoring System), was examined by Ferrada et al., who found that 96% of 23 patients had a low or very low risk profile to develop AML [
34]. A Swiss cohort of 17 patients, two third of whom had had MDS, reported no cases of increased blasts in the bone marrow [
36]. To date, only a few cases of MDS associated with VEXAS have progressed to AML. VEXAS patients, according to IPSS scores, generally have a lower-risk profile MDS compared to those not associated with VEXAS. Since VEXAS primarily affects older patients with a median life expectancy of 10 years, the duration of the inflammatory state may not be sufficient to promote the development of AML. Despite being classified as low-risk MDS, VEXAS patients often experience severe cytopenia and a significant need for transfusions. This has led some authors to characterize VEXAS as "a highly inflammatory clonal cytopenia” [
34,
37].
3.2. Therapeutic Approach
Concerning higher risk MDS, a subset of MDS characterized by a worst prognosis, faster progression, more blast cells in the bone marrow, and severe cytopenias, 5-azacytidine (AZA) is one of the main treatments. This nucleoside analog chemotherapy works by inhibiting DNA methylation. It is administered via injection and is often prescribed to patients who are not candidates for stem cell transplantation. Patients treated with AZA may experience myelosuppression, leading to cytopenias, which can sometimes limit its use. Moreover, AZA may induce inflammatory SIAD, such as neutrophilic dermatosis. A study involving patients with SIAD and MDS found that 19 out of 22 individuals treated with AZA experienced positive effects on SIAD symptoms, with most able to discontinue their immunosuppressive therapy as a result [
38]. Research on AZA’s impact demonstrated that, although treatment increased Treg levels, these cells lacked the ability to proliferate. In vitro studies further revealed that 5-azacytidine reduced the suppressive function of CD4+ regulatory T cells and increased the production of interleukin-17 [
39].
For VEXAS, the current consensus treatment involves corticosteroids combined with an additional immunosuppressive agent, such as anti-IL6, anti-IL1, or JAKi (Janus kinase inhibitors). JAKi, such as ruxolitinib, have shown both anti-inflammatory and potential anti-clonal effects in studies involving myelofibrosis patients, although conclusive evidence of their anti-clonal benefits in VEXAS is still lacking. Surveillance of VAF levels during ruxolitinib treatment for UBA1 mutations has failed to show any notable decrease [
40]. Clinical studies have suggested that AZA may be capable of inducing complete molecular clearance of UBA1 mutations. IDH1 and IDH2 inhibitors, such as Ivosidenib and Enasidenib, have shown promising results in treating MDS with mutations in these genes. Since these mutations are also implicated in both MDS and VEXAS syndrome, IDH inhibitors may offer potential therapeutic benefits for these conditions [
41].
3.2. Is there a Place to Treat the Clone in VEXAS without MDS?
Comont et al. reported on five patients with UBA1 mutation but without diagnostic criteria for a myelodysplastic syndrome treated with AZA with a very good outcome. All five patients achieved a complete inflammatory response, with no relapse observed over a follow-up period ranging from 4 to 37 months, indicating a very favorable outcome [
42].
4. Conclusions
VEXAS syndrome represents a unique intersection of genetic and inflammatory pathophysiology, primarily driven byUBA1 gene mutations. This syndrome illustrates the complex interplay between systemic auto-inflammatory and autoimmune diseases (SIAD) and hematological disorders, particularly myelodysplastic syndromes (MDS). VEXAS patients exhibit distinct clinical features, including a higher prevalence of specific somatic mutations (DNMT3A, TET2), unique bone marrow characteristics, and a generally lower risk of MDS progression. However, despite this lower risk, patients suffer from significant cytopenias and have high transfusion needs due to the syndrome's inflammatory nature.
Treatment strategies for VEXAS differ from typical MDS therapies, frequently involving corticosteroids and immunosuppressive agents. AZA offers significant promise, particularly with its ability to induce complete molecular clearance of UBA1 mutations, making it a promising therapeutic option for managing both the hematological and inflammatory aspects of VEXAS syndrome. For selected patients younger and fit patients, allogeneic stem cell transplantation should be considered, as it remains the only curative option. The persistent inflammatory state in VEXAS not only worsens hematologic dysfunction but also undersocres the bidirectional relationship between inflammation and clonal hematopoiesis. Further research is critical to fully understand the mechanisms underlying this relationship and to develop targeted therapies that effectively address both the inflammatory and hematologic components of VEXAS syndrome.
Author Contributions
Conceptualization, L.W; resources, L.W. and L.C.; writing—original draft preparation, L.W. and L.C.; writing—review and editing, D.C., S.B. and L.-P.Z.; supervision, D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Beck DB, Ferrada MA, Sikora KA, Ombrello AK, Collins JC, Pei W, et al. Somatic Mutations in UBA1 and Severe Adult-Onset Autoinflammatory Disease. N Engl J Med 2020;383:2628–38. [CrossRef]
- Braun T, Fenaux P. Myelodysplastic Syndromes (MDS) and autoimmune disorders (AD): cause or consequence? Best Pract Res Clin Haematol 2013;26:327–36. [CrossRef]
- Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 2014;28:241–7. [CrossRef]
- Garcia-Manero G. Myelodysplastic syndromes: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol 2023;98:1307–25. [CrossRef]
- Stalder G, Ribi C, Alberio L. Syndromes myélodysplasiques et auto-immunité. Rev Med Suisse 2015;469:820–5.
- Au WY, Hawkins BR, Cheng N, Lie AK, Liang R, Kwong YL. Risk of haematological malignancies in HLA-B27 carriers. Br J Haematol 2001;115:320–2. [CrossRef]
- Cai L, Zhang J, Xue X, Wang Z, Wang J, Tang S, et al. Meta-analysis of associations of IL1 receptor antagonist and estrogen receptor gene polymorphisms with systemic lupus erythematosus susceptibility. PloS One 2014;9:e109712. [CrossRef]
- Bodis G, Toth V, Schwarting A. Role of Human Leukocyte Antigens (HLA) in Autoimmune Diseases. Rheumatol Ther 2018;5:5–20. [CrossRef]
- Demeter J, Messer G, Rämisch S, Mee JB, di Giovine FS, Schmid M, et al. Polymorphism within the second intron of the IL-1 receptor antagonist gene in patients with hematopoietic malignancies. Cytokines Mol Ther 1996;2:239–42.
- Huang D, Pirskanen R, Hjelmström P, Lefvert AK. Polymorphisms in IL-1beta and IL-1 receptor antagonist genes are associated with myasthenia gravis. J Neuroimmunol 1998;81:76–81. [CrossRef]
- Kordasti SY, Afzali B, Lim Z, Ingram W, Hayden J, Barber L, et al. IL-17-producing CD4(+) T cells, pro-inflammatory cytokines and apoptosis are increased in low risk myelodysplastic syndrome. Br J Haematol 2009;145:64–72. [CrossRef]
- Kordasti SY, Ingram W, Hayden J, Darling D, Barber L, Afzali B, et al. CD4+CD25high Foxp3+ regulatory T cells in myelodysplastic syndrome (MDS). Blood 2007;110:847–50. [CrossRef]
- Maciejewski JP, Selleri C, Sato T, Anderson S, Young NS. Increased expression of Fas antigen on bone marrow CD34+ cells of patients with aplastic anaemia. Br J Haematol 1995;91:245–52. [CrossRef]
- Zeng W, Miyazato A, Chen G, Kajigaya S, Young NS, Maciejewski JP. Interferon-γ-induced gene expression in CD34 cells: identification of pathologic cytokine-specific signature profiles. Blood 2006;107:167–75. [CrossRef]
- Kitagawa M, Saito I, Kuwata T, Yoshida S, Yamaguchi S, Takahashi M, et al. Overexpression of tumor necrosis factor (TNF)-alpha and interferon (IFN)-gamma by bone marrow cells from patients with myelodysplastic syndromes. Leukemia 1997;11:2049–54. [CrossRef]
- Gañán-Gómez I, Wei Y, Starczynowski DT, Colla S, Yang H, Cabrero-Calvo M, et al. Deregulation of innate immune and inflammatory signaling in myelodysplastic syndromes. Leukemia 2015;29:1458–69. [CrossRef]
- Zhang Q, Zhao K, Shen Q, Han Y, Gu Y, Li X, et al. Tet2 is required to resolve inflammation by recruiting Hdac2 to specifically repress IL-6. Nature 2015;525:389–93. [CrossRef]
- Shiromizu CM, Jancic CC. γδ T Lymphocytes: An Effector Cell in Autoimmunity and Infection. Front Immunol 2018;9:2389. [CrossRef]
- Jachiet V, Fenaux P, Sevoyan A, Hakobyan Y, Ades L, Fain O, et al. Inflammatory and Immune Disorders Associated with Myelodysplastic Syndromes. Hemato 2021;2:329–46. [CrossRef]
- Yue X, Trifari S, Äijö T, Tsagaratou A, Pastor WA, Zepeda-Martínez JA, et al. Control of Foxp3 stability through modulation of TET activity. J Exp Med 2016;213:377–97. [CrossRef]
- Yue X, Rao A. TET family dioxygenases and the TET activator vitamin C in immune responses and cancer. Blood 2020;136:1394–401. [CrossRef]
- Kiladjian J-J, Visentin G, Viey E, Chevret S, Eclache V, Stirnemann J, et al. Activation of cytotoxic T-cell receptor γδ T lymphocytes in response to specific stimulation in myelodysplastic syndromes. Haematologica 2008;93:381–9. [CrossRef]
- Chan, C. J. et al. The receptors CD96 and CD226 oppose each other in the regulation of natural killer cell functions. Nature immunology - Recherche Google n.d. https://www.google.com/search?client=firefox-b-d&q=Chan%2C+C.+J.+et+al.+The+receptors+CD96+and+CD226+oppose+each+other+in+the+regulation+of+natural+killer+cell+functions.+Nature+immunology (accessed June 10, 2024).
- Vallelonga V, Gandolfi F, Ficara F, Della Porta MG, Ghisletti S. Emerging Insights into Molecular Mechanisms of Inflammation in Myelodysplastic Syndromes. Biomedicines 2023;11:2613. [CrossRef]
- Anderson LA, Pfeiffer RM, Landgren O, Gadalla S, Berndt SI, Engels EA. Risks of myeloid malignancies in patients with autoimmune conditions. Br J Cancer 2009;100:822–8. [CrossRef]
- Kristinsson SY, Björkholm M, Hultcrantz M, Derolf ÅR, Landgren O, Goldin LR. Chronic immune stimulation might act as a trigger for the development of acute myeloid leukemia or myelodysplastic syndromes. J Clin Oncol Off J Am Soc Clin Oncol 2011;29:2897–903. [CrossRef]
- Zhao L-P, Boy M, Azoulay C, Clappier E, Sébert M, Amable L, et al. Genomic landscape of MDS/CMML associated with systemic inflammatory and autoimmune disease. Leukemia 2021;35:2720–4. [CrossRef]
- Fraison J-B, Grignano E, Braun T, Adès L, Chollet-Martin S, Roland-Nicaise P, et al. Autoantibodies in myelodysplastic syndromes and chronic myelomonocytic leukemia. Leuk Lymphoma 2019;60:2594–6. [CrossRef]
- Hamidou MA, Derenne S, Audrain MA, Berthelot JM, Boumalassa A, Grolleau JY. Prevalence of rheumatic manifestations and antineutrophil cytoplasmic antibodies in haematological malignancies. A prospective study. Rheumatol Oxf Engl 2000;39:417–20. [CrossRef]
- Lin Y-C, Liang T-H, Chang H-N, Lin J-S, Lin H-Y. Behçet disease associated with myelodysplastic syndrome. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 2008;14:169–74. [CrossRef]
- Oh Y-J, Shin D-Y, Hwang SM, Kim S-M, Im K, Park HS, et al. Mutation of ten-eleven translocation-2 is associated with increased risk of autoimmune disease in patients with myelodysplastic syndrome. Korean J Intern Med 2020;35:457–64. [CrossRef]
- Beck DB, Werner A, Kastner DL, Aksentijevich I. Disorders of ubiquitylation: unchained inflammation. Nat Rev Rheumatol 2022;18:435–47. [CrossRef]
- Gutierrez-Rodrigues F, Kusne Y, Fernandez J, Lasho T, Shalhoub R, Ma X, et al. Spectrum of clonal hematopoiesis in VEXAS syndrome. Blood 2023;142:244–59. [CrossRef]
- Ferrada MA, Savic S, Cardona DO, Collins JC, Alessi H, Gutierrez-Rodrigues F, et al. Translation of cytoplasmic UBA1 contributes to VEXAS syndrome pathogenesis. Blood 2022;140:1496–506. [CrossRef]
- Roupie AL, Guedon A, Terrier B, Lahuna C, Jachiet V, Regent A, et al. Vasculitis associated with myelodysplastic syndrome and chronic myelomonocytic leukemia: French multicenter case-control study. Semin Arthritis Rheum 2020;50:879–84. [CrossRef]
- Caratsch L, Wolff L, Comte D, Lötscher F, Seitz L, Seitz P, et al. VEXAS syndrome: a Swiss national retrospective cohort study 2024. [CrossRef]
- Georgin-Lavialle S, Terrier B, Guedon AF, Heiblig M, Comont T, Lazaro E, et al. Further characterization of clinical and laboratory features in VEXAS syndrome: large-scale analysis of a multicentre case series of 116 French patients. Br J Dermatol 2022;186:564–74. [CrossRef]
- Fraison J-B, Mekinian A, Grignano E, Kahn J-E, Arlet J-B, Decaux O, et al. Efficacy of Azacitidine in autoimmune and inflammatory disorders associated with myelodysplastic syndromes and chronic myelomonocytic leukemia. Leuk Res 2016;43:13–7. [CrossRef]
- Costantini B, Kordasti SY, Kulasekararaj AG, Jiang J, Seidl T, Abellan PP, et al. The effects of 5-azacytidine on the function and number of regulatory T cells and T-effectors in myelodysplastic syndrome. Haematologica 2013;98:1196–205. [CrossRef]
- Heiblig M, Ferrada MA, Koster MJ, Barba T, Gerfaud-Valentin M, Mékinian A, et al. Ruxolitinib is more effective than other JAK Inhibitors to treat VEXAS Syndrome: a retrospective multi center study. Blood 2022:blood.2022016642. [CrossRef]
- Cerchione C, Romano A, Daver N, DiNardo C, Jabbour EJ, Konopleva M, et al. IDH1/IDH2 Inhibition in Acute Myeloid Leukemia. Front Oncol 2021;11:639387. [CrossRef]
- Jachiet V, Kosmider O, Heiblig M, Terrier B, Le Guenno G, Outh R, et al. Efficacité et tolérance de l’azacitidine au cours du syndrome VEXAS avec et sans syndrome myélodysplasique : données du registre français. Rev Médecine Interne 2023;44:A356–7. [CrossRef]
- Maeda A, Tsuchida N, Uchiyama Y, Horita N, Kobayashi S, Kishimoto M, et al. Efficient detection of somatic UBA1 variants and clinical scoring system predicting patients with variants in VEXAS syndrome. Rheumatol Oxf Engl 2023:kead425. [CrossRef]
- Mascaro JM et al. Spanish cohort of VEXAS syndrome: clinical manifestations, outcome of treatments and novel evidences about UBA1 mosaicism. Ann Rheum Dis. 2023 Dec;82(12):1594–605 - Recherche Google n.d. https://www.google.com/search?client=firefox-b-d&q=Mascaro+JM+et+al.+Spanish+cohort+of+VEXAS+syndrome%3A+clinical+manifestations%2C+outcome+of+treatments+and+novel+evidences+about+UBA1+mosaicism.+Ann+Rheum+Dis.+2023+Dec%3B82%2812%29%3A1594%E2%80%93605 (accessed June 12, 2024).
- A M, E G, T B, O D, E L, N C-C, et al. Systemic inflammatory and autoimmune manifestations associated with myelodysplastic syndromes and chronic myelomonocytic leukaemia: a French multicentre retrospective study. Rheumatol Oxf Engl 2016;55. [CrossRef]
- Giannouli S, Voulgarelis M, Zintzaras E, Tzioufas AG, Moutsopoulos HM. Autoimmune phenomena in myelodysplastic syndromes: a 4-yr prospective study. Rheumatol Oxf Engl 2004;43:626–32. [CrossRef]
- Hollanda A de, Beucher A, Henrion D, Ghali A, Lavigne C, Lévesque H, et al. Systemic and immune manifestations in myelodysplasia: A multicenter retrospective study. Arthritis Care Res 2011;63:1188–94. [CrossRef]
- Komrokji RS, Kulasekararaj A, Al Ali NH, Kordasti S, Bart-Smith E, Craig BM, et al. Autoimmune diseases and myelodysplastic syndromes. Am J Hematol 2016;91:E280-283. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).